Discrepancy Between Vaccination Willingness and Actual SARS-CoV-2 Vaccination Status in People with Multiple Sclerosis: A Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Inclusion Criteria
2.2. Data Acquisition
- From June 2019 to June 2020 (baseline survey) [31];
- From May to July 2020 (first follow-up: approximately 3 months after the SARS-CoV-2 outbreak was declared a global pandemic, before vaccines against SARS-CoV-2 were available) [32];
- From October 2021 to January 2022 (second follow-up: approximately 1 year after the market entry of the first SARS-CoV-2 vaccines in Germany) [33].
2.2.1. Data Gathered Before the SARS-CoV-2 Outbreak (Baseline)
2.2.2. Data Collected Early in the SARS-CoV-2 Pandemic (First Follow-Up)
2.2.3. Data Collected After the Start of the SARS-CoV-2 Vaccination Campaign (Second Follow-Up)
2.3. Statistics
3. Results
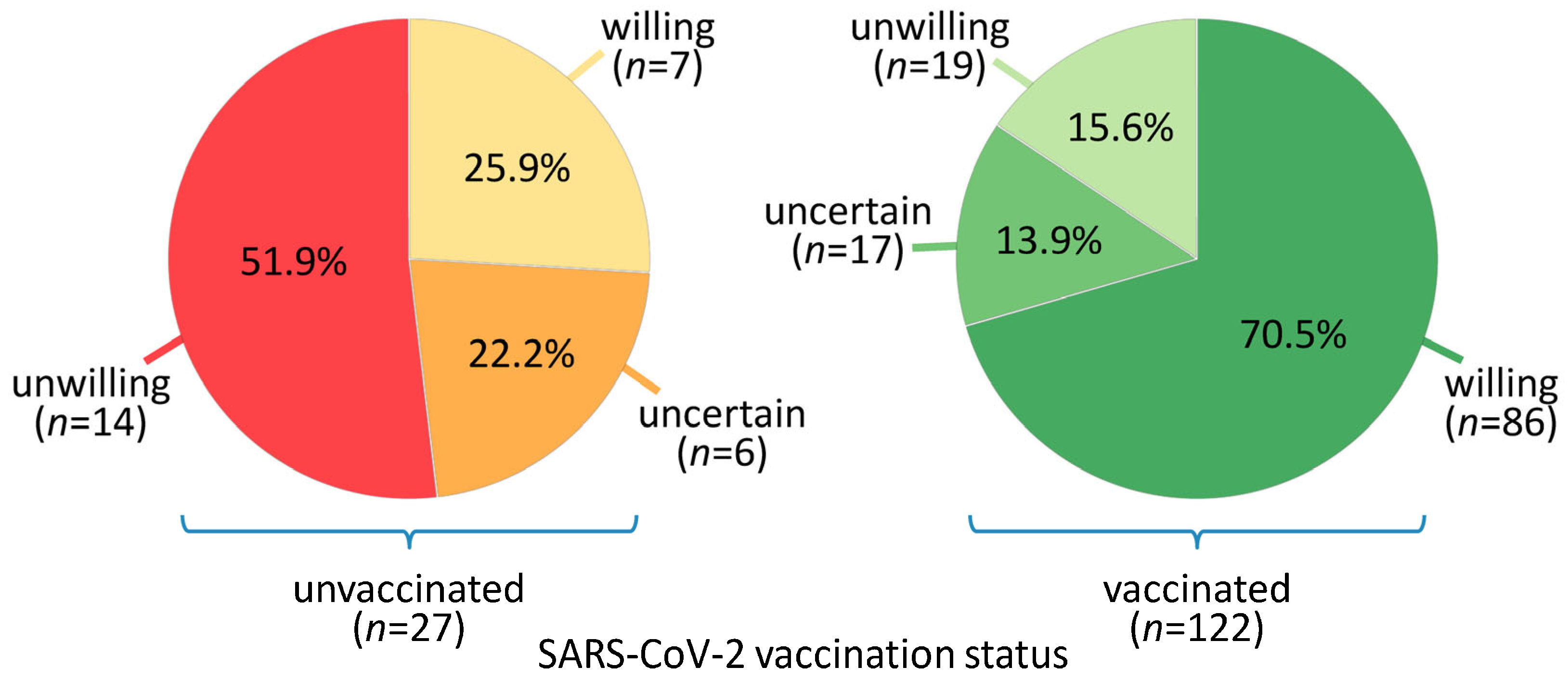
3.1. Patient Characteristics and Grouping of Patients According to Vaccination Willingness and Status
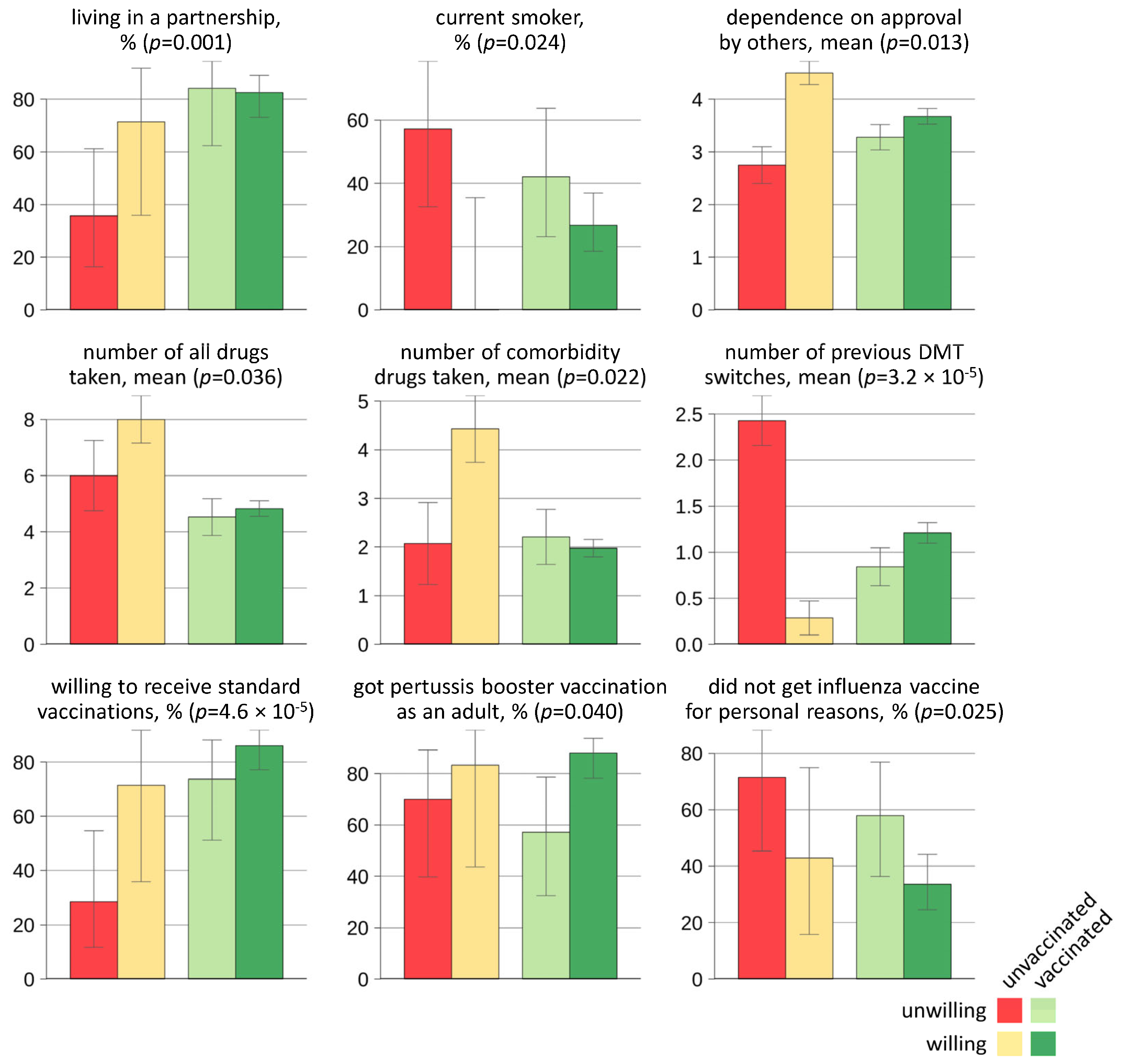
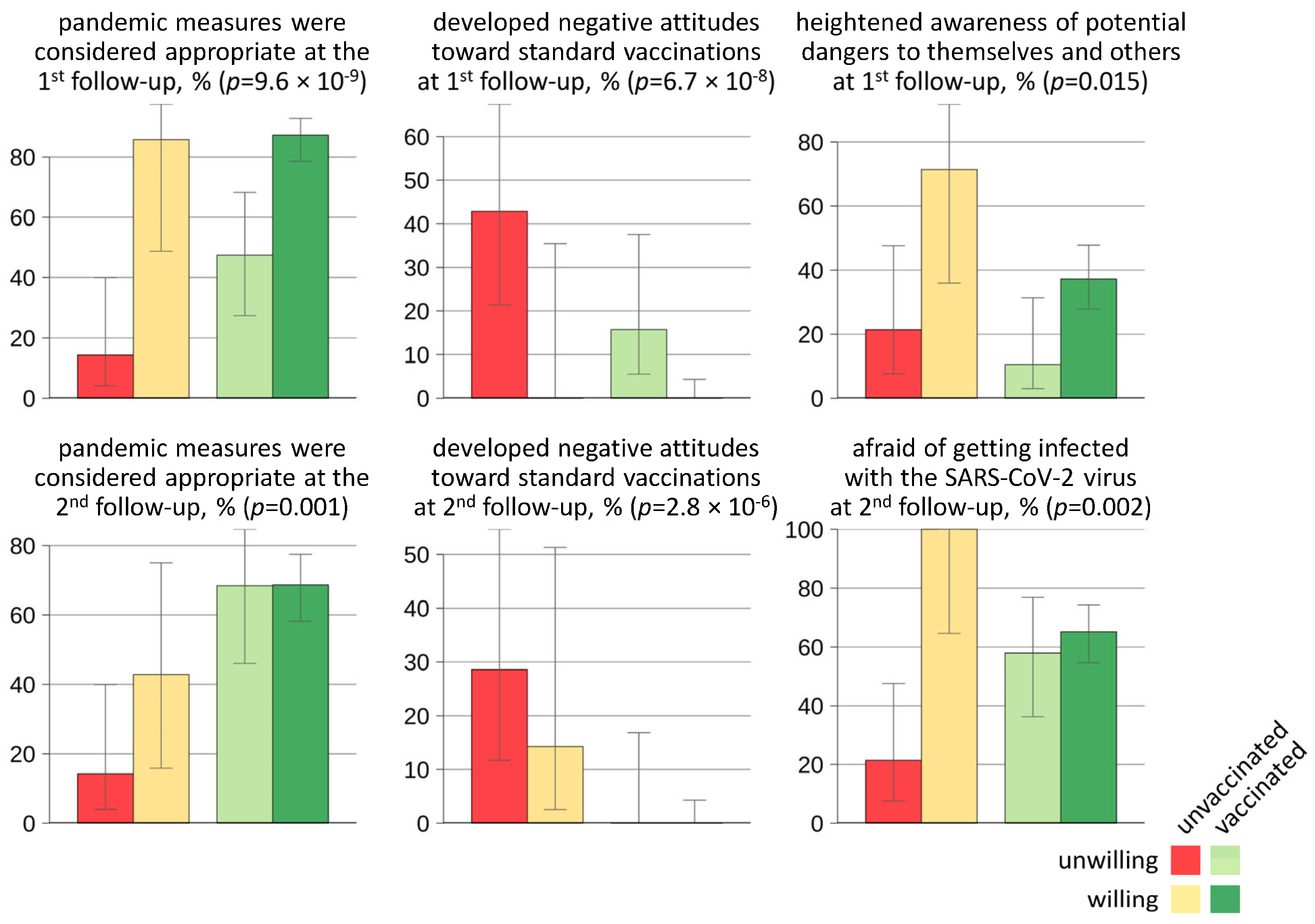
3.2. Factors Associated with Vaccination Willingness and/or Vaccination Status in Relation to SARS-CoV-2
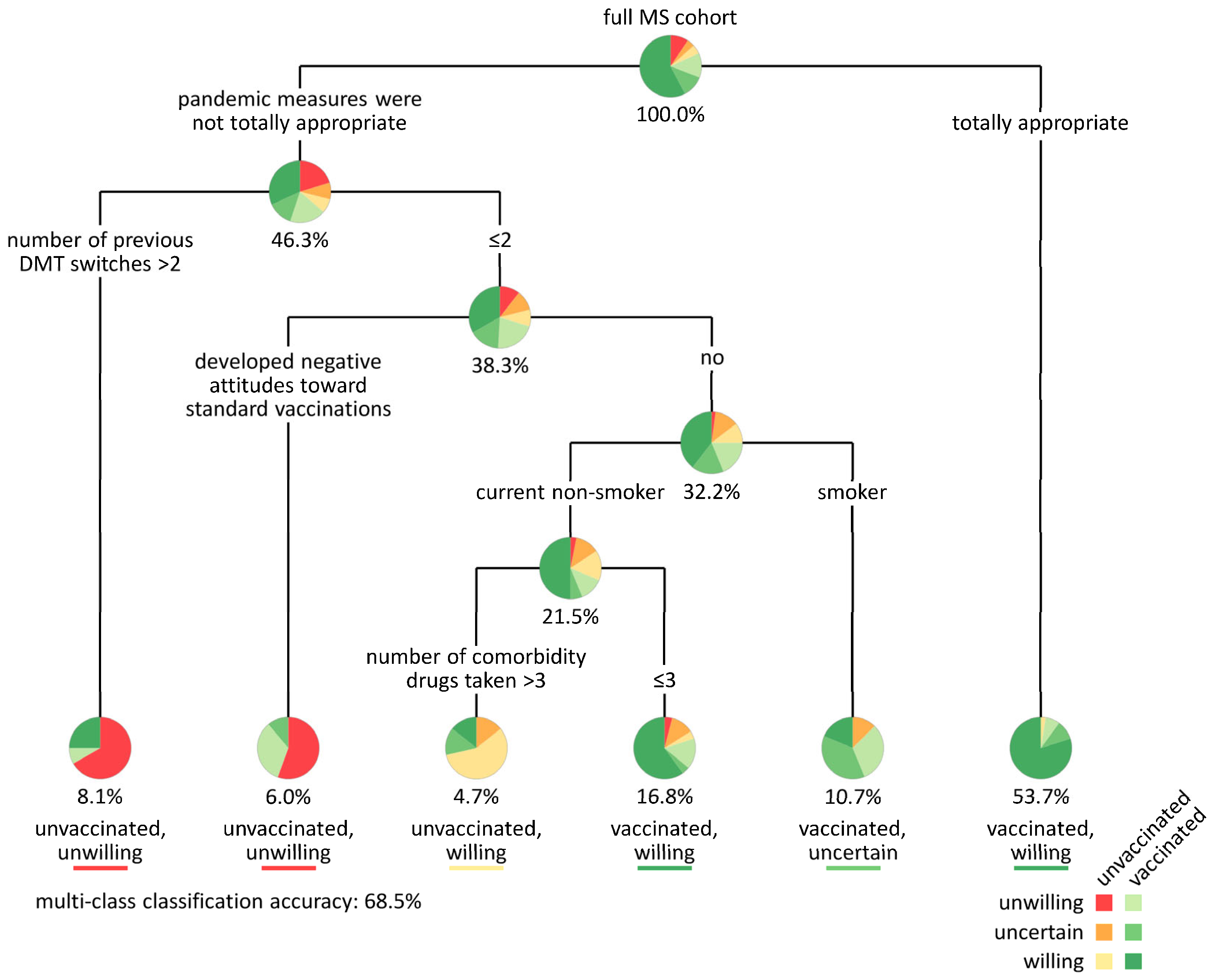
3.3. Classification of MS Patients According to SARS-CoV-2 Vaccination Willingness and Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| pwMS | People with Multiple Sclerosis |
| PTSD | Post-traumatic stress disorder |
| CIS | Clinically isolated syndrome |
| DMT | Disease-modifying therapy |
| EDSS | Expanded Disability Status Scale |
| MS | Multiple Sclerosis |
| PPMS | Primary progressive Multiple Sclerosis |
| RRMS | Relapsing-remitting Multiple Sclerosis |
| SD | Standard deviation |
| SPMS | Secondary progressive Multiple Sclerosis |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome type 2 |
References
- World Health Organization. COVID-19 Vaccines|WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/vaccines (accessed on 10 May 2025).
