Comparative Outcomes of Amblyopia Treatment in High Astigmatism: Stability and Sustained Improvements
Abstract
1. Introduction
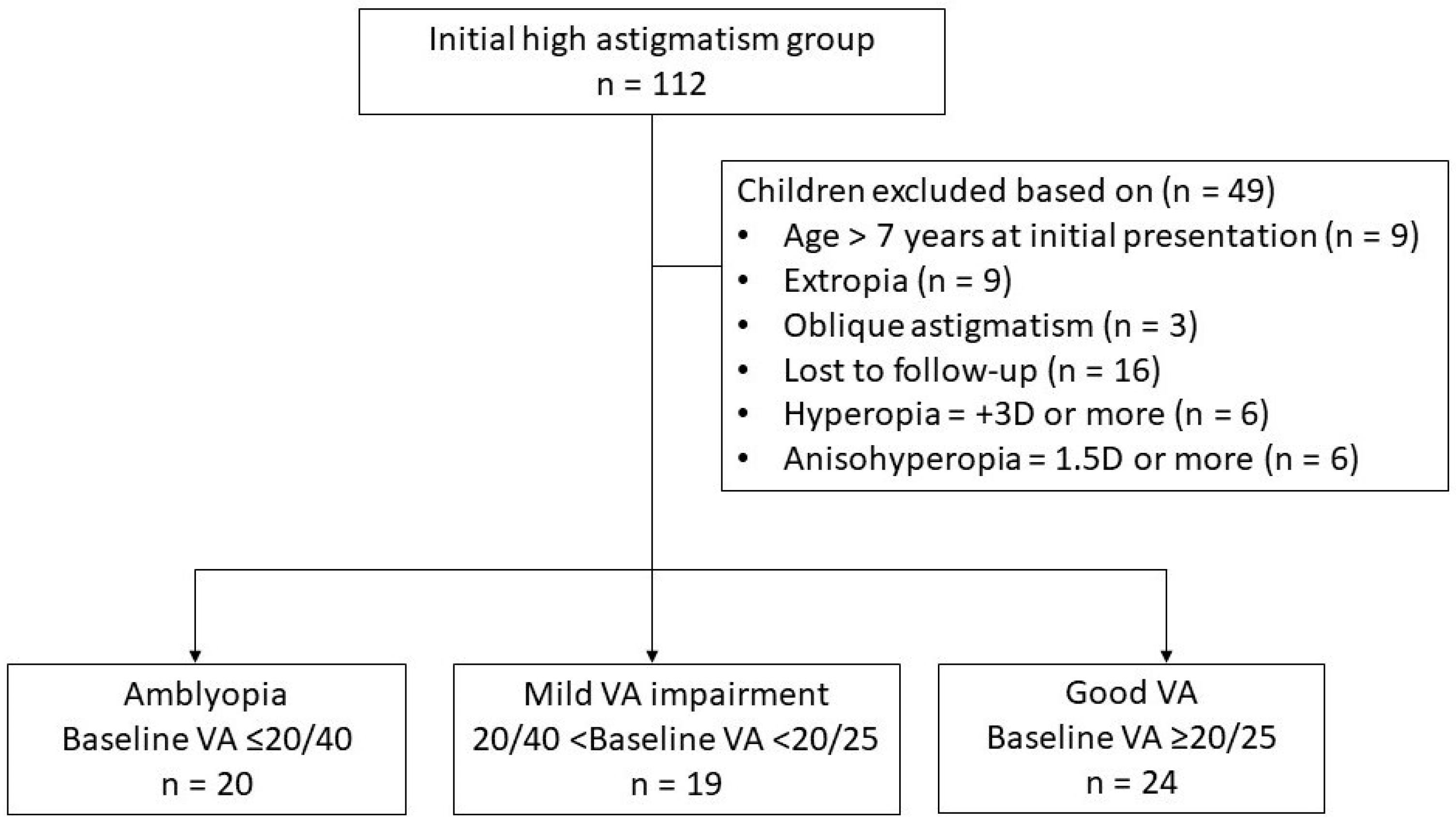
2. Materials and Methods
3. Results
3.1. Baseline Characteristics
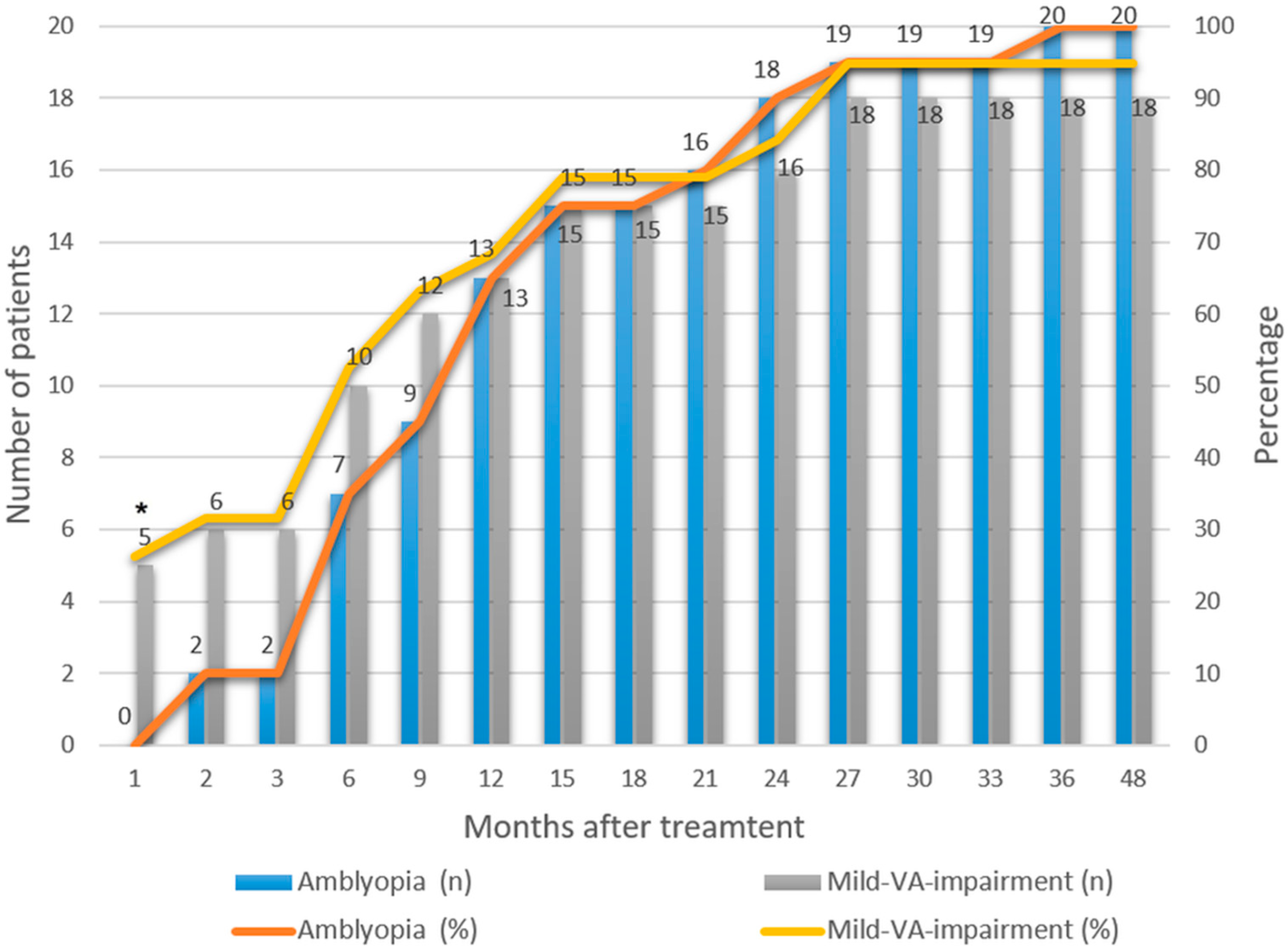
3.2. Rate of Successful Treatment and Treatment Duration
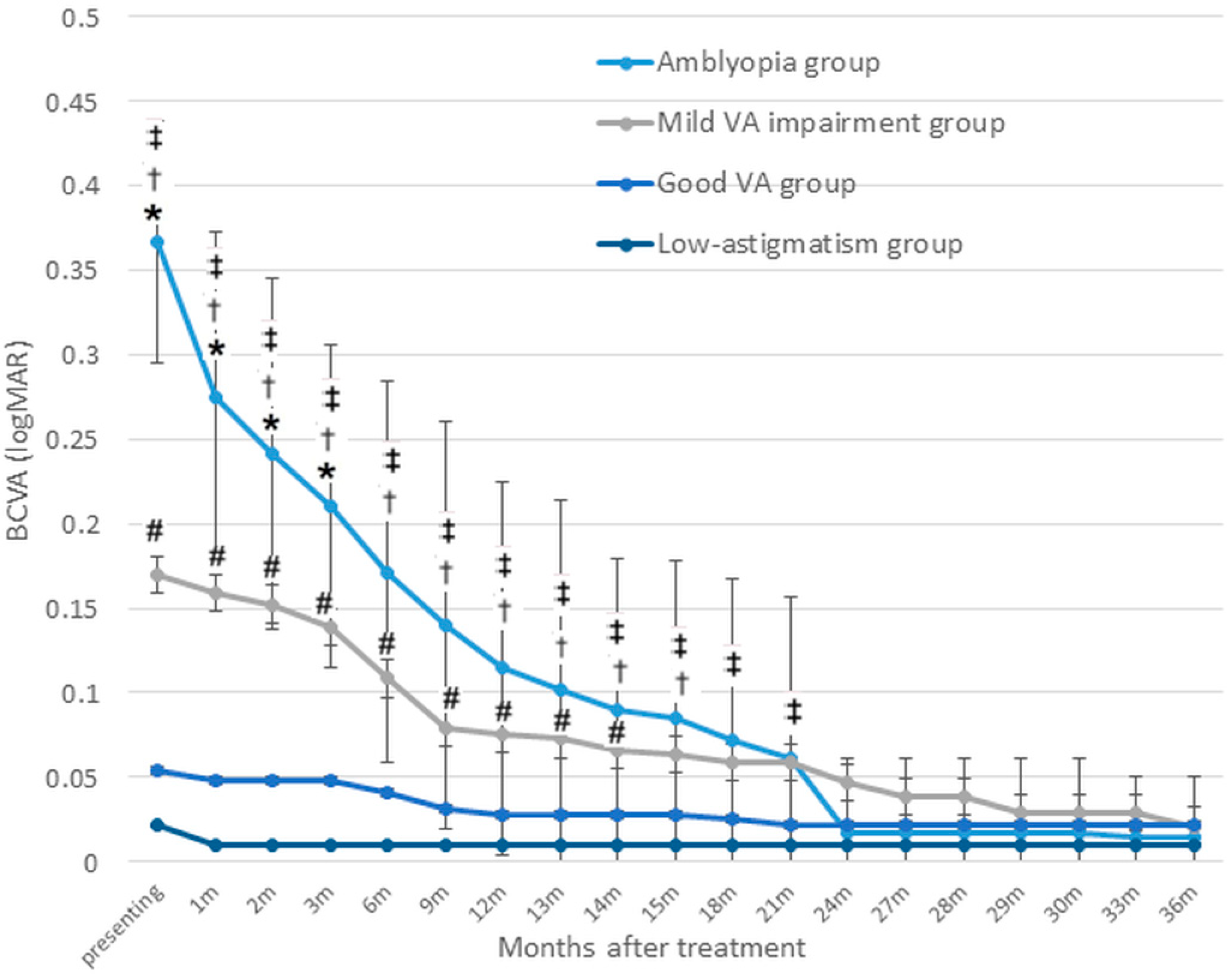
3.3. Changes in VA over Time
3.3.1. VA Improvement over Time Compared with the Baseline Values
3.3.2. Intergroup Comparisons
3.3.3. Trends and Plateau of Changes in VA
3.4. Comparison Between the Patching and No-Patching Subgroups
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BCVA | Best-corrected visual acuity |
| logMAR | Logarithms of the minimal angle of resolution |
| SD | Standard deviation |
| VA | Visual acuity |
References
- Hashemi, H.; Fotouhi, A.; Yekta, A.; Pakzad, R.; Ostadimoghaddam, H.; Khabazkhoob, M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J. Curr. Ophthalmol. 2018, 30, 3–22. [Google Scholar] [CrossRef] [PubMed]
- Harvey, E.M. Development and treatment of astigmatism-related amblyopia. Optom. Vis. Sci. 2009, 86, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Harvey, E.M.; Dobson, V.; Miller, J.M.; Clifford-Donaldson, C.E. Amblyopia in astigmatic children: Patterns of deficits. Vis. Res. 2007, 47, 315–326. [Google Scholar] [CrossRef]
- Mitchell, D.E.; Wilkinson, F. The effect of early astigmatism on the visual resolution of gratings. J. Physiol. 1974, 243, 739–756. [Google Scholar] [CrossRef]
- Cobb, S.R.; MacDonald, C.F. Resolution acuity in astigmats: Evidence for a critical period in the human visual system. Br. J. Physiol. Opt. 1978, 32, 38–49. [Google Scholar]
