Delayed Management of Concurrent Coronal Extrusions and Root Fractures in Two Traumatized Maxillary Immature Permanent Central Incisors: A Case Study
Abstract
1. Introduction
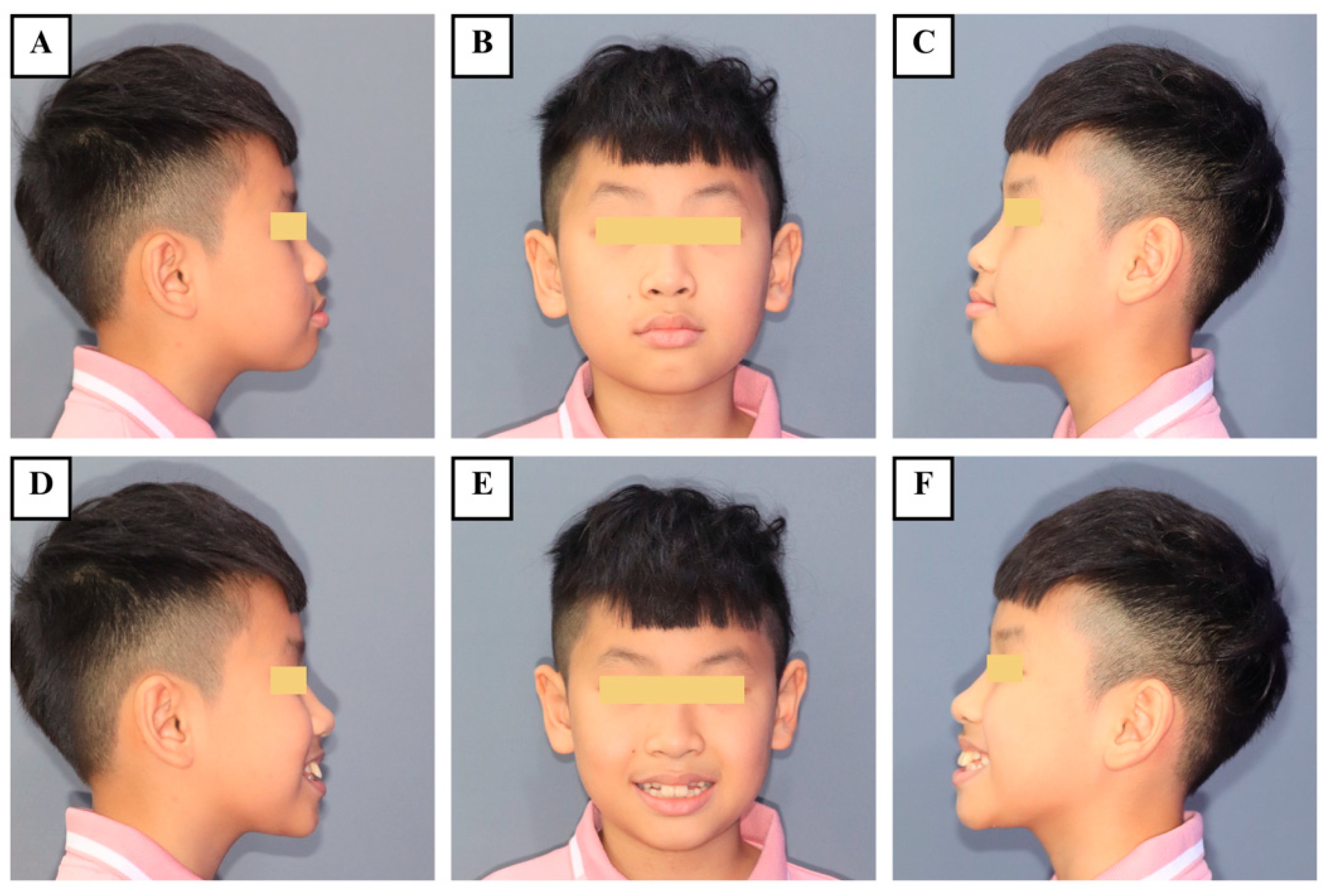
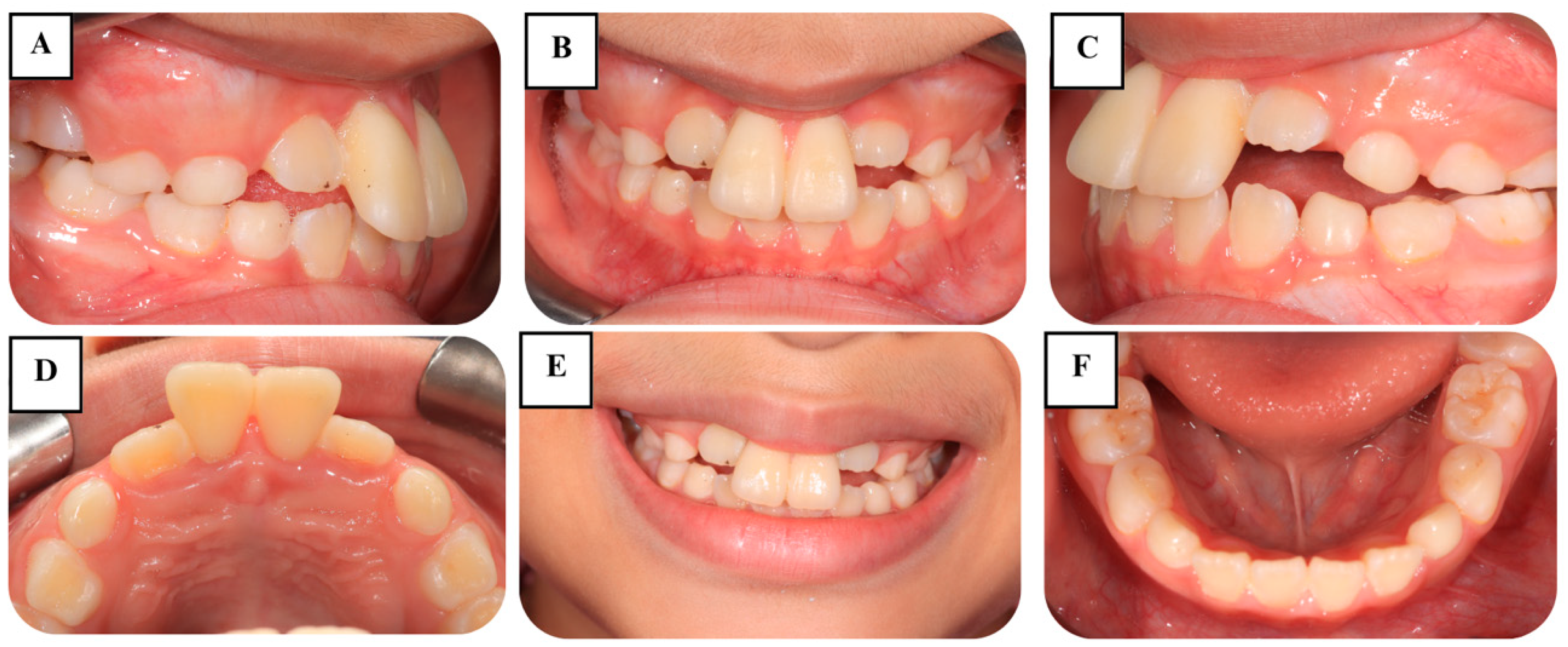
2. Case Presentation
2.1. Case History
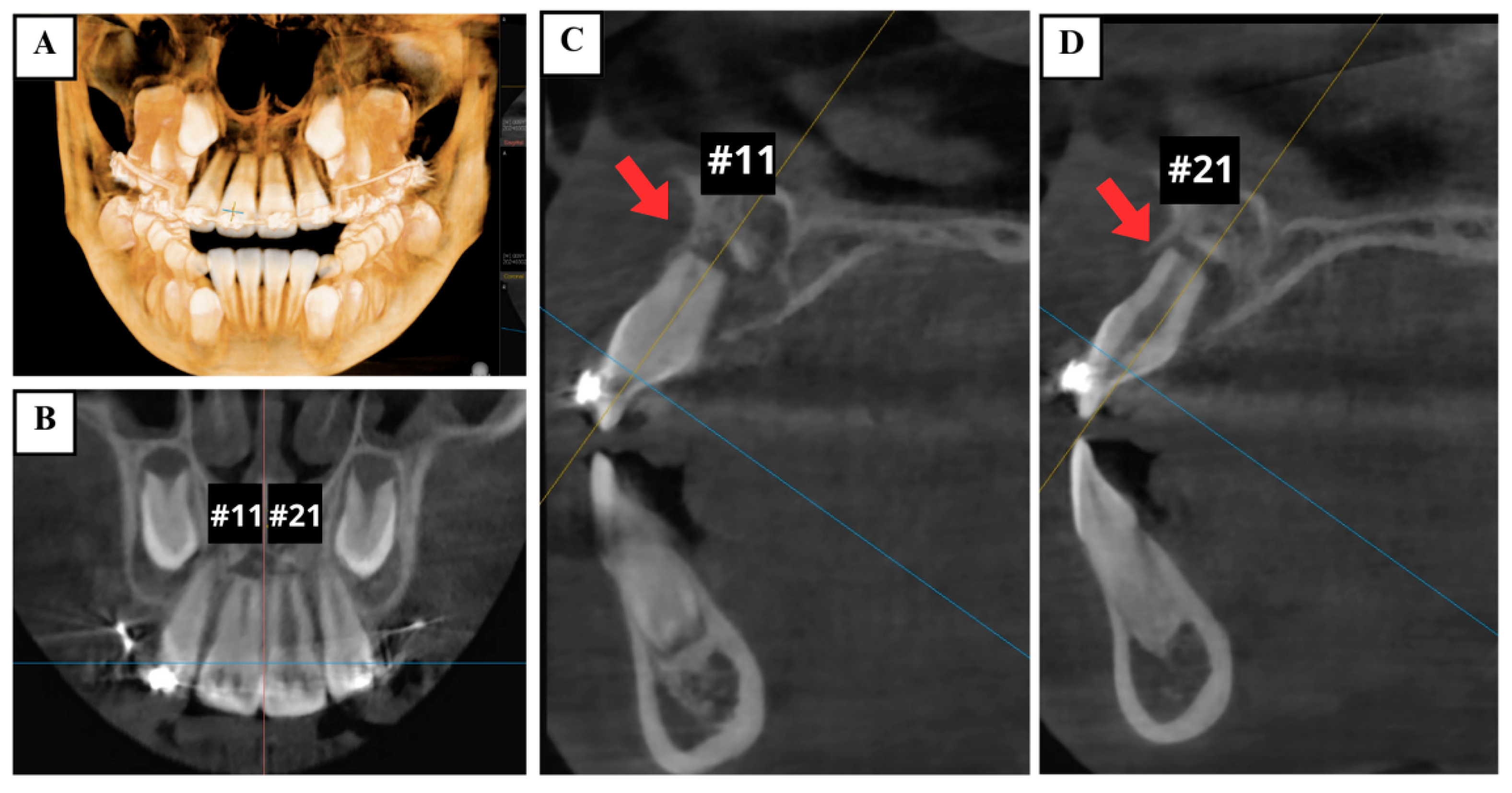
2.2. Preoperative Examination
2.3. Diagnosis
2.4. Treatment Plan
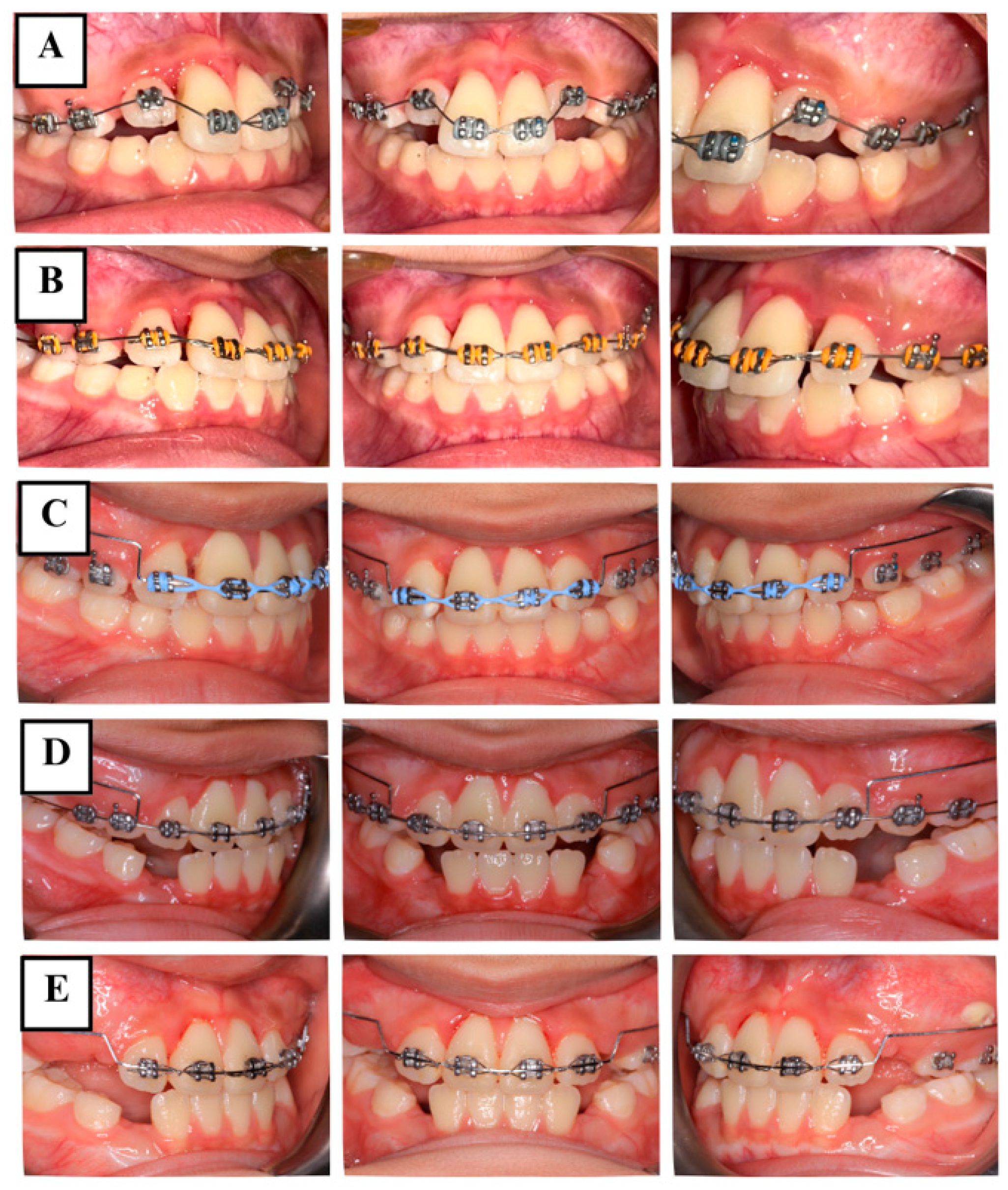
2.5. Treatment Procedures
2.5.1. Phase 1: Periodontal Management
2.5.2. Phase 2: Orthodontic Management
2.5.3. Phase 3: Follow-Up
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petti, S.; Glendor, U.; Andersson, L. World traumatic dental injury prevalence and incidence, a meta-analysis-One billion living people have had traumatic dental injuries. Dent. Traumatol. 2018, 34, 71–86. [Google Scholar] [CrossRef] [PubMed]
- Laforgia, A.; Inchingolo, A.M.; Inchingolo, F.; Sardano, R.; Trilli, I.; Noia, A.D.; Ferrante, L.; Palermo, A.; Inchingolo, A.D.; Dipalma, G. Paediatric dental trauma: Insights from epidemiological studies and management recommendations. BMC Oral Health 2025, 25, 6. [Google Scholar] [CrossRef] [PubMed]
- Qin, Z.; Xin, K.; Liang, Y.; Cui, Y.; Wang, Y.; Qin, Z.; Wu, M.; Wu, D.; You, Y.; Qiu, R. Assessment of knowledge on traumatized immature permanent teeth among dentists in China: A cross-sectional study. BMC Oral Health 2025, 25, 451. [Google Scholar] [CrossRef]
