Incidence of Unapparent Preoperative Deep Vein Thrombosis in Patients with Traumatic Intraarticular Tibial Plateau Fracture
Abstract
1. Introduction
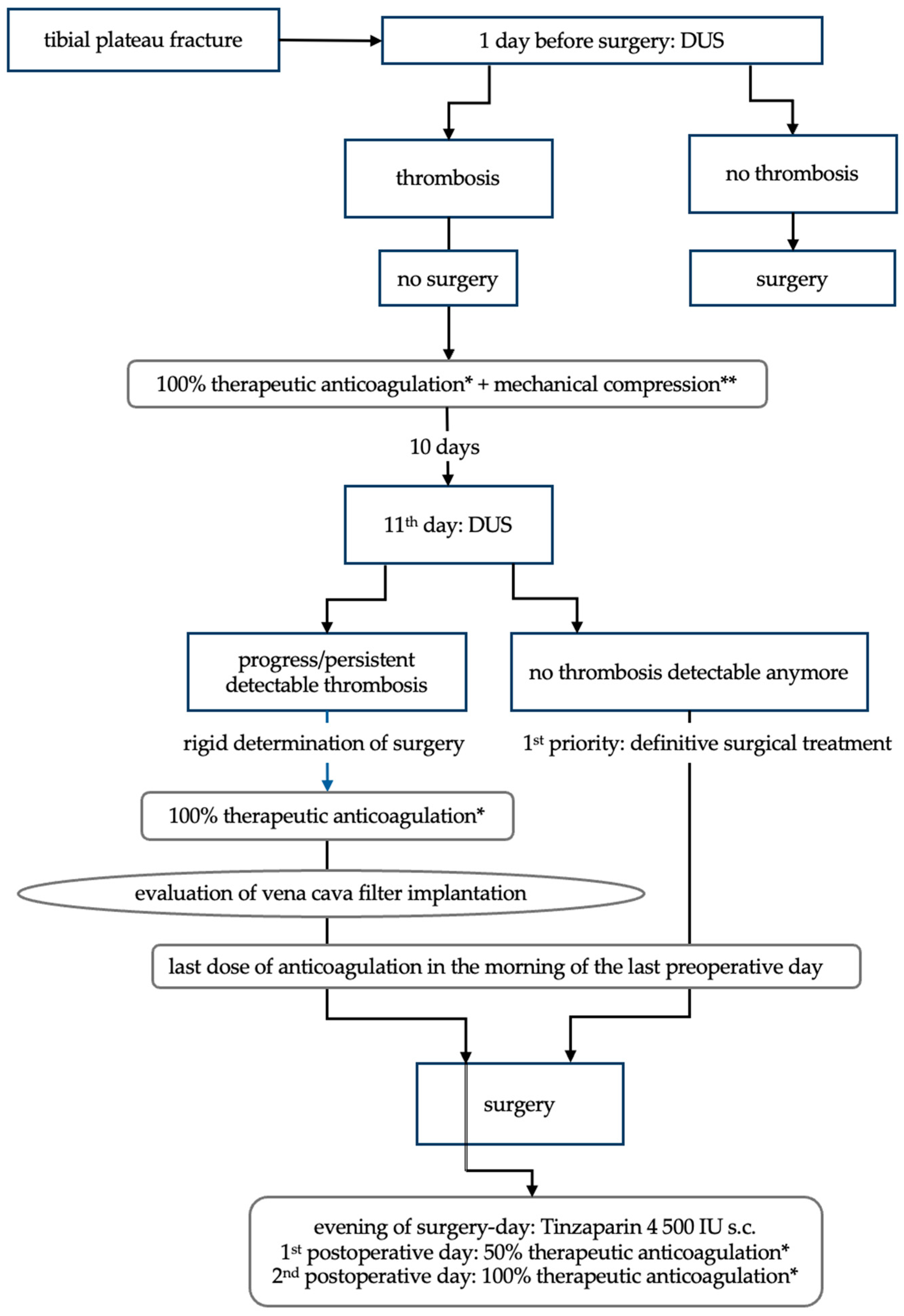
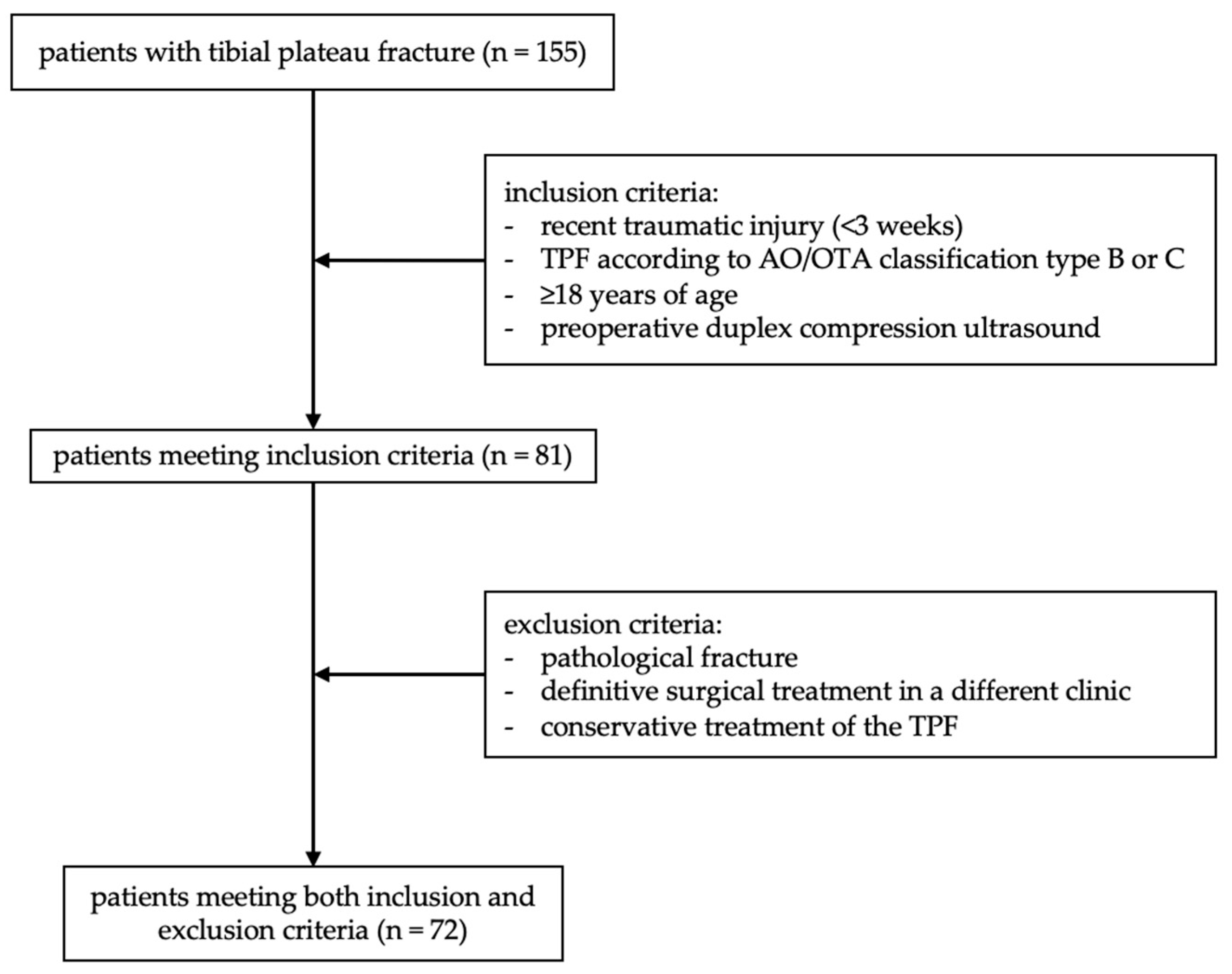
2. Materials and Methods
3. Results
3.1. Patient Cohort
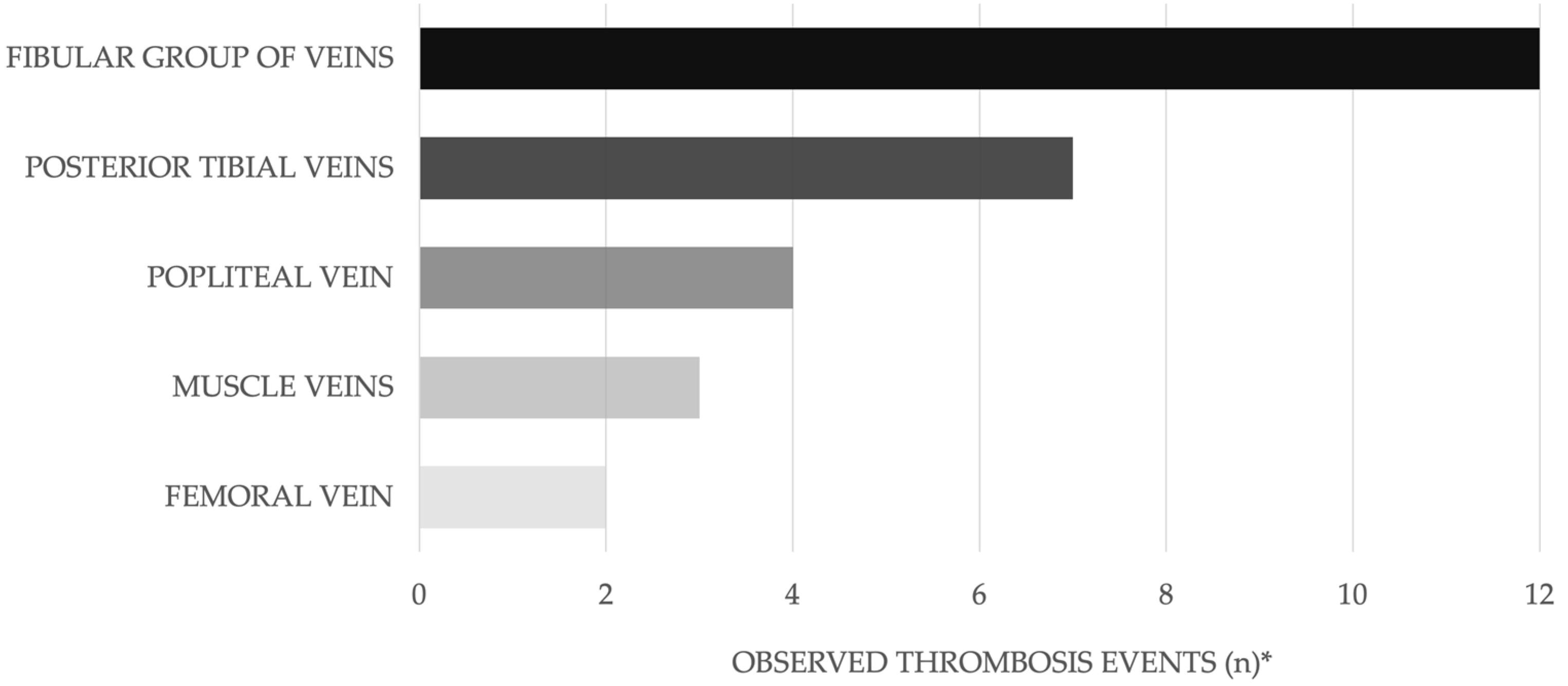
3.2. DVT Patients’ Characteristics
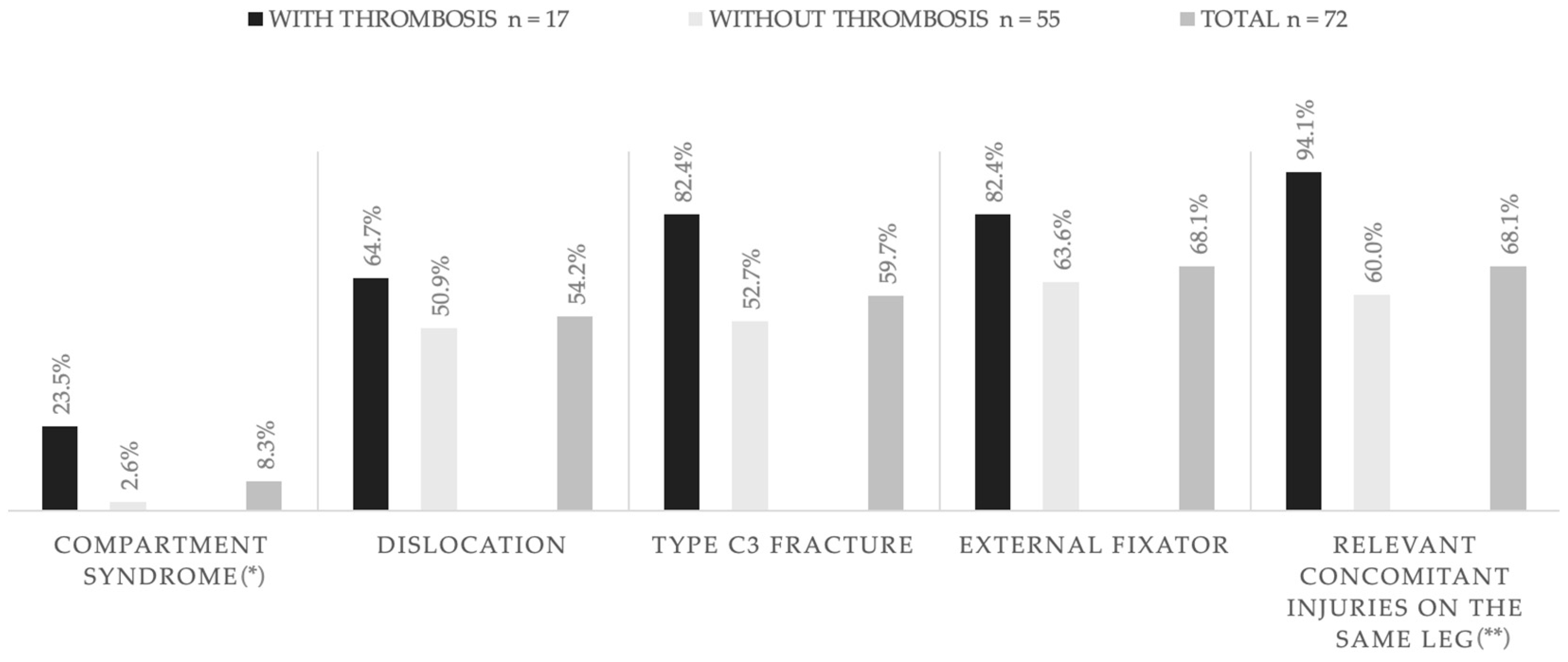
3.3. Known Risk Factors for DVT
3.4. Perioperative Management of DVT Patients
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ASA | American Society of Anesthesiologists |
| BMI | Body mass index |
| DUS | Duplex compression ultrasound |
| DVT | Deep vein thrombosis |
| IU | International units |
| IVC | Inferior vena cava |
| LOS | Length of stay |
| MDPI | Multidisciplinary Digital Publishing Institute |
| PE | Pulmonary embolism |
