Functional Recovery Predictors in Hip Fractures: Insights from a Community Clinical Pathway
Abstract
1. Introduction
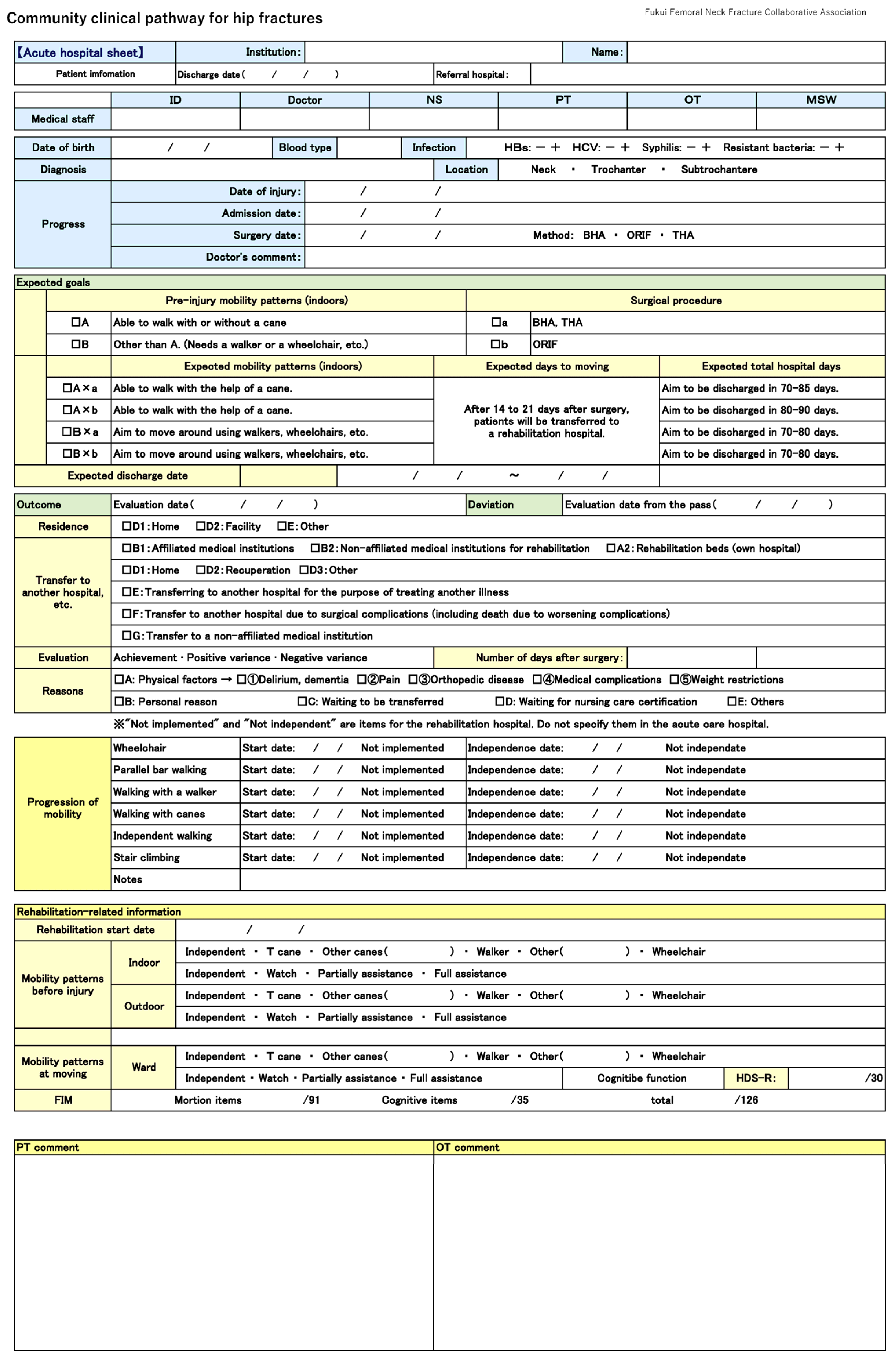
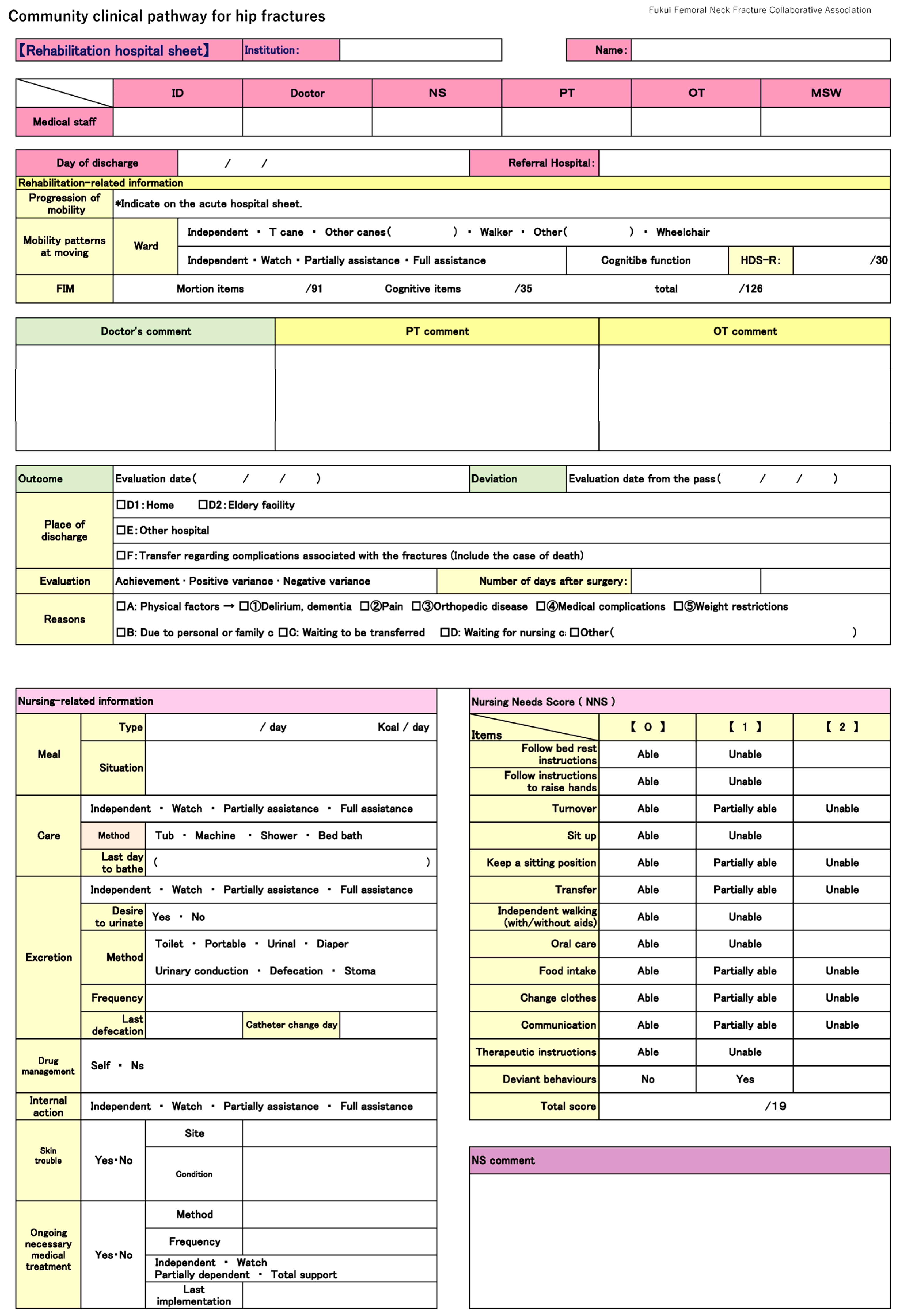
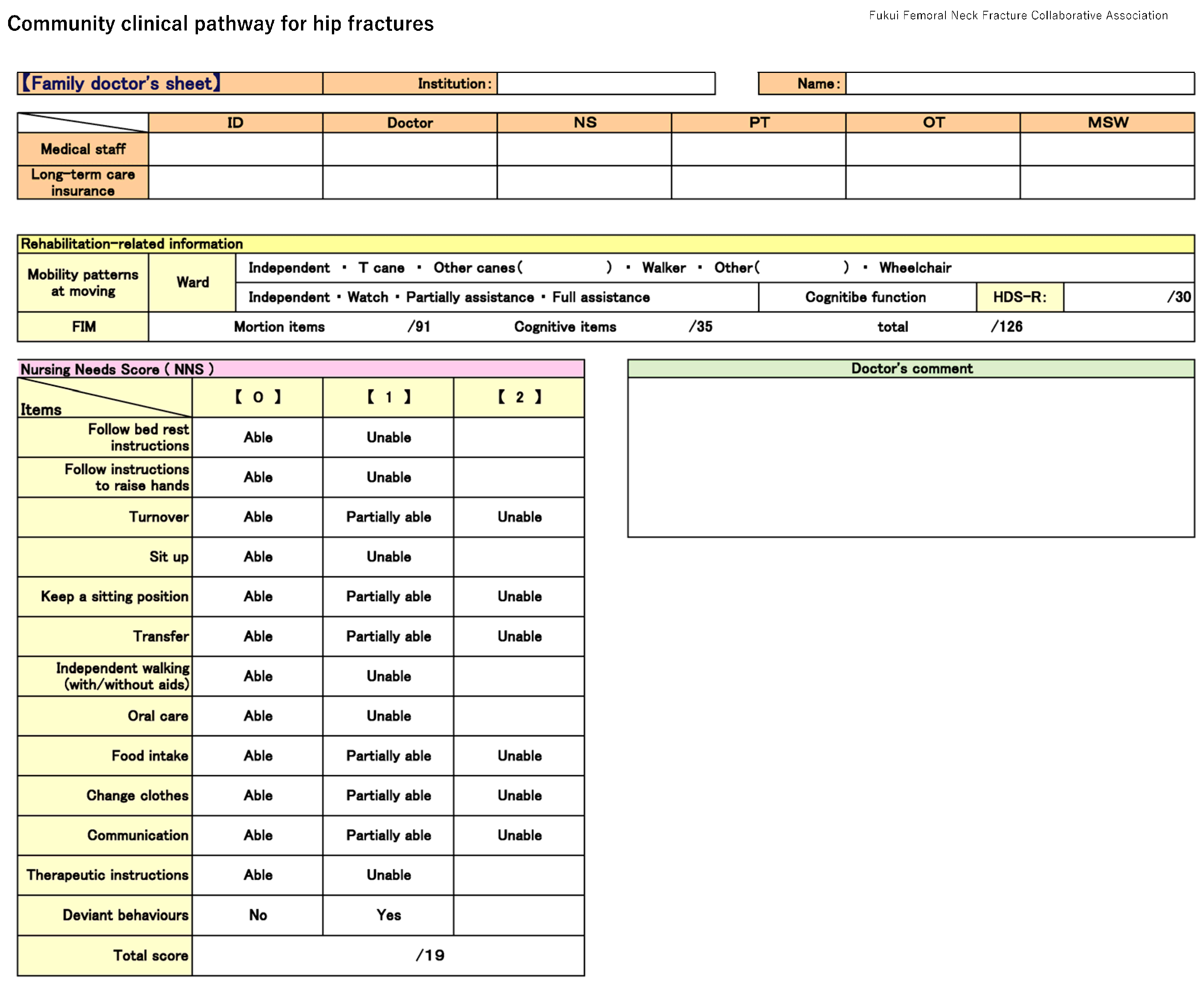
2. Materials and Methods
