Acromioclavicular Reconstruction Using the Lockdown Technique: A Case Series and Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Methods of the Case-Series Study
2.1.1. Patient Selection
2.1.2. Data Extraction, Data Types, and Measures
2.1.3. Surgical Technique
2.1.4. Outcomes
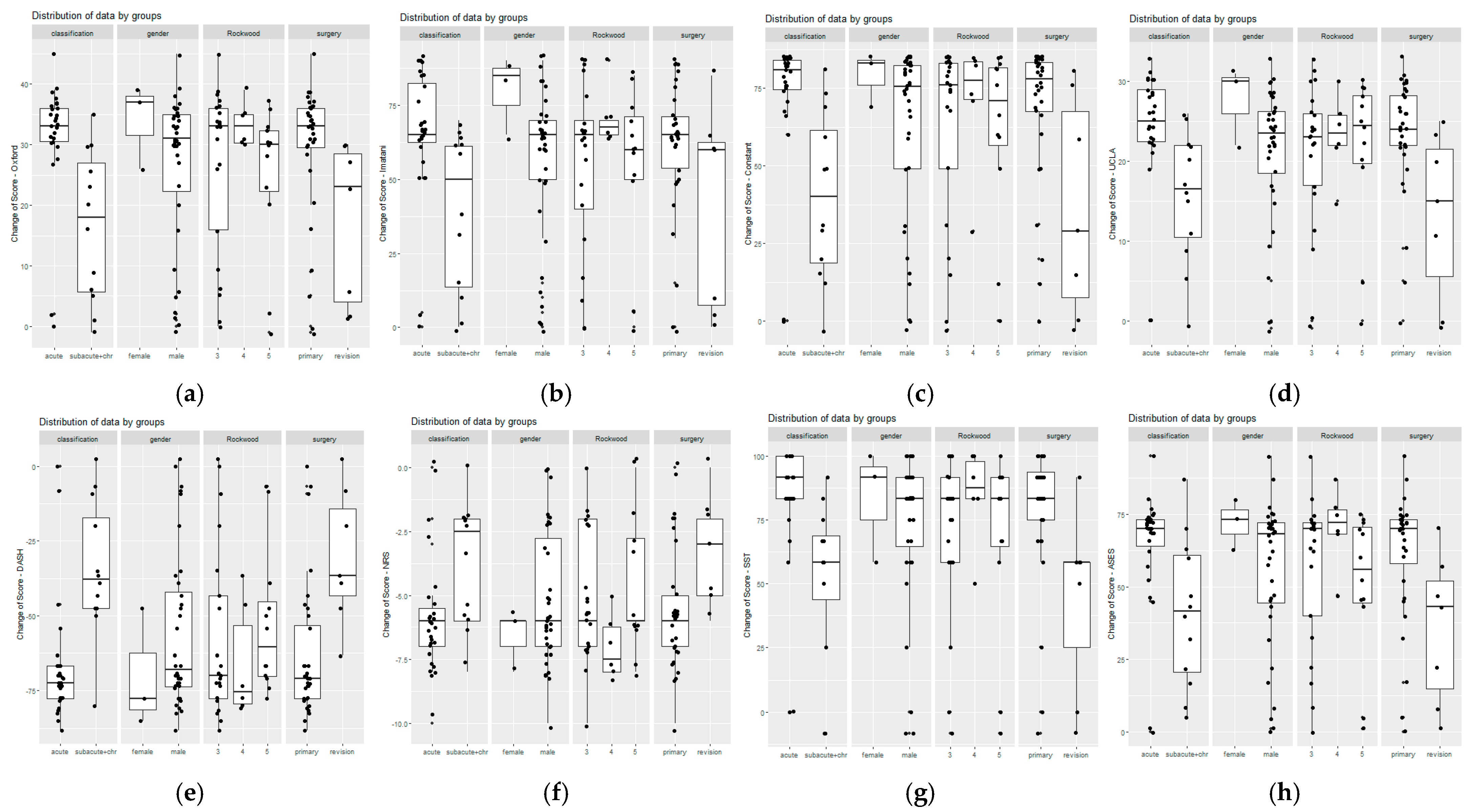
2.1.5. Statistical Methods
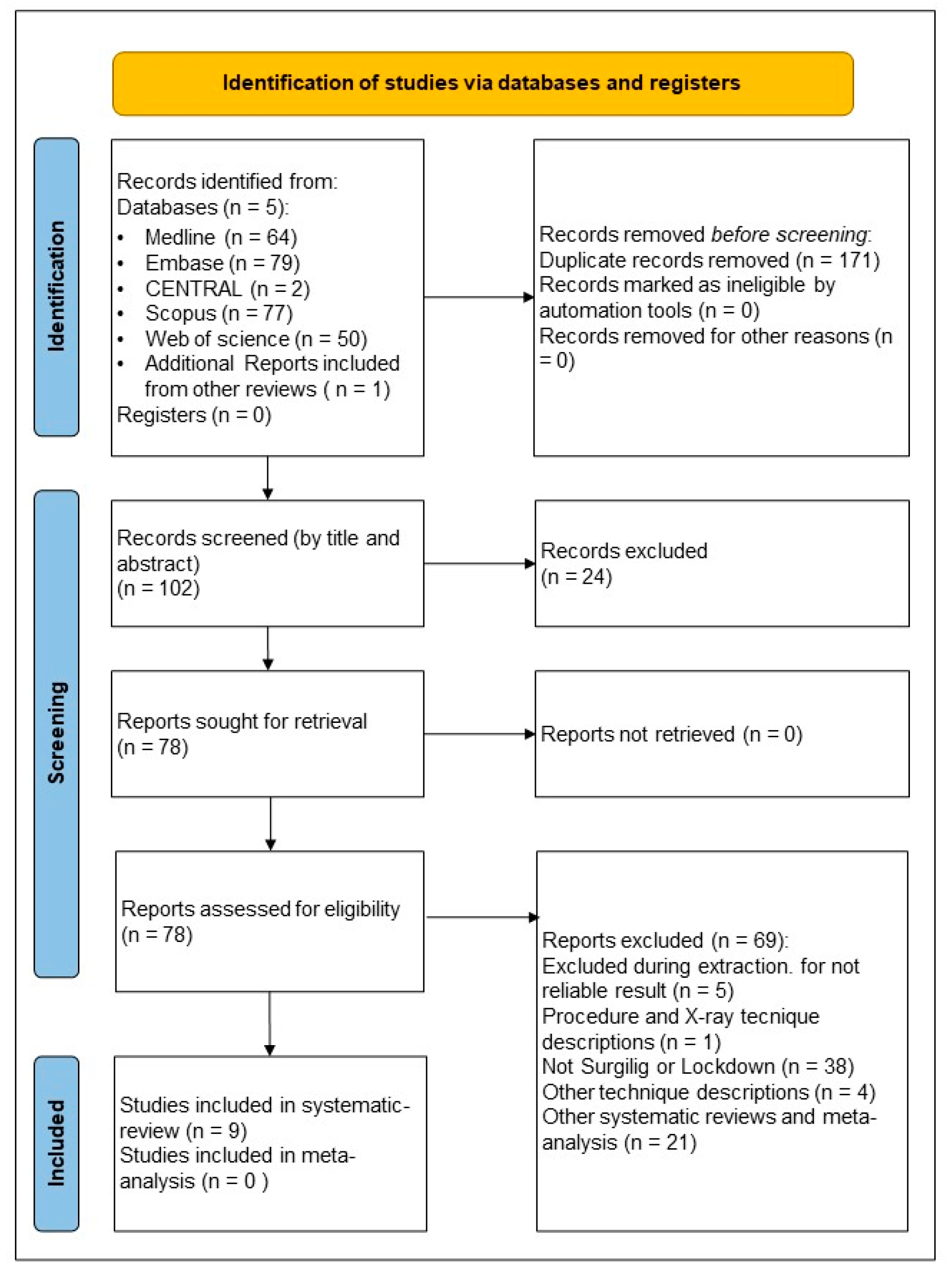
2.2. Methods of the Systematic Review
2.2.1. Information Sources and Search Strategy
2.2.2. Selection Process
2.2.3. Eligibility Criteria
2.2.4. Data Collection Process and Data Items
2.2.5. Evaluation of the Studies and Study Risk of Bias Assessment
3. Results
3.1. Case-Series Study
3.1.1. Case-Series Study, Basic Characteristics
3.1.2. Case-Series Study, Outcomes
3.2. Systematic Search
3.2.1. Systematic Search, Basic Characteristics
3.2.2. Systematic Search, Outcomes
3.2.3. Systematic Search, Complications
3.2.4. Systematic Search, Risk of Bias Assessment
4. Discussion
4.1. Strength and Limitation
4.2. Implications for Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AC | acromioclavicular |
| CC | coracoclavicular |
| OSS | Oxford shoulder score |
| LD | Linear dichroism |
| ORTSD | open reduction and suspensory device fixation |
| UCLA | University of California-Los Angeles shoulder score |
| ASES | American shoulder and elbow surgeons |
| SST | simple shoulder test |
| DASH | disabilities of the arm, shoulder, and hand |
| NRS | numerical Rating Scale |
| vs. | versus |
| spf. | superficial |
| SR | systematic review |
| MA | meta-analysis |
| K-wire | Kirschner wire |
| MCID | minimal clinically important difference |
| NA | not available |
References
