Effect of Photobiomodulation in Patients with Temporomandibular Dysfunction Refractory to Botulinum Toxin Treatment: A Non-Controlled Multicentric Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Registration
2.2. Patients: Inclusion and Exclusion Criteria
2.3. Assessment Tools
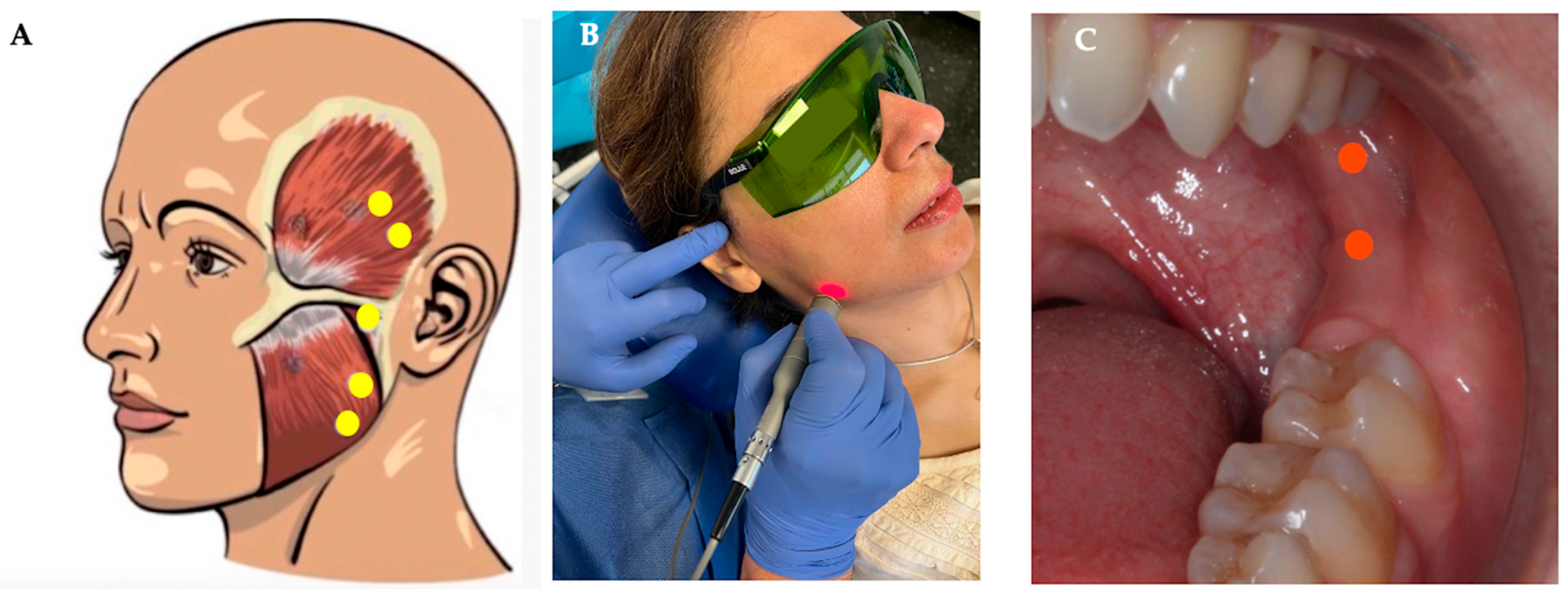
2.4. Treatments
2.5. Data Collection and Statistical Analysis
3. Results
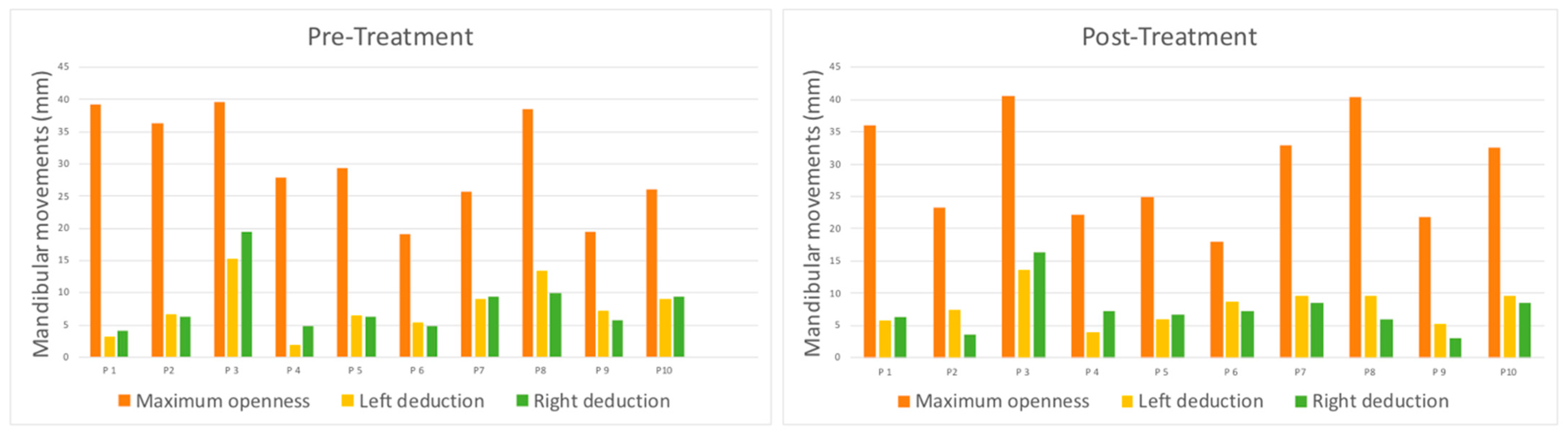
3.1. MMO
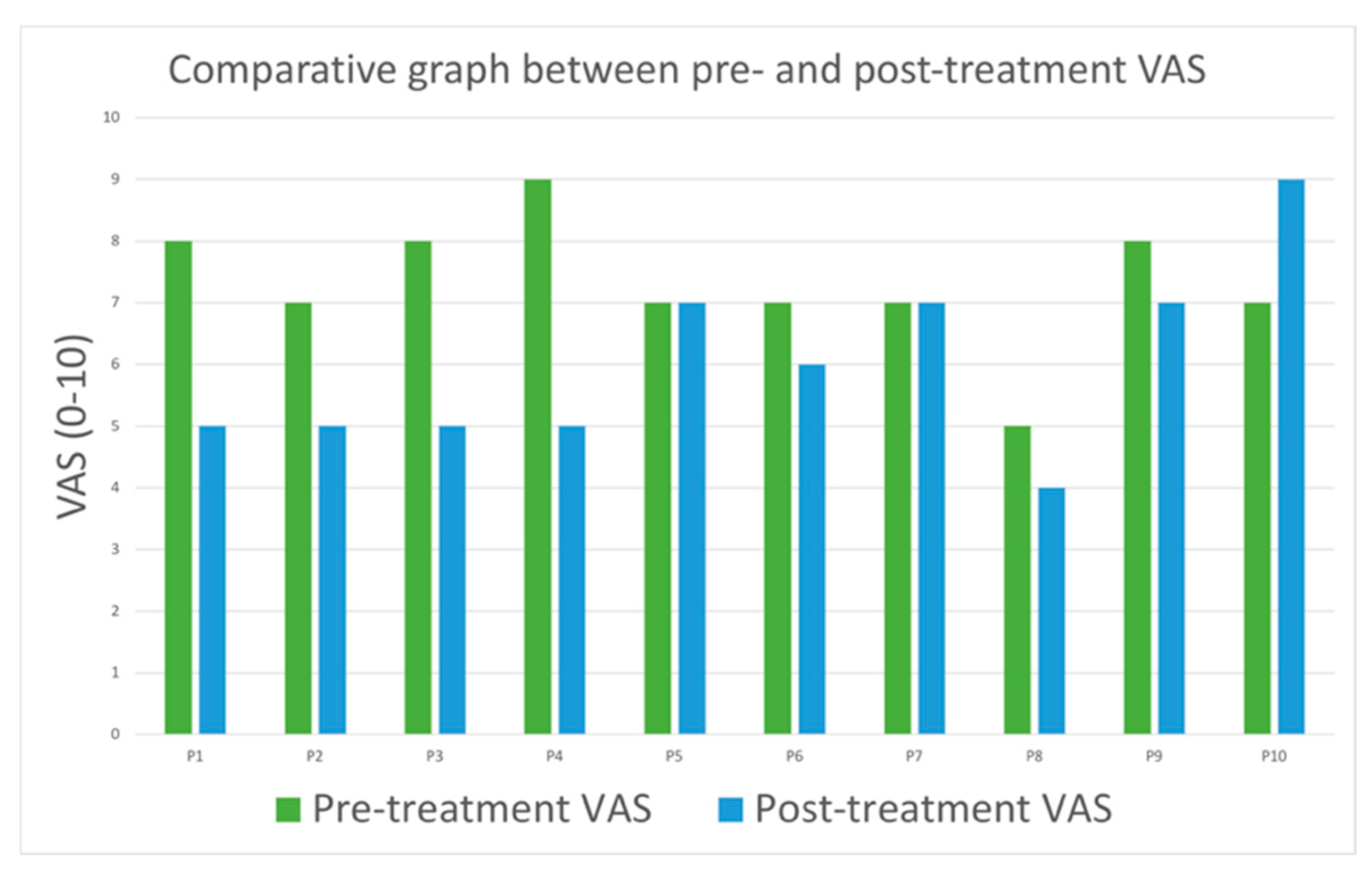
3.2. Pain in Masticatory Muscles
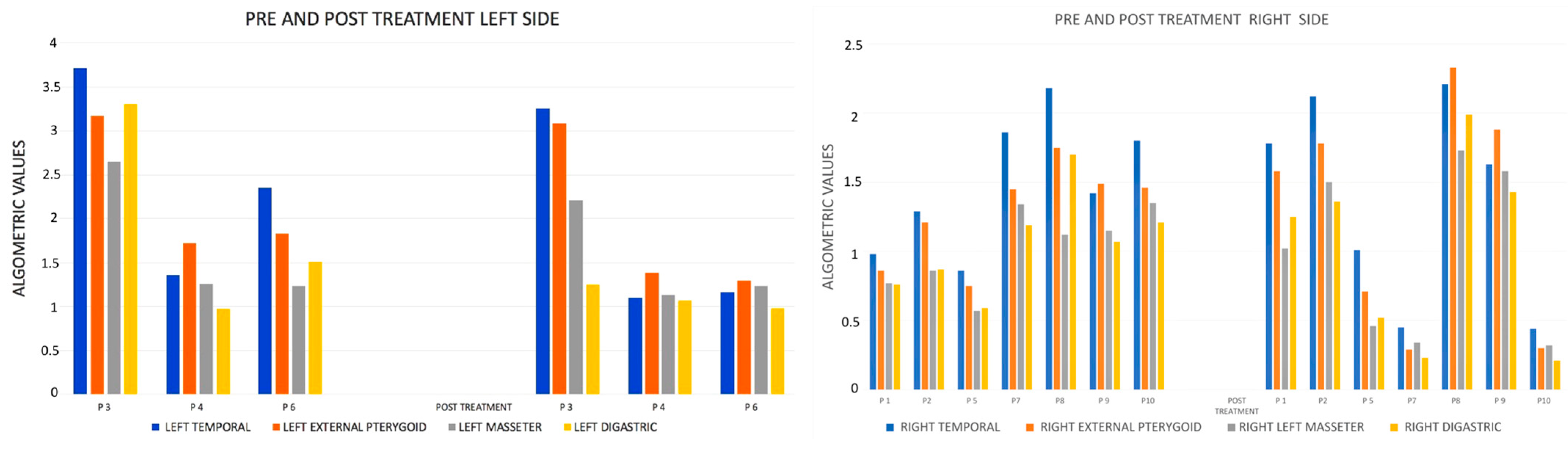
3.3. PP
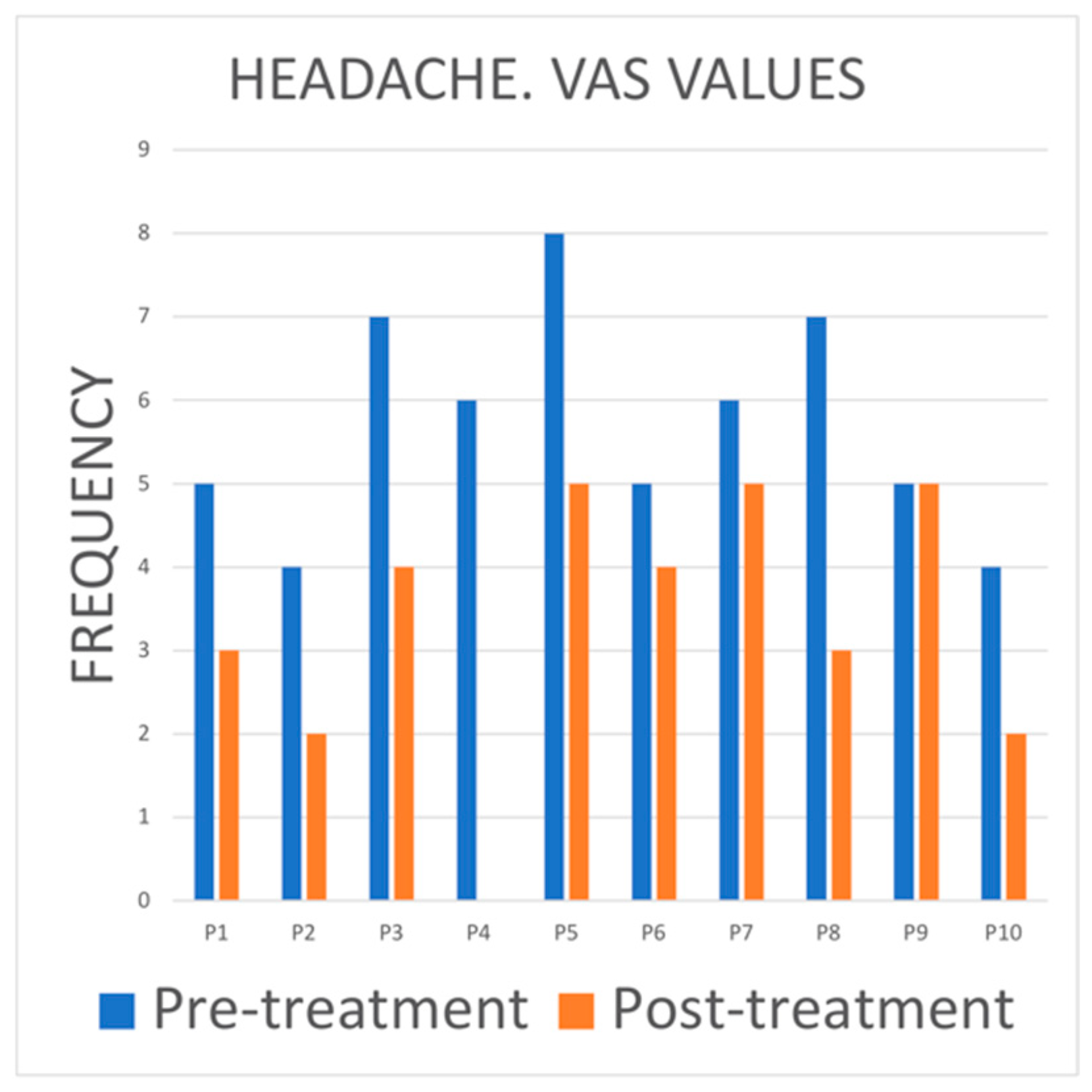
3.4. Headache
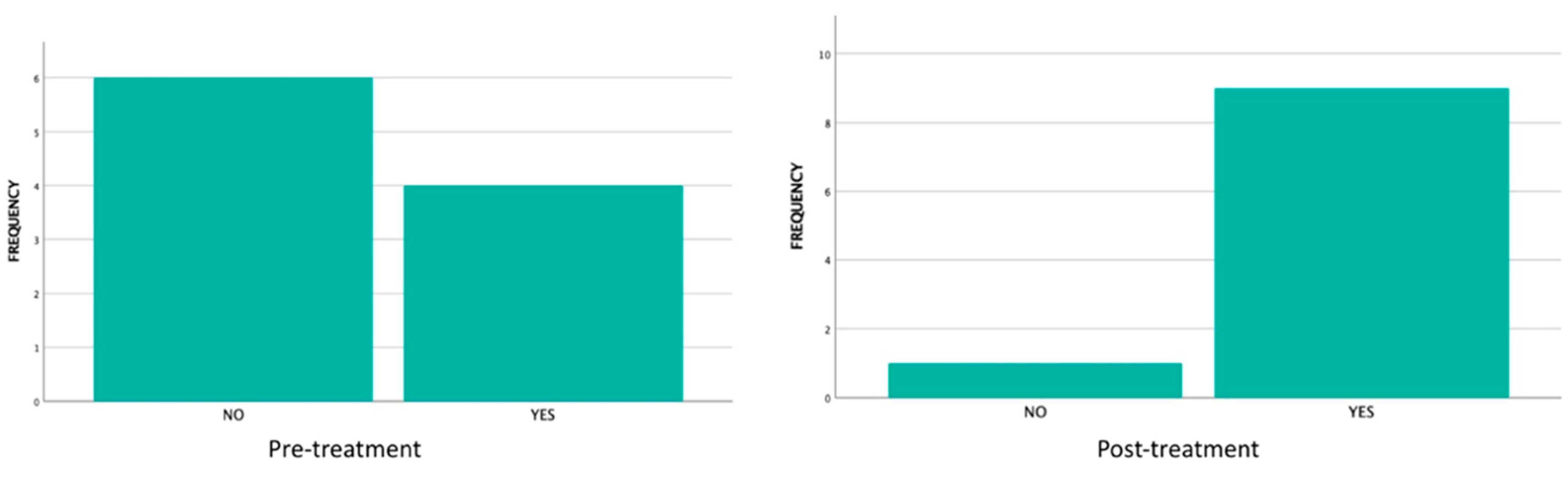
3.5. Clicks and Joint Noises
3.6. Likert Scale
3.7. Adverse Events
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TMD | Temporomandibular disorder |
| TMJs | Temporomandibular joints |
| BTX | Botulinum toxin |
| LLL | Low-level laser |
| PBMT | Photobiomodulation therapy |
| DASS-21 | Depression Anxiety Stress Scales-21 |
| VAS | Visual analog scale |
| PP | Pressure pain |
| MMO | Maximum mouth opening |
| RCT | Randomized controlled trial |
References
- Murphy, M.K.; MacBarb, R.F.; Wong, M.E.; Athanasiou, K.A. Temporomandibular disorders: A review of etiology, clinical management, and tissue engineering strategies. Int. J. Oral Maxillofac. Implant. 2013, 28, e393–e414. [Google Scholar] [CrossRef] [PubMed]
- Tran, C.; Ghahreman, K.; Huppa, C.; Gallagher, J.E. Management of temporomandibular disorders: A rapid review of systematic reviews and guidelines. Int. J. Oral Maxillofac. Surg. 2022, 51, 1211–1225. [Google Scholar] [CrossRef]
- Malgorzata, P.; Piotr, C.; Edward, K. The Mechanism of the Beneficial Effect of Botulinum Toxin Type a Used in the Treatment of Temporomandibular Joints Dysfunction. Mini Rev. Med. Chem. 2017, 17, 445–450. [Google Scholar] [CrossRef]