2.1. Study Population and Assessment Items
2.2. Clinical Assessment
2.3. Statistical Analysis
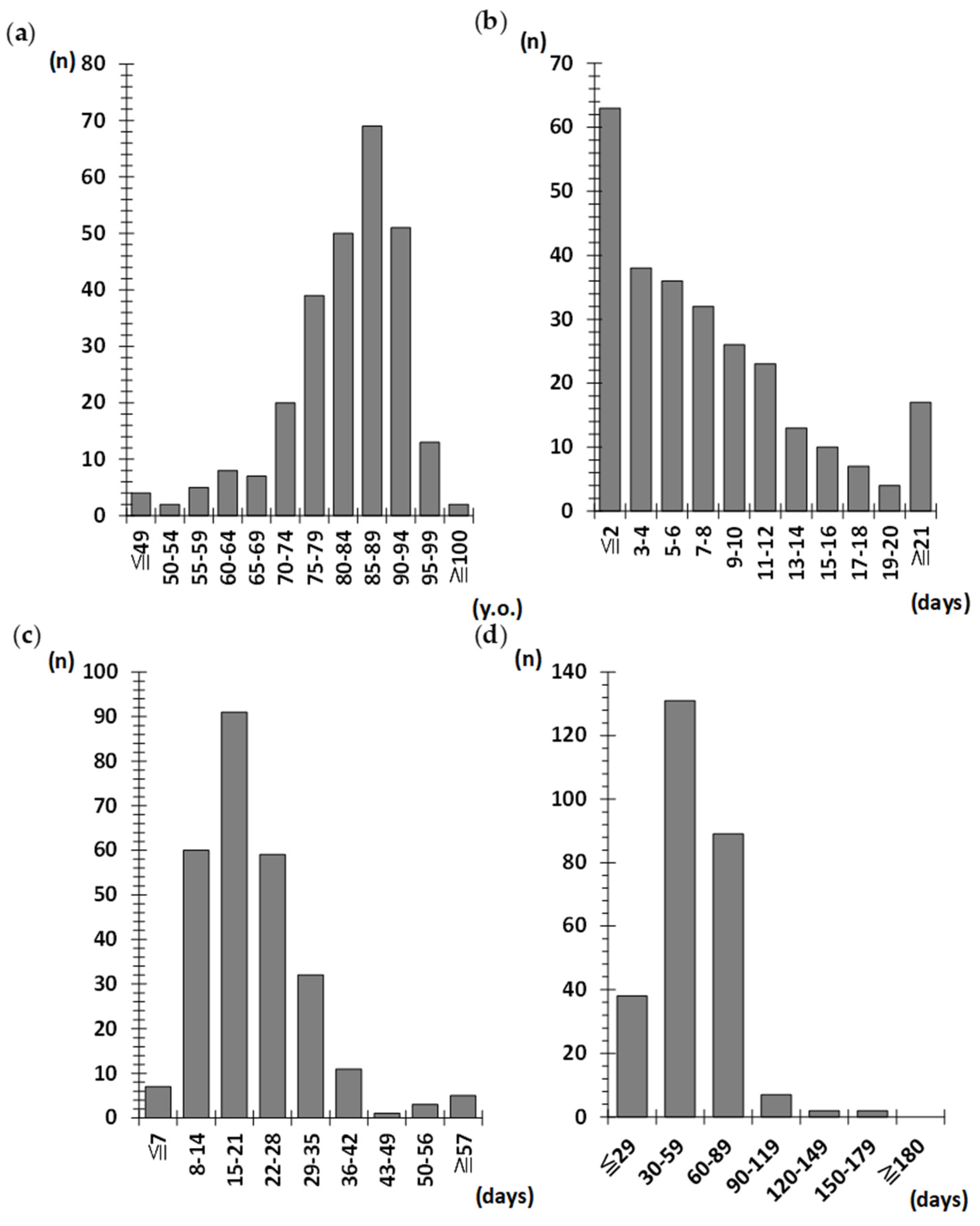
3. Results
3.1. Patient Characteristics and Timing of Surgery
3.2. Changes in Walking Ability
3.3. Factors Influencing Mobility
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADL | Activities of daily living |
| BHA | Bipolar head arthroplasty |
| FAC | Functional Ambulation Category |
| FIM | Functional Independence Measure |
| FLS | Fracture Liaison Service |
| JOANAR | Japanese Orthopaedic Association Nation Registry |
| NNS | Nursing Needs Score |
References
- The Japanese Orthopaedic Association. The Database of Japanese Orthopaedic Association National Registry (JOANR). 2023 Annual Report. 2023. Available online: https://www.joa.or.jp/joa/files/JOANR_annual_report_2023.pdf (accessed on 1 May 2025).