- Cook, J.B.; Krul, K.P. Challenges in Treating Acromioclavicular Separations: Current Concepts. J. Am. Acad. Orthop. Surg. 2018, 26, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, M.F.; Sircana, G.; Cardona, V.; Vismara, V.; Scaini, A.; Salvi, A.G.; Galli, S.; Marchi, G.; Milano, G. Biologic and Synthetic Ligament Reconstructions Achieve Better Functional Scores Compared to Osteosynthesis in the Treatment of Acute Acromioclavicular Joint Dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2175–2193. [Google Scholar] [CrossRef]
- Court-Brown, C.M.; Heckman, J.D.; McQueen, M.M.; Ricci, W.M.; Tornetta, P.; McKee, M.D. Rockwood and Green’s Fractures in Adults; Wolters Kluwer Health: Philadelphia, PA, USA, 2015. [Google Scholar]
- Sirin, E.; Aydin, N.; Mert Topkar, O. Acromioclavicular Joint Injuries: Diagnosis, Classification and Ligamentoplasty Procedures. EFORT Open Rev. 2018, 3, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Carlos, A.J.; Richards, A.M.; Corbett, S.A. Stabilization of Acromioclavicular Joint Dislocation Using the ‘Surgilig’ Technique. Shoulder Elb. 2011, 3, 166–170. [Google Scholar] [CrossRef]
- Kani, K.K.; Porrino, J.A.; Mulcahy, H.; Chew, F.S. Surgical Techniques for Management of Acromioclavicular Joint Separations: Review and Update for Radiologists. Skelet. Radiol. 2020, 49, 1195–1206. [Google Scholar] [CrossRef]
- Hartland, A.W.; Nayar, S.K.; Teoh, K.H.; Rashid, M.S. Clinical Effectiveness of Various Surgical Reconstruction Modalities for Acute ACJ Separation: Protocol for a Systematic Review and Meta-Analysis. Int. J. Surg. Protoc. 2022, 26, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Malahias, M.-A.; Sarlikiotis, T.; Brilakis, E.; Gerogiannis, D.; Avramidis, G.; Antonogiannakis, E. The Clinical Outcome of the ‘Surgilig’ Technique for the Reconstruction of Acromioclavicular Dislocations: A Systematic Review. J. Orthop. 2020, 18, 126–131. [Google Scholar] [CrossRef]