- Minakuchi, H.; Fujisawa, M.; Abe, Y.; Iida, T.; Oki, K.; Okura, K.; Tanabe, N.; Nishiyama, A. Managements of sleep bruxism in adult: A systematic review. Jpn. Dent. Sci. Rev. 2022, 58, 124–136. [Google Scholar] [CrossRef]
- Maiman, T.H. Stimulated Optical Radiation in Ruby. Nature 1960, 187, 493–494. [Google Scholar] [CrossRef]
- Anders, J.J.; Lanzafame, R.J.; Arany, P.R. Low-level light/laser therapy versus photobiomodulation therapy. Photomed. Laser Surg. 2015, 33, 183–184. [Google Scholar] [CrossRef]
- Singh, S.; Chakraborty, A.; Saju, A.R.; Singh, R.; Sen, A.; Shrinivas, S.; Surana, P. Comprehensive Review on Low-Level Laser Therapy in Dentistry. J. Pharm. Bioallied Sci. 2024, 16, S3047–S3049. [Google Scholar] [CrossRef]
- Alsarhan, J.; El Feghali, R.; Alkhudari, T.; Benedicenti, S.; Pasquale, C. Can Photobiomodulation Support the Management of Temporomandibular Joint Pain? Molecular Mechanisms and a Systematic Review of Human Clinical Trials. Photonics 2022, 9, 420. [Google Scholar] [CrossRef]
- de Sousa, D.F.M.; Malavazzi, T.C.D.S.; Deana, A.M.; Horliana, A.C.R.T.; Fernandes, K.P.S.; Bussadori, S.K.; Mesquita-Ferrari, R.A. Simultaneous red and infrared light-emitting diodes reduced pain in individuals with temporomandibular disorder: A randomized, controlled, double-blind, clinical trial. Lasers Med. Sci. 2022, 37, 3423–3431. [Google Scholar] [CrossRef]
- Osman, A.; Wong, J.L.; Bagge, C.L.; Freedenthal, S.; Gutierrez, P.M.; Lozano, G. The Depression Anxiety Stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. J. Clin. Psychol. 2012, 68, 1322–1338. [Google Scholar] [CrossRef]
- Stasiak, G.; Maracci, L.M.; de Oliveira Chami, V.; Pereira, D.D.; Tomazoni, F.; Bernardon Silva, T.; Ferrazzo, V.; Marquezan, M. TMD diagnosis: Sensitivity and specificity of the Fonseca Anamnestic Index. Cranio 2023, 41, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Thong, I.S.K.; Jensen, M.P.; Miró, J.; Tan, G. The validity of pain intensity measures: What do the NRS, VAS, VRS, and FPS-R measure? Scand. J. Pain 2018, 18, 99–107. [Google Scholar] [CrossRef]
