Evaluation of a Primary Health Care Scoliosis Screening Program: A 9-Year Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.1.1. Retrospective Study
- -
- Attendance records for each of the three mandatory screening phases (ages 5–6, 10–11, and 13–14 years) were reviewed to determine adherence to the program.
- -
- Clinical records were examined to identify findings related to spinal alignment and scoliosis suspicion at each screening phase.
- -
- The scoliosis screening protocol consisted of a visual back inspection performed without clothing.
- -
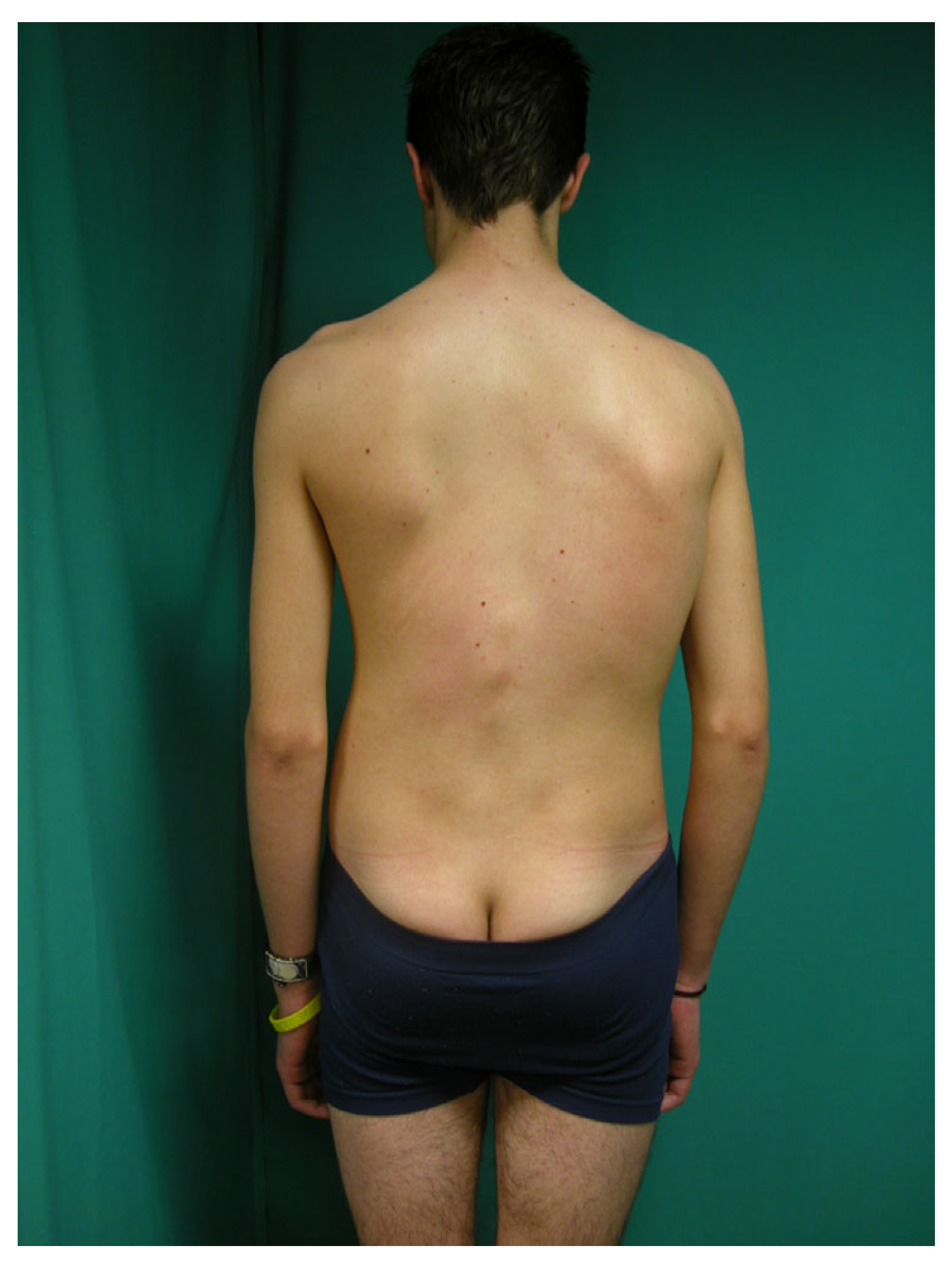
- Pediatricians classified children as having a “normal” or “scoliotic morphotype” based on a visual assessment in the standing position, focusing on the presence of asymmetries and/or uneven levels in the back (Figure 1)
