Abstract
Background: Little is known about the impact of pre-injury OAC/APT on severely injured trauma patients admitted to a level I trauma center. Our study focused on impact of pre-injury OAC/APT on the outcomes of this specific cohort of patients. Methods: A retrospective cohort study on 356 severely injured trauma patients admitted to the resuscitation room in a level I trauma center between 2015 and 2020 was carried out. Results: Of the 356 patients, 20.5% (n = 73) were admitted with pre-injury OAC/APT. Falls from lower heights, categorized as low-energy trauma, were the primary mechanism of injury in patients with pre-injury OAC/APT. Patients with pre-injury OAC/APT were older (p < 0.001), had a higher proportion of severe traumatic brain injuries (TBI) (p < 0.001), and experienced significantly higher mortality rates during their hospital stay (60.3% vs. 15.9%; p < 0.001). There were significant correlations between pre-injury OAC/APT and advanced age (p < 0.001) as well as the severity of head injury (p < 0.001). Patients with pre-injury OAC/APT exhibited significantly higher mortality rates; especially in patients with pre-injury oral anticoagulation therapy. The highest mortality rates were observed in patients with isolated TBI and pre-injury OAC/APT. Conclusions: Trauma patients with pre-injury OAC/APT presented with advanced age and low-energy trauma as the main mechanism of injury. Pre-injury OAC/APT significantly correlated with advanced age and the severity of head injuries, and it may serve as an additional prognostic factor for the outcome of severely injured trauma patients.
1. Introduction
Over the past few decades, an increasing number of geriatric trauma patients have been documented [1,2,3]. Globally, the burden of cardiovascular diseases is consistent with the number of patients with oral anticoagulation (OAC) or antiplatelet therapy (APT), which is continuously increasing [4]. Little is known about the impact of pre-injury OAC or APT on the outcome of the severely injured patient arriving at the resuscitation room [5,6,7], despite the fact that injury-related factors such as the injury mechanism, older age, pre-existing comorbidities, and pre-injury medications were found to influence the outcome of polytrauma patients [8,9,10,11]. Overall, severely injured elderly patients seem to have higher mortality rates despite low-energy trauma mechanisms as the leading cause of injury [12]. Concomitant TBI seems to remain the predominant factor for the outcome of trauma patients [13,14]. When comparing trauma patients arriving in the resuscitation room, those with isolated traumatic brain injury (TBI) are significantly older and undergo considerably more neurosurgical interventions. Yet, there is no difference in mortality rates when compared to polytrauma patients with TBI [13]. The prognosis and prediction of mortality in trauma patients are essential factors in trauma care and depend on various aspects [15]. The hypothesis of our study was that severely injured trauma patients with pre-injury OAC or APT have worse outcomes with regard to mortality than severely injured trauma patients without pre-injury OAC or APT. We aimed to analyze the characteristics and the outcomes of severely injured trauma patients with pre-injury OAC or APT triaged to the resuscitation room and tried to answer the following questions:
- Are there any differences regarding the injury pattern or the clinical characteristics in trauma patients with pre-injury OAC/APT?
- Is the presence of pre-injury OAC/APT linked to the severity of TBI?
- Does pre-injury use of oral anticoagulants (OAC) or antiplatelet therapy (APT) affect the mortality rate of severely injured trauma patients admitted to the resuscitation room of a level I trauma center?
2. Materials and Methods
A retrospective study of adult, severely injured patients admitted to the resuscitation room in a level I trauma center was performed. Polytrauma (PT) patients with severe, multiple injuries (AIS ≥ 3 points in at least two body regions) and patients with isolated severe traumatic brain injury (iTBI) (head injury with an Abbreviated Injury Scale (AIS) ≥ 3 points) were enrolled starting from January 2015 to December 2020. Exclusion criteria were isolated severe injuries in any other body region, patients with minor injuries (ISS < 18 points), and patients < 18 years of age. Four hundred and three consecutive patients were included retrospectively. Of them, 47 patients needed to be excluded due to missing essential data (e.g., missing information about the pre-injury medication), leading to the remaining 356 patients (Figure 1).