- Harvey, E.M.; Dobson, V.; Clifford-Donaldson, C.E.; Miller, J.M. Optical treatment of amblyopia in astigmatic children: The sensitive period for successful treatment. Ophthalmology 2007, 114, 2293–2301. [Google Scholar] [CrossRef]
- Harvey, E.M.; Dobson, V.; Miller, J.M.; Sherrill, D.L. Treatment of astigmatism-related amblyopia in 3-to 5-year-old children. Vis. Res. 2004, 44, 1623–1634. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dobson, V.; Clifford-Donaldson, C.E.; Green, T.K.; Miller, J.M.; Harvey, E.M. Optical treatment reduces amblyopia in astigmatic children who receive spectacles before kindergarten. Ophthalmology 2009, 116, 1002–1008. [Google Scholar] [CrossRef]
- Xiao, X.; Liu, W.M.; Ye, Y.J.; Huang, J.Z.; Luo, W.Q.; Liu, H.T.; Lin, Q.; Zhao, W.X.; Lin, E.W. Prevalence of high astigmatism in children aged 3 to 6 years in Guangxi, China. Optom. Vis. Sci. 2014, 91, 390–396. [Google Scholar] [CrossRef]
- Pascual, M.; Huang, J.; Maguire, M.G.; Kulp, M.T.; Quinn, G.E.; Ciner, E.; Cyert, L.A.; Orel-Bixler, D.; Moore, B.; Ying, G.S. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology 2014, 121, 622–629. [Google Scholar] [CrossRef]
- Pai, A.S.; Rose, K.A.; Leone, J.F.; Sharbini, S.; Burlutsky, G.; Varma, R.; Wong, T.Y.; Mitchell, P. Amblyopia prevalence and risk factors in Australian preschool children. Ophthalmology 2012, 119, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.K.; Chandler, D.L.; Beck, R.W.; Arnold, R.W.; Bacal, D.A.; Birch, E.E.; Felius, J.; Frazier, M.; Holmes, J.M.; Hoover, D.; et al. Treatment of bilateral refractive amblyopia in children three to less than 10 years of age. Am. J. Ophthalmol. 2007, 144, 487–496. [Google Scholar] [CrossRef]
