Comparison of Surgical Outcomes Between Single-Site Laparoscopic Adenomyomectomy and Fundusectomy: Experience from a Single Center
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Data Items and Outcomes
2.3. Patient Characteristics
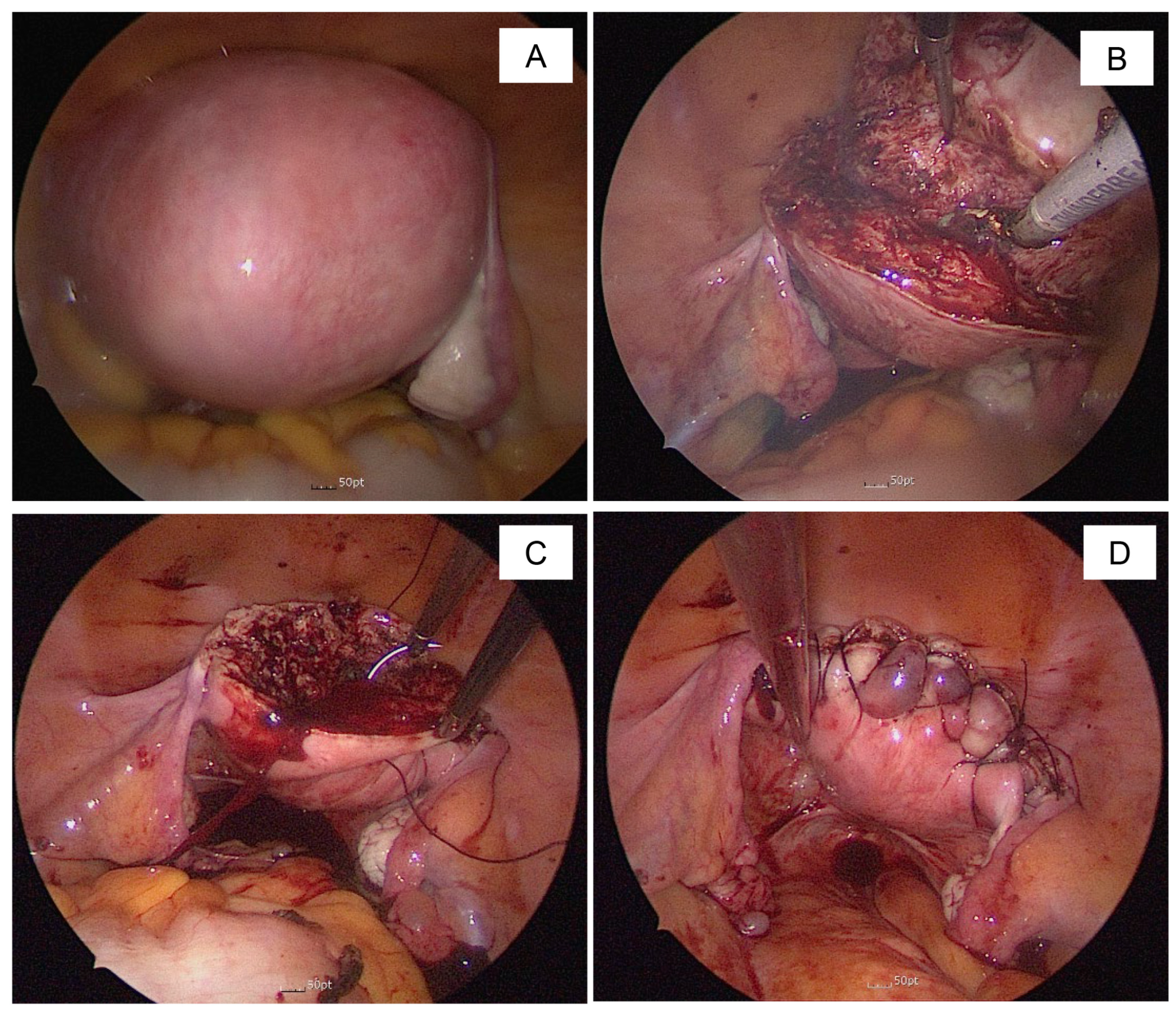
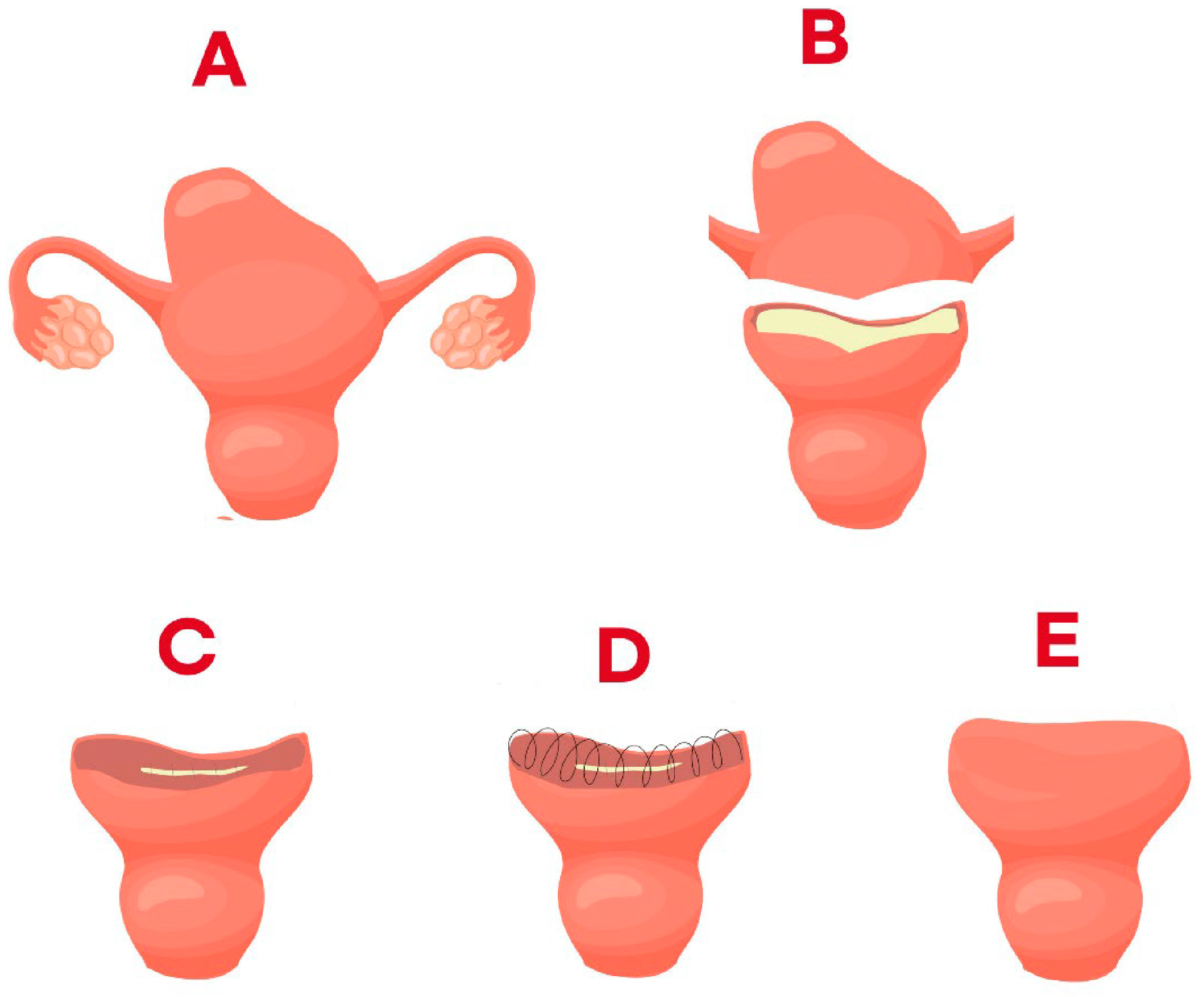
2.4. Surgical Method
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OC | Oral contraceptives |
| LNG-IUS | Levonorgestrel releasing intrauterine system |
| UAE | Uterine artery embolization |
| D&C | Dilatation and curettage |
| CS | Cesarean section |
| HIFU | High-intensity focused ultrasound |
| NSAID | Non-steroidal anti-inflammatory drug |
References
- Jiang, L.; Han, Y.; Song, Z.; Li, Y. Pregnancy Outcomes after Uterus-sparing Operative Treatment for Adenomyosis: A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2023, 30, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Chen, S.; Che, X.; Xu, P.; Huang, X.; Zhang, X. Comparisons of the efficacy and recurrence of adenomyomectomy for severe uterine diffuse adenomyosis via laparotomy versus laparoscopy: A long-term result in a single institution. J. Pain. Res. 2019, 12, 1917–1924. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.H.; Liu, W.M.; Fuh, J.L.; Cheng, M.H.; Chao, H.T. Comparison of surgery alone and combined surgical-medical treatment in the management of symptomatic uterine adenomyoma. Fertil. Steril. 2009, 92, 876–885. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Liu, G.; Liu, C.; Zhang, Z. Recurrence-associated factors of laparoscopic adenomyomectomy for severely symptomatic adenomyoma. Oncol. Lett. 2018, 16, 3430–3438. [Google Scholar] [CrossRef] [PubMed]