- Kocsis, G.; McCulloch, T.; Thyagarajan, D.; Wallace, W.A. The Biological Response to a Failed Extra-Articular Polyester Ligament Used for AC Joint Reconstruction at the Shoulder Girdle—A Retrieval Analysis of Five Cases. Bone Jt. J. 2015, 97-B, 83–88. [Google Scholar] [CrossRef]
- Narang, A.; Abdelwahab, A.; Raj, N.; Cottam, H.; Tolat, A.; Singh, B. Acromioclavicular Joint Stabilization: Our Experience with the Lockdown Technique. J. Orthop. 2023, 44, 53–56. [Google Scholar] [CrossRef]
- Agha, R.A.; Sohrabi, C.; Mathew, G.; Franchi, T.; Kerwan, A.; O’Neill, N. The Process 2020 Guideline: Updating Consensus Preferred Reporting of Case Series in Surgery (Process) Guidelines. Int. J. Surg. 2020, 84, 231–235. [Google Scholar] [CrossRef]
- Lindborg, C.M.; Smith, R.D.; Reihl, A.M.; Bacevich, B.M.; Cote, M.; O’Donnell, E.; Mazzocca, A.D.; Hutchinson, I. Current Concepts in Management of Acromioclavicular Joint Injury. J. Clin. Med. 2024, 13, 1413. [Google Scholar] [CrossRef]
- Jeon, I.H.; Dewnany, G.; Hartley, R.; Neumann, L.; Wallace, W.A. Chronic Acromioclavicular Separation: The Medium Term Results of Coracoclavicular Ligament Reconstruction Using Braided Polyester Prosthetic Ligament. Injury 2007, 38, 1247–1253. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The Prisma 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, Ed000142. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological Quality of Case Series Studies: An Introduction to the Jbi Critical Appraisal Tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef] [PubMed]
- Cochrane, Cochrane Bias Methods Group. Robins-I V2 Tool. 2024. Available online: https://www.riskofbias.info/welcome/robins-i-v2 (accessed on 24 April 2025).