- Armstrong, R.A. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol. Opt. 2013, 33, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Repka, M.X.; Cotter, S.A.; Beck, R.W.; Kraker, R.T.; Birch, E.E.; Everett, D.F.; Hertle, R.W.; Holmes, J.M.; Quinn, G.E.; Sala, N.A.; et al. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology 2004, 111, 2076–2085. [Google Scholar] [CrossRef]
- Wallace, D.K.; Lazar, E.L.; Crouch, E.R.; Hoover, D.L.; Kraker, R.T.; Tamkins, S.M. Time course and predictors of amblyopia improvement with 2 hours of daily patching. JAMA Ophthalmol. 2015, 133, 606–609. [Google Scholar] [CrossRef] [PubMed]
- Repka, M.X.; Beck, R.W.; Holmes, J.M.; Birch, E.E.; Chandler, D.L.; Cotter, S.A.; Hertle, R.W.; Kraker, R.T.; Moke, P.S.; Quinn, G.E.; et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch. Ophthalmol. 2003, 121, 603–611. [Google Scholar] [CrossRef]
- Repka, M.X.; Kraker, R.T.; Holmes, J.M.; Summers, A.I.; Glaser, S.R.; Barnhardt, C.N.; Tien, D.R. Atropine vs patching for treatment of moderate amblyopia: Follow-up at 15 years of age of a randomized clinical trial. JAMA Ophthalmol. 2014, 132, 799–805. [Google Scholar] [CrossRef]
- Holmes, J.M.; Kraker, R.T.; Beck, R.W.; Birch, E.E.; Cotter, S.A.; Everett, D.F.; Hertle, R.W.; Quinn, G.E.; Repka, M.X.; Scheiman, M.M.; et al. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology 2003, 110, 2075–2087. [Google Scholar] [CrossRef]
- Kang, H.; Yeon, K.; Han, S.T. A Review on the Use of Effect Size in Nursing Research. J. Korean Acad. Nurs. 2015, 45, 641–649. [Google Scholar] [CrossRef]
- Stewart, C.E.; Moseley, M.J.; Stephens, D.A.; Fielder, A.R. Treatment dose-response in amblyopia therapy: The Monitored Occlusion Treatment of Amblyopia Study (MOTAS). Investig. Ophthalmol. Vis. Sci. 2004, 45, 3048–3054. [Google Scholar] [CrossRef]