| SPSS | Statistical Package for the Social Sciences |
| TPF | Tibial plateau fracture |
| VTE | Venous thromboembolism |
References
- Aust, G.; Engele, J.; Kirsch, J.; Mayerhofer, A.; Mense, S.; Salvetter, J.; Schulte, E.; Schultz, C.; Wennemuth, G.; Wolff, W.; et al. Duale Reihe Anatomie [Internet], 6th ed.; Georg Thieme Verlag KG: Stuttgart, Germany, 2025; Available online: https://eref.thieme.de/10.1055/b000000824 (accessed on 22 October 2024).
- Niethard, F.U.; Pfeil, J.; Biberthaler, P. (Eds.) Duale Reihe Orthopädie und Unfallchirurgie [Internet], 9th ed.; Georg Thieme Verlag KG: Stuttgart, Germany, 2022; Available online: https://eref.thieme.de/10.1055/b000000573 (accessed on 22 October 2024).
- Elsoe, R.; Larsen, P.; Nielsen, N.P.H.; Swenne, J.; Rasmussen, S.; Ostgaard, S.E. Population-Based Epidemiology of Tibial Plateau Fractures. Orthopedics 2015, 38, e780–e786. [Google Scholar] [CrossRef] [PubMed]
- Manidakis, N.; Dosani, A.; Dimitriou, R.; Stengel, D.; Matthews, S.; Giannoudis, P. Tibial plateau fractures: Functional outcome and incidence of osteoarthritis in 125 cases. Int. Orthop. (SICOT) 2010, 34, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Papagelopoulos, P.J.; Partsinevelos, A.A.; Themistocleous, G.S.; Mavrogenis, A.F.; Korres, D.S.; Soucacos, P.N. Complications after tibia plateau fracture surgery. Injury 2006, 37, 475–484. [Google Scholar] [CrossRef]
- Choo, K.; Morshed, S. Postoperative Complications after Repair of Tibial Plateau Fractures. J. Knee Surg. 2013, 27, 011–020. [Google Scholar] [CrossRef]
- Henkelmann, R.; Frosch, K.