- -
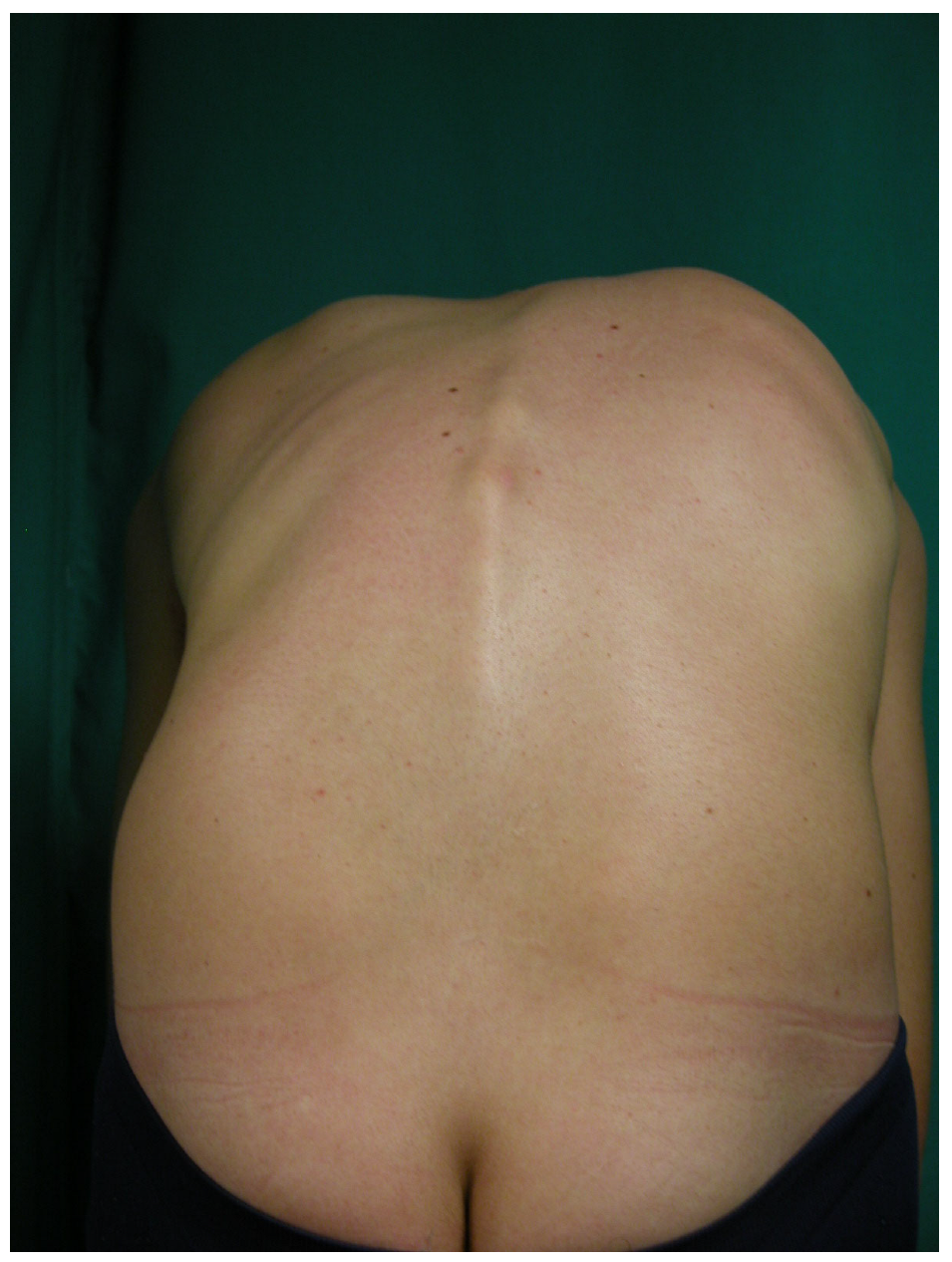
- All participants underwent the forward bending test (FBT) to assess for rib prominence (Figure 2). Community pediatricians documented findings as either “normal” or “Adams positive” when asymmetrical rib prominence was detected, suggesting possible scoliosis [24]. However, quantitative measurement was not performed during the initial PANA screenings.
- -
- Children with suspected scoliosis were referred to orthopedic specialists for further evaluation.
- -
- It is important to note that no quantitative measurement of spinal rotation was performed during these screenings, as a scoliometer was not provided as standard equipment by the Servicio Murciano de Salud.
