The Impact of Comorbidities and Intensive Care Unit (ICU) Admissions on Survival in Kyphoscoliosis-Related Respiratory Failure: A Retrospective Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Chronic Respiratory Failure (CRF) Outpatient Clinic Setting
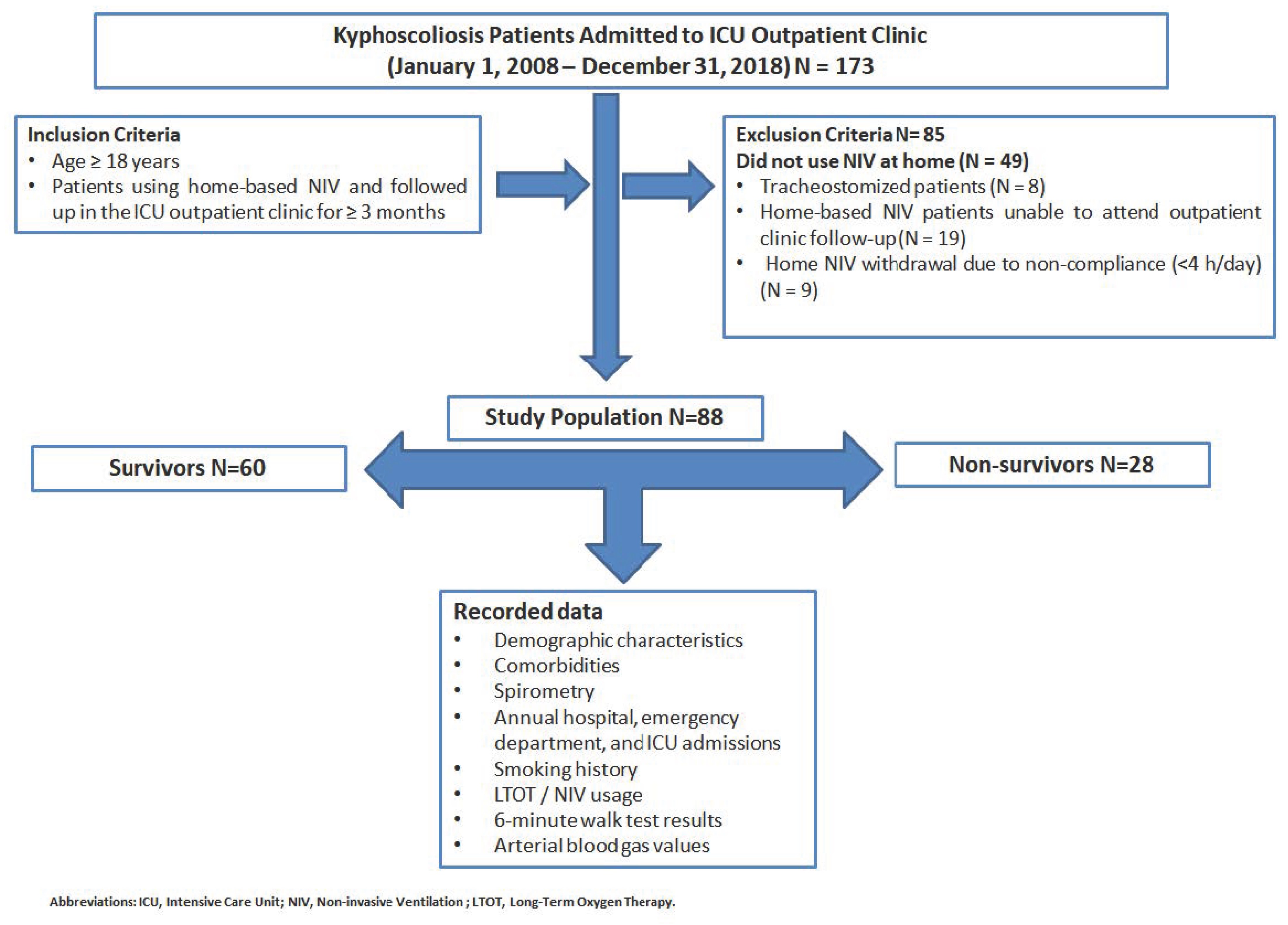
2.2. Patients
- Age ≥ 18 years;
- Patients using home-based NIV followed up in the ICU outpatient clinic ≥ 3 months.
