Presence of Anxiety and Depression in Patients with Open-Angle Glaucoma of Different Degrees of Damage
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants (Respondents)
2.2. Questionnaires
2.3. Statistical Methods
2.4. Study Approval
3. Results
3.1. Basic Characteristics of the Participants
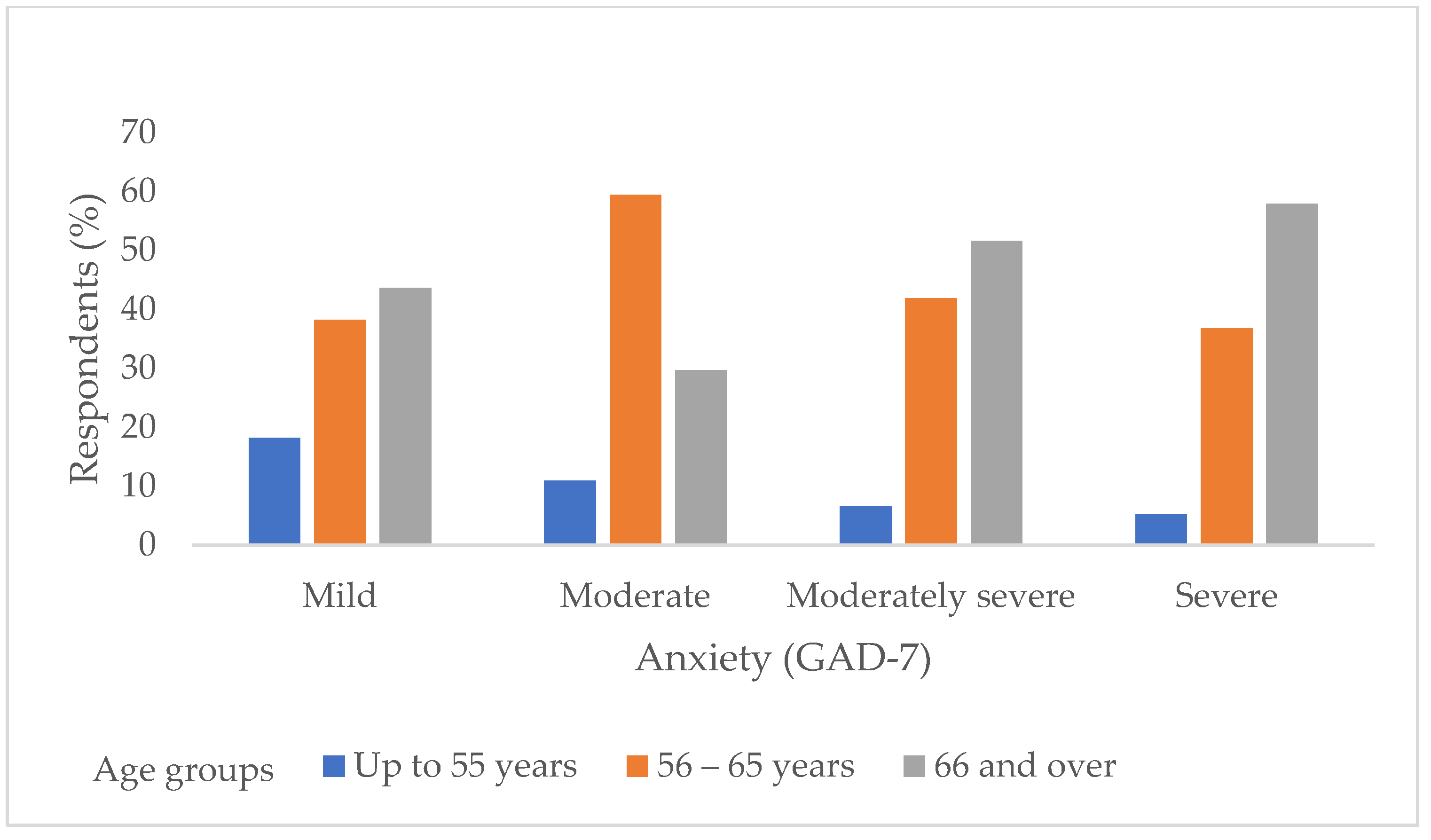
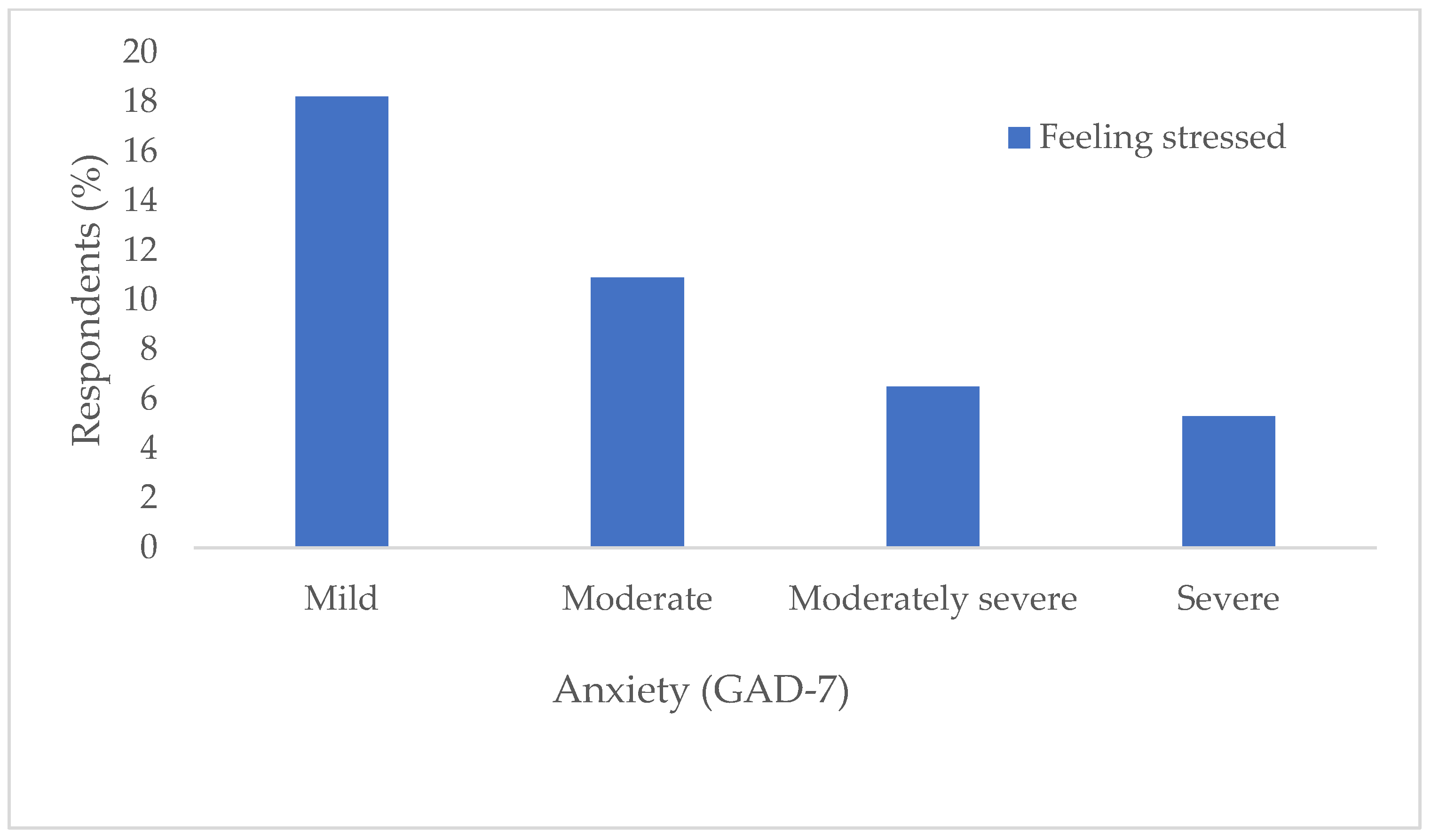
3.2. Correlations Between Glaucoma Stages and Anxiety (GAD-7) Correlation of Respondents’ Anxiety (GAD-7 Questionnaire) with Respondents’ Characteristics
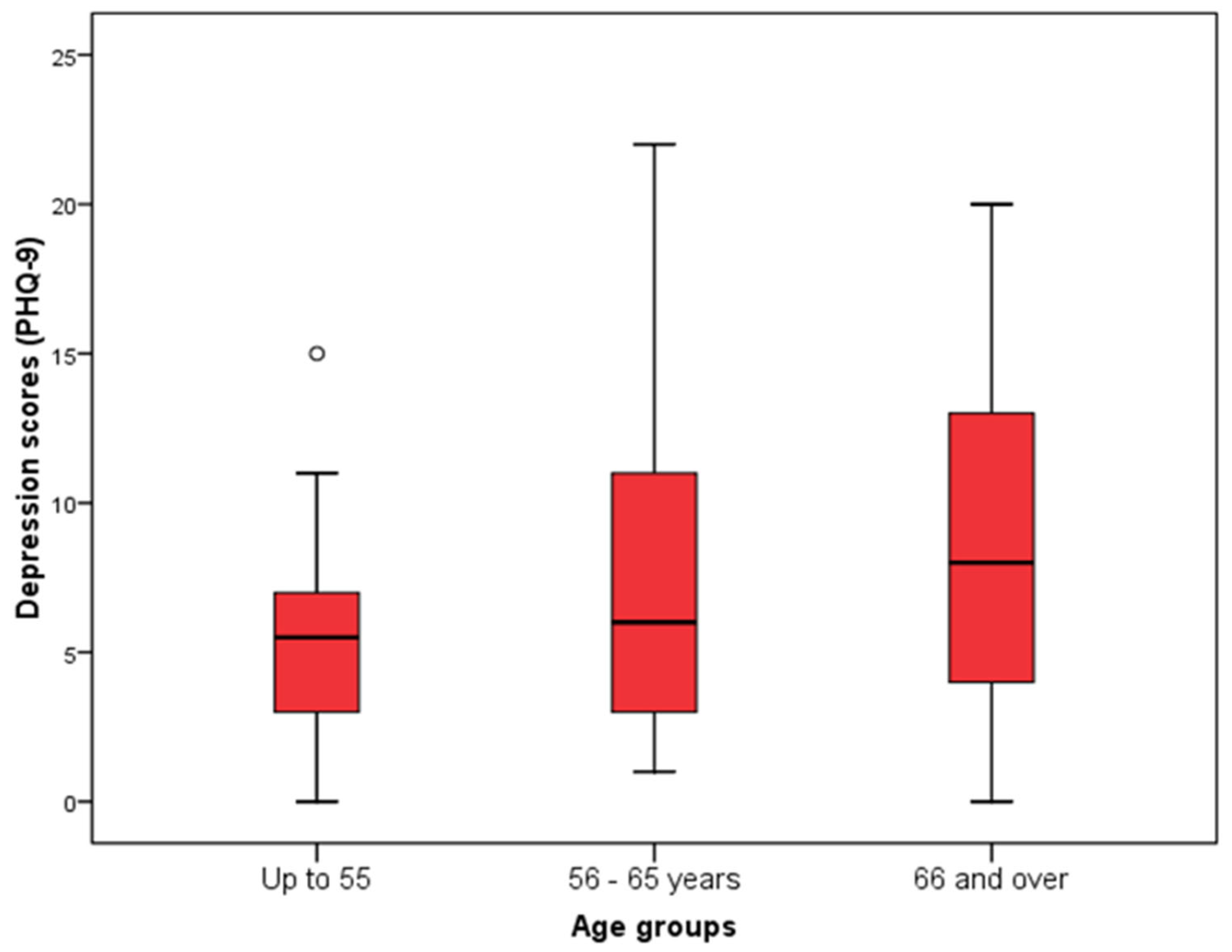
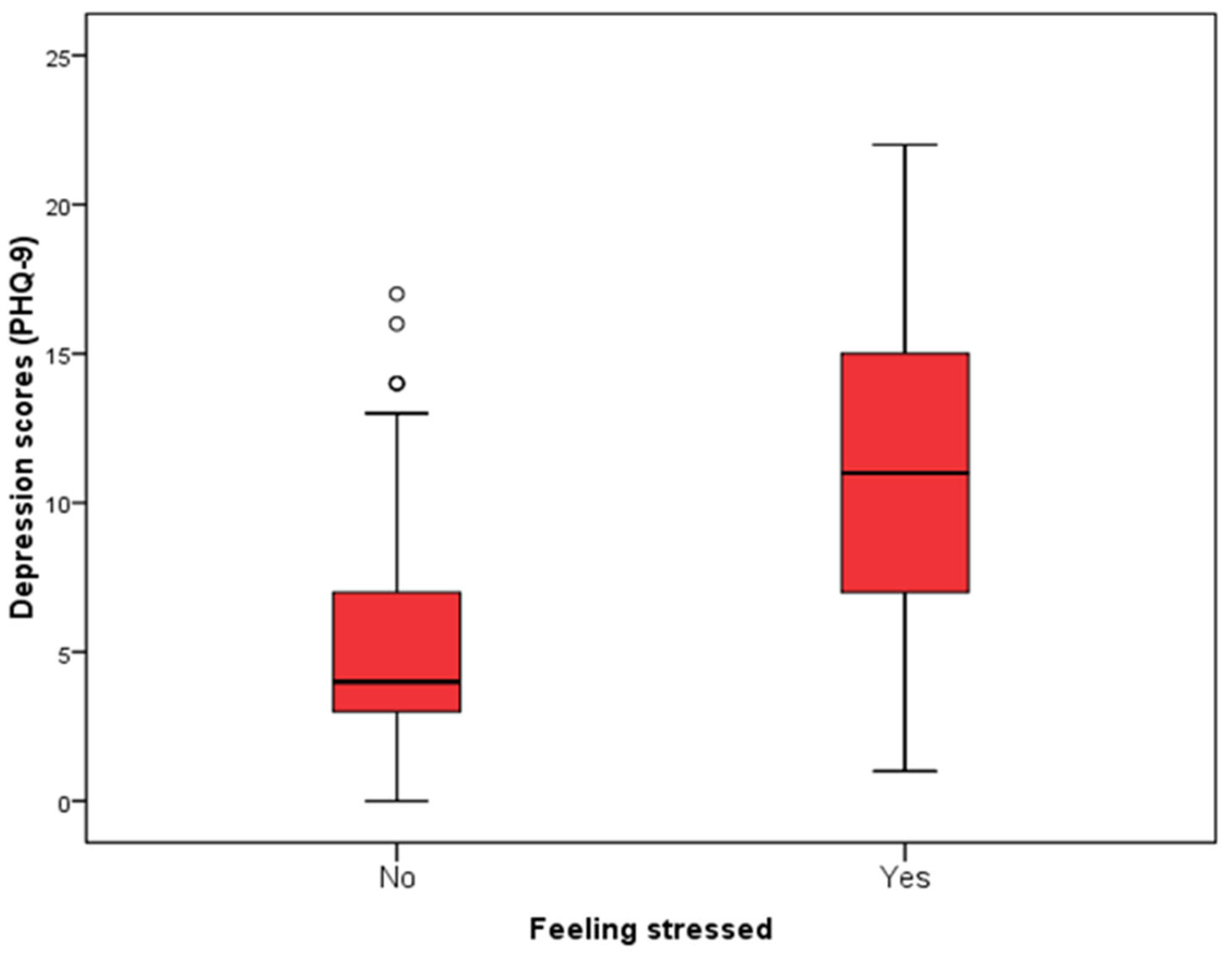
3.3. Correlations Between Glaucoma Stages and Depression (PHQ-9) Association of Depression (PHQ-9 Questionnaire) with Characteristics of the Subjects
3.4. Correlations Between Glaucoma Stages and Psychoneurotic Disorders (CCEI)
3.5. Association of Psychoneurotic Disorders (CCEI Questionnaire) with the Age of the Subjects, the Duration of Treatment and the Stage of Glaucoma
3.6. The Influence of Glaucoma Stage and Other Characteristics of the Subjects on the Severity of Anxiety and Depression
3.7. Correlation of the Depression Subscale with the Characteristics of the Subjects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACG | Angle-closure glaucoma |