- Jebb, A.T.; Ng, V.; Tay, L. A Review of Key Likert Scale Development Advances: 1995–2019. Front. Psychol. 2021, 12, 637547. [Google Scholar] [CrossRef] [PubMed]
- Butcher, N.J.; Monsour, A.; Mew, E.J.; Chan, A.W.; Moher, D.; Mayo-Wilson, E.; Terwee, C.B.; Chee-A-Tow, A.; Baba, A.; Gavin, F.; et al. Guidelines for Reporting Outcomes in Trial Reports: The CONSORT-Outcomes 2022 Extension. JAMA 2022, 328, 2252–2264. [Google Scholar] [CrossRef]
- Thabane, L.; Ma, J.; Chu, R.; Cheng, J.; Ismaila, A.; Rios, L.P.; Robson, R.; Thabane, M.; Giangregorio, L.; Goldsmith, C.H. A tutorial on pilot studies: The what, why and how. BMC Med. Res. Methodol. 2010, 10, 1. [Google Scholar] [CrossRef]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and analysis of pilot studies: Recommendations for good practice. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Rueda, J.A.; López-Valverde, A.; Márquez-Vera, A.; Méndez-Sánchez, R.; López-García, E.; López-Valverde, N. Preliminary Findings of the Efficacy of Botulinum Toxin in Temporomandibular Disorders: Uncontrolled Pilot Study. Life 2023, 13, 345. [Google Scholar] [CrossRef] [PubMed]
- Popescu, M.N.; Beiu, C.; Iliescu, C.A.; Racoviță, A.; Berteanu, M.; Iliescu, M.G.; Stănescu, A.M.A.; Radaschin, D.S.; Popa, L.G. Ultrasound-Guided Botulinum Toxin-A Injections into the Masseter Muscle for Both Medical and Aesthetic Purposes. Toxins 2024, 16, 413. [Google Scholar] [CrossRef]
- Petrucci, A.; Sgolastra, F.; Gatto, R.; Mattei, A.; Monaco, A. Effectiveness of low-level laser therapy in temporomandibular disorders: A systematic review and meta-analysis. J. Orofac. Pain 2011, 25, 298–307. [Google Scholar]