- Krastl, G.; Filippi, A.; Weiger, R. Initial management of dental trauma: Musts, shoulds, and cans. Quintessence Int. 2020, 51, 763–774. [Google Scholar]
- Cvijic, A.; Kvernenes, M.; Åstrøm, A.N.; Tsilingaridis, G.; Bletsa, A. Treatment of Traumatic Dental Injuries in the Public Dental Services-A Qualitative Exploration of Perceived Challenges and Needs. Dent. Traumatol. 2025, 41, 93–103. [Google Scholar] [CrossRef]
- Bourguignon, C.; Cohenca, N.; Lauridsen, E.; Flores, M.T.; O’Connell, A.C.; Day, P.F.; Tsilingaridis, G.; Abbott, P.V.; Fouad, A.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent. Traumatol. 2020, 36, 314–330. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Andreasen, J.O.; Tsilingaridis, G. Root Fractures. In Textbook and Color Atlas of Traumatic Injuries to the Teeth, 5th ed.; Andreasen, F.M., Andreasen, J.O., Andreasen, L., Eds.; Wiley-Blackwell: Oxford, UK, 2019; pp. 377–412. [Google Scholar]
- Abbott, P.V. Diagnosis and management of transverse root fractures. Dent. Traumatol. 2019, 35, 333–347. [Google Scholar] [CrossRef]
- Amaral, M.F.; de Almeida, M.M.; de Faria, L.P.; Brandini, D.A.; Poi, W.R.; Okamoto, R. Treatment of Extrusive Luxation in Permanent Teeth: Literature Review with Systematic Criteria. J. Contemp. Dent. Pract. 2017, 18, 241–245. [Google Scholar]
- Sheikhnezami, M.; Shahmohammadi, R.; Jafarzadeh, H.; Azarpazhooh, A. Long-Term Outcome of Horizontal Root Fractures in Permanent Teeth: A Retrospective Cohort Study. J. Endod. 2024, 50, 579–589. [Google Scholar] [CrossRef]