| ATG | Antiglaucoma |
| CCEI | Crown-Crisp Experiential Index |
| dB | Decibel |
| FFA | Free-floating anxiety |
| GAD-7 | General Anxiety Disorder 7 |
| GAT | Goldmann applanation tonometry |
| GCL | Ganglion cell layer |
| IOP | Intraocular pressure |
| IQR | Interquartile range |
| MD | Mean deviation |
| mmHg | Millimeters of mercury |
| NTG | Normal tension glaucoma |
| OAG | Open-angle glaucoma |
| OR | Odds ratio |
| PHOA | Phobic anxiety |
| PHQ-9 | Patient Health Questionnaire 9 |
| POAG | Primary open-angle glaucoma |
| RNFL | Retinal nerve fibre layer |
| VF | Visual field |
References
- Kaliaperumal, S.; Janani, V.S.; Menon, V.; Sarkar, S.; Behera, G.; Kattamani, S. Study of anxiety in patients with glaucoma undergoing standard automated perimetry and optical coherence tomography—A prospective comparative study. Indian J. Ophthalmol. 2022, 70, 2883–2887. [Google Scholar] [CrossRef] [PubMed]
- Jayaram, H.; Kolko, M.; Friedman, D.S.; Gazzard, G. Glaucoma: Now and beyond. Lancet. 2023, 402, 1788–1801. [Google Scholar] [CrossRef]
- Kang, J.M.; Tanna, A.P. Glaucoma. Med. Clin. N. Am. 2021, 105, 493–510. [Google Scholar] [CrossRef] [PubMed]