- Heidler, F.; Bopp, T.; Schwab, M.; Hoffmann, F.; Schild, H.; Kannler, M.; Pletz, M.; Zettl, U.K. Infektionen und Multiple Sklerose. Fortschr. Neurol. Psychiatr. 2024. [Google Scholar] [CrossRef] [PubMed]
- Reich, D.S.; Lucchinetti, C.F.; Calabresi, P.A. Multiple Sclerosis. N. Engl. J. Med. 2018, 378, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Filippi, M.; Bar-Or, A.; Piehl, F.; Preziosa, P.; Solari, A.; Vukusic, S.; Rocca, M.A. Multiple Sclerosis. Nat. Rev. Dis. Primers 2018, 4, 43. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of Multiple Sclerosis: 2017 Revisions of the McDonald Criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- Rommer, P.S.; Eichstädt, K.; Ellenberger, D.; Flachenecker, P.; Friede, T.; Haas, J.; Kleinschnitz, C.; Pöhlau, D.; Rienhoff, O.; Stahmann, A.; et al. Symptomatology and Symptomatic Treatment in Multiple Sclerosis: Results from a Nationwide MS Registry. Mult. Scler. 2019, 25, 1641–1652. [Google Scholar] [CrossRef]
- Winkelmann, A.; Loebermann, M.; Reisinger, E.C.; Hartung, H.-P.; Zettl, U.K. Disease-Modifying Therapies and Infectious Risks in Multiple Sclerosis. Nat. Rev. Neurol. 2016, 12, 217–233. [Google Scholar] [CrossRef]
- Leung, M.W.Y.; de Garde, E.M.W.V.; Uitdehaag, B.M.J.; Klungel, O.H.; Bazelier, M.T. The Relative Risk of Infection in People with Multiple Sclerosis Using Disease-Modifying Treatment: A Systematic Review of Observational Studies. Neurol. Sci. 2025, 46, 2555–2569. [Google Scholar] [CrossRef] [PubMed]
- Luna, G.; Alping, P.; Burman, J.; Fink, K.; Fogdell-Hahn, A.; Gunnarsson, M.; Hillert, J.; Langer-Gould, A.; Lycke, J.; Nilsson, P.; et al. Infection Risks Among Patients with Multiple Sclerosis Treated With Fingolimod, Natalizumab, Rituximab, and Injectable Therapies. JAMA Neurol. 2020, 77, 184. [Google Scholar] [CrossRef]
- Louapre, C.; Collongues, N.; Stankoff, B.; Giannesini, C.; Papeix, C.; Bensa, C.; Deschamps, R.; Créange, A.; Wahab, A.; Pelletier, J.; et al. Clinical Characteristics and Outcomes in Patients With Coronavirus Disease 2019 and Multiple Sclerosis. JAMA Neurol. 2020, 77, 1079–1088. [Google Scholar] [CrossRef]
- Dyczkowska, K.; Kalinowska-Łyszczarz, A. Navigating the Landscape of COVID-19 for Multiple Sclerosis Patients and Clinicians. Neurol. Neurochir. Pol. 2023, 57, 90–100. [Google Scholar] [CrossRef]
- Schiavetti, I.; Ponzano, M.; Signori, A.; Bovis, F.; Carmisciano, L.; Sormani, M.P. Severe Outcomes of COVID-19 among Patients with Multiple Sclerosis under Anti-CD-20 Therapies: A Systematic Review and Meta-Analysis. Mult. Scler. Relat. Disord. 2022, 57, 103358. [Google Scholar] [CrossRef] [PubMed]
- Etemadifar, M.; Nouri, H.; Maracy, M.R.; Akhavan Sigari, A.; Salari, M.; Blanco, Y.; Sepúlveda, M.; Zabalza, A.; Mahdavi, S.; Baratian, M.; et al. Risk Factors of Severe COVID-19 in People with Multiple Sclerosis: A Systematic Review and Meta-Analysis. Rev. Neurol. 2022, 178, 121–128. [Google Scholar] [CrossRef] [PubMed]
- National Multiple Sclerosis Society. Multiple Sclerosis and COVID-19. Available online: https://www.nationalmssociety.org/managing-ms/living-with-ms/diet-exercise-and-healthy-behaviors/vaccination/covid (accessed on 10 May 2025).
- Pawlitzki, M.; Zettl, U.K.; Ruck, T.; Rolfes, L.; Hartung, H.-P.; Meuth, S.G. Merits and Culprits of Immunotherapies for Neurological Diseases in Times of COVID-19. EBioMedicine 2020, 56, 102822. [Google Scholar] [CrossRef] [PubMed]
- Winkelmann, A.; Loebermann, M.; Barnett, M.; Hartung, H.-P.; Zettl, U.K. Vaccination and Immunotherapies in Neuroimmunological Diseases. Nat. Rev. Neurol. 2022, 18, 289–306. [Google Scholar] [CrossRef]
- Huang, Y.; Rodgers, W.J.; Middleton, R.M.; Baheerathan, A.; Tuite-Dalton, K.A.; Ford, D.V.; Nicholas, R.; Group, M.R.R. Willingness to Receive a COVID-19 Vaccine in People with Multiple Sclerosis—UK MS Register Survey. Mult. Scler. Relat. Disord. 2021, 55, 103175. [Google Scholar] [CrossRef]
- Uhr, L.; Mateen, F.J. COVID-19 Vaccine Hesitancy in Multiple Sclerosis: A Cross-Sectional Survey. Mult. Scler. 2021, 28, 135245852110306. [Google Scholar] [CrossRef]
- Wu, H.; Ward, M.; Brown, A.; Blackwell, E.; Umer, A. COVID-19 Vaccine Intent in Appalachian Patients with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2022, 57, 103450. [Google Scholar] [CrossRef]
- Day, D.; Grech, L.; Nguyen, M.; Bain, N.; Kwok, A.; Harris, S.; Chau, H.; Chan, B.; Blennerhassett, R.; Nott, L.; et al. Serious Underlying Medical Conditions and COVID-19 Vaccine Hesitancy: A Large Cross-Sectional Analysis from Australia. Vaccines 2022, 10, 851. [Google Scholar] [CrossRef]
- Nabavi, S.M.; Mehrabani, M.; Ghalichi, L.; Nahayati, M.A.; Ghaffari, M.; Ashtari, F.; Mohammadianinejad, S.E.; Karimi, S.; Faghani, L.; Yazdanbakhsh, S.; et al. COVID-19 Vaccination Willingness and Acceptability in Multiple Sclerosis Patients: A Cross Sectional Study in Iran. Vaccines 2022, 10, 135. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ten Health Issues WHO Will Tackle This Year. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 10 May 2025).
