Comparative Analysis of SYNTAX and BCIS Jeopardy Score of Diabetics Versus Non-Diabetic Patients with Complex Coronary Artery Disease
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. PCI Procedure
2.3. Study Endpoints
2.4. Statistical Analysis
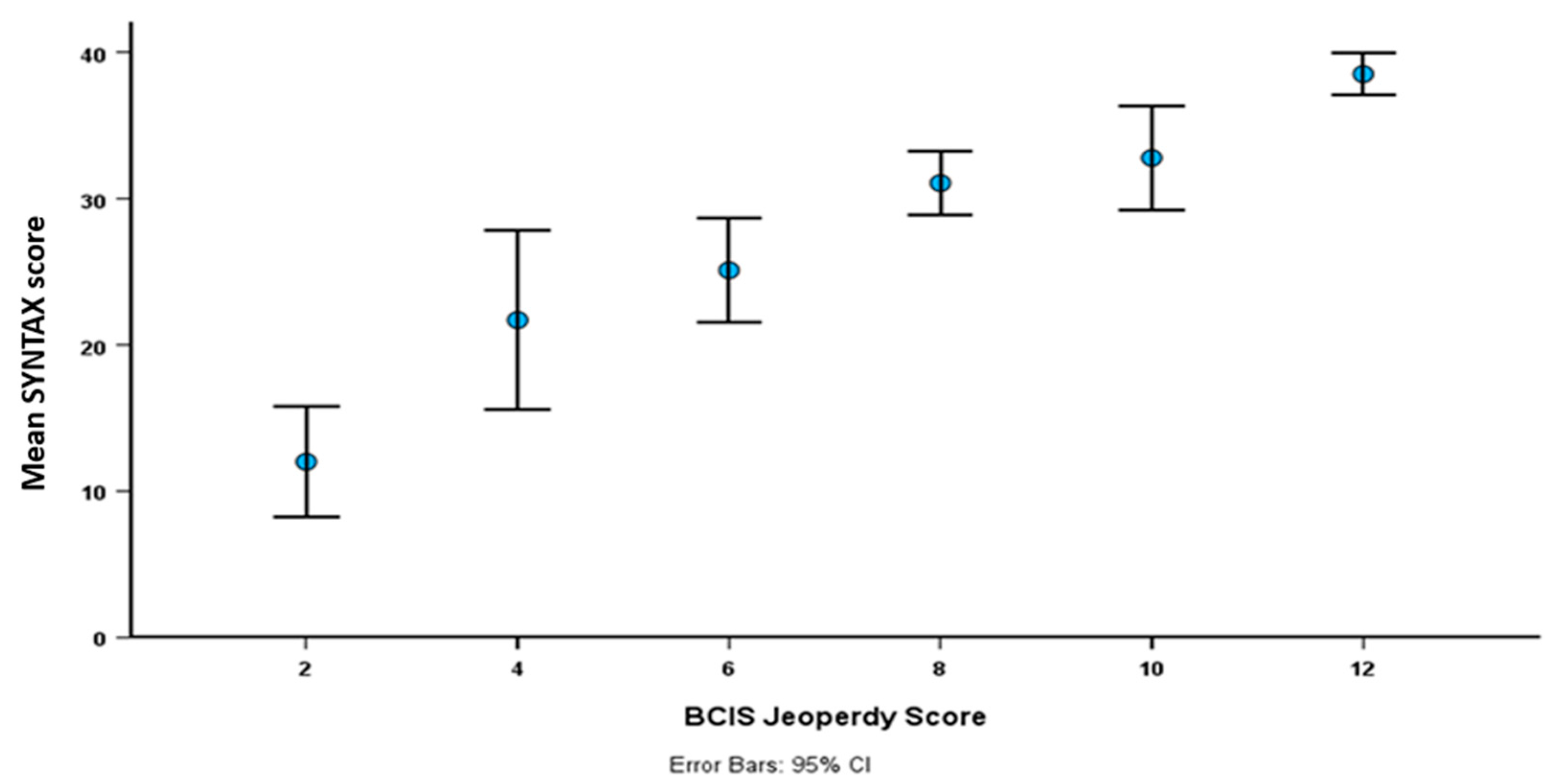
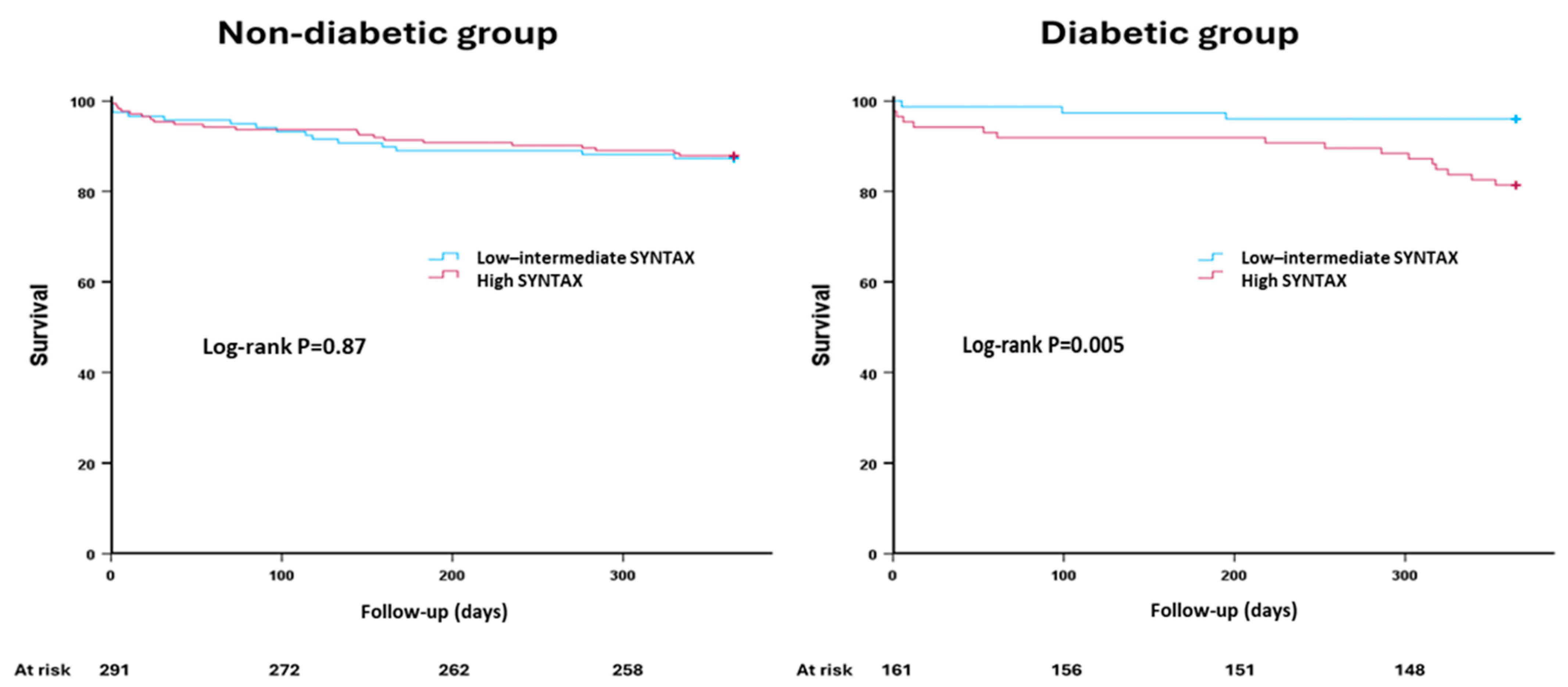
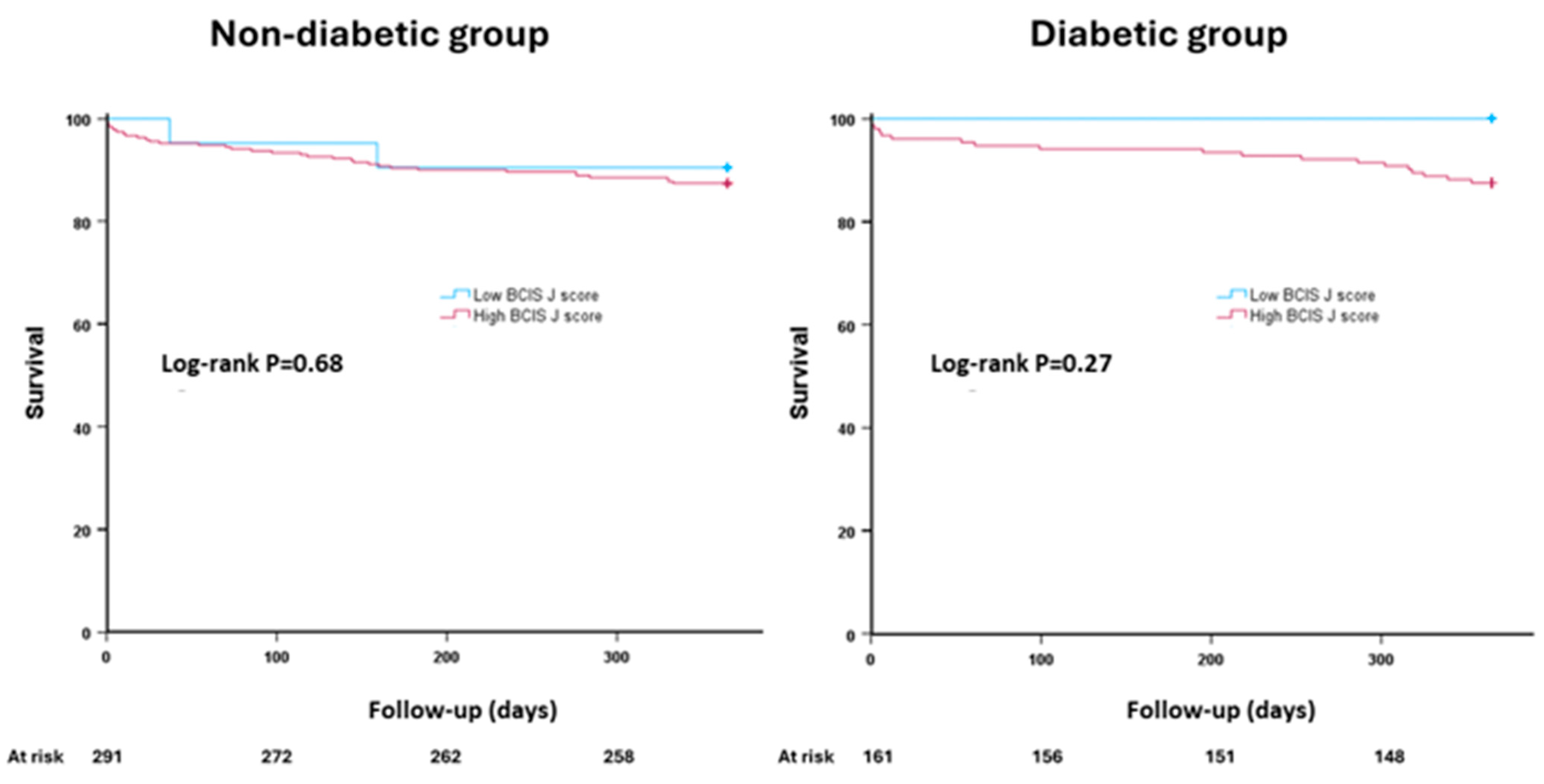
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Wykrzykowska, J.J.; Garg, S.; Girasis, C.; de Vries, T.; Morel, M.A.; van Es, G.A.; Buszman, P.; Linke, A.; Ischinger, T.; Klauss, V.; et al. Value of the SYNTAX score for risk assessment in the all-comers population of the randomized multicenter LEADERS (Limus Eluted from A Durable versus ERodable Stent coating) trial. J. Am. Coll. Cardiol. 2010, 56, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Serruys, P.W.; Morice, M.C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Stahle, E.; Feldman, T.E.; van den Brand, M.; Bass, E.J.; et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef] [PubMed]
- De Silva, K.; Morton, G.; Sicard, P.; Chong, E.; Indermuehle, A.; Clapp, B.; Thomas, M.; Redwood, S.; Perera, D. Prognostic utility of BCIS myocardial jeopardy score for classification of coronary disease burden and completeness of revascularization. Am. J. Cardiol. 2013, 111, 172–177. [Google Scholar] [CrossRef]
- Lee, J.; Ahn, J.M.; Kim, J.H.; Jeong, Y.J.; Hyun, J.; Yang, Y.; Lee, J.S.; Park, H.; Kang, D.Y.; Lee, P.H.; et al. Prognostic Effect of the SYNTAX Score on 10-Year Outcomes After Left Main Coronary Artery Revascularization in a Randomized Population: Insights From the Extended PRECOMBAT Trial. J. Am. Heart Assoc. 2021, 10, e020359. [Google Scholar] [CrossRef]