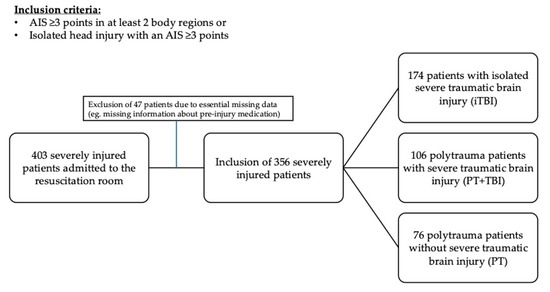
Figure 1.
Inclusion and classification of severely injured patients. AIS: abbreviated injury scale; iTBI: isolated traumatic brain injury; PT: polytrauma; TBI: traumatic brain injury.
The following demographic details were analyzed: sex, age, injury severity score (ISS), AIS, injury mechanism, pre-existing comorbidities, in-hospital complications, length of stay (LOS), and in-hospital mortality. Data were extracted from a consecutive in-hospital database of severely injured patients. The data records of all included patients were screened for pre-existing comorbidities and pre-injury OAC or APT. The primary outcome of interest was the influence of pre-injury OAC/APT on the survival rates during the hospital stay. Subanalyses were performed with regard to the different types of pre-injury medication (OAC or APT).
Statistical Analysis
Continuous variables are presented as means and standard deviation or medians and interquartile range (IQR) depending on their normal or skewed distribution. The Kolmogorov–Smirnov test was used to assess the normal distribution. The Mann–Whitney U or Student’s t-test was performed to compare categorical and continuous variables, and the chi-square test was used to compare qualitative variables. The contingency coefficient was used to detect a potential correlation between categorical variables, and the Spearman correlation coefficient was used for detecting a potential correlation between categorical and continuous variables. To assess potential multicollinearity of age, TBI, and pre-injury OAC/APT; the variance inflation factor (VIF) was calculated. The Kaplan–Meier method with a log-rank test was used for mortality analysis. A univariate Cox regression analysis was performed to detect a potential prognostic factor for survival. Only significant factors (p < 0.05) from the univariate analysis were included in the multivariate Cox regression analysis. All statistical analyses were performed using IBM Statistics Version 29.0 (SPSS Inc. Chicago, IL, USA).
3. Results
A total of 356 patients were enrolled consecutively, with half of them being trauma patients with isolated severe TBI (iTBI; n = 174; 48.9%) and half of them being polytrauma patients (n = 182; 51.1%) presenting either as polytrauma patients with severe head injury (PT+TBI; n = 106) or as polytrauma patients without severe head injury (PT; n = 76). Most patients were male (n = 245; 68.8%) with a median age of 51 years (IQR 39) and a median ISS of 29 points (IQR 11). One hundred and fifteen patients (32.3%) were defined as geriatric (>64 years of age). About 1/5 of all patients were admitted with active pre-injury OAC or APT (n = 73; 20.5%), with equal parts of them presenting with any APT (n = 37; 50.7%) or any OAC (n = 36; 49.3%). Most patients had pre-injury single APT (n = 31; 8.7%), followed by direct OAC (n = 16; 4.5%) and vitamin-K-dependent OAC (n = 15; 4.2%). Dual APT was recorded in six patients (1.7%), a combination of APT and OAC in three patients (0.8%) and two patients had other antithrombotic therapy (low molecular weight heparin (LMWH)). Pre-existing comorbidities were documented in 60.7% of patients (n = 216). The primary mechanism of injury was any traffic-related accident (TRA) in 35.7% of cases (n = 127), followed by falls from lesser height in 31.2% of cases (n = 111), falls from greater height (n = 50; 14.0%), penetrating injuries (n = 19; 5.3%) and other/unknown causes of injury (n = 49; 13.8%). A total of 89 patients (25.0%) died during the hospital stay, with 36 of them during the first 24 h and 53 of them after 24 h during the hospital stay.
Influence of OAC or APT
The characteristics of patients with OAC or APT are shown in Table 1.

Table 1.
Characteristics of severely injured patients. PT: polytrauma; TBI: traumatic brain injury; ISS: injury severity score; IQR: interquartile range. ° chi-square test. * Mann–Whitney U test.