- Takahashi, A.; Naruse, H.; Kitade, I.; Shimada, S.; Tsubokawa, M.; Kokubo, Y.; Matsumine, A. Functional outcomes after the treatment of hip fracture. PLoS ONE 2020, 15, e0236652. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare, Japan. Comprehensive Survey of Living Conditions 2022. 2022. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa22/dl/05.pdf (accessed on 30 October 2024).
- Fragility Fracture Network Japan (FFN-Japan). About FFN-Japan. Available online: https://ffn.or.jp/about_en/ (accessed on 2 March 2025).
- AO/OTA Fracture and Dislocation Classification Compendium. 2018. Available online: https://classification.aoeducation.org/ (accessed on 2 March 2025).
- Orimo, H.; Yaegashi, Y.; Hosoi, T.; Fukushima, Y.; Onoda, T.; Hashimoto, T.; Sakata, K. Hip fracture incidence in Japan: Estimates of new patients in 2012 and 25-year trends. Osteoporos. Int. 2016, 27, 1777–1784. [Google Scholar] [CrossRef] [PubMed]
- Michaëlsson, K.; Baron, J.A.; Byberg, L.; Larsson, S.C.; Melhus, H.; Gedeborg, R. Declining hip fracture burden in Sweden 1998–2019 and consequences for projections through 2050. Sci. Rep. 2024, 14, 706. [Google Scholar] [CrossRef]
- Swayambunathan, J.; Dasgupta, A.; Rosenberg, P.S.; Hannan, M.T.; Kiel, D.P.; Bhattacharyya, T. Incidence of hip fracture over 4 decades in the Framingham heart study. JAMA Intern. Med. 2020, 180, 1225–1231. [Google Scholar] [CrossRef]
- Remily, E.A.; Mohamed, N.S.; Wilkie, W.A.; Mahajan, A.K.; Patel, N.G.; Andrews, T.J.; Nace, J.; Delanois, R.E. Hip fracture trends in America between 2009 and 2016. Geriatr. Orthop. Surg. Rehabil 2020, 28, 2151459320929581. [Google Scholar] [CrossRef]
- Takusari, E.; Sakata, K.; Hashimoto, T.; Fukushima, Y.; Nakamura, T.; Orimo, H. Trends in hip fracture incidence in Japan: Estimates based on nationwide hip fracture surveys from 1992 to 2017. JBMR. Plus 2021, 5, e10428. [Google Scholar] [CrossRef] [PubMed]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights; United Nations: New York, NY, USA, 2019. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf (accessed on 2 July 2024).