- Madani, A.; Ahrari, F.; Fallahrastegar, A.; Daghestani, N. A randomized clinical trial comparing the efficacy of low-level laser therapy (LLLT) and laser acupuncture therapy (LAT) in patients with temporomandibular disorders. Lasers Med. Sci. 2020, 35, 181–192. [Google Scholar] [CrossRef]
- Munguia, F.M.; Jang, J.; Salem, M.; Clark, G.T.; Enciso, R. Efficacy of Low-Level Laser Therapy in the Treatment of Temporomandibular Myofascial Pain: A Systematic Review and Meta-Analysis. J. Oral Facial Pain Headache 2018, 32, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Bueno, C.H.; Pereira, D.D.; Pattussi, M.P.; Grossi, P.K.; Grossi, M.L. Gender differences in temporomandibular disorders in adult populational studies: A systematic review and meta-analysis. J. Oral Rehabil. 2018, 45, 720–729. [Google Scholar] [CrossRef]
- Shaefer, J.R.; Holland, N.; Whelan, J.S.; Velly, A.M. Pain and temporomandibular disorders: A pharmaco-gender dilemma. Dent. Clin. N. Am. 2013, 57, 233–262. [Google Scholar] [CrossRef] [PubMed]
- Basili, M.; Barlattani, A., Jr.; Venditti, A.; Bollero, P. Low-level laser therapy in the treatment of muscle-skelet pain in patients affected by temporo-mandibular disorders. Oral Implantol. 2017, 10, 406–411. [Google Scholar] [CrossRef]
- Sancakli, E.; Gökçen-Röhlıg, B.; Balık, A.; Öngül, D.; Kıpırdı, S.; Keskın, H. Early results of low-level laser application for masticatory muscle pain: A double-blind randomized clinical study. BMC Oral Health 2015, 15, 131. [Google Scholar] [CrossRef]
- Baad-Hansen, L.; Pigg, M.; Yang, G.; List, T.; Svensson, P.; Drangsholt, M. Reliability of intra-oral quantitative sensory testing (QST) in patients with atypical odontalgia and healthy controls—A multicentre study. J. Oral Rehabil. 2015, 42, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Magri, L.V.; Carvalho, V.A.; Rodrigues, F.C.; Bataglion, C.; Leite-Panissi, C.R. Effectiveness of low-level laser therapy on pain intensity, pressure pain threshold, and SF-MPQ indexes of women with myofascial pain. Lasers Med. Sci. 2017, 32, 419–428. [Google Scholar] [CrossRef]