The characteristics of severely injured patients with regard to pre-injury OAC/APT are listed in Table 1. Higher proportions of severe head injuries were documented in patients with pre-injury OAC/APT (p < 0.001) (Figure 2). Significant correlations of pre-injury OAC/APT with advanced age (p < 0.001; contingency coefficient 0.515) and the severity of head injury (p < 0.001; contingency coefficient 0.257) were seen. Age showed a significant correlation with a severe TBI (p < 0.001; Spearman correlation coefficient 0.573). The risk of a severe TBI showed an increase of 2% per year of aging (HR 1.020 95% CI 1.008–1.033 p = 0.002).
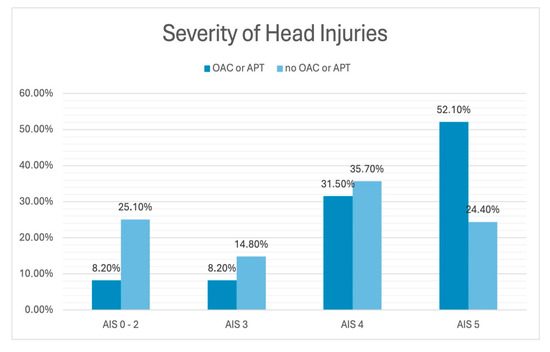
Figure 2.
Frequency of the severity of head injuries with and without pre-injury OAC/APT. OAC: oral anticoagulation; APT: antiplatelet therapy; AIS: abbreviated injury scale.
Kaplan–Meier analyses demonstrated the lowest survival rates in iTBI patients with pre-injury OAC/APT as well as in PT patients (with and without severe TBI) and pre-injury OAC/APT. In contrast, PT patients without pre-injury OAC/APT showed significantly higher survival rates (p < 0.001) (Figure 3). Patients with pre-injury OAC/APT tended to die more often after survival of the first 24 h (26 out of 44 in-hospital deaths; 59.1%). When compared to patients with APT, patients with pre-injury OAC therapy showed significantly higher mortality rates during the hospital stay (73.5% vs. 45.9%; p = 0.018) as well as after 24 h (50.0% vs. 24.3%; p = 0.025).
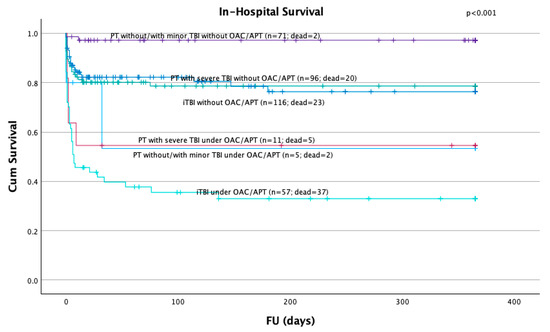
Figure 3.
Survival of all patients with significantly higher mortality rates in patients with isolated severe TBI followed by polytrauma patients with or without head injuries with pre-injury OAC/APT. OAC: oral anticoagulation; APT: antiplatelet therapy; PT: polytrauma; TBI: traumatic brain injury; iTBI: isolated traumatic brain injury.
Univariate Cox regression analysis revealed advanced age > 64 years, severe TBI, pre-existing comorbidities, and pre-injury OAC/APT as potential prognostic factors for survival. Multivariate analysis identified severe TBI and pre-injury OAC/APT as independent prognostic factors for the survival of severely injured trauma patients (Table 2).

Table 2.
Uni- and Multivariate Cox Regression Analysis on potential prognostic factors for the survival of severely injured trauma patients. OAC: oral anticoagulation; APT: anitplatelet therapy; TBI traumatic brain injury; HR hazard ratio; CI confidence interval.
4. Discussion
Although a significant decline in injury-related deaths has been seen in the 1990s [16,17], the mortality rates have remained relatively constant over the past decades [3]. Those rates might be related to the significant increase in the mean age of trauma patients and the known influence of advanced age on their survival [2,16,18]. Accordingly, a significant increase in comorbidities in trauma patients, especially in the elderly ones, has been observed with an expected increase in pre-injury OAC or APT [10,11]. Most patients who arrive at the resuscitation room present either as PT victims with/without severe TBI or as patients with isolated severe TBI, with little difference in the mortality rates among the three groups [13]. In this study, we aimed to see whether pre-injury use of OAC/APT influences the outcome (defined as in-hospital mortality) on these three groups.