- Xu, S.; Chen, J.Y.; Lie, H.M.E.; Hao, Y.; Lie, D.T.T. Minimal Clinically Important Difference of Oxford, Constant, and Ucla Shoulder Score for Arthroscopic Rotator Cuff Repair. J. Orthop. 2020, 19, 21–27. [Google Scholar] [CrossRef]
- Dabija, D.I.; Jain, N.B. Minimal Clinically Important Difference of Shoulder Outcome Measures and Diagnoses: A Systematic Review. Am. J. Phys. Med. Rehabil. 2019, 98, 671–676. [Google Scholar] [CrossRef]
- Franchignoni, F.; Vercelli, S.; Giordano, A.; Sartorio, F.; Bravini, E.; Ferriero, G. Minimal Clinically Important Difference of the Disabilities of the Arm, Shoulder and Hand Outcome Measure (Dash) and Its Shortened Version (Quickdash). J. Orthop. Sports Phys. Ther. 2014, 44, 30–39. [Google Scholar] [CrossRef]
- Tashjian, R.Z.; Shin, J.; Broschinsky, K.; Yeh, C.C.; Martin, B.; Chalmers, P.N.; Greis, P.E.; Burks, R.T.; Zhang, Y. Minimal Clinically Important Differences in the American Shoulder and Elbow Surgeons, Simple Shoulder Test, and Visual Analog Scale Pain Scores After Arthroscopic Rotator Cuff Repair. J. Shoulder Elb. Surg. 2020, 29, 1406–1411. [Google Scholar] [CrossRef]
- Dearden, P.M.C.; Ferran, N.A.; Morris, E.W. Distal Clavicle Osteolysis Following Fixation with a Synthetic Ligament. Int. J. Shoulder Surg. 2011, 5, 101–104. [Google Scholar]
- Platts, C.T.; Chatterjee, A.D.; Tambe, A.A. An Uncommon Complication Following Synthetic Ligament Reconstruction of the Acromioclavicular Joint. Int. J. Shoulder Surg. 2013, 7, 124–125. [Google Scholar] [CrossRef] [PubMed]
- Sarda, P.; Richards, A.M.; Corbett, S.A. Bone Osteolysis Following Acromioclavicular Joint Reconstruction Using Synthetic Ligament (Surgilig™). Shoulder Elb. 2014, 6, 40–43. [Google Scholar] [CrossRef]
- Walters, J.D.; Ignozzi, A.; Bustos, F.; Werner, B.C.; Brockmeier, S.F. Better Radiographic Reduction and Lower Complication Rates with Combined Coracoclavicular and Acromioclavicular Ligament Reconstruction Than with Isolated Coracoclavicular Reconstruction. Arthrosc. Sports Med. Rehabil. 2021, 3, e441–e448. [Google Scholar] [CrossRef]
- Younis, F.; Ajwani, S.; Bibi, A.; Riley, E.; Hughes, P.J. Operative Versus Non-Operative Treatment of Grade Iii Acromioclavicular Joint Dislocations and the Use of Surgilig: A Retrospective Review. Ortop. Traumatol. Rehabil. 2017, 19, 523–530. [Google Scholar] [CrossRef]
- Bhattacharya, R.; Goodchild, L.; Rangan, A. Acromioclavicular Joint Reconstruction Using the Nottingham Surgilig: A Preliminary Report. Acta Orthop. Belg. 2008, 74, 167–172. [Google Scholar]
- Çetinkaya, E.; Gül, M.; Özcafer, R.; Yavuz, U.; Lapçin, O.; Özkan, B.; Kabukcuoglu, Y. Treatment of Acromioclavicular Joint Dislocations by Using Synthetic Polyester Ligament. Bakirkoy Tip. Derg./Med. J. Bakirkoy 2018, 14, 183–189. [Google Scholar] [CrossRef]
- Kumar, V.; Garg, S.; Elzein, I.; Lawrence, T.; Manning, P.; Wallace, W.A. Modified Weaver-Dunn Procedure Versus the Use of a Synthetic Ligament for Acromioclavicular Joint Reconstruction. J. Orthop. Surg. 2014, 22, 199–203. [Google Scholar] [CrossRef]
- Saraglis, G.; Chaudhari, H.; Sanjani, S.R.; Khan, A. Early Loss of Radiographic Reduction After Acute Acromioclavicular Joint Reconstruction: Comparison of Open Double Endobutton Fixation vs. Nottingham Surgilig. Sicot-J. 2022, 8, 46. [Google Scholar] [CrossRef]
- Wood, T.A.; Rosell, P.A.; Clasper, J.C. Preliminary Results of the ‘Surgilig’ Synthetic Ligament in the Management of Chronic Acromioclavicular Joint Disruption. J. R. Army Med. Corps 2009, 155, 191–193. [Google Scholar] [CrossRef]