- Bušić, M.; Elabjer Kuzmanović, B.; Bosnar, D. Seminaria Ophthalmologica, 3rd ed.; Cerovski d.o.o.: Zagreb, Croatia, 2014. [Google Scholar]
- Maričić Došen, V. Glaukom—Rana dijagnostika i liječenje. Medix: Spec. Med. Dvomjesečnik, 2008, 14. Available online: https://www.medix.hr/glaukom--rana-dijagnostika-i-lijecenje_eng (accessed on 30 April 2025).
- Hrvatska enciklopedija. glaukom—Hrvatska enciklopedija [Internet]. Hrvatska enciklopedija. 2025. Available online: https://www.enciklopedija.hr/clanak/glaukom (accessed on 20 March 2025).
- Asrani, S.G.; McGlumphy, E.J.; Al-Aswad, L.A.; Chaya, C.J.; Lin, S.; Musch, D.C.; Pitha, I.; Robin, A.L.; Wirostko, B.; Johnson, T.V. The relationship between intraocular pressure and glaucoma: An evolving concept. Prog. Retin. Eye Res. 2024, 103, 101303. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.K.; Erb, C.; Hoffmann, E.M.; Dietlein, T.; Pfeiffer, N. The Diagnosis and Treatment of Glaucoma. Deutsches Ärzteblatt international [Internet]. 2020 Mar 27. Available online: https://www.aerzteblatt.de/10.3238/arztebl.2020.0225 (accessed on 18 January 2025).