Initially, we observed a significant proportion of severe trauma patients with pre-injury OAC/APT who were admitted to the resuscitation room (one-fifth of all trauma patients). This specific group of patients showed some distinctive clinical characteristics: they presented with a significantly higher median age and showed distinctive injury mechanisms reflecting the advanced age and potential frailty. Most trauma patients with pre-injury OAC/APT were admitted after falls from lesser height as a low-energy injury pattern. In contrast to that, trauma patients without pre-injury OAC/APT were mainly admitted after traffic-related accidents. Despite known injury-related predictors such as type and site of injury, as well as injury severity [11,19,20,21,22,23,24]; advanced age, pre-existing comorbidities, and pre-injury medications were found to have a potential influence on the outcome of polytrauma patients previously [9].
The rates of head injuries increased, particularly among the elderly group of trauma patients [25]. As severe TBI and advanced age are significant prognostic factors for the outcomes of severely injured trauma patients (27), we sought to explore a potential correlation between advanced age, the presence of severe TBI, and pre-injury OAC/APT. We demonstrated that patients with pre-injury OAC/APT appeared significantly more frequently in iTBI patients. Additionally, pre-injury OAC/APT was significantly linked to the severity of head injuries and with advanced age. Age itself showed a significant correlation with the occurrence of severe TBI. Overall, there appears to be a strong relationship between advanced age, OAC/APT intake, and the incidence of severe head injuries in trauma patients.
With regard to the outcome of our patients with pre-injury OAC/APT, those with pre-injury OAC/APT showed the highest mortality rates irrespective of the type of trauma (iTBI or PT). Despite the significant higher mortality rate of patients with pre-injury OAC/APT, the injury severity was similar in both groups. This finding indicates the diminished ability of the ISS to underline singular injuries with major influence on the outcome such as severe head injuries. After multivariate analyses, severe TBI and pre-injury OAC/APT remained independent prognostic factors on the survival of our trauma patients. We demonstrated that with advanced age, the risk of experiencing a severe head injury increases significantly (2% per year of aging). Both severe TBI and pre-injury OAC/APT were closely associated with advanced age, showing a significant correlation between pre-injury OAC/APT and both advanced age and the severity of the head injury. An early detection of potential pre-injury OAC/APT in the elderly trauma patient might be beneficial and potentially should be implemented in specific trauma protocols for the elderly. This might lead to an early initiation of reversal agents and might reduce the severity of head injuries in the elderly leading to a better outcome in this specific cohort of patients.
Overall, the combination of concomitant TBI, advanced age, and pre-injury OAC/APT appears to be the primary factor influencing the outcomes of trauma patients transferred to the resuscitation room.
This study has the characteristic limitations of retrospective, single-center registry data and post hoc analyses with a relatively small sample size. No data on functional outcome or quality-of-life parameters were available. Despite careful data analysis and consecutive inclusion of patients, there might be an inherent selection bias. No data regarding the adherence of OAC/APT, the dosage of the medications or the activity of the drugs were available. Further studies focusing on severely injured patients on OAC/APT are needed with the implementation of prospective trials and specific protocols. Still, little is known about the clinical impact of point of care blood tests and potential reversal of pre-injury OAC/APT in severely injured patients.
5. Conclusions
Severely injured trauma patients with pre-injury OAC/APT display distinctive clinical characteristics, showing advanced age and low-energy trauma as the primary mechanisms of injury. Pre-injury OAC/APT closely correlates with advanced age and the severity of head injuries. Alongside severe TBI, pre-injury OAC/APT appears to be an independent predictor of survival for severely injured trauma patients.
Author Contributions
Conceptualization, V.W., A.A., S.F. and L.L.N.; methodology, V.W.; formal analysis, V.W., S.F., and A.A.; data curation, V.W., S.F. and S.A.; writing—original draft preparation, V.W., A.A. and L.L.N.; writing—review and editing, S.F., S.A., S.H. and L.L.N.; supervision, L.L.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the Medical University of Vienna (1945/2022; approved 23 January 2023).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of this study and the use of anonymized data. There were no risks for the included patients and a sufficient protection of the confidentiality of data.