- Wright, J.; Osarumwense, D.; Ismail, F.; Umebuani, Y.; Orakwe, S. Stabilisation for the Disrupted Acromioclavicular Joint Using a Braided Polyester Prosthetic Ligament. J. Orthop. Surg. 2015, 23, 223–228. [Google Scholar] [CrossRef]
- Saraglis, G.; Prinja, A.; To, K.; Khan, W.; Singh, J. Surgical Treatments for Acute Unstable Acromioclavicular Joint Dislocations. Sicot-J. 2022, 8, 38. [Google Scholar] [CrossRef]
- Sethi, G.K.; Scott, S.M. Subclavian Artery Laceration Due to Migration of a Hagie Pin. Surgery 1976, 80, 644–646. [Google Scholar]
- Tiefenboeck, T.M.; Popp, D.; Boesmueller, S.; Payr, S.; Joestl, J.; Komjati, M.; Binder, H.; Schurz, M.; Ostermann, R.C. Acromioclavicular Joint Dislocation Treated with Bosworth Screw and Additional K-Wiring: Results After 7.8 Years-Still an Adequate Procedure? BMC Musculoskelet. Disord. 2017, 18, 339. [Google Scholar] [CrossRef]
- Faraj, A.A.; Ketzer, B. The Use of a Hook-Plate in the Management of Acromioclavicular Injuries. Report of Ten Cases. Acta Orthop. Belg. 2001, 67, 448–451. [Google Scholar]
- Gumustas, S.A.; Saglam, F.; Komur, B.; Batmaz, A.G.; Yukunc, I.; Tosun, H.B.; Bekler, H.I. Surgical Treatment of type III Acromioclavicular Dislocation: Bosworth Technique Versus Hook Plating. North. Clin. Istanb. 2018, 5, 334–340. [Google Scholar]
- Lee, S.J.; Eom, T.W.; Hyun, Y.S. Complications and Frequency of Surgical Treatment with Ao-Type Hook Plate in Shoulder Trauma: A Retrospective Study. J. Clin. Med. 2022, 11, 1026. [Google Scholar] [CrossRef]
- Moatshe, G.; Kruckeberg, B.M.; Chahla, J.; Godin, J.A.; Cinque, M.E.; Provencher, M.T.; LaPrade, R.F. Acromioclavicular and Coracoclavicular Ligament Reconstruction for Acromioclavicular Joint Instability: A Systematic Review of Clinical and Radiographic Outcomes. Arthroscopy 2018, 34, 1979–1995.e8. [Google Scholar] [CrossRef]
- Verstift, D.E.; Somford, M.P.; van Deurzen, D.F.P.; van den Bekerom, M.P.J. Review of Weaver and Dunn on Treatment of Acromioclavicular Injuries, Especially Complete Acromioclavicular Separation. J. ISAKOS 2021, 6, 116–119. [Google Scholar] [CrossRef]
- Gupta, R.; Sood, M.; Malhotra, A.; Masih, G.D.; Khanna, T.; Raghav, M. Functional Outcome of Modified Weaver Dunn Technique for Acromioclavicular Joint Dislocation. Indian J. Orthop. 2018, 52, 418–422. [Google Scholar] [CrossRef]
- Kukkonen, J.; Kauko, T.; Vahlberg, T.; Joukainen, A.; Aärimaa, V. Investigating Minimal Clinically Important Difference for Constant Score in Patients Undergoing Rotator Cuff Surgery. J. Shoulder Elb. Surg. 2013, 22, 1650–1655. [Google Scholar] [CrossRef]
- Sircana, G.; Saccomanno, M.F.; Mocini, F.; Campana, V.; Messinese, P.; Monteleone, A.; Salvi, A.; Scaini, A.; Megaro, A.; Milano, G. Anatomic Reconstruction of the Acromioclavicular Joint Provides the Best Functional Outcomes in the Treatment of Chronic Instability. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2021, 29, 2237–2248. [Google Scholar] [CrossRef] [PubMed]
- Borbas, P.; Churchill, J.; Ek, E.T. Surgical Management of Chronic High-Grade Acromioclavicular Joint Dislocations: A Systematic Review. J. Shoulder Elb. Surg. 2019, 28, 2031–2038. [Google Scholar] [CrossRef] [PubMed]
- Berthold, D.P.; Muench, L.N.; Beitzel, K.; Archambault, S.; Jerliu, A.; Cote, M.P.; Scheiderer, B.; Imhoff, A.B.; Arciero, R.A.; Mazzocca, A.D. Minimum 10-Year Outcomes After Revision Anatomic Coracoclavicular Ligament Reconstruction for Acromioclavicular Joint Instability. Orthop. J. Sports Med. 2020, 8, 2325967120947033. [Google Scholar] [CrossRef]
- Gowd, A.K.; Liu, J.N.; Cabarcas, B.C.; Cvetanovich, G.L.; Garcia, G.H.; Manderle, B.J.; Verma, N.N. Current Concepts in the Operative Management of Acromioclavicular Dislocations: A Systematic Review and Meta-Analysis of Operative Techniques. Am. J. Sports Med. 2019, 47, 2745–2758. [Google Scholar] [CrossRef] [PubMed]
