Ridge Recontouring with Simultaneous Implant Placement Using Autogenous Bone Core Grafts
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Surgical Protocol
2.4. Statistical Analysis
3. Results
Study Group Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BCB | Bone core block |
| CBCT | Cone beam computer tomography |
| SD | Standard deviation |
References
- Nulty, A. A literature review on prosthetically designed guided implant placement and the factors influencing dental implant success. Br. Dent. J. 2024, 236, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Galiffi, D.; Scrascia, R.; Gualandri, M.; Zadrożny, Ł.; Czajkowska, M.; Catapano, S.; Grande, F.; Baldoni, E.; Lumbau, A.I.; et al. Digital workflow for prosthetically driven implants placement and digital cross mounting: A retrospective case series. Prosthesis 2022, 4, 353–368. [Google Scholar] [CrossRef]
- Alzahrani, K.M. Implant bio-mechanics for successful implant therapy: A systematic review. J. Int. Soc. Prev. Community Dent. 2020, 10, 700–714. [Google Scholar] [CrossRef]
- Al-Oulabi, A.; Abdulkareem, D.; Saleh, A. Neutral zone concept for implant placement in mandibular overdentures: A case report. Dent. Update 2022, 49, 522–525. [Google Scholar] [CrossRef]
- Bustamante, G.; Vives, F.; Angulo, C.; Parra, E. Ultra-slow drilling to obtain autologous bone graft in implantological rehabilitation: A forgotten technique with great advantages. Int. J. Interdiscip. Dent. 2021, 14, 55–57. [Google Scholar] [CrossRef]
- John, V.; Weddell, J.A.; Shin, D.E.; Jones, J.E. Gingivitis and periodontal disease. In McDonald and Avery’s Dentistry for the Child and Adolescent, 10th ed.; Dean, J.A., Ed.; Mosby: St. Louis, MO, USA, 2016; pp. 243–273. [Google Scholar]