- Lešin Gaćina, D.; Jandroković, S.; Marčinko, D.; Škegro, I.; Vidas Pauk, S.; Tomić, M.; Škegro, B.; Barišić Kutija, M.; Ivkić, P.K. Anxiety and Treatment Adherence among Glaucoma Patients during COVID-19 Pandemic and Earthquakes in Croatia. Psychiatr. Danub. 2022, 34, 348–355. [Google Scholar] [CrossRef]
- Zeppieri, M.; Gurnani, B. Applanation Tonometry. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK582132/ (accessed on 9 February 2025).
- Mahabadi, N.; Zeppieri, M.; Tripathy, K. Open Angle Glaucoma. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK441887/ (accessed on 18 January 2025).
- Šikić, J. Oftalmologija, 1st ed.; Narodne Novine: Zagreb, Croatia, 2003. [Google Scholar]
- Bradamante, Ž.; Bradetić, T.; Brzović, Z. Oftalmologija, 1st ed.; Nakladni Zavod Globus: Zagreb, Croatia, 1994. [Google Scholar]
- Čupak, K.; Gabrić, N.; Cerovski, B. Oftalmologija, 2nd ed.; Nakladni Zavod Globus: Zagreb, Croatia, 2004. [Google Scholar]
- Knezović, I. Oftalmologija za Studij Sestrinstva; Visoka Tehnička Škola u Bjelovaru: Bjelovar, Croatia, 2015. [Google Scholar]
- Mandić, Z. Oftalmologija, 1st ed.; Medicinska Naklada: Zagreb, Croatia, 2014. [Google Scholar]
- Dave, S.D.; Zeppieri, M.; Meyer, J.J. Chronic Closed Angle Glaucoma. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK559098/ (accessed on 18 January 2025).