-H.; Glaab, R.; Lill, H.; Schoepp, C.; Seybold, D.; Josten, C.; Hepp, P.; Committee TRAUMA of the AGA-Society for Arthroscopy and Joint Surgery. Infection following fractures of the proximal tibia—A systematic review of incidence and outcome. BMC Musculoskelet. Disord. 2017, 18, 481. [Google Scholar] [CrossRef] [PubMed]
- Arastéh, K.; Dörr, O.; Eich, W.; Ernst, S.; Fischer, K.; Fischer-Rasokat, U.; Fischli, S.; Fleck, R.; Friederich, H.-C.; Hahn, J.-M.; et al. Duale Reihe Innere Medizin. In Innere Medizin. 4., Überarbeitete Auflage; Duale Reihe; Thieme: Stuttgart, Germany, 2018; pp. 321–330. ISBN 978-3-13-118164-0. [Google Scholar]
- Linnemann, B.; Blank, W.; Doenst, T.; Erbel, C.; Isfort, P.; Janssens, U.; Kalka, C.; Klamroth, R.; Kotzerke, J.; Ley, S.; et al. Diagnostik und Therapie der tiefen Venenthrombose und Lungenembolie—AWMF-S2k-Leitlinie. [Internet]. 2023. Available online: https://register.awmf.org/de/leitlinien/detail/065-002 (accessed on 23 May 2024).