- Wilson, L.; Pandeya, N.; Byles, J.; Mishra, G. Hysterectomy and incidence of depressive symptoms in midlife women: The Australian Longitudinal Study on Women’s Health. Epidemiol. Psychiatr. Sci. 2018, 27, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhang, X.; Fan, Y.; Zhang, J.; Chen, B.; Sun, X.; Zhao, X. Correlation analysis of hysterectomy and ovarian preservation with depression. Sci. Rep. 2023, 13, 9744. [Google Scholar] [CrossRef] [PubMed]
- Saremi, A.; Bahrami, H.; Feizy, F. Uterine Fundectomy in Patients With Benign Etiology Undergoing Hysterectomy: New Surgical Technique. JMIR Res. Protoc. 2017, 6, e150. [Google Scholar] [CrossRef] [PubMed]
- Capezzuoli, T.; Toscano, F.; Ceccaroni, M.; Roviglione, G.; Stepniewska, A.; Fambrini, M.; Vannuccini, S.; Petraglia, F. Conservative surgical treatment for adenomyosis: New options for looking beyond uterus removal. Best. Pract. Res. Clin. Obstet. Gynaecol. 2024, 95, 102507. [Google Scholar] [CrossRef] [PubMed]
- Pelage, J.P.; Jacob, D.; Fazel, A.; Namur, J.; Laurent, A.; Rymer, R.; Dref, O.L. Midterm results of uterine artery embolization for symptomatic adenomyosis: Initial experience. Radiology 2005, 234, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Hai, N.; Hou, Q.; Guo, R. Ultrasound-guided transvaginal radiofrequency ablation combined with levonorgestrel-releasing intrauterine system for symptomatic uterine adenomyosis treatment. Int. J. Hyperth. 