- Patients discharged from the ICU without NIV;
- Tracheostomized patients;
- Patients undergoing home-based NIV who were unable to attend outpatient clinic follow-up;
- Home-based NIV withdrawal due to non-compliance (<4 h/day).
2.3. Definitions
2.3.1. Chronic Respiratory Failure
2.3.2. Restrictive Lung Diseases (Kyphoscoliosis)
2.3.3. Indications for NIV Use at Home in Kyphoscoliosis Patients
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NIV | non-invasive ventilation |
| CAD | coronary artery disease |
| ICU | intensive care unit |
| CRF | chronic respiratory failure |
| BMI | body mass index |
| FEV1 | forced expiratory volume in the first second |
| FVC | forced vital capacity |
| mMRC | Modified Medical Research Council |
| ODI | oxygen desaturation index |
| CWD | chest wall deformities |
| PaCO2 | partial arterial carbon dioxide pressure |
| PaO2 | partial arterial oxygen pressure |
References
- Marwah, V.; Dhar, R.; Choudhary, R.; Elliot, M. Domiciliary noninvasive ventilation for chronic respiratory diseases. Med. J. Armed Forces India 2022, 78, 380–386. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Simonds, A.K.; Elliott, M.W. Outcome of domiciliary nasal intermittent positive pressure ventilation in restrictive and obstructive disorders. Thorax 1995, 50, 604–609. [Google Scholar] [CrossRef] [PubMed]
- Buyse, B.; Meersseman, W.; Demedts, M. Treatment of chronic respiratory failure in kyphoscoliosis: Oxygen or ventilation? Eur. Respir. J. 2003, 22, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Piesiak, P.; Brzecka, A.; Kosacka, M.; Jankowska, R. Efficacy of noninvasive volume targeted ventilation in patients with chronic respiratory failure due to kyphoscoliosis. Adv. Exp. Med. Biol. 2015, 838, 53–58. [Google Scholar] [PubMed]
- Gustafson, T.; Franklin, K.A.; Midgren, B.; Pehrsson, K.; Ranstam, J.; Ström, K. Survival of patients with kyphoscoliosis receiving mechanical ventilation or oxygen at home. Chest 2006, 130, 1828–1833. [Google Scholar] [CrossRef] [PubMed]
- Chailleux, E.; Fauroux, B.; Binet, F.; Dautzenberg, B.; Polu, J.M. Predictors of survival in patients receiving domiciliary oxygen therapy or mechanical ventilation. A 10-year analysis of ANTADIR Observatory. Chest 1996, 109, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Martí, S.; Pallero, M.; Ferrer, J.; Ríos, J.; Rodríguez, E.; Morell, F.; Muñoz, X. Predictors of mortality in chest wall disease treated with noninvasive home mechanical ventilation. Respir. Med. 2010, 104, 1843–1849. [Google Scholar] [CrossRef] [PubMed]
- Adıgüzel, N.; Karakurt, Z.; Güngör, G.; Moçin, O.; Balcı, M.; Saltürk, C.; Kargın, F.; Takır, H.B.; Güven, A.; Yarkın, T. Management of kyphoscoliosis patients with respiratory failure in the intensive care unit and during long term follow up. Multidiscip. Respir. Med. 2012, 7, 30. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Acartürk Tunçay, E.; Karakurt, Z.; Aksoy, E.; Saltürk, C.; Gungor, S.; Ciftaslan, N.; Irmak, İ.; Yavuz, D.; Ocakli, B.; Adıgüzel, N. Eosinophilic and non-eosinophilic COPD patients with chronic respiratory failure: Neutrophil-to-lymphocyte ratio as an exacerbation marker. Int. J. Chron. Obs. Pulmon. Dis. 2017, 12, 3361–3370. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Markou, N.K.; Mryianthefs, P.M.; Baltopoulos, G.J. Respiratory failure: An overview. Crit. Care Nurs. Q. 2004, 27, 353–379. [Google Scholar] [CrossRef]
- Özer, S.; Adıyaman, F.M.; Yamanel, H.L. Noninvasive Mechanical Ventilation in Restrictive Lung Diseases. In Noninvasive Mechanical Ventilation Application, 1st ed.; Kunter, E., Öcal, S., Eds.; Turkiye Klinikleri: Ankara, Türkiye, 2019; pp. 61–64. [Google Scholar]
- Social Security Institution, Health Practice Notification, Official Gazette. Available online: https://www.resmigazete.gov.tr/eskiler/2012/06/20120622-24.htm (accessed on 1 January 2018).