- Wendelboe, A.M.; Raskob, G.E. Global Burden of Thrombosis: Epidemiologic Aspects. Circ. Res. 2016, 118, 1340–1347. [Google Scholar] [CrossRef]
- Li, J.; Wang, P.; Zhang, B.; Zhuang, Y.; Xue, H.; Qu, S.; Fei, C.; Yang, N.; Tian, D.; Zhang, K. Relationship Between the Incidence of Deep Vein Thrombosis During Hospitalization and the Energy of Injury in Tibial Plateau Fractures. Clin. Appl. Thromb. Hemost. 2020, 26, 1076029620913948. [Google Scholar] [CrossRef]
- Wang, H.; Kandemir, U.; Liu, P.; Zhang, H.; Wang, P.-F.; Zhang, B.-F.; Shang, K.; Fu, Y.-H.; Ke, C.; Zhuang, Y.; et al. Perioperative incidence and locations of deep vein thrombosis following specific isolated lower extremity fractures. Injury 2018, 49, 1353–1357. [Google Scholar] [CrossRef]
- Zhu, Y.; Chen, W.; Li, J.; Zhao, K.; Zhang, J.; Meng, H.; Zhang, Y.; Zhang, Q. Incidence and locations of preoperative deep venous thrombosis (DVT) of lower extremity following tibial plateau fractures: A prospective cohort study. J. Orthop. Surg. Res. 2021, 16, 113. [Google Scholar] [CrossRef]
- Goel, D.P.; Buckley, R.; deVries, G.; Abelseth, G.; Ni, A.; Gray, R. Prophylaxis of deep-vein thrombosis in fractures below the knee: A Prospective Randomised Controlled Trial. J. Bone Jt. Surg. Br. Vol. 2009, 91, 388–394. [Google Scholar] [CrossRef]
- Knudson, M.M.; Ikossi, D.G.; Khaw, L.; Morabito, D.; Speetzen, L.S. Thromboembolism After Trauma: An Analysis of 1602 Episodes From the American College of Surgeons National Trauma Data Bank. Ann. Surg. 2004, 240, 490–498. [Google Scholar] [CrossRef]
- Stannard, J.P.; Lopez-Ben, R.R.; Volgas, D.A.; Anderson, E.R.; Busbee, M.; Karr, D.K.; McGwin, G.R.; Alonso, J.E. Prophylaxis Against Deep-Vein Thrombosis Following Trauma: A Prospective, Randomized Comparison of Mechanical and Pharmacologic Prophylaxis. J. Bone Jt. Surg. 2006, 88, 261–266. [Google Scholar] [CrossRef]
- Whiting, P.S.; White-Dzuro, G.A.; Greenberg, S.E.; VanHouten, J.P.; Avilucea, F.R.; Obremskey, W.T.; Sethi, M.K. Risk Factors for Deep Venous Thrombosis Following Orthopaedic Trauma Surgery: An Analysis of 56,000 patients. Arch. Trauma Res. 2016, 5, e32915. [Google Scholar] [CrossRef] [PubMed]
- Barco, S.; Mahmoudpour, S.H.; Valerio, L.; Klok, F.A.; Münzel, T.; Middeldorp, S.; Ageno, W.; Cohen, A.T.; Hunt, B.J.; Konstantinides, S.V. Trends in mortality related to pulmonary embolism in the European Region, 2000–2015: Analysis of vital registration data from the WHO Mortality Database. Lancet Respir. Med. 2020, 8, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.T.; Agnelli, G.; Anderson, F.A.; Arcelus, J.; Bergqvist, D.; Brecht, J.G.; Greer, I.A.; Heit, J.A.; Hutchinson, J.L.; Kakkar, A.K.; et al. Venous thromboembolism (VTE) in Europe: The number of VTE events and associated morbidity and mortality. Thromb. Haemost. 2007, 98, 756–764. [Google Scholar] [CrossRef]
- Meinberg, E.; Agel, J.; Roberts, C.; Karam, M.; Kellam, J. Fracture and Dislocation Classification Compendium—2018. J. Orthop. Trauma 2018, 32, S1–S10. [Google Scholar] [CrossRef]
- Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). S3-Leitlinie Prophylaxe der Venösen Thromboembolie (VTE)—2. Komplett Überarbeitete AUFLAGE (Stand 15.10.2015) [Internet]. 2015. Available online: https://register.awmf.org/de/leitlinien/detail/003-001 (accessed on 20 December 2024).