- Califf, R.M.; Phillips, H.R., 3rd; Hindman, M.C.; Mark, D.B.; Lee, K.L.; Behar, V.S.; Johnson, R.A.; Pryor, D.B.; Rosati, R.A.; Wagner, G.S.; et al. Prognostic value of a coronary artery jeopardy score. J. Am. Coll. Cardiol. 1985, 5, 1055–1063. [Google Scholar] [CrossRef]
- Perera, D.; Clayton, T.; O’Kane, P.D.; Greenwood, J.P.; Weerackody, R.; Ryan, M.; Morgan, H.P.; Dodd, M.; Evans, R.; Canter, R.; et al. Percutaneous Revascularization for Ischemic Left Ventricular Dysfunction. N. Engl. J. Med. 2022, 387, 1351–1360. [Google Scholar] [CrossRef]
- Perera, D.; Clayton, T.; Petrie, M.C.; Greenwood, J.P.; O’Kane, P.D.; Evans, R.; Sculpher, M.; McDonagh, T.; Gershlick, A.; de Belder, M.; et al. Percutaneous Revascularization for Ischemic Ventricular Dysfunction: Rationale and Design of the REVIVED-BCIS2 Trial: Percutaneous Coronary Intervention for Ischemic Cardiomyopathy. JACC Heart Fail. 2018, 6, 517–526. [Google Scholar] [CrossRef]
- Fuster, V.; Farkouh, M.E. Main Results of the Future REvascularization evaluation in patients with diabetes mellitus: Optimal management of multivessel disease (FREEDOM) trial. Circulation 2012, 126, 2779. [Google Scholar] [CrossRef]
- Esper, R.B.; Ribeiro, E.E.; Hueb, W.; Domanski, M.; Hamza, T.; Siami, S.; Farkouh, M.E.; Fuster, V. The role of the syntax score in predicting clinical outcome in diabetic patients after percutaneous coronary intervention and coronary artery bypass graft: A freedom trial sub-analysis. Circulation 2017, 136, A19046. [Google Scholar]
- Alkhalil, M.; McCune, C.; McClenaghan, L.; Mailey, J.; Collins, P.; Kearney, A.; Todd, M.; McKavanagh, P. Clinical Outcomes of Deferred Revascularisation Using Fractional Flow Reserve in Diabetic Patients. Cardiovasc. Revasc. Med. 2020, 21, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Fearon, W.F.; Zimmermann, F.M.; Ding, V.Y.; Takahashi, K.; Piroth, Z.; van Straten, A.H.M.; Szekely, L.; Davidavicius, G.; Kalinauskas, G.; Mansour, S.; et al. Outcomes after fractional flow reserve-guided percutaneous coronary intervention versus coronary artery bypass grafting (FAME 3): 5-year follow-up of a multicentre, open-label, randomised trial. Lancet 2025, 405, 1481–1490. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.H.; Park, T.K.; Song, Y.B.; Lee, J.M.; Lee, J.Y.; Lee, S.J.; Lee, S.Y.; Kim, S.M.; Yun, K.H.; Cho, J.Y.; et al. Intravascular Imaging and Angiography Guidance in Complex Percutaneous Coronary Intervention Among Patients With Diabetes: A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw. Open 2024, 7, e2417613. [Google Scholar] [CrossRef] [PubMed]
- Kuzemczak, M.; Ibrahem, A.; Alkhalil, M. Colchicine in Patients with Coronary Artery Disease with or Without Diabetes Mellitus: A Meta-analysis of Randomized Clinical Trials. Clin. Drug Investig. 2021, 41, 667–674. [Google Scholar] [CrossRef]
- Santos-Pardo, I.; Andersson Franko, M.; Lagerqvist, B.; Ritsinger, V.; Eliasson, B.; Witt, N.; Norhammar, A.; Nystrom, T. Glycemic Control and Coronary Stent Failure in Patients With Type 2 Diabetes Mellitus. J. Am. Coll. Cardiol. 2024, 84, 260–272. [Google Scholar] [CrossRef]
- Farag, M.; Al-Atta, A.; Abdalazeem, I.; Salim, T.; Alkhalil, M.; Egred, M. Clinical outcomes of percutaneous coronary intervention in high-risk patients turned down for surgical revascularization. Catheter. Cardiovasc. Interv. 2022, 100, 360–366. [Google Scholar] [CrossRef]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthelemy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. The Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef]
- Esper, R.B.; Farkouh, M.E.; Ribeiro, E.E.; Hueb, W.; Domanski, M.; Hamza, T.H.; Siami, F.S.; Godoy, L.C.; Mathew, V.; French, J.; et al. SYNTAX Score in Patients With Diabetes Undergoing Coronary Revascularization in the FREEDOM Trial. J. Am. Coll. Cardiol. 2018, 72, 2826–2837. [Google Scholar] [CrossRef]