- -
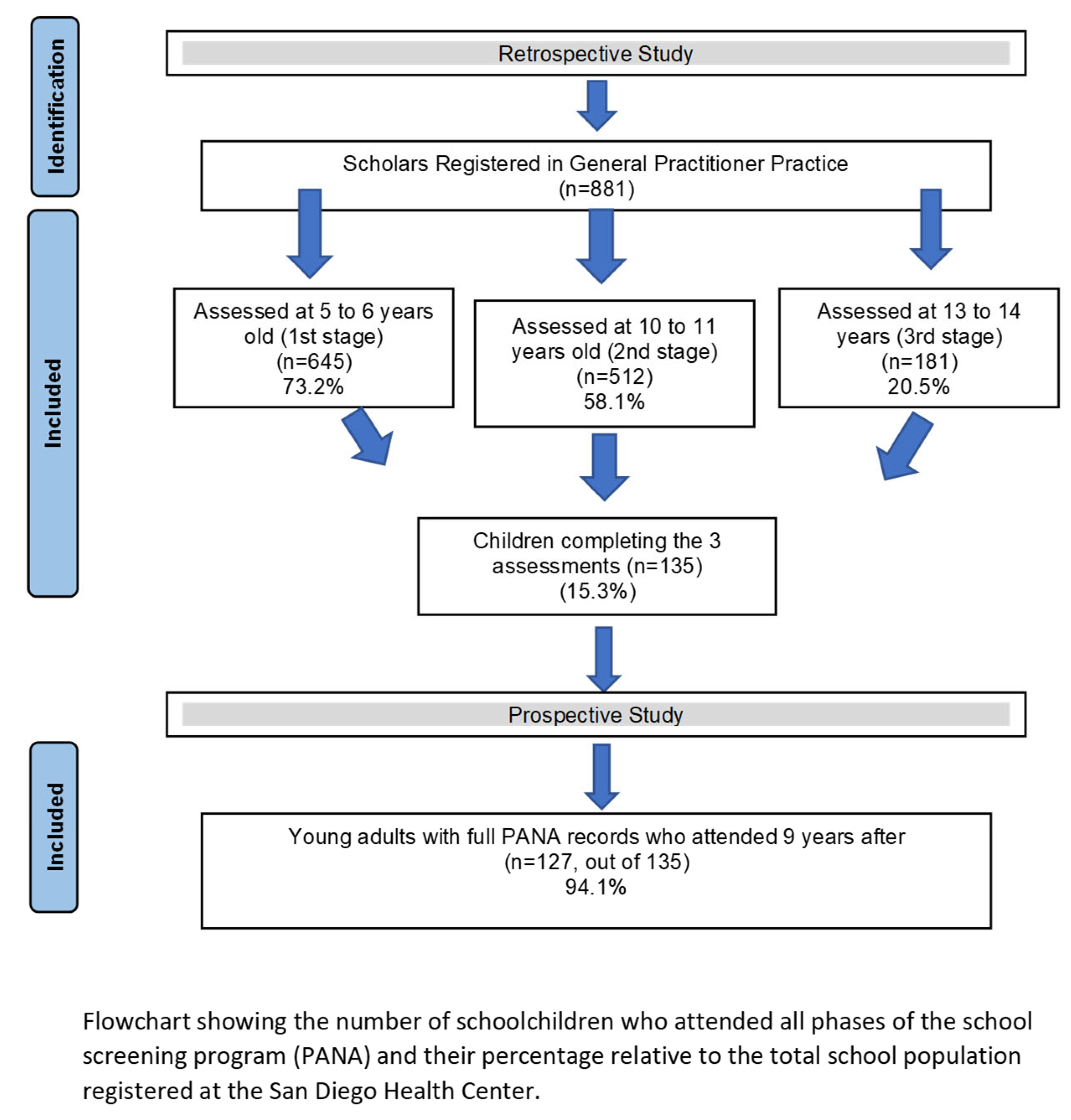
- The initial target population consisted of 881 schoolchildren (both male and female) who were scheduled to participate in all three phases of the PANA health screening program during three years. Figure 3 illustrates the sample distribution and dropout rates across the study timeline.
2.1.2. Prospective Study
- -
- A single trained physician conducted the follow-up evaluations to ensure consistency in examination techniques.
- -
- Assessments included a standing posture evaluation and a forward bending test (FBT) with a scoliometer.