- Schellong, S.M. Die Ultraschalluntersuchung der Beinvenen bei Verdacht auf Venenthrombose—Eine Übersicht. Z. Für Gefäßmedizin 2009, 6, 5–10. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Daabiss, M. American Society of Anaesthesiologists physical status classification. Indian J. Anaesth. 2011, 55, 111. [Google Scholar] [CrossRef]
- Oestern, H.J.; Tscherne, H. Pathophysiology and Classification of Soft Tissue Injuries Associated with Fractures. In Fractures with Soft Tissue Injuries [Internet]; Tscherne, H., Gotzen, L., Eds.; Springer: Berlin/Heidelberg, Germany, 1984; pp. 1–9. ISBN 978-3-540-13082-6/978-3-642-69499-8. Available online: http://link.springer.com/10.1007/978-3-642-69499-8_1 (accessed on 12 June 2024).
- Henkelmann, R.; Glaab, R.; Mende, M.; Ull, C.; Braun, P.-J.; Katthagen, C.; Gensior, T.J.; Frosch, K.-H.; Hepp, P.; Committee TRAUMA of the AGA-Society for Arthroscopy and Joint Surgery. Impact of surgical site infection on patients’ outcome after fixation of tibial plateau fractures: A retrospective multicenter study. BMC Musculoskelet. Disord. 2021, 22, 531. [Google Scholar] [CrossRef]
- Cong, Y.; Huang, H.; Zhang, B.-F.; Deng, H.; Lei, J.; Ke, C.; Han, S.; Zhang, K.; Wang, P. The Correlation Between Preoperative Lower Extremity Deep Vein Thrombosis (DVT) and the Time from Injury to Surgery (TFITS). Clin. Appl. Thromb. Hemost. 2022, 28, 10760296221108961. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.; Wang, B.; Li, Q.; Zhang, Y.; Xie, W. Study on the Risk Factors of Preoperative Deep Vein Thrombosis (DVT) in Patients With Lower Extremity Fracture. Clin. Appl. Thromb. Hemost. 2021, 27, 10760296211002900. [Google Scholar] [CrossRef] [PubMed]
- Brill, J.B.; Badiee, J.; Zander, A.L.; Wallace, J.D.; Lewis, P.R.; Sise, M.J.; Bansal, V.; Shackford, S.R. The rate of deep vein thrombosis doubles in trauma patients with hypercoagulable thromboelastography. J. Trauma Acute Care Surg. 2017, 83, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Chen, X.; Wang, Y.; Li, L. Analysis of the occurrence of deep venous thrombosis in lower extremity fractures: A clinical study. Pak. J. Med. Sci. 2018, 34, 828–832. [Google Scholar] [CrossRef]
- Cai, X.; Wang, Z.; Wang, X.-L.; Xue, H.-Z.; Li, Z.-J.; Jiang, W.-Q.; Nian, Y.-W.; Zhu, Y.-J.; Zhang, K.; Huang, W. Correlation Between the Fracture Line Plane and Perioperative Deep Vein Thrombosis in Patients with Tibial Fracture. Clin. Appl. Thromb. Hemost. 2021, 27, 107602962110672. [Google Scholar] [CrossRef]
- Jørgensen, C.T.; Tavoly, M.; Førsund, E.; Pettersen, H.H.; Tjønnfjord, E.; Ghanima, W.; Brækkan, S.K. Incidence of bleeding and recurrence in isolated distal deep vein thrombosis: Findings from the Venous Thrombosis Registry in Østfold Hospital. J. Thromb. Haemost. 2023, 21, 2824–2832. [Google Scholar] [CrossRef]
- Kahn, S.R.; Comerota, A.J.; Cushman, M.; Evans, N.S.; Ginsberg, J.S.; Goldenberg, N.A.; Gupta, D.K.; Prandoni, P.; Vedantham, S.; Walsh, M.E.; et al. The Postthrombotic Syndrome: Evidence-Based Prevention, Diagnosis, and Treatment Strategies: A Scientific Statement From the American Heart Association. Circulation 2014, 130, 1636–1661. [Google Scholar] [CrossRef]
- Nosaka, M.; Ishida, Y.; Kimura, A.; Kondo, T. Time-dependent appearance of intrathrombus neutrophils and macrophages in a stasis-induced deep vein thrombosis model and its application to thrombus age determination. Int. J. Leg. Med. 2009, 123, 235–240. [Google Scholar] [CrossRef]