- Mayer, D.; Barun, B.; Lazibat, K.; Lasić, S.; Adamec, I.; Gabelić, T.; Krbot Skorić, M.; Habek, M. COVID-19 Vaccination Uptake in People with Multiple Sclerosis Compared to the General Population. Acta Neurol. Belg. 2023, 123, 2269–2275. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Proietti, F.; Landi, D.; Ponzano, M.; Cola, G.; Di Mauro, G.; Mataluni, G.; Nicoletti, C.G.; Curcio, G.; Marfia, G.A. COVID-19 Vaccine Hesitancy among Italian People with Multiple Sclerosis. Neurol. Sci. 2023, 44, 803–808. [Google Scholar] [CrossRef]
- Xiang, X.M.; Hollen, C.; Yang, Q.; Brumbach, B.H.; Spain, R.I.; Wooliscroft, L. COVID-19 Vaccination Willingness among People with Multiple Sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2021, 7, 205521732110171. [Google Scholar] [CrossRef]
- Yazdani, A.; Mirmosayyeb, O.; Ghaffary, E.M.; Hashemi, M.S.; Ghajarzadeh, M. COVID-19 Vaccines and Patients with Multiple Sclerosis: Willingness, Unwillingness and Hesitancy: A Systematic Review and Meta-Analysis. Neurol. Sci. 2022, 43, 4085–4094. [Google Scholar] [CrossRef]
- Streckenbach, B.; Baldt, J.; Heidler, F.; Frahm, N.; Langhorst, S.E.; Mashhadiakbar, P.; Burian, K.; Zettl, U.K.; Richter, J. General Vaccination Willingness and Current Vaccination Status in Relation to Clinical and Psychological Variables in Patients with Multiple Sclerosis. Vaccine 2022, 40, 3236–3243. [Google Scholar] [CrossRef] [PubMed]
- Heidler, F.; Baldt, J.; Frahm, N.; Langhorst, S.E.; Mashhadiakbar, P.; Streckenbach, B.; Zettl, U.K.; Richter, J. Vaccination Setting of Patients with Autoimmune Diseases in Times of Severe Acute Respiratory Syndrome Coronavirus Type 2 Pandemic Using the Example of Multiple Sclerosis Patients: A Longitudinal Multicenter Study. Eur. Neurol. 2021, 85, 104–111. [Google Scholar] [CrossRef]
- Burian, K.; Heidler, F.; Frahm, N.; Hecker, M.; Langhorst, S.E.; Mashhadiakbar, P.; Streckenbach, B.; Baldt, J.; Meißner, J.; Richter, J.; et al. Vaccination Status and Self-Reported Side Effects after SARS-CoV-2 Vaccination in Relation to Psychological and Clinical Variables in Patients with Multiple Sclerosis. Sci. Rep. 2024, 14, 12248. [Google Scholar] [CrossRef]
- Magyari, M.; Sorensen, P.S. Comorbidity in Multiple Sclerosis. Front. Neurol. 2020, 11, 851. [Google Scholar] [CrossRef] [PubMed]
- Kurtzke, J.F. Rating Neurologic Impairment in Multiple Sclerosis: An Expanded Disability Status Scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Sørensen, P.S.; Thompson, A.J.; Wolinsky, J.S.; Balcer, L.J.; Banwell, B.; Barkhof, F.; et al. Defining the Clinical Course of Multiple Sclerosis: The 2013 Revisions. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef]
- Frahm, N.; Hecker, M.; Zettl, U.K. Polypharmacy among Patients with Multiple Sclerosis: A Qualitative Systematic Review. Expert. Opin. Drug Saf. 2020, 19, 139–145. [Google Scholar] [CrossRef]
- Kanning, U. NEO-Fünf-Faktoren-Inventar Nach Costa Und McCrae (NEO-FFI). Z. Arb. Organ. 2009, 53, 194–198. [Google Scholar] [CrossRef]
- Costa, P.T. McCrae RR Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual; Psychological Assessment Resources: Odessa, Ukraine, 1992. [Google Scholar]
- Schwartz, E.S.; Chapman, B.P.; Duberstein, P.R.; Weinstock-Guttman, B.; Benedict, R.H.B. The NEO-FFI in Multiple Sclerosis: Internal Consistency, Factorial Validity, and Correspondence Between Self and Informant Reports. Assessment 2011, 18, 39–49. [Google Scholar] [CrossRef]
- Richter, J.; Eisemann, M.; Richter, G. Zur deutschsprachigen Version des Temperament- und Charakterinventars. Z. Klin. Psychol. Psychother. 2000, 29, 117–126. [Google Scholar] [CrossRef]
- Cloninger, C.R. A Psychobiological Model of Temperament and Character. Arch. Gen. Psychiatry 1993, 50, 975. [Google Scholar] [CrossRef]
- Fossati, A.; Cloninger, C.R.; Villa, D.; Borroni, S.; Grazioli, F.; Giarolli, L.; Battaglia, M.; Maffei, C. Reliability and Validity of the Italian Version of the Temperament and Character Inventory-Revised in an Outpatient Sample. Compr. Psychiatry 2007, 48, 380–387. [Google Scholar] [CrossRef]
- Farmer, R.F.; Goldberg, L.R. A Psychometric Evaluation of the Revised Temperament and Character Inventory (TCI-R) and the TCI-140. Psychol. Assess. 2008, 20, 281–291. [Google Scholar] [CrossRef]
- Pais Ribeiro, J.L.; Martins Da Silva, A.; Vilhena, E.; Moreira, I.; Santos, E.; Mendonça, D. The Hospital Anxiety and Depression Scale, in Patients with Multiple Sclerosis. Neuropsychiatr. Dis. Treat. 2018, 14, 3193–3197. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The Validity of the Hospital Anxiety and Depression Scale: An Updated Literature Review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Marrie, R.A.; Zhang, L.; Lix, L.M.; Graff, L.A.; Walker, J.R.; Fisk, J.D.; Patten, S.B.; Hitchon, C.A.; Bolton, J.M.; Sareen, J.; et al. The Validity and Reliability of Screening Measures for Depression and Anxiety Disorders in Multiple Sclerosis. Mult. Scler. Relat. Disord. 2018, 20, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Janssens, A.C.J.W.; van Doorn, P.A.; de Boer, J.B.; van der Meché, F.G.A.; Passchier, J.; Hintzen, R.Q. Impact of Recently Diagnosed Multiple Sclerosis on Quality of Life, Anxiety, Depression and Distress of Patients and Partners. Acta Neurol. Scand. 2003, 108, 389–395. [Google Scholar] [CrossRef]