- -
- -
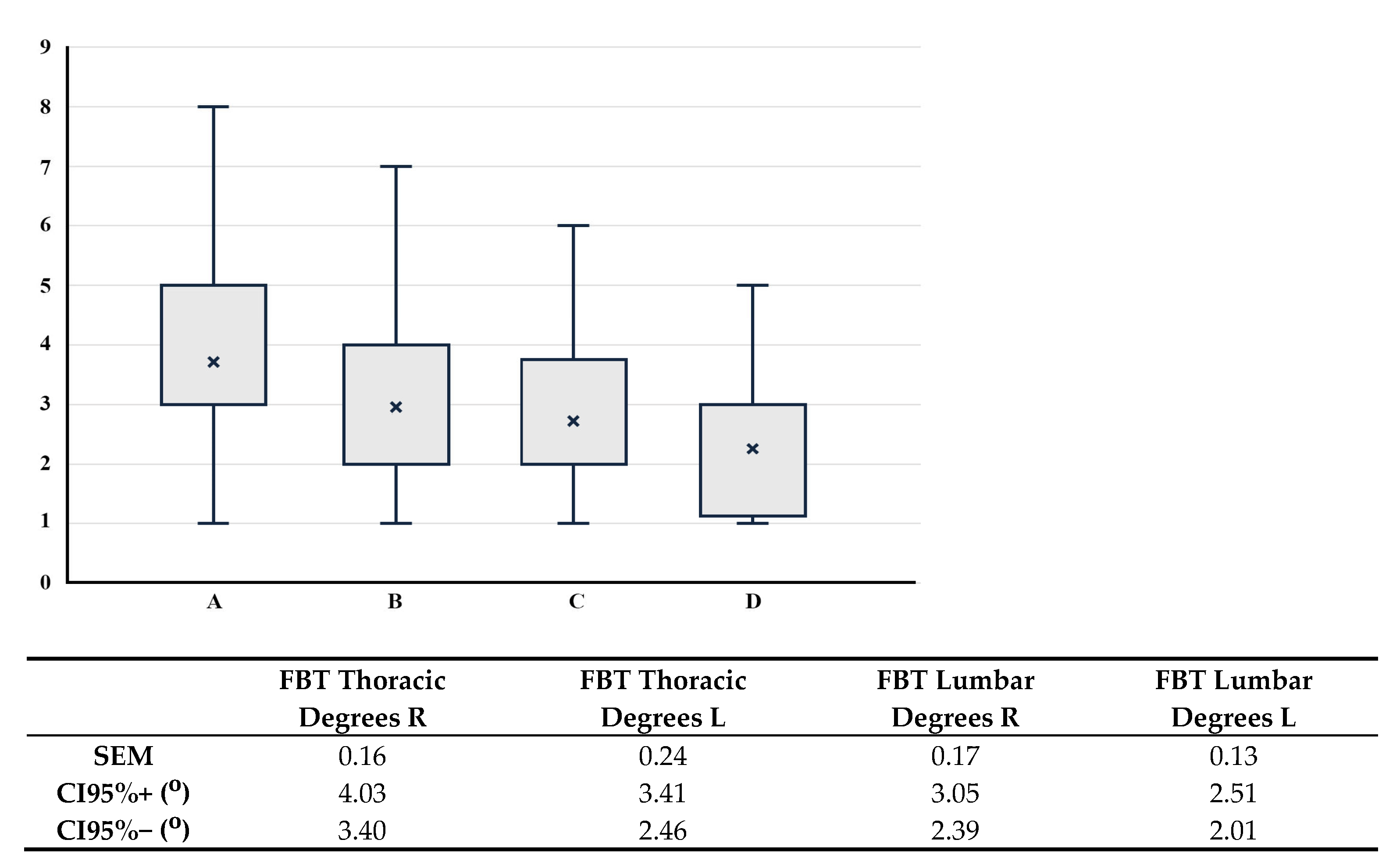
- Forward bending test with Scoliometer Measurement: During the prospective phase, rib prominences were quantified using a Scoliometer Osi 1995 (Baseline® Scoliometer. Fabrication Enterprises Inc., White Plains, NY, USA) [29] while subjects performed the FBT (Figure 4). In accordance with established clinical guidelines, scoliosis was suspected when vertebral rotation exceeded five degrees [5,8,22].
- -
- The scoliometer used was the Osi 1995 model to quantify vertebral rotation during FBT.
- -
- The examining physician underwent specialized training in scoliosis detection techniques.
- -
- Reliability testing was conducted, and the examiner achieved a high intraclass correlation coefficient (ICC > 0.90) for scoliometer measurements, ensuring measurement accuracy and reproducibility.