- Martetschläger, F.; Horan, M.P.; Warth, R.J.; Millett, P.J. Complications After Anatomic Fixation and Reconstruction of the Coracoclavicular Ligaments. Am. J. Sports Med. 2013, 41, 2896–2903. [Google Scholar] [CrossRef]
- Ma, R.; Smith, P.A.; Smith, M.J.; Sherman, S.L.; Flood, D.; Li, X. Managing and Recognizing Complications After Treatment of Acromioclavicular Joint Repair or Reconstruction. Curr. Rev. Musculoskelet. Med. 2015, 8, 75–82. [Google Scholar] [CrossRef]
- Sinagra, Z.P.; Kop, A.; Pabbruwe, M.; Parry, J.; Clark, G. Foreign Body Reaction Associated with Artificial Lars Ligaments: A Retrieval Study. Orthop. J. Sports Med. 2018, 6, 2325967118811604. [Google Scholar] [CrossRef]
- Boström Windhamre, H.; von Heideken, J.; Une-Larsson, V.; Ekström, W.; Ekelund, A. No Difference in Clinical Outcome at 2-Year Follow-Up in Patients with type III and V Acromioclavicular Joint Dislocation Treated with Hook Plate or Physiotherapy: A Randomized Controlled Trial. J. Shoulder Elb. Surg. 2022, 31, 1122–1136. [Google Scholar] [CrossRef] [PubMed]
- Canadian Orthopaedic Trauma Society. Multicenter Randomized Clinical Trial of Nonoperative Versus Operative Treatment of Acute Acromio-Clavicular Joint Dislocation. J. Orthop. Trauma 2015, 29, 479–487. [Google Scholar] [CrossRef]
- Murray, I.R.; Robinson, P.G.; Goudie, E.B.; Duckworth, A.D.; Clark, K.; Robinson, C.M. Open Reduction and Tunneled Suspensory Device Fixation Compared with Nonoperative Treatment for Type-III and Type-IV Acromioclavicular Joint Dislocations: The Acorn Prospective, Randomized Controlled Trial. J. Bone Jt. surgery. Am. Vol. 2018, 100, 1912–1918. [Google Scholar] [CrossRef]
- Tauber, M.; Hoffelner, T.; Lehmann, L.; Kraus, N.; Scheibel, M.; Moroder, P. Prospective Multicenter Randomized Controlled Trial of Surgical Versus Nonsurgical Treatment for Acute Rockwood Type 3 Acromioclavicular Injury. Orthop. J. Sports Med. 2023, 11, 23259671231190411. [Google Scholar] [CrossRef] [PubMed]
- Hegyi, P.; Erőss, B.; Izbéki, F.; Párniczky, A.; Szentesi, A. Accelerating the Translational Medicine Cycle: The Academia Europaea Pilot. Nat. Med. 2021, 27, 1317–1319. [Google Scholar] [CrossRef] [PubMed]
- Hegyi, P.; Petersen, O.H.; Holgate, S.; Erőss, B.; Garami, A.; Szakács, Z.; Dobszai, D.; Balaskó, M.; Kemény, L.; Peng, S.; et al. Academia Europaea Position Paper on Translational Medicine: The Cycle Model for Translating Scientific Results into Community Benefits. J. Clin. Med. 2020, 9, 1532. [Google Scholar] [CrossRef] [PubMed]

| Basic Characteristics | All Patient | Time | Surgery | |||
|---|---|---|---|---|---|---|
| Acute <3 Weeks | Chronic >3 Weeks | Primary (Non-Previously Operated) | Non-Primary Operation (Revision) | |||
| No. of patients | 39 | 27 | 12 | 32 | 7 | |
| Primary/Revision | 32/7 | 25/2 | 7/5 | - | - | |
| Acute/chronic | - | - | 25/7 | 2/5 | ||
| Gender (M/F) | 36/3 | 25/2 | 11/1 | 29/3 | 7/0 | |
| Mean age at op. (years) | 38.90 ± 12.68 | 35.52 ± 9.46 | 46.5 ± 15.2 | 36.69 ± 12.08 | 36.91 ± 14.33 | |
| Mean time of interval (injury—op) (weeks) | 26.69 ± 84.36 | 1.07 ± 0.65 | 84.33 ± 139.11 | 25.44 ± 87.90 | 23.62 ± 87.86 | |
| Mean time to return to work | 7.73 ± 9.95 | 6.87 ± 10.49 | 9.66 ± 8.73 | 8.57 ± 11.68 | 8.84 ± 11.73 | |
| Follow-up (months) | 24.51 ± 10.12 | 23.18 ± 8.98 | 27.53 ± 12.19 | 23.84 ± 10.45 | 22.76 ± 9.72 | |
| Rockwood classification: | ||||||
| III | 21 (54%) | 15 (55%) | 6 (50%) | 18 (56%) | 3 (43%) | |
| IV | 6 (15%) | 4 (15%) | 2 (17%) | 5 (16%) | 1 (14%) | |