- Czaplicki, C.; Albadawi, H.; Partovi, S.; Gandhi, R.T.; Quencer, K.; Deipolyi, A.R.; Oklu, R. Can thrombus age guide thrombolytic therapy? Cardiovasc. Diagn. Ther. 2017, 7 (Suppl. S3), S186–S196. [Google Scholar] [CrossRef]
- Liu, D.; Zhu, Y.; Chen, W.; Li, J.; Zhao, K.; Zhang, J.; Meng, H.; Zhang, Y. Relationship between the inflammation/immune indexes and deep venous thrombosis (DVT) incidence rate following tibial plateau fractures. J. Orthop. Surg. Res. 2020, 15, 241. [Google Scholar] [CrossRef]
- Auer, R.; Riehl, J. The incidence of deep vein thrombosis and pulmonary embolism after fracture of the tibia: An analysis of the National Trauma Databank. J. Clin. Orthop. Trauma 2017, 8, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Yan, X.; Fei, C.; Zhang, B.; Xing, J.; Zhang, K.; Kandemir, U. Incidence and risk factors of clinically important venous thromboembolism in tibial plateau fractures. Sci. Rep. 2022, 12, 20206. [Google Scholar] [CrossRef]
- Xu, Y.; Li, Q.; Shen, T.; Su, P.; Zhu, Y. An efficacy analysis of surgical timing and procedures for high-energy complex tibial plateau fractures. Orthop. Surg. 2013, 5, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Zhang, S.; Qiu, X.; Huang, H.; Sheng, H.; Zhang, Y.; Chang, J.; Kuang, J.; Yang, J. Optimal surgical timing and approach for tibial plateau fracture. Technol. Health Care 2022, 30, 545–551. [Google Scholar] [CrossRef]
- Patterson, J.T.; Morshed, S. Chemoprophylaxis for Venous Thromboembolism in Operative Treatment of Fractures of the Tibia and Distal Bones: A Systematic Review and Meta-analysis. J. Orthop. Trauma 2017, 31, 453–460. [Google Scholar] [CrossRef] [PubMed]
| Unit/Specification | Thrombosis n = 17 | No Thrombosis n = 55 | Total n = 72 | p-Value | |
|---|---|---|---|---|---|
| Age | years | 53.1 ± 14.7 | 52.1 ± 14.9 | 52.3 ± 14.7 | 0.65 |
| BMI | kg/m2 | 24.5 [6] | 26 [8] | 25.6 [7] | 0.17 |
| Charlson Comorbidity Index * | 1.5 ± 1.2 | 1.6 ± 1.5 | 1.5 ± 1.4 | ||
| Sex | female/male | 11/6 (64.7/35.3) | 29/26 (52.7/47.3) | 40/32 (55.6/44.4) | 0.39 |
| Weight class | underweight | 1 (5.9) | 0 (0) | 1 (1.4) | 0.44 |
| normal weight | 10 (58.8) | 24 (43.6) | 34 (47.2) | ||
| overweight | 4 (23.5) | 14 (25.5) | 18 (25) | ||
| obesity I | 1 (5.9) | 9 (16.4) | 10 (13.9) | ||
| obesity II | 1 (5.9) | 5 (9.1) | 6 (8.3) | ||
| obesity III | 0 (0) | 3 (5.5) | 3 (4.2) | ||
| ASA classification score | I | 2 (11.8) | 8 (14.5) | 10 (13.9) | 0.58 |
| II | 12 (70.6) | 42 (76.4) | 54 (75) | ||
| III | 3 (17.6) | 5 (9.1) | 8 (11.1) | ||
| Patient characteristics | |||||
| thromboembolic events in the past | 0 (0) | 8 (14.5) | 8 (11.1) | 0.19 | |
| cancer | 0 (0) | 0 (0) | 0 (0) | n.a. | |
| coagulopathy | 2 (11.8) | 0 (0) | 2 (2.8) | 0.053 | |
| long-term anticoagulant medication intake | 0 (0) | 6 (10.9) | 6 (8.3) | 0.33 | |
| Diabetes mellitus | 1 (5.9) | 7 (12.7) | 8 (11.1) | 0.67 | |
| arterial hypertension | 5 (29.4) | 21 (38.2) | 26 (36.1) | 0.51 | |
| dyslipidemia | 2 (11.8) | 6 (10.9) | 8 (11.1) | 1 | |
| alcohol abuse | 1 (5.9) | 3 (5.5) | 4 (5.6) | 1 | |
| drug abuse | 0 (0) | 3 (5.5) | 3 (4.2) | 1 | |
| nicotine abuse | 3 (17.6) | 15 (27.3) | 18 (25) | 0.53 | |
| Unit/Specification | Thrombosis n = 17 | No Thrombosis n = 55 | Total n = 72 | p-Value | |
|---|---|---|---|---|---|
| time from injury to surgery | days | 20.1 ± 3.9 | 8 ± 3.5 | 9 ± 9 | <0.001 |
| time from admission to surgery | days | 18.8 ± 3.9 | 7.1 ± 3.5 | 9.85 ± 6.1 | <0.001 |