3. Results
3.1. Retrospective Study
3.2. Prospective Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grivas, T.B.; Vsiliadis, E.S.; Rodopoulos, G. Aetiology of idiopathic scoliosis. What have we learned from school screening? Stud. Health Technol. Inform. 2008, 140, 240–244. [Google Scholar] [PubMed]
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J. Child. Orthop. 2013, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.C.; Castelein, R.M.; Chu, W.C.; Danielsson, A.J.; Dobbs, M.B.; Grivas, T.B.; Gurnett, C.A.; Luk, K.D.; Moreau, A.; Newton, P.O.; et al. Adolescent Idiopathic Scoliosis. Nat. Rev. Dis. Primers 2015, 1, 15030. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force. Screening for adolescent idiopathic scoliosis: Policy statement. JAMA 1993, 269, 2664–2666. [Google Scholar] [CrossRef]
- Álvarez, L.I.; Nuñez, A. Escoliosis idiopática. Rev. Pediatr. Aten. Primaria 2011, 13, 135–146. [Google Scholar]
- Plaszewski, M.; Bettany-Saltikov, J. Are current scoliosis school screening recommendations evidence-based and up to date? A best evidence synthesis umbrella review. Eur. Spine J. 2014, 23, 2572–2585. [Google Scholar] [CrossRef]
- Li, X.K.; Wu, Z.G.; Wang, H.Q. Adolescent Idiopathic Scoliosis in China: An Ongoing Warm Debate from Bedside to Public. Spine 2016, 41, 369–370. [Google Scholar] [CrossRef]
- Altaf, F.; Gibson, A.; Dannawi, Z.; Noordeen, H. Adolescent idiopathic scoliosis. Bone Jt. Surg. 2013, 346, f2508. [Google Scholar] [CrossRef]
- Pesenti, S.; Jouve, J.L.; Morin, C.; Wolff, S.; De Gauzy, J.S.; Chalopin, A.; Ibnoulkhatib, A.; Polirsztok, E.; Walter, A.; Schuller, S.; et al. Evolution of adolescent idiopathic scoliosis: Results of a multicenter study at 20 years’ follow-up. Orthop. Traumatol. Surg. Res. 2015, 101, 619–622. [Google Scholar] [CrossRef]
- Labelle, H.; Richards, S.B.; De Kleuver, M.; Grivas, T.B.; Luk, K.D.K.; Wong, H.K.; Thometz, J.; Beauséjour, M.; Turgeon, I.; Fong, D.Y.T. Screening for adolescent idiopathic scoliosis: An information statement by the scoliosis research society international task force. Scoliosis 2013, 8, 17. [Google Scholar] [CrossRef]
- Workman, J.K.; Wilkes, J.; Presson, A.P.; Xu, Y.; Heflin, J.A.; Smith, J.T. Variation in Adolescent Idiopathic Scoliosis Surgery: Implications for Improving Healthcare Value. J. Pediatr. 2018, 195, 213–219.e3. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Effects of bracing in adolescents with idiopathic scoliosis. N. Eng. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Kluszczyński, M.; Zaborowska-Sapeta, K.; Kowalski, I.; Karpiel, I. The Effectiveness of Early Rehabilitation in Limiting the Progression of Idiopathic Scoliosis. J. Clin. Med. 2024, 13, 1422. [Google Scholar] [CrossRef]
- Richards, S.; Vitale, M.G. Screening in idiopathic Scoliosis in Adolescents. An information statement. J. Bone Jt. Surg. Am. 2008, 90, 195–198. [Google Scholar] [CrossRef]
- Grossman, D.C.; Curry, S.J.; Owens, D.K.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Screening for Adolescent Idiopathic Scoliosis: US Preventive Services Task Force Recommendation Statement. US Preventive Services Task Force. JAMA 2018, 319, 165–172. [Google Scholar]
- Screening for Adolescent Idiopathic Scoliosis: Position Statement. En: NHS. Available online: https://posna.org/POSNA/media/Documents/Position%20Statements/1122-Screening-for-the-Early-Detection-of-Idiopathic-Scoliosis-in-Adolescents.pdf (accessed on 27 March 2018).
- Goldbloom, R. Screening for Adolescent Idiopathic Scoliosis. En: Canadian Services Task Force. Available online: http://canadiantaskforce.ca/wp-content/uploads/2013/03/Chapter31_idio_adoles_scoliosis94.pdf?d2b9b5 (accessed on 27 March 2018).