| V | 12 (31%) | 8 (30%) | 4 (23%) | 9 (28%) | 3 (43%) | |
| Acute | Chronic | Difference | p Value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Acute | Chronic | (diff. Acute -diff.chr) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| OSS | 12.93 | ±7.14 | 44.56 | ±9.08 | 29.11 | ±12.60 | 45.83 | ±2.29 | −31.63 | ±9.62 | −16.67 | ±12.42 | 0.0017 |
| IMITANI | 26.11 | ±16.78 | 91.67 | ±19.22 | 52.08 | ±30.41 | 91.67 | ±9.13 | −65.56 | ±22.12 | −39.58 | ±27.26 | 0.0096 |
| CONSTANT | 18.22 | ±15.37 | 91.11 | ±17.33 | 47.83 | ±25.66 | 88.17 | ±9.53 | −72.89 | ±22.07 | −40.33 | ±26.96 | 0.0017 |
| UCLA | 8.52 | ±4.85 | 32.59 | ±6.20 | 17.00 | ±6.86 | 32.58 | ±3.63 | −24.07 | ±7.78 | −15.58 | ±8.27 | 0.0069 |
| DASH | 73.64 | ±16.35 | 7.65 | ±17.41 | 41.90 | ±21.55 | 6.97 | ±8.69 | 65.98 | ±20.24 | 34.93 | ±22.85 | 0.0004 |
| SST (%) | 6.47 | ±17.51 | 88.59 | ±19.65 | 34.74 | ±27.72 | 86.12 | ±10.26 | −82.12 | ±25.91 | −51.38 | ±32.54 | 0.0099 |
| ASES | 26.63 | ±15.07 | 90.44 | ±20.09 | 52.08 | ±26.12 | 93.25 | ±6.55 | −63.81 | ±20.83 | −41.17 | ±25.67 | 0.0151 |
| NRS (1–10) | 6.78 | ±1.76 | 0.85 | ±2.38 | 4.58 | ±2.81 | 0.92 | ±0.94 | 5.93 | ±2.34 | 3.66 | ±2.42 | 0.0131 |
| No. of Group | Patient ID | Previous Surgery | Proud Metalwork | Implant Loosening | Discharge | Trauma | Reoperation | Reason of Reoperation | Time Until Reoperation (Days) | Lockdown Implant Extracted | Result of Bacteriogram | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acute | 27 | 1 | 2 | 1 | 4 | 3 | 5 | 525.6 ± 613.48 | 4 | |||
| H1 | 1 | 0 | 0 | 1 | 0 | 1 | discharge | 18 | 1 | S. aureus | ||
| H7 | 0 | 0 | 1 | 1 | 1 | 1 | trauma | 1045 | 1 | 0 | ||
| H8 | 0 | 0 | 0 | 1 | 0 | 1 | discharge | 58 | 0 | 0 | ||
| H27 | 0 | 0 | 0 | 0 | 1 | 1 | trauma | 1326 | 1 | 0 | ||
| P4 | 0 | 0 | 0 | 1 | 1 | 1 | trauma | 181 | 1 | S. aureus | ||
| H13 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| H22 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Chronic | 12 | 1 | 1 | 1 | 3 | 1 | 3 | 141.33 ± 216.23 | 2 | |||
| O3 | 0 | 0 | 1 | 1 | 0 | 1 | discharge | 19 | 1 | C. acnes | ||
| O4 | 1 | 0 | 0 | 1 | 1 | 1 | trauma | 391 | 1 | 0 | ||
| P5 | 0 | 0 | 0 | 1 | 0 | 1 | discharge | 14 | 1 | S. aureus | ||
| O2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Year of Publication | Origin of Authors | No. of Cases | Study Design | Male | Female | Mean Age (Year) | Rockwood Classification | Mean Interval (Months) | Mean Follow Up (Months) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Narang et al. [10] | 2023 | UK | 42 | RCS | 39 | 3 | 42.2 | 8:III; 4:IV; 30:V; | 71.1 | 68 |
| Jeon et al. [13] | 2007 | South Korea | 11 | RCS | 11 | 0 | 39 | 9:III; 1: IV; 1:V; | 18 | 55 |
| Bhattacharya et al. [27] | 2008 | UK | 11 | PCS | 10 | 1 | 35.1 | >III | 21 | 24 |
| Wood et al. [31] | 2009 | UK | 10 | RCS | NA | NA | NA | >III | NA | 6 |
| Carlos et al. [5] | 2011 | UK | 45 | PCS | 32 | 13 | 37.6 | >III | 7.2 | 26.9 |
| Cetinkaya et al. [28] | 2018 | Turkey | 16 | RCS | 16 | 0 | 38.5 | >III | NA | 20 |
| Kumar et al. [29] | 2014 | UK | 24 | RCS | NA | NA | 42 | 13:III; 4:IV; 7:V; | 39 | 30 |
| Saraglis et al. [30] | 2022 | UK | 25 | RCS | 22 | 3 | 36 | IV: 19; V:6 | NA | NA |
| Wright et al. [32] | 2015 | UK | 21 | RCS | 21 | 0 | 43 | 12:III; 1:IV; 8:V; | 6.80 | 30 |
| No. of patients | 205 | |||||||||
| No. of studies | 9 |
| Oxford | ASES | Nottingham | Imitani | Constant | |
| Preop. | 2 | 0 | 1 | 0 | 0 |
| Postop. | 5 | 0 | 1 | 2 | 5 |
| UCLA | Simple | Pain (NRS) | Deformity | Complications | |
| Preop. | 0 | 0 | 2 | 1 | |
| Postop. | 1 | 1 | 4 | 0 | 8 |