- Düzenli, H.; Doğan, O.T.; Berk, S.; Ozşahin, S.L.; Akkurt, I. Kronik solunum yetmezliği olan olgularda uzun süreli oksijen tedavisinin yaşam süresi üzerine etkisi [The effects of long-term oxygen therapy on survival in patients with chronic respiratory failure]. Tuberk. Toraks. 2008, 56, 179–186. [Google Scholar] [PubMed]
- Tsolaki, V.; Pastaka, C.; Kostikas, K.; Karetsi, E.; Dimoulis, A.; Zikiri, A.; Koutsokera, A.; Gourgoulianis, K.I. Noninvasive ventilation in chronic respiratory failure: Effects on quality of life. Respiration 2011, 81, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Nicolini, A.; Barlascini, C.; Piroddi, I.M.; Garuti, G.; Banfi, P.I. Effectiveness and safety of mouthpiece ventilation and nocturnal non-invasive ventilation in patients with kyphoscoliosis: Short and long-term outcomes after an episode of acute respiratory failure. Rev. Port. Pneumol. 2016, 22, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, T.; Ohi, M.; Oga, T.; Machida, K.; Chihara, Y.; Harada, Y.; Takahashi, K.; Sumi, K.; Handa, T.; Niimi, A.; et al. Importance of the PaCO(2) from 3 to 6 months after initiation of long-term non-invasive ventilation. Respir. Med. 2010, 104, 1850–1857. [Google Scholar] [CrossRef] [PubMed]
- Leger, P.; Bedicam, J.M.; Cornette, A.; Reybet-Degat, O.; Langevin, B.; Polu, J.M.; Jeannin, L.; Robert, D. Nasal intermittent positive pressure ventilation. Long-term follow-up in patients with severe chronic respiratory insufficiency. Chest 1994, 105, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.R.; Grunstein, R.R.; Chan, S.; Bye, P.T.; Sullivan, C.E. Noninvasive ventilatory support during sleep improves respiratory failure in kyphoscoliosis. Chest 1988, 94, 811–815. [Google Scholar] [CrossRef] [PubMed]

| Survivors n = 60 | Non-Survivors n = 28 | p-Value | |
|---|---|---|---|
| Age, median (IQR) | 60 (49–69) | 62 (52–73) | 0.54 |
| Male, n (%) | 30 (50) | 16 (57) | 0.53 |
| BMI, median (IQR) (kg/m2) | 23 (20–26) | 22 (18–31) | 0.79 |
| Biomass, n (%) | 6 (11) | 5 (18) | 0.4 |
| Smoking, n (%) | |||
| 35 (59) | 15 (54) | 0.04 |
| 7 (12) | 9 (32) | |
| 17 (29) | 4 (14) | |
| mMRC score, n (%) | |||
| 0 (0) | 1 (4) | <0.001 |
| 8 (14) | 0 (0) | |