- Cotter, S.A.; Edwards, A.R.; Wallace, D.K.; Beck, R.W.; Arnold, R.W.; Astle, W.F.; Barnhardt, C.N.; Birch, E.E.; Donahue, S.P.; Everett, D.F.; et al. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology 2006, 113, 895–903. [Google Scholar] [CrossRef] [PubMed]
- Cotter, S.A.; Varma, R.; Tarczy-Hornoch, K.; McKean-Cowdin, R.; Lin, J.; Wen, G.; Wei, J.; Borchert, M.; Azen, S.P.; Torres, M.; et al. Risk factors associated with childhood strabismus: The multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology 2011, 118, 2251–2261. [Google Scholar] [CrossRef]
- Harvey, E.M.; Dobson, V.; Miller, J.M.; Clifford-Donaldson, C.E. Changes in visual function following optical treatment of astigmatism-related amblyopia. Vis. Res. 2008, 48, 773–787. [Google Scholar] [CrossRef]
- Stewart, C.E.; Moseley, M.J.; Fielder, A.R.; Stephens, D.A. Refractive adaptation in amblyopia: Quantification of effect and implications for practice. Br. J. Ophthalmol. 2004, 88, 1552–1556. [Google Scholar] [CrossRef]
- Lin, P.W.; Chang, H.W.; Lai, I.C.; Teng, M.C. Visual outcomes after spectacles treatment in children with bilateral high refractive amblyopia. Clin. Exp. Optom. 2016, 99, 550–554. [Google Scholar] [CrossRef] [PubMed]
- Fronius, M.; Cirina, L.; Ackermann, H.; Kohnen, T.; Diehl, C.M. Efficiency of electronically monitored amblyopia treatment between 5 and 16 years of age: New insight into declining susceptibility of the visual system. Vis. Res. 2014, 103, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Hussein, M.A.; Coats, D.K.; Muthialu, A.; Cohen, E.; Paysse, E.A. Risk factors for treatment failure of anisometropic amblyopia. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2004, 8, 429–434. [Google Scholar] [CrossRef]