- Chen, J.; Huang, Z.; Ge, M.; Gao, M. Efficacy of low-level laser therapy in the treatment of TMDs: A meta-analysis of 14 randomised controlled trials. J. Oral Rehabil. 2015, 42, 291–299. [Google Scholar] [CrossRef]
- Aisaiti, A.; Zhou, Y.; Wen, Y.; Zhou, W.; Wang, C.; Zhao, J.; Yu, L.; Zhang, J.; Wang, K.; Svensson, P. Effect of photobiomodulation therapy on painful temporomandibular disorders. Sci. Rep. 2021, 11, 9049. [Google Scholar] [CrossRef]
- Zhang, Y.; Qian, Y.; Huo, K.; Liu, J.; Huang, X.; Bao, J. Efficacy of laser therapy for temporomandibular disorders: A systematic review and meta-analysis. Complement. Ther. Med. 2023, 74, 102945. [Google Scholar] [CrossRef]
- Xu, G.Z.; Jia, J.; Jin, L.; Li, J.H.; Wang, Z.Y.; Cao, D.Y. Low-Level Laser Therapy for Temporomandibular Disorders: A Systematic Review with Meta-Analysis. Pain Res. Manag. 2018, 2018, 4230583. [Google Scholar] [CrossRef]
- Del Vecchio, A.; Floravanti, M.; Boccassini, A.; Vestri, A.; Di Paolo, C.; Romeo, U. Evaluation of the efficacy of a new low-level laser therapy home protocol in the treatment of temporomandibular joint disorder-related pain: A randomized, double-blind, placebo-controlled clinical trial. Cranio 2021, 39, 141–150. [Google Scholar] [CrossRef]
- Plesh, O.; Adams, S.H.; Gansky, S.A. Temporomandibular joint and muscle disorder-type pain and comorbid pains in a national US sample. J. Orofac. Pain 2011, 25, 190–198. [Google Scholar]
- Gonçalves, D.A.; Camparis, C.M.; Franco, A.L.; Fernandes, G.; Speciali, J.G.; Bigal, M.E. How to investigate and treat: Migraine in patients with temporomandibular disorders. Curr. Pain Headache Rep. 2012, 16, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Chaves, T.C.; Dach, F.; Florencio, L.L.; Carvalho, G.F.; Gonçalves, M.C.; Bigal, M.E.; Speciali, J.G.; Bevilaqua-Grossi, D. Concomitant