2021, 38, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Liang, E.; Brown, B.; Rachinsky, M. A clinical audit on the efficacy and safety of uterine artery embolisation for symptomatic adenomyosis: Results in 117 women. Aust. N. Z. J. Obstet. Gynaecol. 2018, 58, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Hong, G.Y.; Lee, K.H.; Song, J.H.; Kim, T.E. Safety and efficacy of ultrasound-guided high-intensity focused ultrasound treatment for uterine fibroids and adenomyosis. Ultrasound Med. Biol. 2019, 45, 3214–3221. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhu, X.; He, S.; Jiang, Z.; Li, H.; Tian, X.; Long, W.; Xue, M.; Deng, X.; Ye, M. High-intensity focused ultrasound in the management of adenomyosis: Long-term results from a single center. Int. J. Hyperthermia. 2021, 38, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Fortin, C.; Hur, C.; Falcone, T. Impact of Laparoscopic Hysterectomy on Quality of Life. J. Minim. Invasive Gynecol. 2019, 26, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Tian, H.; Lin, D.; Zhao, L.; Wang, H.; Hao, Y. Risk of Recurrence and Reintervention After Uterine-Sparing Interventions for Symptomatic Adenomyosis: A Systematic Review and Meta-Analysis. Obstet. Gynecol. 2023, 141, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Tellum, T.; Omtvedt, M.; Naftalin, J.; Hirsch, M.; Jurkovic, D. A systematic review of outcome reporting and outcome measures in studies investigating uterine-sparing treatment for adenomyosis. Hum. Reprod. Open 2021, 2021, hoab030. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.T.; Seow, K.M.; Wang, P.H. Adenomyomectomy: A complicated surgery. Taiwan. J. Obstet. Gynecol. 2022, 61, 407–408. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.; Jin, L.; Zheng, S.; Shao, M.; Cui, D.; Hu, M. Laparoscopically assisted Adenomyomectomy Using the Double/Multiple-Flap Method with Temporary Occlusion of the Bilateral Uterine Artery and Utero-Ovarian Vessels in Comparison with the Double/Multiple-Flap Only Method. Geburtshilfe Frauenheilkd. 2021, 81, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Shin, C.S.; Ko, Y.B.; Nam, S.Y.; Yim, H.S.; Lee, K.H. Laparoscopic assisted adenomyomectomy using double flap method. Obstet. Gynecol. Sci. 2014, 57, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Saremi, A.; Bahrami, H.; Salehian, P.; Hakak, N.; Pooladi, A. Treatment of adenomyomectomy in women with severe uterine adenomyosis using a novel technique. Reprod. Biomed. Online 2014, 28, 753–760. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Mean ± SD No of Patients (%) |
|---|---|
| Age (years) | 42.82 ± 5.84 |
| BMI (kg/m2) | 22.98 ± 3.53 |
| Previous abdominal operative history | 97 (36.6%) |
| Number of previous abdominal operative history | 0.53 ± 0.80 |
| Previous operation type | |
| CS | 22 (8.3%) |
| Twice or more CS | 29 (10.9%) |
| Myomectomy | 15 (5.7%) |
| Adnexa operation | 22 (8.3%) |
| Appendectomy | 4 (1.5%) |
| Diagnostic laparoscopy | 0 |
| Cholecystectomy | 4 (1.5%) |
| Other abdominal surgery | 1 (0.4%) |