- Marasca, B.; Ndokaj, A.; Duś-Ilnicka, I.; Nisii, A.; Marasca, R.; Bossù, M.; Ottolenghi, L.; Polimeni, A. Management of transverse root fractures in dental trauma. Dent. Med. Probl. 2022, 59, 637–645. [Google Scholar] [CrossRef]
- Andreasen, J.O. Luxation of permanent teeth due to trauma. A clinical and radiographic follow-up study of 189 injured teeth. Scand. J. Dent. Res. 1970, 78, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, R.; Lizio, A.; Cervino, G.; Fabiana, N.; Francesco, P.; Ausiello, P.; Cicciù, M. The Horizontal Root Fractures. Diagnosis, Clinical Management and Three-Year Follow-Up. Open Dent. J. 2018, 12, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Andreasen, F.M.; Mejàre, I.; Cvek, M. Healing of 400 intra-alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent. Traumatol. 2004, 20, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Zangani, A.; Mallus, T.; Marogna, G.; Carboni, L. Extrusive and Lateral Luxation Injuries in permanent teeth: Literature Review and Treatment Complications Update. Eur. J. Paediatr. Dent. 2024, 25, 163–167. [Google Scholar]
- Yu, C.Y.; Abbott, P.V. Responses of the pulp, periradicular and soft tissues following trauma to the permanent teeth. Aust. Dent. J. 2016, 61 (Suppl. S1), 39–58. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Andreasen, F.M.; Mejàre, I.; Cvek, M. Healing of 400 intra-alveolar root fractures. 1. Effect of pre-injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent. Traumatol. 2004, 20, 192–202. [Google Scholar] [CrossRef]