- Marrie, R.A.; Patel, R.; Bernstein, C.N.; Bolton, J.M.; Graff, L.A.; Marriott, J.J.; Hitchon, C.A.; Figley, C.R.; Kornelsen, J.; Fisk, J.D. Anxiety and Depression Affect Performance on the Symbol Digit Modalities Test over Time in MS and Other Immune Disorders. Mult. Scler. 2021, 27, 1284–1292. [Google Scholar] [CrossRef]
- Walters, J.T.R.; Bisson, J.I.; Shepherd, J.P. Predicting Post-Traumatic Stress Disorder: Validation of the Trauma Screening Questionnaire in Victims of Assault. Psychol. Med. 2007, 37, 143–150. [Google Scholar] [CrossRef]
- Brewin, C.R. Systematic Review of Screening Instruments for Adults at Risk of PTSD. J. Trauma. Stress 2005, 18, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Brewin, C.R.; Rose, S.; Andrews, B.; Green, J.; Tata, P.; McEvedy, C.; Turner, S.; Foa, E.B. Brief Screening Instrument for Post-Traumatic Stress Disorder. Br. J. Psychiatry 2002, 181, 158–162. [Google Scholar] [CrossRef]
- Knipscheer, J.; Sleijpen, M.; Frank, L.; De Graaf, R.; Kleber, R.; Ten Have, M.; Dückers, M. Prevalence of Potentially Traumatic Events, Other Life Events and Subsequent Reactions Indicative for Posttraumatic Stress Disorder in the Netherlands: A General Population Study Based on the Trauma Screening Questionnaire. Int. J. Environ. Res. Public. Health 2020, 17, 1725. [Google Scholar] [CrossRef]
- Irizar, P.; Stevelink, S.A.M.; Pernet, D.; Gage, S.H.; Greenberg, N.; Wessely, S.; Goodwin, L.; Fear, N.T. Probable Post-Traumatic Stress Disorder and Harmful Alcohol Use among Male Members of the British Police Forces and the British Armed Forces: A Comparative Study. Eur. J. Psychotraumatol. 2021, 12, 1891734. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.A.L.; Colville, G.A.; Ramnarayan, P.; Woolfall, K.; Heward, Y.; Morrison, R.; Savage, A.; Fraser, J.; Griksaitis, M.J.; Inwald, D.P. Psychological Impact of Working in Paediatric Intensive Care. A UK-Wide Prevalence Study. Arch. Dis. Child. 2020, 105, 470–475. [Google Scholar] [CrossRef]
- Monschein, T.; Hartung, H.-P.; Zrzavy, T.; Barnett, M.; Boxberger, N.; Berger, T.; Chataway, J.; Bar-Or, A.; Rommer, P.S.; Zettl, U.K. Vaccination and Multiple Sclerosis in the Era of the COVID-19 Pandemic. J. Neurol. Neurosurg. Psychiatry 2021, 92, 1033–1043. [Google Scholar] [CrossRef]
- Robert Koch Institute. Empfehlungen Der STIKO. Available online: https://www.rki.de/DE/Themen/Infektionskrankheiten/Impfen/Staendige-Impfkommission/Empfehlungen-der-STIKO/empfehlungen-der-stiko-node.html (accessed on 10 May 2025).
- Grech, L.; Kwok, A.; Nguyen, M.; Winkel, A.; Butler, E.; Allan, M.; Bain, N.; Segelov, E.; on behalf of the MSVACCS Investigators. COVID-19 Vaccine Status, Intent, Hesitancy, and Disease-Related Beliefs in People with Multiple Sclerosis. Vaccines 2023, 11, 410. [Google Scholar] [CrossRef] [PubMed]
- Hernández-García, I.; Rodríguez-Montolio, J.; Almeida-Zurita, M.; Cheli-Gracia, D.; Sahuquillo, B.D.M.; Aibar-Remón, C.; Garcés-Redondo, M. COVID-19 Vaccination Coverage and Associated Factors in Patients with Multiple Sclerosis. Vaccines 2024, 12, 126. [Google Scholar] [CrossRef] [PubMed]
- Inojosa, H.; Schriefer, D.; Atta, Y.; Dillenseger, A.; Proschmann, U.; Schleußner, K.; Woopen, C.; Ziemssen, T.; Akgün, K. Insights from Real-World Practice: The Dynamics of SARS-CoV-2 Infections and Vaccinations in a Large German Multiple Sclerosis Cohort. Vaccines 2024, 12, 265. [Google Scholar] [CrossRef]
- Serrazina, F.; Sobral Pinho, A.; Cabral, G.; Salavisa, M.; Correia, A.S. Willingness to Be Vaccinated against COVID-19: An Exploratory Online Survey in a Portuguese Cohort of Multiple Sclerosis Patients. Mult. Scler. Relat. Disord. 2021, 51, 102880. [Google Scholar] [CrossRef]
- Moniz Dionísio, J.; Santos, M.; Rodrigues, A.M.; Rêgo, A.; Vítor, J.; Delgado, S.; Pinheiro, R.; Neves, P.; Figueiredo, C.; Costa, J.B.; et al. Opinions, Beliefs and Knowledge of People with Multiple Sclerosis on COVID-19 Pandemic and Vaccine. Mult. Scler. Relat. Disord. 2021, 54, 103113. [Google Scholar] [CrossRef]
- Yap, S.M.; Al Hinai, M.; Gaughan, M.; Callanan, I.; Kearney, H.; Tubridy, N.; McGuigan, C. Vaccine Hesitancy among People with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2021, 56, 103236. [Google Scholar] [CrossRef]
- Ziello, A.; Scavone, C.; Di Battista, M.E.; Salvatore, S.; Di Giulio Cesare, D.; Moreggia, O.; Allegorico, L.; Sagnelli, A.; Barbato, S.; Manzo, V.; et al. Influenza Vaccine Hesitancy in Patients with Multiple Sclerosis: A Monocentric Observational Study. Brain Sci. 2021, 11, 890. [Google Scholar] [CrossRef]