| Preoperative longitudinal length of uterus (cm) | 10.17 ± 7.33 |
| Volume of uterus (gm) | 300.19 ± 175.85 |
| CA125 (U/mL) | 92.00 ± 128.82 |
| Combined endometriosis | 63 (23.8%) |
| Operative indication | |
| Menorrhagia | 114 (43.0%) |
| Dysmenorrhea | 94 (35.5%) |
| Enlarged size | 9 (3.4%) |
| Pelvic pain | 17 (6.4%) |
| Urinary frequency | 9 (3.4%) |
| Combined ovarian mass | 3 (1.1%) |
| Palpable abdominal huge mass | 1 (0.4%) |
| Combined myoma | 17 (6.4%) |
| Clinical Outcome | Mean ± SD, No. of Patients (%) | ||
|---|---|---|---|
| Fundusectomy | Adenomyomectomy | p-Value | |
| Number of patients | 141 | 124 | |
| Age (years) | 45.06 ± 4.60 | 40.27 ± 6.07 | 0.00 |
| 20–29 | 0 | 8 (6.5%) | |
| 30–39 | 18 (12.8%) | 44 (35.5%) | |
| 40–49 | 101 (71.6%) | 69 (55.6%) | |
| >50 | 22 (15.6%) | 3 (2.4%) | |
| Preoperative longitudinal length of uterus (cm) | 10.04 ± 1.90 | 10.32 ± 10.56 | 0.76 |
| Preoperative weight of uterus (gm) | 332.55 ± 193.97 | 263.09 ± 144.53 | 0.00 |
| Previous abdominal operative history | 57(40.4%) | 40(32.3%) | 0.20 |
| Number of previous abdominal operative history | 0.58 ± 0.85 | 0.47 ± 0.74 | 0.25 |
| Previous operation type | |||
| CS | 2 (5.7%) | 9 (3.9%) | |
| Twice CS | 2 (5.7%) | 2 (0.9%) | |
| Myomectomy | 7 (20.0%) | 10 (4.4%) | |
| Adnexa operation | 2 (5.7%) | 7 (3.1%) | |
| Appendectomy | 0 | 7 (3.1%) | |
| Diagnostic laparoscopy | 7 (3.1%) | ||
| Cholecystectomy | 1 (2.9%) | 2 (0.9%) | |
| Other abdominal surgery | 1 (2.9%) | 1 (0.4%) | |
| Combined with myoma | 6 (4.3%) | 11 (8.9%) | |