- Wilkinson, J.; Bass, C.; Diem, S.; Gravley, A.; Harvey, L.; Maciosek, M.; McKeon, K.; Milteer, L.; Owens, J.; Rothe, P. Health Care Guideline. Preventive Services for Children and Adolescents; Institute for Clinical Systems Improvement (ICSI): Bloomington, MN, USA, 2013. [Google Scholar]
- Trobisch, P.; Suess, O.; Schwab, F. Idiopathic scoliosis. Dtsch. Arztebl. Int. 2011, 107, 875–883. [Google Scholar] [CrossRef]
- Zheng, Y.; Dang, Y.; Wu, X.; Yang, Y.; Reinhardt, J.; He, C.; Wong, M. Epidemiological study of adolescent idiopathic scoliosis in Eastern China. J. Rehabil. Med. 2017, 49, 512–519. [Google Scholar] [CrossRef]
- Santonja, F.; Andújar, P. Escoliosis. In Manual de Exploración Musculoesquelética; Santonja, F., Ed.; Panamericana: Madrid, Spain, 2022; pp. 23–34. [Google Scholar]
- Yufra, D.H.; Giordana, G. Escoliosis Idiopática del Adolescente en la Provincia de Jujuy. Chequeo Selectivo 2007–2009. Rev. Asoc. Argent. Ortop. Traumatol. 2011, 76, 211–223. [Google Scholar]
- Hernández, J.A.; Santonja, F.; García, I.; Ortiz, E. Prevalencia de la escoliosis idiopática en Murcia. Rev. Ortop. Traumatol. 1988, 32, 181–184. [Google Scholar]
- Lonstein, J.E.; Bjorklund, S.; Wanninger, M.H.; Nelson, R.P. Voluntary school screening for scoliosis in Minnesota. J. Bone Jt. Surg. 1982, 64, 481–488. [Google Scholar] [CrossRef]
- Espín Ríos, M.; Cervantes Pardo, A. Programa de Atención al Niño y al Adolescente: Guía de Apoyo al Programa; Consejería de Sanidad: Murcia, Spain, 2007; pp. 23–47. [Google Scholar]
- Navarro Alonso, J.A. Programa de Atención al Niño (PAN). In Región de Murcia; Consejería de Sanidad: Murcia, Spain, 1992; ISBN 84-87686. [Google Scholar]
- Côté, P.; Kreitz, B.G.; Cassidy, J.D.; Dzus, A.K.; Martel, J. A study of the diagnostic accuracy and reliability of the scoliometer and Adam’s forward bend test. Spine 1998, 23, 796–802. [Google Scholar] [CrossRef] [PubMed]
- Mittal, R.L.; Aggerwal, R.; Sarwal, A.K. School screening for scoliosiss in India. The evaluation of a scoliometer. Int. Orthop. 1987, 11, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Lonstein, J.; John, E. Point of View: Cut-off Point of the Scoliometer in School Scoliosis Screening. Spine 1997, 22, 1989. [Google Scholar] [CrossRef]
- Zurita Ortega, F.; Moreno Lorenzo, C.; Martínez Martínez, A.; Zurita Ortega, A.; Castro Sánchez, A.M. Cribado de la escoliosis en una población escolar de 8 a 12 años de la provincia de Granada. An. Pediatr. 2008, 69, 342–350. [Google Scholar] [CrossRef]
- Brooks, H.L.; Azen, S.P.; Gerberg, E.L. Scoliosis a prospective epidemiologycal study. J. Bone Jt. Surg. 1975, 57, 968–972. [Google Scholar] [CrossRef]
- Ostojic, Z.; Kristo, T.; Petrovic, P.; Vasilj, I.; Santic, Z. Prevalence of scoliosis in school-children from Mostar, Bosnia and Her-zegovina. Coll. Antropol. 2006, 30819, 59–64. [Google Scholar]
- Jenyo, M.S.; Asekun-Olarinmoye, E.O. Prevalence of scoliosis in secondary school children in Osogbo, Osun State, Nigeria. Afr. J. Med. Sci. 2005, 34, 361–364. [Google Scholar]
- Bunnell, W.P. Selective screening for scoliosis. Clin. Orthop. Relat. Res. 2005, 434, 40–45. [Google Scholar] [CrossRef]
- Daruwalla, J.S.; Balasubramaniam, P.; Chay, S.O.; Rajan, U.; Lee, H.P. Idiopathic scoliosis. Prevalence and ethnic distribution in Singapore schoolchildren. J. Bone Jt. Surg. 1985, 67, 182–184. [Google Scholar] [CrossRef]
- Navarro, J.A. Resultados de reconocimiento médico con el programa de salud escolar de la Región de Murcia. In Valoración Médico-Deportiva del Escolar; Santonja, F., Martínrz, I., Eds.; Secretariado de Publicaciones e Intercambio Científico, Universidad Murcia: Murcia, Spain, 1992; pp. 115–119. [Google Scholar]