- Gerussi, V.; Peghin, M.; Palese, A.; De Martino, M.; Graziano, E.; Chiappinotto, S.; Fonda, F.; Bontempo, G.; Semenzin, T.; Martini, L.; et al. SARS-CoV-2 and Influenza Vaccine Hesitancy during the COVID-19 Pandemic in a Dynamic Perspective. Hum. Vaccines Immunother. 2024, 20, 2358565. [Google Scholar] [CrossRef] [PubMed]
- Boziki, M.; Styliadis, C.; Bakirtzis, C.; Grigoriadou, E.; Sintila, A.-S.; Nikolaidis, I.; Vrienniou, A.; Geys, L.; Pelidou, S.-H.; Probert, L.; et al. A National Representative, Cross-Sectional Study by the Hellenic Academy of NeuroImmunology (HEL.A.NI.) on COVID-19 and Multiple Sclerosis: Overall Impact and Willingness Toward Vaccination. Front. Neurol. 2021, 12, 757038. [Google Scholar] [CrossRef]
- Ehde, D.M.; Roberts, M.K.; Herring, T.E.; Alschuler, K.N. Willingness to Obtain COVID-19 Vaccination in Adults with Multiple Sclerosis in the United States. Mult. Scler. Relat. Disord. 2021, 49, 102788. [Google Scholar] [CrossRef]
- Ehde, D.M.; Roberts, M.K.; Humbert, A.T.; Herring, T.E.; Alschuler, K.N. COVID-19 Vaccine Hesitancy in Adults with Multiple Sclerosis in the United States: A Follow up Survey during the Initial Vaccine Rollout in 2021. Mult. Scler. Relat. Disord. 2021, 54, 103163. [Google Scholar] [CrossRef] [PubMed]
- Gad, A.H.E.; Ahmed, S.M.; Garadah, M.Y.A.; Dahshan, A. Multiple Sclerosis Patients’ Response to COVID-19 Pandemic and Vaccination in Egypt. Egypt. J. Neurol. Psychiatry Neurosurg. 2022, 58, 131. [Google Scholar] [CrossRef] [PubMed]
- Ghadiri, F.; Sahraian, M.A.; Saeedi, R.; Naser Moghadasi, A. Attitudes toward Vaccination in Patients with Multiple Sclerosis: A Report from Iran. Mult. Scler. Relat. Disord. 2021, 53, 103045. [Google Scholar] [CrossRef]
- Heidler, F.; Baldt, J.; Frahm, N.; Langhorst, S.E.; Mashhadiakbar, P.; Streckenbach, B.; Burian, K.; Zettl, U.K.; Richter, J. Vaccination Willingness in Association with Personality Traits in Patients with Multiple Sclerosis in the Course of SARS-CoV-2 Pandemic. Sci. Rep. 2022, 12, 15147. [Google Scholar] [CrossRef]
- Abbasi, N.; Ghadiri, F.; Moghadasi, A.N.; Azimi, A.; Navardi, S.; Heidari, H.; Karaminia, M.; Sahraian, M.A. COVID-19 Vaccine Hesitancy in Iranian Patients with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2022, 60, 103723. [Google Scholar] [CrossRef]
- Diem, L.; Friedli, C.; Chan, A.; Salmen, A.; Hoepner, R. Vaccine Hesitancy in Patients With Multiple Sclerosis: Preparing for the SARS-CoV-2 Vaccination Challenge. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e991. [Google Scholar] [CrossRef]
- Frahm, N.; Fneish, F.; Ellenberger, D.; Haas, J.; Loebermann, M.; Parciak, T.; Peters, M.; Pöhlau, D.; Rodgers, J.; Röper, A.-L.; et al. SARS-CoV-2 Vaccination in Patients with Multiple Sclerosis in Germany and the United Kingdom: Gender-Specific Results from a Longitudinal Observational Study. Lancet Reg. Health Eur. 2022, 22, 100502. [Google Scholar] [CrossRef]
- Purvis, R.S.; Moore, R.; Willis, D.E.; Hallgren, E.; McElfish, P.A. Factors Influencing COVID-19 Vaccine Decision-Making among Hesitant Adopters in the United States. Hum. Vaccines Immunother. 2022, 18, 2114701. [Google Scholar] [CrossRef] [PubMed]
- Oshio, T.; Kimura, H.; Nishizaki, T.; Kuwahara, S. Pre-Pandemic Social Isolation as a Predictor of the Adverse Impact of the Pandemic on Self-Rated Health: A Longitudinal COVID-19 Study in Japan. Prev. Med. 2022, 164, 107329. [Google Scholar] [CrossRef]
- Mhereeg, M.; Jones, H.; Kennedy, J.; Seaborne, M.; Parker, M.; Kennedy, N.; Akbari, A.; Zuccolo, L.; Azcoaga-Lorenzo, A.; Davies, A.; et al. COVID-19 Vaccination in Pregnancy: The Impact of Multimorbidity and Smoking Status on Vaccine Hesitancy, a Cohort Study of 25,111 Women in Wales, UK. BMC Infect. Dis. 2023, 23, 594. [Google Scholar] [CrossRef]
- Jackson, S.E.; Paul, E.; Brown, J.; Steptoe, A.; Fancourt, D. Negative Vaccine Attitudes and Intentions to Vaccinate Against Covid-19 in Relation to Smoking Status: A Population Survey of UK Adults. Nicotine Tob. Res. 2021, 23, 1623–1628. [Google Scholar] [CrossRef] [PubMed]
- Gilan, D.; Birkenbach, M.; Wossidlo, M.; Sprengholz, P.; Betsch, C.; Hahad, O.; Lieb, K. Fear of COVID-19 Disease and Vaccination as Predictors of Vaccination Status. Sci. Rep. 2023, 13, 8865. [Google Scholar] [CrossRef]
- Oniszczenko, W.; Turek, A. The Relationship between Fear of COVID-19 Infection, Fear of COVID-19 Vaccination and Big Five Personality Traits: A Mediation Model. Curr. Issues Personal. Psychol. 2023, 11, 1–10. [Google Scholar] [CrossRef]
- Mertens, G.; Lodder, P.; Smeets, T.; Duijndam, S. Fear of COVID-19 Predicts Vaccination Willingness 14 Months Later. J. Anxiety Disord. 2022, 88, 102574. [Google Scholar] [CrossRef]
- Statista. Impfquote Gegen das Coronavirus (COVID-19) in Deutschland nach Bundesländern (Stand: 5. März 2024). Available online: https://de.statista.com/statistik/daten/studie/1195108/umfrage/impfungen-gegen-das-coronavirus-je-einwohner-nach-bundeslaendern/ (accessed on 10 May 2025).