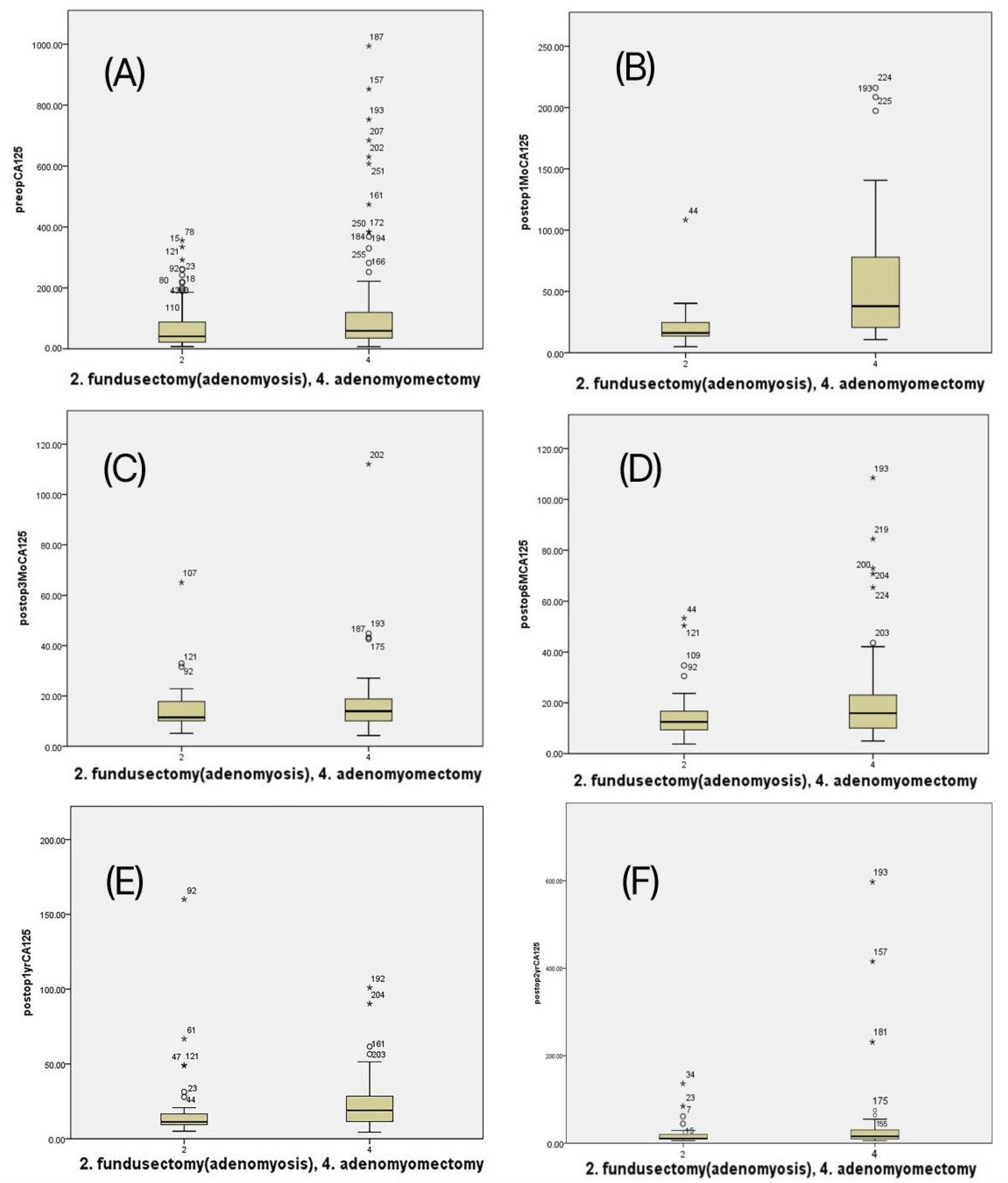
| Preoperative CA125 (U/mL) | 68.37 ± 70.26 | 119.55 ± 170.03 | 0.00 |
| Combined with predicted endometriosis | 22 (15.6%) | 41 (33.1%) | 0.00 |
| Clinical Outcome | Mean ± SD, No. of Patients (%) | ||
|---|---|---|---|
| Fundusectomy | Adenomyomectomy | p-Value | |
| Largest size of resected adenomyosis (cm) | 5.90 ± 1.94 | 5.46 ± 1.78 | 0.05 |
| Weight of resected adenomyosis (gm) | 275.73 ± 173.56 | 94.34 ± 94.14 | 0.00 |
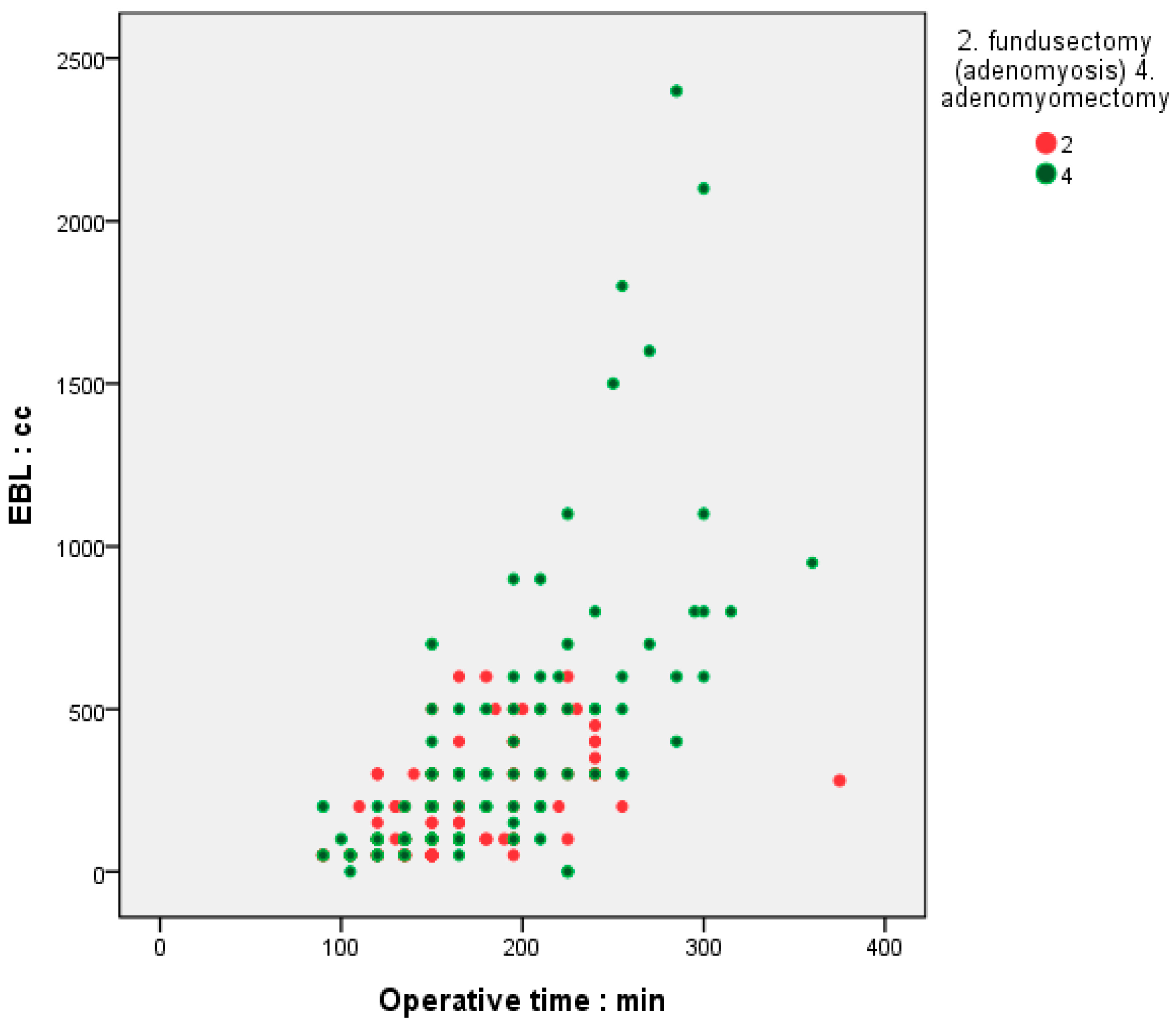
| Operation time (min) | 158.19 ± 42.93 | 179.11 ± 56.95 | 0.00 |
| Estimated blood loss (mL) | 175.04 ± 142.76 | 347.97 ± 409.78 | 0.00 |
| Change in hemoglobin (g/dL) | 1.46 ± 0.81 | 1.79 ± 1.29 | 0.13 |
| Change in hematocrit (%) | 4.77 ± 2.74 | 4.83 ± 3.19 | 0.87 |
| Transfusion | 9 (6.4%) | 19 (15.3%) | 0.01 |
| Pelvic adhesion due to previous operation | |||
| grade 3 | 3 (2.1%) | 2 (1.6%) | |
| grade 4 | 14 (9.9%) | 4 (3.2%) | 0.07 |
| Pelvic endometriosis | |||
| grade 3 | 16 (11.3%) | 7 (5.6%) | |
| grade 4 | 19 (13.5%) | 30 (24.2%) | |
| Cooperated with pelvic peritonectomy | 26 (18.4%) | 27 (21.8%) | 0.61 |
| Complication | 0.03 | ||
| Transfusion | 9 (6.4%) | 19 (15.3%) | |
| Bladder injury | 0 | 0 | |
| Bowel injury | 0 | 1 (0.8%) | |
| Postoperative fever | 0 | 4 (1.6%) | |
| Intraperitoneal hematoma | 0 | 0 | |
| Reoperation | 0 | 0 | |
| Postoperative hospital stay | 0.47 | ||
| ≤3 days | 139 (98.6%) | 121 (97.6%) | |
| 6–8 days | 1 (0.7%) | 2 (1.6%) | |
| 9–12 days | 1 (0.7%) | 0 | |