- Mateo, G.D.; Mazón-Esteve, J.P.; Pineda-Villacorta, C.R.; Blaya-Tarraga, J.A.; Diaz-Fernandez, J.M. Frequency of surgical bone augmentation methods complementary to dental implant placement: A study evaluated with cone beam computed tomography. J. Clin. Exp. Dent. 2023, 15, e1029–e1034. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kandhari, S.; Khalid, S.; James, A.; Laverty, D.P. Bone grafting techniques and materials for implant dentistry. Br. Dent. J. 2023, 235, 180–189. [Google Scholar] [CrossRef]
- Khoury, F.; Doliveux, R. The bone core technique for the augmentation of limited bony defects: Five-year prospective study with a new minimally invasive technique. Int. J. Periodontics Restor. Dent. 2018, 38, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Khoury, F.; Zastera, A. Reconstructing peri-implant bone defects using minimally invasive autologous bone augmentation. Smile Int. 2023, 1, 48–51. [Google Scholar]
- STROBE Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). Available online: https://www.strobe-statement.org/ (accessed on 12 May 2025).
- Misch, C.E. Contemporary Implant Dentistry, 3rd ed.; Mosby: St. Louis, MO, USA, 2014. [Google Scholar]
- Lim, H.C.; Ha, K.I.; Hong, J.Y.; Han, J.Y.; Shin, S.I.; Shin, S.Y.; Herr, Y.; Chung, J.-H. Comparison of the bone harvesting capacity of an intraoral bone harvesting device and three different implant drills. Biomed. Res. Int. 2017, 2017, 7819080. [Google Scholar] [CrossRef]
- Nurcahyanti, H.; Amalia, M. Comparison of xenograft and alloplast bone grafts for infrabony bone defect: Literature review. J. Food Pharm. Sci. 2023, 11, 851–859. [Google Scholar] [CrossRef]
- Cui, X.; Reason, T.; Pardi, V.; Rapoport, D.; Morrison, W. CBCT analysis of crestal soft tissue thickness before implant placement and its relationship with cortical bone thickness. BMC Oral. Health. 2022, 22, 593. [Google Scholar] [CrossRef] [PubMed]
- Pramstraller, M. The Edentulous Posterior Ridge: Novel Diagnostic and Therapeutic Approaches for Bone Augmentation. Dissertation, Ph.D. Thesis, University of Ferrara, Ferrara, Italy, 2018. [Google Scholar]