Data Availability Statement
The datasets generated and analyzed in the current manuscript are not publicly available due to data protection regulations. The data used and analyzed in this study are available from the corresponding author solely upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| OAC | Oral anticoagulation |
| APT | Antiplatelet therapy |
| TBI | Traumatic brain injury |
| PT | Polytrauma |
| iTBI | Isolated traumatic brain injury |
| AIS | Abbreviated injury scale |
| ISS | Injury severity score |
| LOS | Length of stay |
| IQR | Interquartile range |
| TRA | Traffic-related accident |
| HR | Hazard ratio |
| CI | Confidence interval |
References
- Lowe, J.A.; Pearson, J.; Leslie, M.; Griffin, R. Ten-Year Incidence of High-Energy Geriatric Trauma at a Level 1 Trauma Center. J. Orthop. Trauma 2018, 32, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Kalbas, Y.; Lempert, M.; Ziegenhain, F.; Scherer, J.; Neuhaus, V.; Lefering, R.; Teuben, M.; Sprengel, K.; Pape, H.C.; Jensen, K.O.; et al. A retrospective cohort study of 27,049 polytraumatized patients age 60 and above: Identifying changes over 16 years. Eur. Geriatr. Med. 2022, 13, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Weihs, V.; Frenzel, S.; Dedeyan, M.; Hruska, F.; Staats, K.; Hajdu, S.; Negrin, L.L.; Aldrian, S. 25-Year experience with adult polytraumatized patients in a European level 1 trauma center: Polytrauma between 1995 and 2019. What has changed? A retrospective cohort study. Arch. Orthop. Trauma Surg. 2022, 143, 2409–2415. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Boltz, M.M.; Podany, A.B.; Hollenbeak, C.S.; Armen, S.B. Injuries and outcomes associated with traumatic falls in the elderly population on oral anticoagulant therapy. Injury 2015, 46, 1765–1771. [Google Scholar] [CrossRef]
- Feeney, J.M.; Neulander, M.; DiFiori, M.; Kis, L.; Shapiro, D.S.; Jayaraman, V.; Marshall, W.T., 3rd; Montgomery, S.C. Direct oral anticoagulants compared with warfarin in patients with severe blunt trauma. Injury 2017, 48, 47–50. [Google Scholar] [CrossRef]
- Hwang, P.; Ong, A.W.; Muller, A.; McNicholas, A.; Martin, A.; Sigal, A.; Fernandez, F.B. Geriatric Patients on Antithrombotic Agents Who Fall: Does Trauma Team Activation Improve Outcomes? Am. Surg. 2019, 85, 721–724. [Google Scholar] [CrossRef]
- Kerschbaum, M.; Lang, S.; Henssler, L.; Ernstberger, A.; Alt, V.; Pfeifer, C.; Worlicek, M.; Popp, D. Influence of Oral Anticoagulation and Antiplatelet Drugs on Outcome of Elderly Severely Injured Patients. J. Clin. Med. 2021, 10, 1649. [Google Scholar] [CrossRef]
- Sammy, I.; Lecky, F.; Sutton, A.; Leaviss, J.; O’Cathain, A. Factors affecting mortality in older trauma patients-A systematic review and meta-analysis. Injury 2016, 47, 1170–1183. [Google Scholar] [CrossRef]
- DiMaggio, C.; Ayoung-Chee, P.; Shinseki, M.; Wilson, C.; Marshall, G.; Lee, D.C.; Wall, S.; Maulana, S.; Leon Pachter, H.; Frangos, S. Traumatic injury in the United States: In-patient epidemiology 2000-2011. Injury 2016, 47, 1393–1403. [Google Scholar] [CrossRef]
- Tornetta, P., 3rd; Mostafavi, H.; Riina, J.; Turen, C.; Reimer, B.; Levine, R.; Behrens, F.; Geller, J.; Ritter, C.; Homel, P. Morbidity and mortality in elderly trauma patients. J. Trauma 1999, 46, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Van Ameijden, S.; de Jongh, M.; Poeze, M. The severely injured older patient: Identifying patients at high risk for mortality using the Dutch National Trauma Registry. Eur. J. Trauma Emerg. Surg. 2025, 51, 54. [Google Scholar] [CrossRef] [PubMed]
- Niemeyer, M.; Jochems, D.; Houwert, R.M.; van Es, M.A.; Leenen, L.; van Wessem, K. Mortality in polytrauma patients with moderate to severe TBI on par with isolated TBI patients: TBI as last frontier in polytrauma patients. Injury 2022, 53, 1443–1448. [Google Scholar] [CrossRef]