| ≥13 days | 0 | 0 | |
| Clinical Outcome | Mean ± SD, No of Patients (%) | ||
|---|---|---|---|
| Fundusectomy | Adenomyomectomy | p-Value | |
| Preoperative longitudinal length of uterus (cm) | 10.04 ± 1.90 | 10.32 ± 10.56 | 0.76 |
| Preoperative volume of uterus (gm) | 332.55 ± 193.97 | 263.09 ± 144.53 | 0.00 |
| Preoperative CA125 (U/mL) | 68.37 ± 70.26 | 119.55 ± 170.03 | 0.00 |
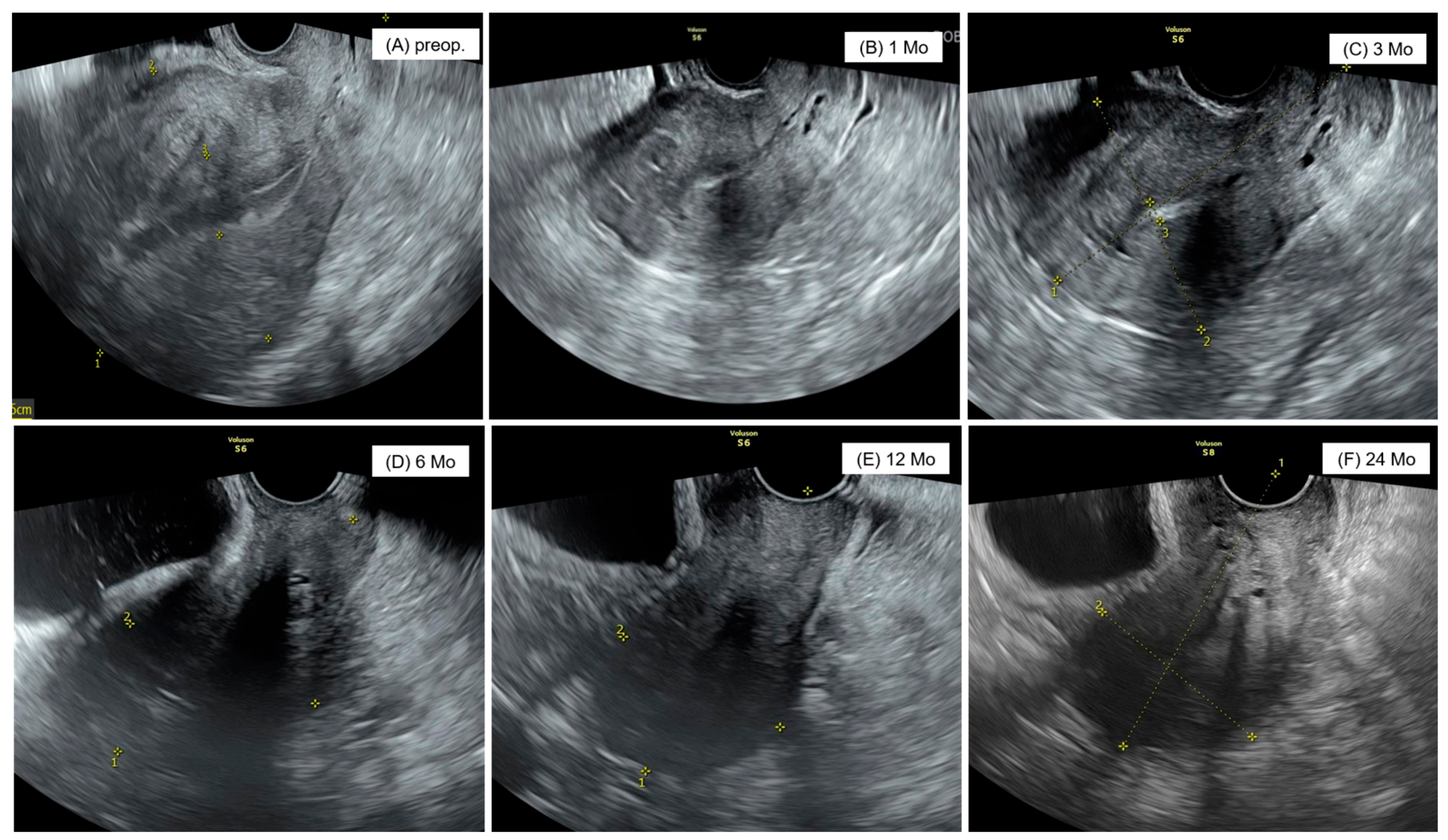
| Postoperative state 1 Mo later | |||
| Longitudinal length of uterus (cm) | 7.02 ± 1.02 | 8.51 ± 4.41 | 0.00 |
| Weight of uterus (gm) | 83.09 ± 40.20 | 136.48 ± 75.76 | 0.00 |
| CA125 (U/mL) | 19.73 ± 14.49 | 63.56 ± 62.06 | 0.00 |
| Postoperative state 3 Mo later | |||
| Longitudinal length of uterus (cm) | 6.61 ± 0.97 | 7.26 ± 1.28 | 0.00 |
| Volume of uterus (gm) | 72.09 ± 32.32 | 94.45 ± 66.12 | 0.00 |
| CA125 (U/mL) | 16.19 ± 11.50 | 19.63 ± 19.68 | 0.41 |
| Postoperative state 6 Mo later | |||
| Longitudinal length of uterus (cm) | 6.49 ± 1.04 | 7.58 ± 1.64 | 0.00 |
| Volume of uterus (gm) | 64.54 ± 42.36 | 108.52 ± 79.84 | 0.00 |
| CA125 (U/mL) | 14.42 ± 9.09 | 22.49 ± 20.58 | 0.00 |
| Postoperative state 12 Mo later | |||
| Longitudinal length of uterus (cm) | 6.61 ± 1.18 | 7.73 ± 1.31 | 0.00 |
| Volume of uterus (gm) | 63.27 ± 35.39 | 109.95 ± 78.97 | 0.00 |
| CA125 (U/mL) | 17.16 ± 21.91 | 25.36 ± 20.87 | 0.06 |
| Postoperative state 24 Mo later | |||
| Longitudinal length of uterus (cm) | 6.38 ± 1.09 | 7.80 ±1.47 | 0.00 |
| Volume of uterus (gm) | 58.11 ± 31.12 | 128.55 ± 143.16 | 0.00 |