- European Glaucoma Society Terminology and Guidelines for Glaucoma, 5th Edition. Br. J. Ophthalmol. 2021, 105 (Suppl. S1), 1–169. [CrossRef]
- Sihota, R.; Angmo, D.; Ramaswamy, D.; Dada, T. Simplifying “target” intraocular pressure for different stages of primary open-angle glaucoma and primary angle-closure glaucoma. Indian J. Ophthalmol. 2018, 66, 495. [Google Scholar] [CrossRef]
- Wu, N.; Kong, X.; Sun, X. Anxiety and depression in Chinese patients with glaucoma and its correlations with vision-related quality of life and visual function indices: A cross-sectional study. BMJ Open 2022, 12, e046194. [Google Scholar] [CrossRef]
- Agorastos, A.; Skevas, C.; Matthaei, M.; Otte, C.; Klemm, M.; Richard, G.; Huber, C.G. Depression, anxiety, and disturbed sleep in glaucoma. J. Neuropsychiatry Clin. Neurosci. 2013, 25, 205–213. [Google Scholar] [CrossRef]
- Kang, E.; Wen, Z.; Song, H.; Christian, K.M.; Ming, G.L. Adult Neurogenesis and Psychiatric Disorders. Cold Spring Harb. Perspect. Biol. 2016, 8, a019026. [Google Scholar] [CrossRef]
- Lim, M.C.; Shiba, D.R.; Clark, I.J.; Kim, D.Y.; Styles, D.E.; Brandt, J.D.; Watnik, M.R.; Barthelow, I.J. Personality type of the glaucoma patient. J. Glaucoma. 2007, 16, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Zimet, C.N.; Berger, A.S. Emotional factors in primary glaucoma: An evaluation of psychological test data. Psychosom. Med. 1960, 22, 391–399. [Google Scholar] [CrossRef]
- Pappa, C.; Hyphantis, T.; Pappa, S.; Aspiotis, M.; Stefaniotou, M.; Kitsos, G.; Psilas, K.; Mavreas, V. Psychiatric manifestations and personality traits associated with compliance with glaucoma treatment. J. Psychosom. Res. 2006, 61, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Scuderi, G.; Pompili, M.; Innamorati, M.; Pasquale, N.; Pontremolesi, S.; Erbuto, D.; Mazzeo, F.; Venturini, P.; Lester, D.; Serafini, G.; et al. Affective temperaments are associated with higher hopelessness and perceived disability in patients with open-angle glaucoma. Int. J. Clin. Pract. 2011, 65, 976–984. [Google Scholar] [CrossRef]
- Igarashi, Y.; Sato, E.; Ito, A.; Miyauchi, O.; Ikejiri, M.; Hanawa, T.; Tsuyama, Y.; Mizota, A.; Fujimoto, N.; Adachi-Usami, E. Comparison of Yatabe-Guilford personality test results in retinitis pigmentosa and glaucoma patients. Jpn. J. Ophthalmol. 2003, 47, 1–5. [Google Scholar] [CrossRef]
- Bubella, R.M.; Bubella, D.M.; Cillino, S. Type A behavior pattern: Is it a risk factor for open-angle chronic glaucoma? J. Glaucoma. 2014, 23, 199–201. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, H.; Altinyazar, V.; Yilmaz, S.G.; Ömürlü, İ.K.; Kocatürk, T.; Yazici, A.; Değirmenci, C.; Dündar, S.O.; Ates, H. The temperament and character personality profile of the glaucoma patient. BMC Ophthalmol. 2015, 15, 125. [Google Scholar] [CrossRef][Green Version]
- Crown, S.; Crisp, A.H. Crown-Crispov Indeks Iskustva; Naklada Slap: Jastrebarsko, Croatia, 1994. [Google Scholar]
- Pačić Turk, L.; Tomašić, B.; Divčić, B. Povezanost demografskih, socijalnih i zdravstvenih čimbenika, neuroticizma i obilježja emocionalnosti s poremećajima hranjenja. Klin. Psihol. 2013, 6, 1–25. [Google Scholar]
- Birtchnell, J.; Evans, C.; Kennard, J. The total score of the Crown-Crisp Experiential Index: A useful and valid measure of psychoneurotic pathology. Br. J. Med. Psychol. 1988, 61 Pt 3, 255–266. [Google Scholar] [CrossRef]
- Živkov, A. Procjena Anksioznosti i Depresivnosti Studenata Fakulteta za Dentalnu Medicinu i Zdravstvo Osijek. Diploma Thesis, Sveučilište Josipa Jurja Strossmayera u Osijeku, Fakultet za dentalnu medicinu i zdravstvo Osijek, Osijek, Croatia, 2022. [Google Scholar]
- Islam, S.; Akter, R.; Sikder, T.; Griffiths, M.D. Prevalence and Factors Associated with Depression and Anxiety Among First-Year University Students in Bangladesh: A Cross-Sectional Study. Int. J. Ment. Health Addict. 2022, 20, 1289–1302. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Löwe, B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Daniel, W.W. Biostatistics: A Foundation for Analysis in the Health Sciences; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2012. [Google Scholar]
- Armitage, P.; Perry, G. Statistical Methods in Medical Research; Wiley-Blackwell: Hoboken, NJ, USA, 2001. [Google Scholar]
- MedCalc Software Ltd., Ostend, Belgium. Available online: https://www.medcalc.org (accessed on 27 March 2025).
- EQUATOR The EQUATOR Network | Enhancing the QUAlity and Transparency Of Health Research [Internet]. Equator-network.org. 2019. Available online: https://www.equator-network.org/ (accessed on 25 January 2025).