| 26 (47) | 1 (4) | |
| 14 (25) | 21 (75) | |
| 8 (14) | 5 (17) | |
| Daily NIV usage time in hour, median (IQR) | 5 (4–7) | 6 (4–8) | 0.08 |
| Comorbidities, n (%) | 33 (55) | 14 (50) | 0.66 |
| 19 (32) | 7 (25) | 0.52 |
| 8 (13) | 10 (36) | 0.015 |
| 4 (7) | 3 (11) | 0.51 |
| 5 (8) | 4 (13) | 0.39 |
| 2 (3) | 1 (4) | 0.95 |
| Hospital admissions within 1 year before home-based NIV, median (IQR) | 1 (1–2) | 2 (1–3) | 0.002 |
| ICU admissions within 1 year before home-based NIV, median (IQR) | 1 (1–1) | 1 (1–1) | 0.53 |
| Hospital admission after initiation of home-based NIV therapy in a year, median (IQR) | 0 (0–0) | 0 (0–1) | 0.04 |
| Total hospital admission after initiation of home-based NIV therapy, median (IQR) | 0 (0–0) | 0 (0–0) | 0.4 |
| ICU admission after initiation of home-based NIV therapy in a year, median (IQR) | 0 (0–0) | 0 (0–1) | <0.001 |
| Total ICU admission after initiation of home-based NIV therapy, median (IQR) | 0 (0–0) | 1 (0–1) | 0.002 |
| ABG values (first outpatient clinic visit after the initiation of home-based NIV), median (IQR) | |||
| 7.42 (7.38–7.45) | 7.41 (7.38–7.42) | 0.15 |
| 48 (44–53) | 48.5 (46–54) | 0.48 |
| 65 (58–74) | 68.5 (62–75) | 0.21 |
| 5.4 (3.9–8.6) | 6.5 (3.7–7.7) | 1.0 |
| 93 (90–96) | 94 (92–95) | 0.79 |
| ABG values (at the last outpatient clinic visit), median (IQR) | |||
| 7.40 (7.37–7.43) | 7.49 (7.45–7.52) | 0.018 |
| 49 (45–52) | 52 (43–59) | 0.30 |
| 66 (60–74) | 66 (62–82) | 0.61 |
| 5.4 | 6.5 (2.6–9) | 0.70 |
| 94 (91–95) | 94 (90–97) | 0.88 |
| Pulmonary function test (first outpatient clinic visit after the initiation of home-based NIV), median (IQR) | |||
| 600 (460–810) | 715 (460–870) | 0.45 |
| 31 (22–37) | 36 (28–46) | 0.69 |
| 685 (530–960) | 825 (575–1068) | 0.42 |
| 30 (21–35) | 36 (28–42) | 0.83 |
| 79 (77–85) | 84 (77–91) | 0.45 |
| Pulmonary function test (at last outpatient clinic visit), median (IQR) | |||
| 550 (430–690) | 640 (500–1010) | 0.29 |
| 28 (23–36) | 30 (29–60) | 0.29 |
| 630 (530–810) | 650 (610–900) | 0.53 |
| 28 (21–37) | 33 (23–55) | 0.32 |
| 78 (75–86) | 82 (80–86) | 0.09 |
| 6MWT at first outpatient clinic visit, median (IQR) | 371 (288–441) | 357 (245–455) | 0.68 |