- Farkouh, M.E.; Domanski, M.; Sleeper, L.A.; Siami, F.S.; Dangas, G.; Mack, M.; Yang, M.; Cohen, D.J.; Rosenberg, Y.; Solomon, S.D.; et al. Strategies for multivessel revascularization in patients with diabetes. N. Engl. J. Med. 2012, 367, 2375–2384. [Google Scholar] [CrossRef]
- Abdallah, M.S.; Wang, K.; Magnuson, E.A.; Spertus, J.A.; Farkouh, M.E.; Fuster, V.; Cohen, D.J. Quality of life after PCI vs CABG among patients with diabetes and multivessel coronary artery disease: A randomized clinical trial. JAMA 2013, 310, 1581–1590. [Google Scholar] [CrossRef] [PubMed]
- Gebert, Z.M.; Kwiecinski, J.; Weir-McCall, J.R.; Adamson, P.D.; Mills, N.L.; Roditi, G.; van Beek, E.J.R.; Nicol, E.D.; Berman, D.S.; Slomka, P.J.; et al. Impact of diabetes mellitus on coronary artery plaque characteristics and outcomes in the SCOT-HEART trial. J. Cardiovasc. Comput. Tomogr. 2025, 19, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Latif, A.; Ahsan, M.J.; Kabach, A.; Kapoor, V.; Mirza, M.; Ahsan, M.Z.; Kearney, K.; Panaich, S.; Cohen, M.; Goldsweig, A.M. Impact of Diabetes Mellitus on Outcomes of Percutaneous Coronary Intervention in Chronic Total Occlusions: A Systematic Review and Meta-Analysis. Cardiovasc. Revasc. Med. 2022, 37, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Parachini, J.R.; Karatasakis, A.; Karmpaliotis, D.; Alaswad, K.; Jaffer, F.A.; Yeh, R.W.; Patel, M.; Bahadorani, J.; Doing, A.; Nguyen-Trong, P.K.; et al. Impact of diabetes mellitus on acute outcomes of percutaneous coronary intervention in chronic total occlusions: Insights from a US multicentre registry. Diabet. Med. 2017, 34, 558–562. [Google Scholar] [CrossRef]