- Sabel, B.A.; Wang, J.; Cárdenas-Morales, L.; Faiq, M.; Heim, C. Mental stress as consequence and cause of vision loss: The dawn of psychosomatic ophthalmology for preventive and personalized medicine. EPMA J. 2018, 9, 133–160. [Google Scholar] [CrossRef] [PubMed]
- Groff, M.L.; Choi, B.; Lin, T.; Mcllraith, I.; Hutnik, C.; Malvankar-Mehta, M.S. Anxiety, depression, and sleep-related outcomes of glaucoma patients: Systematic review and meta-analysis. Can. J. Ophthalmol. 2023, 58, 346–355. [Google Scholar] [CrossRef]
- Zhang, N.; Wang, J.; Li, Y.; Jiang, B. Prevalence of primary open angle glaucoma in the last 20 years: A meta-analysis and systematic review. Sci. Rep. 2021, 11, 13762. [Google Scholar] [CrossRef]
- Shin, D.Y.; Jung, K.I.; Park, H.Y.L.; Park, C.K. The effect of anxiety and depression on progression of glaucoma. Sci. Rep. 2021, 11, 1769. [Google Scholar] [CrossRef]
- Yin, J.; Li, H.; Guo, N. Prevalence of Depression and Anxiety Disorders in Patients with Glaucoma: A Systematic Review and Meta-Analysis Based on Cross-Sectional Surveys. Actas Esp. Psiquiatr. 2024, 52, 325–333. [Google Scholar] [CrossRef]
- InformedHealth.org [Internet]. Glaucoma: Learn More—Treatment Options for Glaucoma; Institute for Quality and Efficiency in Health Care (IQWiG): Cologne, Germany, 2006. Available online: https://www.ncbi.nlm.nih.gov/books/NBK367575/ (accessed on 12 April 2025).
- Dayal, A.; Sodimalla, K.V.K.; Chelerkar, V.; Deshpande, M. Prevalence of Anxiety and Depression in Patients With Primary Glaucoma in Western India. J. Glaucoma 2022, 31, 37–40. [Google Scholar] [CrossRef]
- Onwubiko, S.N.; Nwachukwu, N.Z.; Muomah, R.C.; Okoloagu, N.M.; Ngwegu, O.M.; Nwachukwu, D.C. Factors associated with depression and anxiety among glaucoma patients in a tertiary hospital South-East Nigeria. Niger. J. Clin. Pract. 2020, 23, 315–321. [Google Scholar]
| Instrument | Purpose/Primary Focus | Number of Items | Clinical Validation | Usability for Patients |
|---|---|---|---|---|
| CCEI (Crown–Crisp Experiential Index) | Assesses six domains of neurotic disorders: free-floating anxiety, phobic anxiety, obsessiveness, somatic symptoms, depression, and hysteria | 48 | Validated in multiple clinical populations; commonly used in psychoneurotic assessments [32] | Moderate—requires more time and cognitive effort |
| GAD-7 (Generalized Anxiety Disorder-7) | Screens for and measures severity of generalized anxiety disorder | 7 | Widely validated and recommended for clinical use [36] | High—short, simple, and user-friendly |
| PHQ-9 (Patient Health Questionnaire-9) | Screens for and evaluates severity of depressive symptoms | 9 | High clinical validity and reliability [37] | High—brief and easy to administer |
| Sex [n (%)] | |
| Male | 68 (34) |
| Female | 132 (66) |
| Age groups [n (%)] | |
| Up to 55 | 22 (11.0) |
| 56–65 years | 92 (46.0) |
| 66 and over | 86 (43.0) |
| OAG stage [n (%)] | |
| Stage I | 68 (34.0) |
| Stage II | 65 (32.5) |
| Stage III | 67 (33.5) |
| Earlier ophthalmological state [n (%)] | 36 (18.0) |
| Subjective feeling under stress [n (%)] | 93 (46.5) |
| Achieved IOP goal [n (%)] | 150 (75) |
| Age (years) [Median (IQR)] | 65 (60–68) |
| Length of treatment (months) [Median (IQR)] | 96 (39–156) |
| Number of application of ATG therapy per day [Median (IQR)] | 2 (1–2) |
| OAG stage [n (%)] | |
| Stage I | 68 (34.0) |
| Stage II | 65 (32.5) |
| Stage III | 67 (33.5) |
| GAD-7 Total Score [Median (IQR)] | 8 (4–12) |
| Level of anxiety [n (%)] | |
| Mild (0–4) | 55 (27.5) |
| Moderate (5–9) | 64 (32.0) |
| Moderately Severe (10–14) | 62 (31.0) |
| Severe anxiety (15–21) | 19 (9.5) |
| PHQ-9 Total Score [Median (IQR)] | 7 (3–11) |
| Level of depression [n (%)] | |
| Minor (0–4) | 69 (34.5) |
| Mild (5–9) | 62 (31.0) |
| Moderate (10–14) | 38 (19.0) |