Migraine and Temporomandibular Disorders are Associated With Higher Heat Pain Hyperalgesia and Cephalic Cutaneous Allodynia. Clin. J. Pain 2016, 32, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Furquim, B.D.; Flamengui, L.M.; Conti, P.C. TMD and chronic pain: A current view. Dent. Press J. Orthod. 2015, 20, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Wänman, A.; Marklund, S. Treatment outcome of supervised exercise, home exercise and bite splint therapy, respectively, in patients with symptomatic disc displacement with reduction: A randomised clinical trial. J. Oral Rehabil. 2020, 47, 143–149. [Google Scholar] [CrossRef]
- Gazal, G. Overcoming temporomandibular joint clicking and pain. Cranio 2020, 38, 209–211. [Google Scholar] [CrossRef]
- Liu, L.; Chen, Q.; Lyu, T.; Zhao, L.; Miao, Q.; Liu, Y.; Nie, L.; Fu, F.; Li, S.; Zeng, C.; et al. Effect of acupuncture for temporomandibular disorders: A randomized clinical trial. QJM 2024, 117, 647–656. [Google Scholar] [CrossRef]
- Singh, B.P.; Singh, N.; Jayaraman, S.; Kirubakaran, R.; Joseph, S.; Muthu, M.S.; Jivnani, H.; Hua, F. Occlusal interventions for managing temporomandibular disorders. Cochrane Database Syst. Rev. 2024, 9, CD012850. [Google Scholar] [CrossRef]
- Eldridge, S.M.; Lancaster, G.A.; Campbell, M.J.; Thabane, L.; Hopewell, S.; Coleman, C.L.; Bond, C.M. Defining Feasibility and Pilot Studies in Preparation for Randomised Controlled Trials: Development of a Conceptual Framework. PLoS ONE 2016, 11, e0150205. [Google Scholar] [CrossRef] [PubMed]
- Ahmed Ali, U.; Ten Hove, J.R.; Reiber, B.M.; van der Sluis, P.C.; Besselink, M.G. Sample size of surgical randomized controlled trials: A lack of improvement over time. J. Surg. Res. 2018, 228, 1–7. [Google Scholar] [CrossRef] [PubMed]