| Article | Number of Patients | Implant Loosening, Osteolysis | Subluxation | Other (Stiffness, Graft Rupture, Subacromial Impingement) | Proud/Prominence Metalwork | Superficial Infection, Discharge | Trauma | Previous Surgery | # of Reoperation | Reoperation Due to Non Re-Injury | Reasons for Reop | Previous Surgery | Time Until Reoperation (Months) | Lockdown Implant Extracted | Result of Bacteriogram |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Narang et al. [10] | 42 | 0 | 8 (X-ray) | 3 (stiffness) | 5 (proud) | 1 | 0 | 0 | 2 | 2 | Proud metal. | NA | NA | 2 | NA |
| Jeon et al. [13] | 11 | 1 (loosening) | 11 (X-ray) | 2 (sub) | 0 | 0 | 1 | 3 (Weaver Dunn) | 2 | 2 | Subacr. Burs. | 0 | 6–10 | 1 | NA |
| Bhattacharya et al. [27] | 11 | 4 (lysis) | 0 | 1 (graft) | 4 (prom.) | 0 | NA | 0 | 1 | 1 | Graft rupture | 0 | 6 | 1 | NA |
| Wood et al. [31] | 10 | 0 | 0 | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Carlos et al. [5] | 45 | 1 (loosenin)g | 13 migration = sublux (X-ray) | 0 | 6 (skin irritation) | NA | 0 | NA | 7 | 7 | 6 inf., 1 loosening | NA | 9 | 6 | 0 |
| Cetinkaya et al. [28] | 16 | 1 (lysis) | 1 (X-ray) | 0 | 0 | 0 | 0 | 1 (K-wire) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Kumar et al. [29] | 24 | 0 | 0 | 0 | 0 | 4 | 1 | NA | 1 | 0 | 0 | 0 | NA | 0 | 0 |
| Saraglis et al. [30] | 25 | 1 (osteolysis) | 0 | 0 | 0 | 3 | 0 | 0 | 1 | 1 | infection | 0 | NA | 1 | 0 |
| Wright et al. [32] | 21 | 0 | 0 | 1 (subacrom. imp.) | 0 | 0 | 1 | NA | 1 | 1 | Subacr. Burs. | 0 | NA | 0 | 0 |
| 205 | 8 | 33 | 7 | 15 | 8 | 3 | 4 | 15 | 14 | 6–10 | 11 | 0 | |||
| 100% | 3.9% | 16.1% | 3.4% | 7.3% | 3.9% | 1.5% | 2.0% | 7.3% | 6.8% | 5% |
| Complication Differences | ||||
|---|---|---|---|---|
| Our Results | Sys Search | |||
| No. of patients | 39 | 205 | ||
| No. of complications (without trauma) | 12 | 30.8% | 71 | 34.6% |
| Time interval (from injury to surgery, weeks) | 26.69 ± 84.36 (0.5–510) | 108.72 ± 98.04 (27.2–284.4) | ||
| Stiffness, subacromial imp, graft failure | 0 | 0.0% | 7 | 3.4% |
| Subluxation | 0 | 0.0% | 33 | 16.1% |
| Proud metalwork, graft rupture, bursitis, stiffness | 3 | 7.7% | 15 | 7.3% |
| Implant loose | 2 | 5.1% | 8 | 3.9% |
| Spf. infection | 7 | 17.9% | 8 | 3.9% |
| Re-injury | 4 | 10.3% | 3 | 1.5% |
| Previous surgery | 7 | 17.9% | 4 | 2.0% |
| Re-op. | 8 | 20.5% | 15 | 7.3% |
| Implant remove | 6 | 15.4% | 11 | 5.4% |
| Implant failure | 2 | 5.1% | 11 | 5.4% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovacs, K.; Váncsa, S.; Abonyi-Tóth, Z.; Hegyi, P.; Soos, G.; Rabai, K.; Bogosi, T.; Kocsis, G. Acromioclavicular Reconstruction Using the Lockdown Technique: A Case Series and Systematic Review. J. Clin. Med. 2025, 14, 4046. https://doi.org/10.3390/jcm14124046
Kovacs K, Váncsa S, Abonyi-Tóth Z, Hegyi P, Soos G, Rabai K, Bogosi T, Kocsis G. Acromioclavicular Reconstruction Using the Lockdown Technique: A Case Series and Systematic Review. Journal of Clinical Medicine. 2025; 14(12):4046. https://doi.org/10.3390/jcm14124046
Chicago/Turabian StyleKovacs, Krisztian, Szilárd Váncsa, Zsolt Abonyi-Tóth, Peter Hegyi, Gergely Soos, Kalman Rabai, Tibor Bogosi, and Gyorgy Kocsis. 2025. "Acromioclavicular Reconstruction Using the Lockdown Technique: A Case Series and Systematic Review" Journal of Clinical Medicine 14, no. 12: 4046. https://doi.org/10.3390/jcm14124046
APA StyleKovacs, K., Váncsa, S., Abonyi-Tóth, Z., Hegyi, P., Soos, G., Rabai, K., Bogosi, T., & Kocsis, G. (2025). Acromioclavicular Reconstruction Using the Lockdown Technique: A Case Series and Systematic Review. Journal of Clinical Medicine, 14(12), 4046. https://doi.org/10.3390/jcm14124046