- Rouhani, A.; Javidi, B.; Habibi, M.; Jafarzadeh, H. Intentional replantation: A procedure as a last resort. J. Contemp. Dent. Pract. 2011, 12, 486–492. [Google Scholar]
- Spinas, E.; Pipi, L.; Mezzena, S.; Giannetti, L. Use of Orthodontic Methods in the Treatment of Dental Luxations: A Scoping Review. Dent. J. 2021, 9, 18. [Google Scholar] [CrossRef]
- Spinas, E.; Pipi, L.; Dettori, C. Extrusive Luxation Injuries in Young Patients: A Retrospective Study with 5-Year Follow-Up. Dent. J. 2020, 8, 136. [Google Scholar] [CrossRef]
- Ebrahim, F.H.; Kulkarni, G. Fixed orthodontic appliances in the management of severe dental trauma in mixed dentition: A case report. J. Can. Dent. Assoc. 2013, 79, d131. [Google Scholar]
- Alaçam, A.; Uçüncü, N. Combined apexification and orthodontic intrusion of a traumatically extruded immature permanent incisor. Dent. Traumatol. 2002, 18, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Sübay, R.K.; Kayataş, M.; Caniklioğlu, C. Delayed multidisciplinary management of an extrusively luxated maxillary central incisor. Dent. Traumatol. 2007, 23, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Elbay, Ü.Ş.; Baysal, A.; Elbay, M.; Sarıdağ, S. Multidisciplinary approach to delayed treatment of traumatic teeth injuries involving extrusive luxation, avulsion and crown fracture. Oper. Dent. 2014, 39, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Yoon, J.; Lee, B.; Chang, H.; Hwang, I.; Oh, W.; Hwang, Y. Treatment of horizontal root-fractured maxillary incisors. Oral Biol. Res. 2019, 43, 236–242. [Google Scholar] [CrossRef]