- Scheiman, M.M.; Hertle, R.W.; Beck, R.W.; Edwards, A.R.; Birch, E.; Cotter, S.A.; Crouch, E.R., Jr.; Cruz, O.A.; Davitt, B.V.; Donahue, S.; et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch. Ophthalmol. 2005, 123, 437–447. [Google Scholar] [CrossRef]
- Holmes, J.M.; Beck, R.W.; Kraker, R.T.; Astle, W.F.; Birch, E.E.; Cole, S.R.; Cotter, S.A.; Donahue, S.; Everett, D.F.; Hertle, R.W.; et al. Risk of amblyopia recurrence after cessation of treatment. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2004, 8, 420–428. [Google Scholar] [CrossRef]
- Bhola, R.; Keech, R.V.; Kutschke, P.; Pfeifer, W.; Scott, W.E. Recurrence of amblyopia after occlusion therapy. Ophthalmology 2006, 113, 2097–2100. [Google Scholar] [CrossRef]
- Lewis, T.L.; Maurer, D. Multiple sensitive periods in human visual development: Evidence from visually deprived children. Dev. Psychobiol. 2005, 46, 163–183. [Google Scholar] [CrossRef] [PubMed]
- Steele, A.L.; Bradfield, Y.S.; Kushner, B.J.; France, T.D.; Struck, M.C.; Gangnon, R.E. Successful treatment of anisometropic amblyopia with spectacles alone. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2006, 10, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Dobson, V.; Miller, J.M.; Harvey, E.M.; Mohan, K.M. Amblyopia in astigmatic preschool children. Vis. Res. 2003, 43, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, D.E.; Freeman, R.D.; Millodot, M.; Haegerstrom, G. Meridional amblyopia: Evidence for modification of the human visual system by early visual experience. Vis. Res. 1973, 13, 535–558. [Google Scholar] [CrossRef]