- Konstantinidis, N.V.; Werner, G.S.; Deftereos, S.; Di Mario, C.; Galassi, A.R.; Buettner, J.H.; Avran, A.; Reifart, N.; Goktekin, O.; Garbo, R.; et al. Temporal Trends in Chronic Total Occlusion Interventions in Europe. Circ. Cardiovasc. Interv. 2018, 11, e006229. [Google Scholar] [CrossRef]
- Mauriello, A.; Ascrizzi, A.; Molinari, R.; Falco, L.; Caturano, A.; D’Andrea, A.; Russo, V. Pharmacogenomics of Cardiovascular Drugs for Atherothrombotic, Thromboembolic and Atherosclerotic Risk. Genes 2023, 14, 2057. [Google Scholar] [CrossRef]
| Whole Cohort (n = 452) | Non-Diabetic (n = 291) | Diabetic (n = 161) | p Value | |
|---|---|---|---|---|
| Age | 72 ± 11 | 73 ± 11 | 70 ± 11 | 0.001 |
| Female gender | 132 (29%) | 79 (27%) | 53 (33%) | 0.20 |
| BMI | 29 ± 6 | 27 ± 5 | 31 ± 7 | <0.001 |
| Stable angina | 206 (46%) | 137 (47%) | 69 (43%) | 0.39 |
| Previous MI | 115 (25%) | 70 (24%) | 45 (28%) | 0.36 |
| PVD | 77 (17%) | 44 (15%) | 33 (21%) | 0.14 |
| Previous CVA | 47 (11%) | 38 (13%) | 9 (6%) | 0.013 |
| Previous CABG | 35 (8%) | 21 (7%) | 14 (9%) | 0.56 |
| COPD | 76 (17%) | 58 (20%) | 18 (11%) | 0.043 |
| Preserved LV | 205 (52%) | 136 (53%) | 69 (51%) | 0.65 |
| CKD | 159 (36%) | 91 (32%) | 68 (43%) | 0.022 |
| Euro Score II | 6 ± 6 | 6 ± 6 | 7 ± 7 | 0.24 |
| Left main | 190 (42%) | 127 (44%) | 63 (39%) | 0.35 |
| Number of lesions | 2 (1–3) | 2 (1–3) | 2 (1–3) | 0.85 |
| Number of stents | 3 (2–4) | 2 (1–3) | 2 (1–3) | 0.93 |
| SYNTAX score | 33 ± 13 | 34 ± 13 | 33 ± 12 | 0.41 |
| SYNTAX II score | 30 ± 17 | 31 ± 16 | 28 ± 17 | 0.08 |
| High SYNTAX | 259 (57%) | 173 (60%) | 86 (53%) | 0.21 |
| BCIS-JS | 12 (8–12) | 12 (8–12) | 12 (8–12) | 0.99 |
| High BCIS-JS | 422 (93%) | 270 (93%) | 152 (94%) | 0.51 |
| Optimal medical treatment | 305 (67%) | 185 (64%) | 120 (75%) | 0.12 |