- Huang, R.; Zhou, C.; Zhan, L.; Liu, Y.; Liu, X.; Du, Q.; Wang, J.; Zhao, W.; Song, G.; Wu, L.; et al. Experts consensus on management of tooth luxation and avulsion. Int. J. Oral Sci. 2024, 16, 57. [Google Scholar] [CrossRef]
- Cvek, M.; Andreasen, J.O.; Borum, M.K. Healing of 208 intra-alveolar root fractures in patients aged 7–17 years. Dent. Traumatol. 2001, 17, 53–62. [Google Scholar] [CrossRef]
- Cvek, M.; Tsilingaridis, G.; Andreasen, J.O. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7–17 years. Dent. Traumatol. 2008, 24, 379–387. [Google Scholar] [CrossRef]
- Hammarstrom, L.; Lindskog, S. General morphological aspects of resorption of teeth and alveolar bone. Int. Endod. J. 1985, 18, 93–108. [Google Scholar] [CrossRef]
- Kahler, B.; Hu, J.Y.; Marriot-Smith, C.S.; Heithersay, G.S. Splinting of teeth following trauma: A review and a new splinting recommendation. Aust. Dent. J. 2016, 61 (Suppl. S1), 59–73. [Google Scholar] [CrossRef]
- Andreasen, F.M. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endod. Dent. Traumatol. 1989, 5, 111–131. [Google Scholar] [CrossRef]
- Tripathi, U.; Khattri, N.; Agarwal, S.; Nagar, N.; Pandey, H.; Gupta, A. Utility Arches: Simple Yet Effective. IOSR J. Dent. Med. Sci. 2024, 23, 29–32. [Google Scholar]
- Andreasen, J.O.; Andreasen, F.M. Luxation injuries. In Textbook and Color Atlas of Traumatic Injuries to the Teeth, 3rd ed.; Copenhagen: Munksgaard, Denmark, 1993; pp. 315–381. [Google Scholar]