- Komang-Agung, I.S.; Dwi-Purnomo, S.B.; Susilowati, A. Prevalence Rate of Adolescent Idiopathic Scoliosis: Results of School-based Screening in Surabaya, Indonesia Malays. Orthop. J. 2017, 11, 17–22. [Google Scholar]
- Weigert, K.P. Detection pattern and outcome assessment in adolescent idiopathic scoliosis. Dan. Med. Bull. 2006, 53, 217. [Google Scholar]
- Yong, F.; Wong, H.K.; Chow, K.Y. Prevalence of adolescent idiopathic scoliosis among female school children in Singapore. Ann. Acad. Med. 2009, 38, 1056–1063. [Google Scholar] [CrossRef]
- Chen, C.; Yu, R.; Xu, W.; Li, Z.; Li, Y.; Hu, R.; Zhu, X. A Practical Study of Diagnostic Accuracy: Scoliosis Screenings of Middle School Students by a Trained Nurse with a Smartphone Versus a Spine Surgeon with a Scoliometer. Spine 2020, 45, E266–E271. [Google Scholar] [CrossRef]
- Cárcamo, M.; Cárcamo, M.; Espinoza, P.; Rodas, M.; Urrejola, Ó.; Bettany-Saltikov, J.; Grivas, T.B. Prevalencia, riesgo de progresión y calidad de vida en estudiantes tamizados para escoliosis idiopática adolescente. Andes pediatr 2023, 94, 78–85. [Google Scholar] [CrossRef]
- Malfair, D.; Flemming, A.K.; Dvorak, M.F.; Munk, P.L.; Vertinsky, A.T.; Heran, M.K. Radiographic evaluation of scoliosis: Review. Am. J. Roentgenol. 2010, 194, S8–S22. [Google Scholar] [CrossRef]
- Chen, X.; Ye, Y.; Zhu, Z.; Zhang, R.; Wang, W.; Wu, M.; Lu, X.; Yan, B.; Liang, Q. Association between incorrect postures and curve magnitude of adolescent idiopathic scoliosis in China. J. Orthop. Surg. Res. 2024, 19, 300. [Google Scholar] [CrossRef]
- Dunn, J.; Henrikson, N.B.; Morrison, C.C.; Blasi, P.R.; Nguyen, M.; Lin, J.S. Screening for adolescent idiopathic scoliosis: A systematic evidence review for the U.S. Preventive Services Task Force. JAMA 2018, 319, 173–187. [Google Scholar] [CrossRef]
- British Orthopaedic Association and the British Scoliosis Society. School screening for scoliosis. Br. J. Med. 1983, 287, 963–964. [Google Scholar] [CrossRef][Green Version]
- Gammon, S.R.; Mehlman, C.T.; Chan, W.; Heifetz, J.; Durrett, G.; Wall, E.J. A Comparison of Thoracolumbosacral Orthoses and SpineCor Treatment of Adolescent Idiopathic Scoliosis Patients Using the Scoliosis Research Society Standardized Criteria. J. Pediatr. Orthop. 2010, 30, 531–538. [Google Scholar] [CrossRef]
- Burton, M.S. Diagnosis and treatment of adolescent idiopathic scoliosis. Pediatr. Ann. 2013, 42, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Ceballos-Laita, L.; Carrasco-Uribarren, A.; Cabanillas-Barea, S.; Pérez-Guillén, S.; Pardos-Aguilella, P.; Jiménez Del Barrio, S. The effectiveness of Schroth method in Cobb angle, quality of life and trunk rotation angle in adolescent idiopathic scoliosis: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2023, 59, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Hresko, M.T.; Talwalkar, V.; Schwend, R. Early Detection of Idiopathic Scoliosis in Adolescents. J. Bone Jt. Surg. Am. 2016, 98, e67. [Google Scholar] [CrossRef] [PubMed]
- Altaf, F.; Drinkwater, J.; Phan, K.; Cree, A.K. Systematic Review of School Scoliosis Screening. Spine Deform. 2017, 5, 303–309. [Google Scholar] [CrossRef]
- Sanabria, A.J.; Rigau, D.; Rotaeche, R.; Selva, A.; Marzo-Castillejo, M.; Alonso-Coello, P. Sistema GRADE: Metodología para la realización de recomendaciones para la práctica clínica. Aten. Primaria 2015, 47, 48–55. [Google Scholar] [CrossRef]