- United Nations. COVID-19 Making Worrying Comeback WHO Warns, Amid Summertime Surge. Available online: https://news.un.org/en/story/2024/08/1152866 (accessed on 10 May 2025).
- Epstein, S.; Xia, Z.; Lee, A.J.; Dahl, M.; Edwards, K.; Levit, E.; Longbrake, E.E.; Perrone, C.; Kavak, K.; Weinstock-Guttman, B.; et al. Vaccination Against SARS-CoV-2 in Neuroinflammatory Disease: Early Safety/Tolerability Data. Mult. Scler. Relat. Disord. 2022, 57, 103433. [Google Scholar] [CrossRef]
| Characteristic | Statistics |
|---|---|
| Age (years), mean ± SD | 48.4 ± 11.8 |
| Sex, n (%) | |
| Women | 96 (64.4) |
| Men | 53 (35.6) |
| Employment status, n (%) | |
| Full-time work | 42 (28.2) |
| Part-time work | 32 (21.5) |
| Unemployed | 5 (3.4) |
| Old-age pension | 9 (6.0) |
| Disability pension | 61 (40.9) |
| Partnership, n (%) | |
| No | 35 (23.5) |
| Yes | 114 (76.5) |
| Current smoker, n (%) | |
| No | 97 (65.1) |
| Yes | 52 (34.9) |
| Disease course, n (%) | |
| CIS | 8 (5.4) |
| RRMS | 95 (63.8) |
| SPMS | 36 (24.2) |
| PPMS | 10 (6.7) |
| Disease duration (years), median (range) | 10 (0–37) |
| EDSS score, median (range) | 3.5 (0.0–8.5) |
| Patient care, n (%) | |
| Outpatient | 122 (81.9) |
| Inpatient | 27 (18.1) |
| Comorbidities, n (%) | |
| 0 | 39 (26.2) |
| 1 | 28 (18.8) |
| ≥2 | 82 (55.0) |
| Number of drugs taken, n (%) | |
| 0 | 1 (0.7) |
| 1–4 | 71 (47.7) |
| 5–9 | 65 (43.6) |
| ≥10 | 12 (8.1) |
| DMT use, n (%) | |
| No | 32 (21.5) |
| Yes | 117 (78.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heidler, F.; Hecker, M.; Frahm, N.; Baldt, J.; Langhorst, S.E.; Mashhadiakbar, P.; Streckenbach, B.; Burian, K.; Richter, J.; Zettl, U.K. Discrepancy Between Vaccination Willingness and Actual SARS-CoV-2 Vaccination Status in People with Multiple Sclerosis: A Longitudinal Study. J. Clin. Med. 2025, 14, 3689. https://doi.org/10.3390/jcm14113689
Heidler F, Hecker M, Frahm N, Baldt J, Langhorst SE, Mashhadiakbar P, Streckenbach B, Burian K, Richter J, Zettl UK. Discrepancy Between Vaccination Willingness and Actual SARS-CoV-2 Vaccination Status in People with Multiple Sclerosis: A Longitudinal Study. Journal of Clinical Medicine. 2025; 14(11):3689. https://doi.org/10.3390/jcm14113689
Chicago/Turabian StyleHeidler, Felicita, Michael Hecker, Niklas Frahm, Julia Baldt, Silvan Elias Langhorst, Pegah Mashhadiakbar, Barbara Streckenbach, Katja Burian, Jörg Richter, and Uwe Klaus Zettl. 2025. "Discrepancy Between Vaccination Willingness and Actual SARS-CoV-2 Vaccination Status in People with Multiple Sclerosis: A Longitudinal Study" Journal of Clinical Medicine 14, no. 11: 3689. https://doi.org/10.3390/jcm14113689
APA StyleHeidler, F., Hecker, M., Frahm, N., Baldt, J., Langhorst, S. E., Mashhadiakbar, P., Streckenbach, B., Burian, K., Richter, J., & Zettl, U. K. (2025). Discrepancy Between Vaccination Willingness and Actual SARS-CoV-2 Vaccination Status in People with Multiple Sclerosis: A Longitudinal Study. Journal of Clinical Medicine, 14(11), 3689. https://doi.org/10.3390/jcm14113689