- Wang, S.H.; Shen, Y.W.; Fuh, L.J.; Peng, S.L.; Tsai, M.T.; Huang, H.L.; Hsu, J.-T. Relationship between cortical bone thickness and cancellous bone density at dental implant sites in the jawbone. Diagnostics 2020, 10, 710. [Google Scholar] [CrossRef] [PubMed]

| Total number of surgical procedures | 38 |
| Gender distribution | 29 females |
| 10 males | |
| Age range (years old) | 26–77 |
| Mean age (years old) | 49 (±12.27) |
| Smoking status | 32 nonsmokers (83.2%) |
| 6 smokers (15.8%) | |
| Total number of osteosynthesis screws used | 90 |
| Total number of osteosynthesis screws removed | 21 |
| Implant diameter range (mm) | 3.1 to 4.8 |
| Implant failure | 1 case (2.6%) |
| Mean initial width of the crest (mm) | 5.95 (±0.72) |
| Bone graft width (mm) | 2.5 (bone core diameter) |
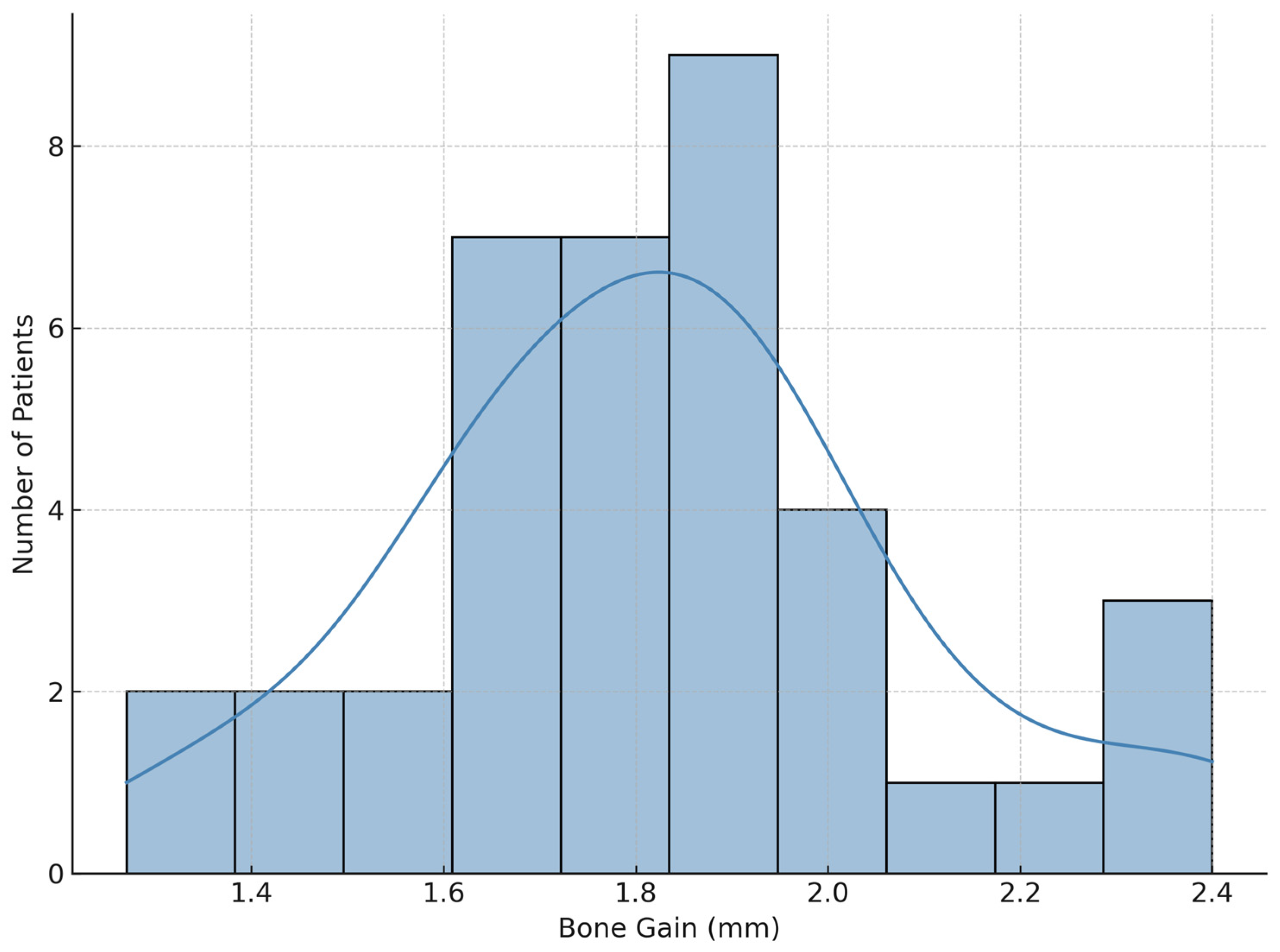
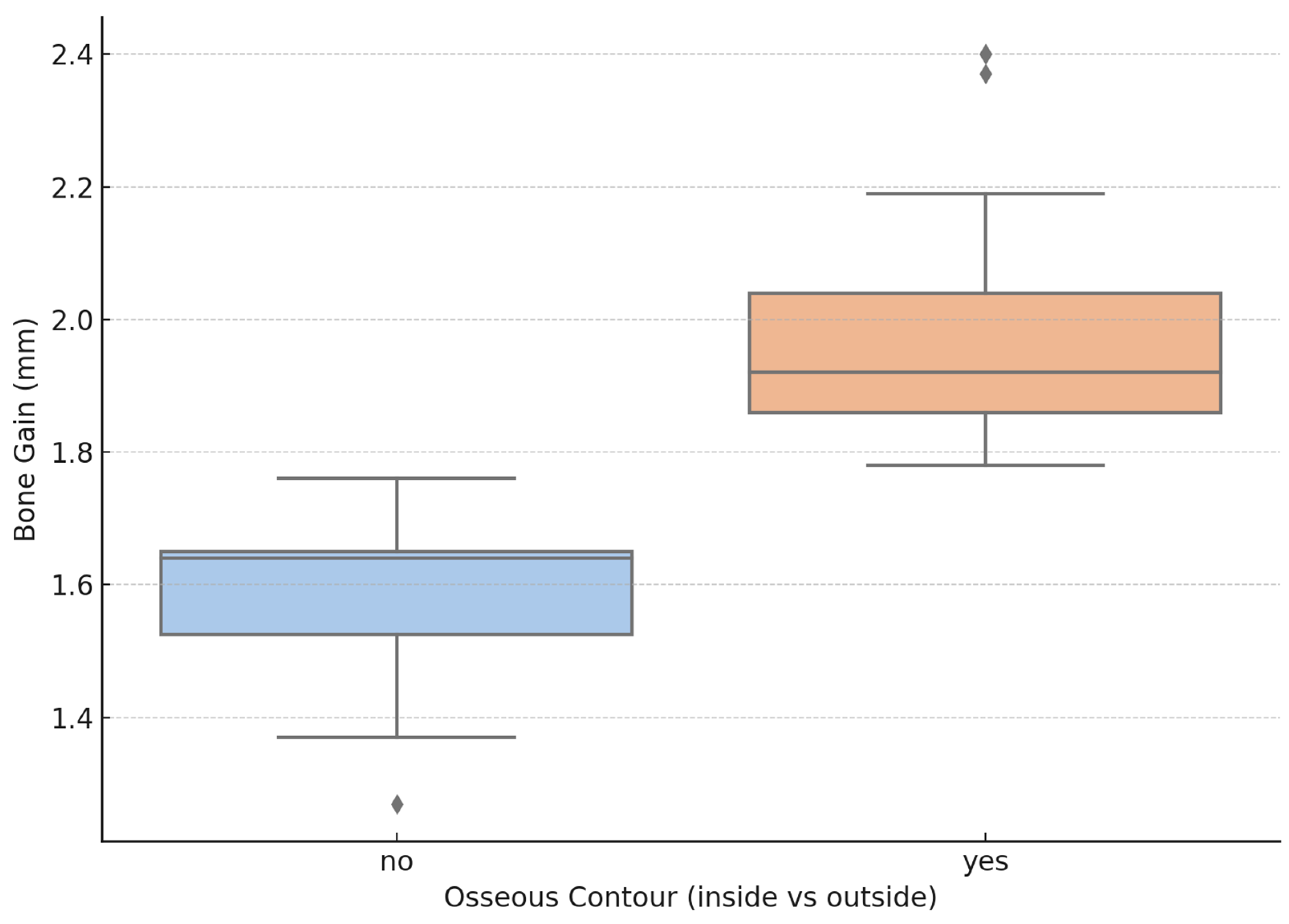
| Average horizontal bone gain (mm) | 1.8 (±0.28) |
| Follow-up period | 1.8–8.3 years |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbu, H.M.; Petris, A.S.; Iancu, S.A.; Burcea, A.; Banateanu, A.M.; Caruntu, A. Ridge Recontouring with Simultaneous Implant Placement Using Autogenous Bone Core Grafts. J. Clin. Med. 2025, 14, 3541. https://doi.org/10.3390/jcm14103541
Barbu HM, Petris AS, Iancu SA, Burcea A, Banateanu AM, Caruntu A. Ridge Recontouring with Simultaneous Implant Placement Using Autogenous Bone Core Grafts. Journal of Clinical Medicine. 2025; 14(10):3541. https://doi.org/10.3390/jcm14103541
Chicago/Turabian StyleBarbu, Horia Mihail, Andreea Sorina Petris, Stefania Andrada Iancu, Alexandru Burcea, Andreea Mariana Banateanu, and Ana Caruntu. 2025. "Ridge Recontouring with Simultaneous Implant Placement Using Autogenous Bone Core Grafts" Journal of Clinical Medicine 14, no. 10: 3541. https://doi.org/10.3390/jcm14103541
APA StyleBarbu, H. M., Petris, A. S., Iancu, S. A., Burcea, A., Banateanu, A. M., & Caruntu, A. (2025). Ridge Recontouring with Simultaneous Implant Placement Using Autogenous Bone Core Grafts. Journal of Clinical Medicine, 14(10), 3541. https://doi.org/10.3390/jcm14103541