- Wen, G.; Tarczy-Hornoch, K.; McKean-Cowdin, R.; Cotter, S.A.; Borchert, M.; Lin, J.; Kim, J.; Varma, R. Prevalence of Myopia, Hyperopia, and Astigmatism in Non-Hispanic White and Asian Children: Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology 2013, 120, 2109–2116. [Google Scholar] [CrossRef]
| High Astigmatism Group | Low Astigmatism Group (n = 46) | ||||
|---|---|---|---|---|---|
| Amblyopia (VA ≤ 20/40) (n = 20) | Mild VA Impairment (20/40 < VA < 20/25) (n = 19) | Good VA (VA ≥ 20/25) (n = 24) | p Value * | ||
| Sex (male/female) | 7/13 | 11/8 | 12/12 | 0.350 | 23/23 |
| Age (years) | |||||
| 3 to <4 | 5 | 3 | 3 | 3 | |
| 4 to <5 | 8 | 6 | 7 | 7 | |
| 5 to <6 | 6 | 7 | 10 | 11 | |
| 6 to ≤7 | 1 | 3 | 4 | 25 | |
| Mean (±SD; range) | 4.51 (±0.88; 3–6.8) | 4.96 (±0.98; 3.6–6.8) | 5.03 (±1.0; 3–6.8) | 0.142 | 5.89 (±1.15; 3.1–7) |
| Cylindrical power (D) † | |||||
| 0 to <−0.50 | 17 | ||||
| −0.50 to <−1.00 | 11 | ||||
| −1.00 to ≤−1.50 | 18 | ||||
| −2.50 to <−3.50 | 9 | 11 | 14 | ||
| −3.50 to <−4.50 | 6 | 6 | 9 | ||
| −4.50 to <−5.50 | 3 | 1 | 1 | ||
| −5.50 to ≤−6.50 | 2 | 1 | 0 | ||
| Mean (±SD; range) | −3.84 (±1.13; −6.50 to −2.50) | −3.34 (±0.82; −5.50 to −2.50) | −3.25 (±0.59; −4.50 to −2.50) | 0.177 | −0.70 (±0.46; −1.50 to 0) |
| High Astigmatism Group | Low Astigmatism Group (n = 46) | ||||
|---|---|---|---|---|---|
| Amblyopia (VA ≤ 20/40) (n = 20) | Mild VA Impairment (20/40 < VA < 20/25) (n = 19) | Good VA (VA ≥ 20/25) (n = 24) | p Value * | ||
| BCVA† at baseline (logMAR), mean (±SD; range) | 0.37 (±0.07; 0.30–0.52) | 0.17 (±0.03; 0.16–0.22) | 0.05 (±0.05; 0.00–0.10) | 0.00 | 0.02 (±0.04; 0.00–0.10) |