- Bras, J.; Prats, R. Actividades de prevención y promoción de la salud en la infancia y la adolescencia. In Atención Primaria Conceptos, Organización y Práctica Clínica, 6th ed.; Martín, A., Cano, J.F., Eds.; Elsevier: Barcelona, Spain, 2008; pp. 528–554. [Google Scholar]
- Vercauteren, M.; Van Beneden, M.; Verplaetse, R.; Croene, P.H.; Uyttendaele, D.; Verdonk, R. Trunk Asymmetries in a Belgian School Population. Spine 1982, 7, 555–562. [Google Scholar] [CrossRef]
- Luan, F.J.; Wan, Y.; Mak, K.C.; Ma, C.J.; Wang, H.Q. Cancer and mortality risks of patients with scoliosis from radiation exposure: A systematic review and meta-analysis. Eur. Spine J. 2020, 29, 3123–3134. [Google Scholar] [CrossRef]

| Interventions/Examinations | Age | |||
|---|---|---|---|---|
| Rotation Degrees | Thoracic Spine | Lumbar Spine | ||
| 0–3° | 37 | 29.1 (%) | 83 | 65.4 (%) |
| 4–5° | 72 | 56.7 (%) | 41 | 32.3 (%) |
| * 6–7° | 15 | 11.8 (%) | 1 | 0.8 (%) |
| * >7° | 3 | 2.4 (%) | 2 | 1.6 (%) |
| Total | 127 | 127 | ||
| Scoliometer ≤ 5° | Scoliometer > 5° | Total | ||
|---|---|---|---|---|
| Positive Adam’s test | 3 False positives | 1 True positives | 4 | Specificity 96.7% PPV 25% |
| Negative Adam’s test (Second and third stages) | 88 True negatives | 16 False negatives | 104 | Sensibility 5.9% NPV 84.6% |
| Total | 91 | 17 | 108 |
| Forward Bending Test | Scoliometer ≤ 5° | Scoliometer > 5° | Total | ||
|---|---|---|---|---|---|
| 2nd Stage | 3rd Stage | ||||
| Positive | Negative | 7 | 1 | 8 | |
| Negative | Positive | 11 | 0 | 11 | |
| Specificity | Sensibility | NPV | PPV | ||
| Positive | Negative | 90.7% | 10.5% | 85.2% | 16.7% |
| Negative | Positive | 87% | 5.3% | 83.9% | 6.7% |
| Thoracic FBT | Lumbar FBT | ||
|---|---|---|---|
| n | 13 | n | 15 |
| % | 10.3 | % | 11.9 |
| Mean degrees | 2.2 | Mean degrees | 2.3 |
| SD degrees | 0.8 | SD degrees | 0.9 |
| Thoracic FBT | Lumbar FBT | |||||
|---|---|---|---|---|---|---|
| Scap Prot R | Scap Prot L | No Scap Prot | Scap Prot R | Scap Prot L | No Scap Prot | |
| n | 45 | 62 | 12 | 38 | 63 | 11 |
| mean (°) | 3.78 | 3.13 | 3.58 | 1.71 | 2.48 | 2.36 |
| SD (°) | 1.80 | 1.02 | 1.78 | 0.61 | 0.98 | 0.67 |
| SEM (°) | 0.27 | 0.13 | 0.51 | 0.10 | 0.12 | 0.20 |
| IC95+ (°) | 4.30 | 3.38 | 4.59 | 1.90 | 2.72 | 2.76 |
| IC95− (°) | 3.25 | 2.88 | 2.58 | 1.52 | 2.23 | 1.97 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rios-de-Moya-Angeler, R.; Santonja-Medina, F.; Sanz-Mengibar, J.M.; Ríos-Bernabé, R.; Hurtado-Avilés, J.; Santonja-Renedo, F. Evaluation of a Primary Health Care Scoliosis Screening Program: A 9-Year Follow-Up Study. J. Clin. Med. 2025, 14, 3870. https://doi.org/10.3390/jcm14113870
Rios-de-Moya-Angeler R, Santonja-Medina F, Sanz-Mengibar JM, Ríos-Bernabé R, Hurtado-Avilés J, Santonja-Renedo F. Evaluation of a Primary Health Care Scoliosis Screening Program: A 9-Year Follow-Up Study. Journal of Clinical Medicine. 2025; 14(11):3870. https://doi.org/10.3390/jcm14113870
Chicago/Turabian StyleRios-de-Moya-Angeler, Rafael, Fernando Santonja-Medina, Jose Manuel Sanz-Mengibar, Rafael Ríos-Bernabé, José Hurtado-Avilés, and Fernando Santonja-Renedo. 2025. "Evaluation of a Primary Health Care Scoliosis Screening Program: A 9-Year Follow-Up Study" Journal of Clinical Medicine 14, no. 11: 3870. https://doi.org/10.3390/jcm14113870
APA StyleRios-de-Moya-Angeler, R., Santonja-Medina, F., Sanz-Mengibar, J. M., Ríos-Bernabé, R., Hurtado-Avilés, J., & Santonja-Renedo, F. (2025). Evaluation of a Primary Health Care Scoliosis Screening Program: A 9-Year Follow-Up Study. Journal of Clinical Medicine, 14(11), 3870. https://doi.org/10.3390/jcm14113870