| Moderately Severe (15–19) | 28 (14.0) |
| Severe depression (20–27) | 3 (1.5) |
| Median (IQR) GAD-7 | Difference | 95% Confidence Interval | p | |
|---|---|---|---|---|
| Gender | ||||
| Men | 8 (4–12) | 0 | −1–2 | 0.99 * |
| Women | 8 (4–12) | |||
| Age groups | ||||
| Up to 55 years | 5 (3–9) | 0.06 † | ||
| 56–65 years | 8 (5–12) | - | - | |
| 66 and over | 9 (4–13) | |||
| OAG stage | ||||
| Stage I | 7 (5–12) | 0.91 † | ||
| Stage II | 8 (4–12) | - | - | |
| Stage III | 8 (4–12) | |||
| Feeling stressed | ||||
| No | 5 (3–9) | 5 | 3–6 | <0.001 * |
| Yes | 11 (7–14) | |||
| Achieved IOP target values | ||||
| No | 7 (4–11) | 1 | 0–3 | 0.13 * |
| Yes | 8 (4–13) | |||
| Spearman’s Rho Correlation Coefficient (p Value) | |||
|---|---|---|---|
| Age of the Respondent | Length of Treatment | Glaucoma Stage | |
| GAD-7 scale—all respondents | 0.133 (0.06) | 0.124 (0.08) | 0.001 (0.99) |
| GAD-7 scale | |||
| IOP target values not achieved | −0.157 (0.28) | 0.209 (0.15) | 0.110 (0.45) |
| IOP target values achieved | 0.215 (0.008) | 0.120 (0.14) | 0.036 (0.66) |
| Median (IQR) | Difference | 95% Confidence Interval | p | |
|---|---|---|---|---|
| Sex | ||||
| Male | 7 (4–11) | 0 | −1–2 | 0.76 * |
| Female | 7 (3–12) | |||
| Age groups | ||||
| Up to 55 | 6 (3–7) | - | - | 0.03 †§ |
| 56–65 years | 6 (3–11) | |||
| 66 and over | 8 (4–13) | |||
| OAG stage | ||||
| Stage I | 6 (4–11) | 0.95 † | ||
| Stage II | 7 (3–11) | - | - | |
| Stage III | 7 (3–12) | |||
| Feeling stressed | ||||
| No | 4 (3–7) | 6 | 4–7 | <0.001 * |
| Yes | 11 (7–15) | |||
| Achieved IOP target values | ||||
| Not | 6 (3–9) | 1 | −1–2 | 0.31 * |
| That | 7 (4–12) | |||
| Spearman’s Rho Correlation Coefficient (p Value) | |||
|---|---|---|---|
| Age of Subjects | Length of Treatment | Degree of Glaucoma | |
| PHQ-9 scale—all respondents | 0.182 (0.01) | 0.199 (0.005) | 0.020 (0.78) |
| PHQ-9 scale | |||
| IOP target values not achieved | −0.152 (0.29) | 0.144 (0.32) | 0.154 (0.29) |
| IOP target values achieved | 0.269 (0.001) | 0.221 (0.006) | 0.035 (0.67) |
| Median (IQR) | Range from Minimum to Maximum Value | |
|---|---|---|
| Free floating anxiety (FFA) | 5 (2–10) | 0–16 |
| Phobic anxiety (PHOA) | 5 (4–7) | 0–16 |
| Obsessiveness | 8 (6–10) | 0–14 |
| Somatic manifestations of anxiety | 7 (4–10) | 0–16 |
| Depression | 7 (4–9) | 0–14 |
| Hysteria | 4 (2–5) | 0–12 |
| Number (%) of Respondents in Relation to the Severity of Each Subscale | ||
| Not Expressed | Expressed | |
| Free floating anxiety (FFA) | 119 (59.5) | 81 (40.5) |
| Phobic anxiety (PHOA) | 133 (66.5) | 67 (33.5) |
| Obsessiveness | 158 (79.0) | 42 (21.0) |
| Somatic manifestations of anxiety | 133 (66.5) | 67 (33.5) |
| Depression | 102 (51.0) | 98 (49.0) |
| Hysteria | 146 (73.0) | 54 (27.0) |
| Spearman’s Correlation Coefficient Rho (p Value) | |||
|---|---|---|---|
| Age of the Respondent | Duration of Treatment | Glaucoma Stage | |
| All respondents | |||
| Free floating anxiety (FFA) | 0.068 (0.34) | 0.109 (0.12) | −0.006 (0.94) |
| Phobic anxiety (PHOA) | 0.042 (0.56) | 0.051 (0.48) | 0.049 (0.49) |
| Obsessiveness | 0.050 (0.48) | 0.050 (0.48) | −0.147 (0.04) |
| Somatic manifestations of anxiety | 0.190 (0.01) | 0.164 (0.02) | 0.022 (0.76) |
| Depression | 0.183 (0.01) | 0.082 (0.25) | 0.023 (0.75) |
| Hysteria | −0.021 (0.77) | 0.051 (0.48) | −0.134 (0.06) |
| Target IOP not reached | |||
| Free floating anxiety (FFA) | −0.344 (0.01) | 0.022 (0.88) | −0.053 (0.71) |
| Phobic anxiety (PHOA) | −0.062 (0.67) | 0.011 (0.94) | 0.154 (0.29) |
| Obsessiveness | −0.057 (0.69) | 0.013 (0.93) | −0.104 (0.47) |
| Somatic manifestations of anxiety | 0.034 (0.81) | 0.042 (0.77) | −0.053 (0.71) |
| Depression | −0.040 (0.78) | 0.090 (0.54) | −0.084 (0.56) |
| Hysteria | −0.125 (0.39) | −0.086 (0.55) | −0.323 (0.02) |