| CA125 (U/mL) | 20.69 ± 22.07 | 55.02 ± 122.45 | 0.14 |
| Reoperation | 0 | 8 (6.5%) | 0.00 |
| Hysterectomy | 0 | 4 (50%) | |
| Fundusectomy | 0 | 4 (50%) | |
| Long term complication | 0 | 0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, J.H.; Kim, Y.R.; Kim, B.R.; Lee, J.W.; Oh, S.Y.; Yun, J.H.; Han, M.S.; Song, Y.J.; Kim, K.H. Comparison of Surgical Outcomes Between Single-Site Laparoscopic Adenomyomectomy and Fundusectomy: Experience from a Single Center. J. Clin. Med. 2025, 14, 4044. https://doi.org/10.3390/jcm14124044
Jeong JH, Kim YR, Kim BR, Lee JW, Oh SY, Yun JH, Han MS, Song YJ, Kim KH. Comparison of Surgical Outcomes Between Single-Site Laparoscopic Adenomyomectomy and Fundusectomy: Experience from a Single Center. Journal of Clinical Medicine. 2025; 14(12):4044. https://doi.org/10.3390/jcm14124044
Chicago/Turabian StyleJeong, Jae Hyeok, Yoo Ri Kim, Bo Ram Kim, Ji Won Lee, Seung Yeon Oh, Jeong Hye Yun, Myoung Seok Han, Yong Jung Song, and Ki Hyung Kim. 2025. "Comparison of Surgical Outcomes Between Single-Site Laparoscopic Adenomyomectomy and Fundusectomy: Experience from a Single Center" Journal of Clinical Medicine 14, no. 12: 4044. https://doi.org/10.3390/jcm14124044
APA StyleJeong, J. H., Kim, Y. R., Kim, B. R., Lee, J. W., Oh, S. Y., Yun, J. H., Han, M. S., Song, Y. J., & Kim, K. H. (2025). Comparison of Surgical Outcomes Between Single-Site Laparoscopic Adenomyomectomy and Fundusectomy: Experience from a Single Center. Journal of Clinical Medicine, 14(12), 4044. https://doi.org/10.3390/jcm14124044