| 6MWT at last outpatient clinic visit, median (IQR) | 444 (345–489) | 426 (372–480) | 0.79 |
| Survival days, median (IQR) | 2499 (1430–3586) | 1144 (910–2336) | 0.003 |
| Follow-up days, median (IQR) | 1975 (863–2726) | 679 (98–1615) | 0.001 |
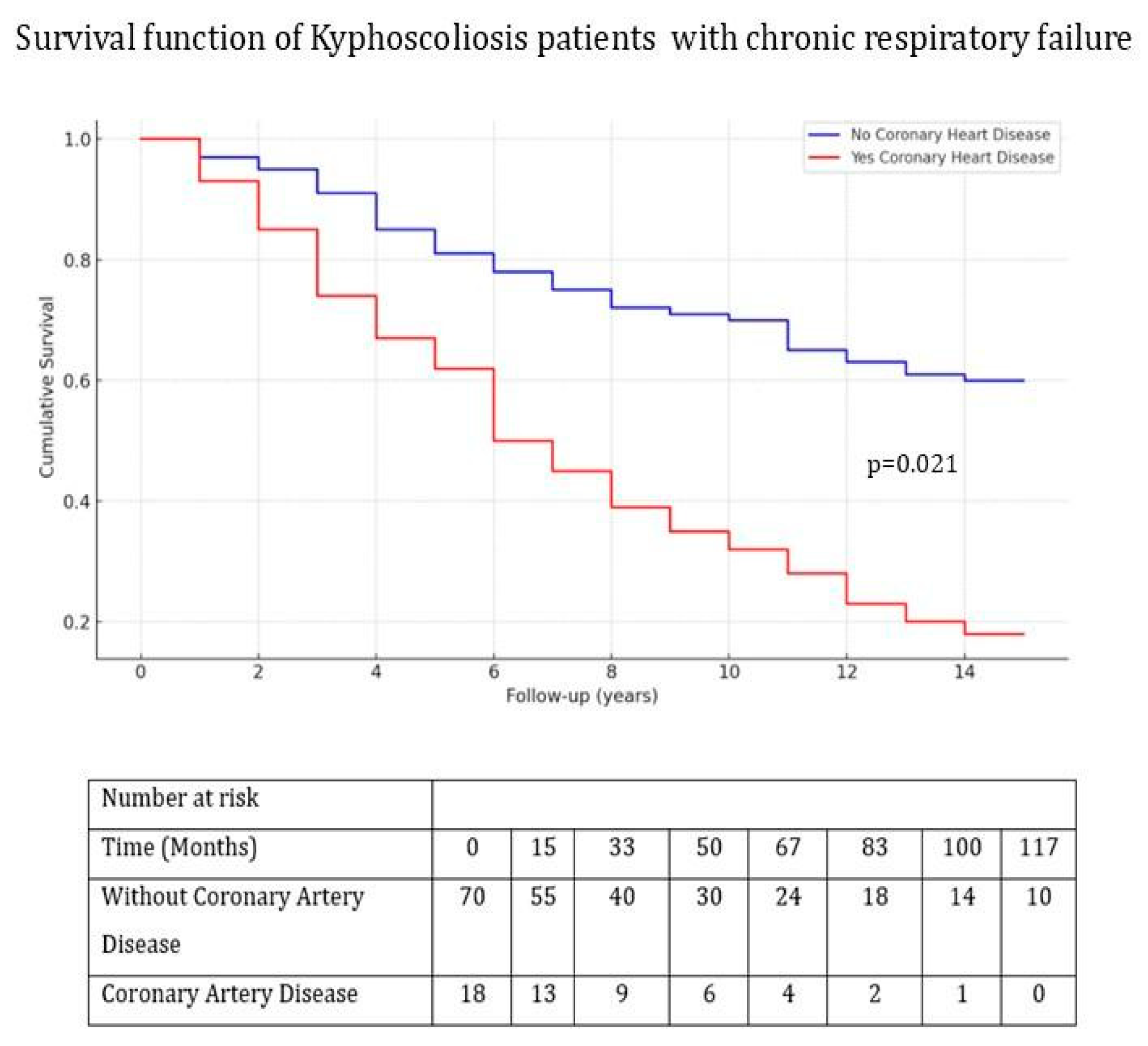
| HR | 95% CI | p-Value | |
|---|---|---|---|
| Lower–Upper | |||
| mMRC score ≥ 2 | 2.093 | 0.269–16.310 | 0.581 |
| CAD | 5.687 | 1.343–24.076 | 0.018 |
| Total ICU admission after initiation of home-based NIV therapy | 1.969 | 1.007–3.849 | 0.04 |
| pH at the last outpatient visit | 0.501 | 0.01–0.692 | 0.003 |
| Smoking status | 1.224 | 0.515–2.910 | 0.648 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tunçay, E.; Güngör, S.; Ertam, B.N.; Ocaklı, B.; Aksoy, E.; Yazıcıoğlu Moçin, Ö.; Güngor, G.; Adıgüzel, N.; Karakurt, Z. The Impact of Comorbidities and Intensive Care Unit (ICU) Admissions on Survival in Kyphoscoliosis-Related Respiratory Failure: A Retrospective Cohort Study. J. Clin. Med. 2025, 14, 3516. https://doi.org/10.3390/jcm14103516
Tunçay E, Güngör S, Ertam BN, Ocaklı B, Aksoy E, Yazıcıoğlu Moçin Ö, Güngor G, Adıgüzel N, Karakurt Z. The Impact of Comorbidities and Intensive Care Unit (ICU) Admissions on Survival in Kyphoscoliosis-Related Respiratory Failure: A Retrospective Cohort Study. Journal of Clinical Medicine. 2025; 14(10):3516. https://doi.org/10.3390/jcm14103516
Chicago/Turabian StyleTunçay, Eylem, Sinem Güngör, Buse Nur Ertam, Birsen Ocaklı, Emine Aksoy, Özlem Yazıcıoğlu Moçin, Gökay Güngor, Nalan Adıgüzel, and Zühal Karakurt. 2025. "The Impact of Comorbidities and Intensive Care Unit (ICU) Admissions on Survival in Kyphoscoliosis-Related Respiratory Failure: A Retrospective Cohort Study" Journal of Clinical Medicine 14, no. 10: 3516. https://doi.org/10.3390/jcm14103516
APA StyleTunçay, E., Güngör, S., Ertam, B. N., Ocaklı, B., Aksoy, E., Yazıcıoğlu Moçin, Ö., Güngor, G., Adıgüzel, N., & Karakurt, Z. (2025). The Impact of Comorbidities and Intensive Care Unit (ICU) Admissions on Survival in Kyphoscoliosis-Related Respiratory Failure: A Retrospective Cohort Study. Journal of Clinical Medicine, 14(10), 3516. https://doi.org/10.3390/jcm14103516