| time from injury to DUS | days | 8 [7] | 5 [2] | 6 [3] | 0.003 |
| time from DUS to surgery | days | 13 [7] | 1 [1] | 1 [5] | <0.001 |
| duration of surgery | minutes | 202 ± 48 | 199 ± 69 | 200 ± 64 | 0.69 |
| LOS in hospital | days | 29 [5] | 17 [10] | 19 [15] | <0.001 |
| mechanism of trauma | high-energy | 16 (94.1) | 44 (80) | 60 (83.3) | 0.27 |
| low-energy | 1 (5.9) | 11 (20) | 12 (16.7) | ||
| transfer from a different hospital | 10 (58.8) | 30 (54.5) | 40 (55.6) | 0.76 | |
| dislocation | 11 (64.7) | 28 (50.9) | 39 (54.2) | 0.32 | |
| site of injury | right | 8 (47.1) | 24 (43.6) | 32 (44.4) | 0.80 |
| left | 9 (52.9) | 31 (56.4) | 40 (55.6) | ||
| AO/OTA type | B1 | 0 (0) | 4 (7.3) | 4 (5.6) | 0.21 |
| B3 | 3 (17.6) | 20 (36.4) | 23 (31.9) | ||
| C1 | 0 (0) | 2 (3.6) | 2 (2.8) | ||
| C3 | 14 (82.4) | 29 (52.7) | 43 (59.7) | ||
| open versus closed fracture | open | 2 (11.8) | 3 (5.5) | 5 (6.9) | 0.59 |
| closed | 15 (88.2) | 52 (94.5) | 67 (93.1) | ||
| soft tissue injury (open fracture) | II | 1 (5.9) | 2 (3.6) | 3 (4.2) | 1 |
| III | 1 (5.9) | 1 (1.8) | 2 (2.8) | ||
| soft tissue injury (closed fracture) | I | 5 (29.4) | 22 (40) | 27 (37.5) | 0.19 |
| II | 8 (47.1) | 27 (49.1) | 35 (48.6) | ||
| III | 2 (11.8) | 1 (1.8) | 3 (4.2) | ||
| no information | 0 (0) | 2 (3.6) | 2 (2.8) | ||
| affected condyles | unicondylar | 11 (64.7) | 42 (76.4) | 53 (73.6) | 0.36 |
| bicondylar | 6 (35.3) | 13 (23.6) | 19 (26.4) | ||
| compartment syndrome | 4 (23.5) | 2 (3.6) | 6 (8.3) | 0.025 | |
| concomitant injuries on the same leg * | none | 1 (5.9) | 22 (40) | 23 (31.9) | 0.008 |
| not relevant | 0 (0) | 0 (0) | 0 (0) | ||
| relevant | 16 (94.1) | 33 (60) | 49 (68.1) | ||
| concomitant injuries in other body regions * | none | 10 (58.8) | 38 (69.1) | 48 (66.7) | 0.61 |
| not relevant | 2 (11.8) | 4 (7.3) | 6 (8.3) | ||
| relevant | 5 (29.4) | 13 (23.6) | 18 (25) | ||
| form of immobilisation | external fixator | 14 (82.4) | 35 (63.6) | 49 (68.1) | 0.15 |
| splint | 3 (17.6) | 20 (36.4) | 23 (31.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hermel, H.; Yacoub, S.; Souleiman, F.; Kohlmann, F.; Kühnapfel, A.; Kleber, C.; Mühlberg, K.S.; Henkelmann, R. Incidence of Unapparent Preoperative Deep Vein Thrombosis in Patients with Traumatic Intraarticular Tibial Plateau Fracture. J. Clin. Med. 2025, 14, 3490. https://doi.org/10.3390/jcm14103490
Hermel H, Yacoub S, Souleiman F, Kohlmann F, Kühnapfel A, Kleber C, Mühlberg KS, Henkelmann R. Incidence of Unapparent Preoperative Deep Vein Thrombosis in Patients with Traumatic Intraarticular Tibial Plateau Fracture. Journal of Clinical Medicine. 2025; 14(10):3490. https://doi.org/10.3390/jcm14103490
Chicago/Turabian StyleHermel, Henriette, Simon Yacoub, Firas Souleiman, Friederike Kohlmann, Andreas Kühnapfel, Christian Kleber, Katja S. Mühlberg, and Ralf Henkelmann. 2025. "Incidence of Unapparent Preoperative Deep Vein Thrombosis in Patients with Traumatic Intraarticular Tibial Plateau Fracture" Journal of Clinical Medicine 14, no. 10: 3490. https://doi.org/10.3390/jcm14103490
APA StyleHermel, H., Yacoub, S., Souleiman, F., Kohlmann, F., Kühnapfel, A., Kleber, C., Mühlberg, K. S., & Henkelmann, R. (2025). Incidence of Unapparent Preoperative Deep Vein Thrombosis in Patients with Traumatic Intraarticular Tibial Plateau Fracture. Journal of Clinical Medicine, 14(10), 3490. https://doi.org/10.3390/jcm14103490