- Levin, L.; Day, P.F.; Hicks, L.; O’Connell, A.; Fouad, A.F.; Bourguignon, C.; Abbott, P.V. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: General introduction. Dent. Traumatol. 2020, 36, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Rajasekhar, R.; Soman, S.; Sebastian, V.M.; Muliyar, S.; Cherian, N.M. Indexes for periapical health evaluation: A review. Int. Dent. Res. 2022, 12, 97–106. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vo, T.T.T.; Do, T.N.A. Delayed Management of Concurrent Coronal Extrusions and Root Fractures in Two Traumatized Maxillary Immature Permanent Central Incisors: A Case Study. J. Clin. Med. 2025, 14, 3605. https://doi.org/10.3390/jcm14103605
Vo TTT, Do TNA. Delayed Management of Concurrent Coronal Extrusions and Root Fractures in Two Traumatized Maxillary Immature Permanent Central Incisors: A Case Study. Journal of Clinical Medicine. 2025; 14(10):3605. https://doi.org/10.3390/jcm14103605
Chicago/Turabian StyleVo, Thi Thuy Tien, and Thi Ngoc Anh Do. 2025. "Delayed Management of Concurrent Coronal Extrusions and Root Fractures in Two Traumatized Maxillary Immature Permanent Central Incisors: A Case Study" Journal of Clinical Medicine 14, no. 10: 3605. https://doi.org/10.3390/jcm14103605
APA StyleVo, T. T. T., & Do, T. N. A. (2025). Delayed Management of Concurrent Coronal Extrusions and Root Fractures in Two Traumatized Maxillary Immature Permanent Central Incisors: A Case Study. Journal of Clinical Medicine, 14(10), 3605. https://doi.org/10.3390/jcm14103605