| Target IOP achieved | |||
| Free floating anxiety (FFA) | 0.174 (0.03) | 0.143 (0.08) | 0.043 (0.60) |
| Phobic anxiety (PHOA) | 0.077 (0.35) | 0.067 (0.42) | 0.052 (0.53) |
| Obsessiveness | 0.096 (0.24) | 0.068 (0.41) | −0.094 (0.26) |
| Somatic manifestations of anxiety | 0.222 (0.01) | 0.197 (0.02) | 0.073 (0.37) |
| Depression | 0.251 (<0.001) | 0.100 (0.23) | 0.100 (0.23) |
| Hysteria | 0.016 (0.84) | 0.100 (0.22) | −0.028 (0.74) |
| β | Wald | p | Odds Ratio (OR) | 95% Confidence Interval | |
|---|---|---|---|---|---|
| PHQ-9 | |||||
| Age (66 and over) | 0.06 | 5.50 | 0.02 | 2.03 | 1.03–3.99 |
| Feeling stressed | 2.27 | 39.3 | <0.001 | 9.47 | 4.75–19.59 |
| Constant | −6.27 | 10.7 | 0.001 | ||
| GAD-7 | |||||
| Feeling stressed | 1.79 | 21.4 | <0.001 | 6.02 | 2.82–12.9 |
| Constant | 0.32 | 2.68 | 0.04 | ||
| FFA (CCEI) | |||||
| Sex (Female) | 1.11 | 7.97 | 0.005 | 3.03 | 1.40–6.52 |
| Feeling stressed | 2.04 | 28.9 | <0.001 | 7.70 | 3.66–16.21 |
| Constant | −2.03 | 30.6 | <0.001 | ||
| PHOA (CCEI) | |||||
| Sex (Female) | 1.81 | 21.3 | <0.001 | 6.12 | 2.84–13.2 |
| Age | 0.08 | 6.05 | 0.01 | 1.08 | 1.02–1.15 |
| Feeling stressed | 1.20 | 9.88 | 0.002 | 3.33 | 1.57–7.05 |
| Constant | −6.9 | 2.1 | 0.001 |
| Median (IQR) Depression Subscales | Difference | 95% Confidence Interval | p * | |
|---|---|---|---|---|
| Sex | ||||
| Male | 5 (4–8) | 1 | 0–2 | 0.006 |
| Female | 7 (5–9) | |||
| Age groups | ||||
| Under 55 years | 5 (4–6) | 0.007 †§ | ||
| 56–65 years | 6 (4–9) | - | - | |
| 66 and over | 7 (4–9) | |||
| Stage of OAG | ||||
| Stage I | 7 (4–9) | 0.94 † | ||
| Stage II | 6 (4–9) | - | - | |
| Stage III | 7 (4–9) | |||
| Feeling stressed | ||||
| No | 5 (3–7) | 3 | 2–3 | <0.001 |
| Yes | 8 (6–10) | |||
| Achieved IOP target values | ||||
| No | 6 (4–8) | 1 | 0–2 | 0.15 |
| Yes | 7 (4–9) | |||
| Number (%) of Respondents According to Severity of Depression | p * | |||
|---|---|---|---|---|
| No (n = 102) | Yes (n = 98) | Total (n = 200) | ||
| Sex | ||||
| Male | 37 (36.3) | 31 (31.6) | 68 (34) | 0.49 |
| Female | 65 (63.7) | 67 (68.4) | 132 (66) | |
| Age groups | ||||
| Up to 55 years | 18 (17.6) | 4 (4.1) | 22 (11) | 0.001 |
| 56–65 years | 51 (50) | 41 (41.8) | 92 (46) | |
| 66 and over | 33 (32.4) | 53 (54.1) | 86 (43) | |
| Stage of OAG | ||||
| Stage I | 34 (33.3) | 34 (34.7) | 68 (34) | 0.46 |
| Stage II | 37 (36.3) | 28 (28.6) | 65 (32.5) | |
| Stage III | 31 (30.4) | 36 (36.7) | 67 (33.5) | |
| Target IOP achieved | 73 (71.6) | 77 (78.6) | 150 (75) | 0.25 |
| Feeling stressed | 34 (33.3) | 59 (60.2) | 93 (46.5) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olujić, M.; Biuk, D.; Balog, S.; Kotromanović Šimić, I.; Kotromanović, D.; Dodig-Ćurković, K. Presence of Anxiety and Depression in Patients with Open-Angle Glaucoma of Different Degrees of Damage. J. Clin. Med. 2025, 14, 3954. https://doi.org/10.3390/jcm14113954
Olujić M, Biuk D, Balog S, Kotromanović Šimić I, Kotromanović D, Dodig-Ćurković K. Presence of Anxiety and Depression in Patients with Open-Angle Glaucoma of Different Degrees of Damage. Journal of Clinical Medicine. 2025; 14(11):3954. https://doi.org/10.3390/jcm14113954
Chicago/Turabian StyleOlujić, Marija, Dubravka Biuk, Slaven Balog, Ivana Kotromanović Šimić, Darko Kotromanović, and Katarina Dodig-Ćurković. 2025. "Presence of Anxiety and Depression in Patients with Open-Angle Glaucoma of Different Degrees of Damage" Journal of Clinical Medicine 14, no. 11: 3954. https://doi.org/10.3390/jcm14113954
APA StyleOlujić, M., Biuk, D., Balog, S., Kotromanović Šimić, I., Kotromanović, D., & Dodig-Ćurković, K. (2025). Presence of Anxiety and Depression in Patients with Open-Angle Glaucoma of Different Degrees of Damage. Journal of Clinical Medicine, 14(11), 3954. https://doi.org/10.3390/jcm14113954