| Device | Year | Type | Wavelength (nm) | Out Power (W) | Tip Area | Laser Dose per Session at Each Point | Exposure Time per Point/ Session | Total Laser Dose per Session | Total Laser Dose per Treatment (4 Sessions) | Total Energy (10 Patients) |
|---|---|---|---|---|---|---|---|---|---|---|
| Diode laser EPIC X (BIOLASE®) Stellahelz, Biolase, Spain | 2023 | Epic X | 940 nm | 0.9 W | 1.5 cm2 beam +/− tip | 10.0 J/cm2 | 17 s. | 105 J | 420 J | 4200 J |
| Gender | Age | Employment Status | Side Treated | Symptoms of TMDs (Fonseca Index) | DASS-21 | Joint Cracking | Headache | Pain |
|---|---|---|---|---|---|---|---|---|
| ♀ (100%) | 50 ± 11.2 years | Working 80% | Right side 70% | 100% | 10% mild anxiety | 90% | 40% | 80% |
| Mean | SD | t | p-Value | ||
|---|---|---|---|---|---|
| Pair 1 | Pre-maximum openness–post-maximum openness | 0.876 | 6.039 | 0.459 | 0.657 |
| Pair 2 | Pre-left diduction–post-left diduction | −0.219 | 2.226 | −0.311 | 0.763 |
| Pair 3 | Pre-right diduction–post-right diduction | 0.653 | 2.453 | 0.841 | 0.422 |
| Mean | SD | t | p-Value | ||
|---|---|---|---|---|---|
| Pair 1 | Pre-treatment and post-treatment | 2.400 | 1.713 | 4.431 | 0.002 * |
| Mean | SD | t | p-Value | ||
|---|---|---|---|---|---|
| Pair 1 | Left temporal pre- and post-treatment | 0.633 | 0.491 | 2.233 | 0.155 |
| Pair 2 | Left ext. pteryg. pre- and post-treatment | 0.320 | 0.220 | 2.512 | 0.129 |
| Pair 3 | Left masseter pre- and post-treatment | 0.190 | 0.226 | 1.456 | 0.238 |
| Pair 4 | Left digastric pre- and post-treatment | 0.826 | 1.105 | 1.295 | 0.325 |
| Mean | SD | t | p-Value | ||
|---|---|---|---|---|---|
| Pair 1 | Right temporal pre- and post-treatment | 0.107 | 0.926 | 0.306 | 0.770 |
| Pair 2 | Right ext. pteryg. pre- and post-treatment | 0.014 | 0.818 | 0.046 | 0.965 |
| Pair 3 | Right masseter pre- and post-treatment | 0.030 | 0.718 | 0.110 | 0.916 |
| Pair 4 | Right digastric pre- and post-treatment | 0.194 | 1.364 | −1.411 | 0.208 |