| Whole Cohort (n = 452) | Non-Diabetic (n = 291) | Diabetic (n = 161) | p Value | |
|---|---|---|---|---|
| Procedural complications | 29 (6.4%) | 18 (6.2%) | 11 (6.8%) | 0.79 |
| In-hospital death | 10 (2.2%) | 7 (2.4%) | 3 (1.9%) | 0.71 |
| Death at one month | 19 (4.2%) | 6 (3.7%) | 13 (4.5%) | 0.71 |
| One year mortality | 55 (12.2%) | 36 (12.4%) | 19 (11.8%) | 0.86 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdeldayem, T.; Memon, S.; Omari, M.; Farag, M.; Al-Atta, A.; Ibrahem, A.; Salim, T.; Bawamia, B.; Egred, M.; Alkhalil, M. Comparative Analysis of SYNTAX and BCIS Jeopardy Score of Diabetics Versus Non-Diabetic Patients with Complex Coronary Artery Disease. J. Clin. Med. 2025, 14, 3433. https://doi.org/10.3390/jcm14103433
Abdeldayem T, Memon S, Omari M, Farag M, Al-Atta A, Ibrahem A, Salim T, Bawamia B, Egred M, Alkhalil M. Comparative Analysis of SYNTAX and BCIS Jeopardy Score of Diabetics Versus Non-Diabetic Patients with Complex Coronary Artery Disease. Journal of Clinical Medicine. 2025; 14(10):3433. https://doi.org/10.3390/jcm14103433
Chicago/Turabian StyleAbdeldayem, Tarek, Saif Memon, Muntaser Omari, Mohamed Farag, Ayman Al-Atta, Abdalazeem Ibrahem, Tarik Salim, Bilal Bawamia, Mohaned Egred, and Mohammad Alkhalil. 2025. "Comparative Analysis of SYNTAX and BCIS Jeopardy Score of Diabetics Versus Non-Diabetic Patients with Complex Coronary Artery Disease" Journal of Clinical Medicine 14, no. 10: 3433. https://doi.org/10.3390/jcm14103433
APA StyleAbdeldayem, T., Memon, S., Omari, M., Farag, M., Al-Atta, A., Ibrahem, A., Salim, T., Bawamia, B., Egred, M., & Alkhalil, M. (2025). Comparative Analysis of SYNTAX and BCIS Jeopardy Score of Diabetics Versus Non-Diabetic Patients with Complex Coronary Artery Disease. Journal of Clinical Medicine, 14(10), 3433. https://doi.org/10.3390/jcm14103433