- Weihs, V.; Heel, V.; Dedeyan, M.; Lang, N.W.; Frenzel, S.; Hajdu, S.; Heinz, T. Age and traumatic brain injury as prognostic factors for late-phase mortality in patients defined as polytrauma according to the New Berlin Definition: Experiences from a level I trauma center. Arch. Orthop. Trauma Surg. 2021, 141, 1677–1681. [Google Scholar] [CrossRef]
- Saad, S.; Mohamed, N.; Moghazy, A.; Ellabban, G.; El-Kamash, S. Venous glucose, serum lactate and base deficit as biochemical predictors of mortality in patients with polytrauma. Ulus Travma Acil Cerrahi Derg. 2016, 22, 29–33. [Google Scholar] [CrossRef][Green Version]
- Probst, C.; Pape, H.C.; Hildebrand, F.; Regel, G.; Mahlke, L.; Giannoudis, P.; Krettek, C.; Grotz, M.R. 30 years of polytrauma care: An analysis of the change in strategies and results of 4849 cases treated at a single institution. Injury 2009, 40, 77–83. [Google Scholar] [CrossRef]
- Regel, G.; Lobenhoffer, P.; Grotz, M.; Pape, H.C.; Lehmann, U.; Tscherne, H. Treatment results of patients with multiple trauma: An analysis of 3406 cases treated between 1972 and 1991 at a German Level I Trauma Center. J. Trauma 1995, 38, 70–78. [Google Scholar] [CrossRef]
- Doran, J.; Salih, M.; Bell, A.; Kinsella, A.; Joyce, D.; Burke, F.; Moran, P.; Cosgrave, D.; Bates, J.; Meshkat, B.; et al. Major trauma patients and their outcomes—A retrospective observational study of critical care trauma admissions to a trauma unit with special services. Injury 2024, 55, 111622. [Google Scholar] [CrossRef]
- Bingold, T.M.; Lefering, R.; Zacharowski, K.; Meybohm, P.; Waydhas, C.; Rosenberger, P.; Scheller, B.; Group, D.I.C.R. Individual Organ Failure and Concomitant Risk of Mortality Differs According to the Type of Admission to ICU—A Retrospective Study of SOFA Score of 23,795 Patients. PLoS ONE 2015, 10, e0134329. [Google Scholar] [CrossRef]
- Lichte, P.; Kobbe, P.; Almahmoud, K.; Pfeifer, R.; Andruszkow, H.; Hildebrand, F.; Lefering, R.; Pape, H.C.; Trauma Register, D.G.U. Post-traumatic thrombo-embolic complications in polytrauma patients. Int. Orthop. 2015, 39, 947–954. [Google Scholar] [CrossRef]
- Peltan, I.D.; Vande Vusse, L.K.; Maier, R.V.; Watkins, T.R. An International Normalized Ratio-Based Definition of Acute Traumatic Coagulopathy Is Associated with Mortality, Venous Thromboembolism, and Multiple Organ Failure After Injury. Crit. Care Med. 2015, 43, 1429–1438. [Google Scholar] [CrossRef] [PubMed]
- Lefering, R.; Huber-Wagner, S.; Nienaber, U.; Maegele, M.; Bouillon, B. Update of the trauma risk adjustment model of the TraumaRegister DGU: The Revised Injury Severity Classification, version II. Crit. Care 2014, 18, 476. [Google Scholar] [CrossRef]
- Huber, S.; Biberthaler, P.; Delhey, P.; Trentzsch, H.; Winter, H.; van Griensven, M.; Lefering, R.; Huber-Wagner, S.; Trauma Register, D.G.U. Predictors of poor outcomes after significant chest trauma in multiply injured patients: A retrospective analysis from the German Trauma Registry (Trauma Register DGU(R)). Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 52. [Google Scholar] [CrossRef]
- Wong, T.H.; Krishnaswamy, G.; Nadkarni, N.V.; Nguyen, H.V.; Lim, G.H.; Bautista, D.C.; Chiu, M.T.; Chow, K.Y.; Ong, M.E. Combining the new injury severity score with an anatomical polytrauma injury variable predicts mortality better than the new injury severity score and the injury severity score: A retrospective cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 25. [Google Scholar] [CrossRef]
- Injury, G.B.D.T.B.; Spinal Cord Injury, C. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 56–87. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).