| Mean | SD | t | p-Value | ||
|---|---|---|---|---|---|
| Pair 1 | Pre-treatment and post-treatment | −0.500 | 0.527 | −3.000 | 0.015 * |
| Patients | Totally Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| 1 | x | ||||
| 2 | x | ||||
| 3 | x | ||||
| 4 | x | ||||
| 5 | x | ||||
| 6 | x | ||||
| 7 | x | ||||
| 8 | x | ||||
| 9 | - | - | - | - | - |
| 10 | x |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rueda, J.A.B.; López-Valverde, A.; Marquez-Vera, A.; Ferreira, N.d.R.; Macedo de Sousa, B.; López-Valverde, N. Effect of Photobiomodulation in Patients with Temporomandibular Dysfunction Refractory to Botulinum Toxin Treatment: A Non-Controlled Multicentric Pilot Study. J. Clin. Med. 2025, 14, 3778. https://doi.org/10.3390/jcm14113778
Rueda JAB, López-Valverde A, Marquez-Vera A, Ferreira NdR, Macedo de Sousa B, López-Valverde N. Effect of Photobiomodulation in Patients with Temporomandibular Dysfunction Refractory to Botulinum Toxin Treatment: A Non-Controlled Multicentric Pilot Study. Journal of Clinical Medicine. 2025; 14(11):3778. https://doi.org/10.3390/jcm14113778
Chicago/Turabian StyleRueda, José Antonio Blanco, Antonio López-Valverde, Antonio Marquez-Vera, Natàlia dos Reis Ferreira, Bruno Macedo de Sousa, and Nansi López-Valverde. 2025. "Effect of Photobiomodulation in Patients with Temporomandibular Dysfunction Refractory to Botulinum Toxin Treatment: A Non-Controlled Multicentric Pilot Study" Journal of Clinical Medicine 14, no. 11: 3778. https://doi.org/10.3390/jcm14113778
APA StyleRueda, J. A. B., López-Valverde, A., Marquez-Vera, A., Ferreira, N. d. R., Macedo de Sousa, B., & López-Valverde, N. (2025). Effect of Photobiomodulation in Patients with Temporomandibular Dysfunction Refractory to Botulinum Toxin Treatment: A Non-Controlled Multicentric Pilot Study. Journal of Clinical Medicine, 14(11), 3778. https://doi.org/10.3390/jcm14113778