| Final VA (logMAR), mean (±SD; range) | 0.01 (±0.04; 0.00–0.10) | 0.02 (±0.05; 0.00–0.16) | 0.02 (±0.04; 0.00–0.10) | 0.32 | 0.01 (±0.02; 0.00–0.10) |
| Time to achieve successful treatment (weeks) ‡, median (IQR) | 37.5 (17.04–72.39) | 22.5 (4.00–58.14) | 0.25 | ||
| Age at treatment success (years) ‡, mean (±SD; range) | 5.73 (±0.85; 4.6–7.6) | 5.75 (±1.4; 4.1–8.8) | 0.48 | ||
| Time to reach final VA (weeks), median (IQR) | 57.77 (34.86–91.39) | 38.86 (24–84.71) | 3.93 (0–27.5) | 0.00 | |
| Time of last follow-up from treatment success (weeks), median (IQR) ‡ | 66.79 (46.36–158.5) | 84.29 (24–194.86) | 0.98 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-C.; Lee, L.-C.; Chang, H.-C.; Huang, C.-H.; Chien, K.-H. Comparative Outcomes of Amblyopia Treatment in High Astigmatism: Stability and Sustained Improvements. J. Clin. Med. 2025, 14, 3577. https://doi.org/10.3390/jcm14103577
Hsu C-C, Lee L-C, Chang H-C, Huang C-H, Chien K-H. Comparative Outcomes of Amblyopia Treatment in High Astigmatism: Stability and Sustained Improvements. Journal of Clinical Medicine. 2025; 14(10):3577. https://doi.org/10.3390/jcm14103577
Chicago/Turabian StyleHsu, Chia-Chen, Lung-Chi Lee, Hsu-Chieh Chang, Chun-Hao Huang, and Ke-Hung Chien. 2025. "Comparative Outcomes of Amblyopia Treatment in High Astigmatism: Stability and Sustained Improvements" Journal of Clinical Medicine 14, no. 10: 3577. https://doi.org/10.3390/jcm14103577
APA StyleHsu, C.-C., Lee, L.-C., Chang, H.-C., Huang, C.-H., & Chien, K.-H. (2025). Comparative Outcomes of Amblyopia Treatment in High Astigmatism: Stability and Sustained Improvements. Journal of Clinical Medicine, 14(10), 3577. https://doi.org/10.3390/jcm14103577