- Xu, B.Y.; Yan, S.; Low, L.L.; Vasanwala, F.F.; Low, S.G. Predictors of poor functional outcomes and mortality in patients with hip fracture: A systematic review. B.M.C. Musculoskelet. Disord. 2019, 20, 568. [Google Scholar] [CrossRef]
- Buecking, B.; Bohl, K.; Eschbach, D.; Bliemel, C.; Aigner, R.; Balzer-Geldsetzer, M.; Dodel, R.; Ruchholtz, S.; Debus, F. Factors influencing the progress of mobilization in hip fracture patients during the early postsurgical period?—A prospective observational study. Arch. Gerontol. Geriatr. 2015, 60, 457–463. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Foss, N.B.; Kehlet, H. Factors with independent influence on the ‘timed up and go’ test in patients with hip fracture. Physiother. Res. Int. 2009, 14, 30–41. [Google Scholar] [CrossRef]
- Hulsbæk, S.; Larsen, R.F.; Troelsen, A. Predictors of not regaining basic mobility after hip fracture surgery. Disabil. Rehabil. 2015, 37, 1739–1744. [Google Scholar] [CrossRef]
- Cabinet Office, Government of Japan. Annual Report on the Ageing Society: Summary FY2022. 2022. Available online: https://www8.cao.go.jp/kourei/english/annualreport/2022/pdf/2022.pdf (accessed on 30 October 2024).
- Prestmo, A.; Hagen, G.; Sletvold, O.; Helbostad, J.L.; Thingstad, P.; Taraldsen, K.; Lydersen, S.; Halsteinli, V.; Saltnes, T.; Lamb, S.E.; et al. Comprehensive geriatric care for patients with hip fractures: A prospective, randomised, controlled trial. Lancet 2015, 385, 1623–1633. [Google Scholar] [CrossRef]
- Thingstad, P.; Taraldsen, K.; Saltvedt, I.; Sletvold, O.; Vereijken, B.; Lamb, S.E.; Helbostad, J.L. The long-term effect of comprehensive geriatric care on gait after hip fracture: The Trondheim Hip Fracture Trial—A randomised controlled trial. Osteoporos. Int. 2016, 27, 933–942. [Google Scholar] [CrossRef]
- Tarazona-Santabalbina, F.J.; Belenguer-Varea, Á.; Rovira, E.; Cuesta-Peredó, D. Orthogeriatric care: Improving patient outcomes. Clin. Interv. Aging 2016, 11, 843–856. [Google Scholar] [CrossRef]
- Salpakoski, A.; Törmäkangas, T.; Edgren, J.; Sihvonen, S.; Pekkonen, M.; Heinonen, A.; Pesola, M.; Kallinen, M.; Rantanen, T.; Sipilä, S. Walking recovery after a hip fracture: A prospective follow-up study among community-dwelling over 60-year old men and women. BioMed Res. Int. 2014, 2014, 289549. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.T. Factors affecting functional prognosis of patients with hip fracture. Eur. J. Phys. Rehabil. Med. 2011, 47, 257–264. [Google Scholar]
- Martín-Martín, L.M.; Arroyo-Morales, M.; Sánchez-Cruz, J.J.; Valenza-Demet, G.; Valenza, M.C.; Jiménez-Moleón, J.J. Factors influencing performance-oriented mobility after hip fracture. J. Aging Health 2015, 27, 827–842. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Hip fracture: Management. NICE Guideline [NG124]. Updated January 2023. Available online: https://www.nice.org.uk/guidance/ng124 (accessed on 30 March 2025).
- Sasabuchi, Y.; Matsui, H.; Lefor, A.K.; Fushimi, K.; Yasunaga, H. Timing of surgery for hip fractures in the elderly: A retrospective cohort study. Injury 2018, 49, 1848–1854. [Google Scholar] [CrossRef]
- Ibe, T.; Ishizaki, T.; Oku, H.; Ota, K.; Takabatake, Y.; Iseda, A.; Ishikawa, Y.; Ueda, A. Predictors of pressure ulcer and physical restraint prevalence in Japanese acute care units. Jpn. J. Nurs. Sci. 2008, 5, 91–98. [Google Scholar] [CrossRef]
- Ariza-Vega, P.; Lozano-Lozano, M.; Olmedo-Requena, R.; Martín-Martín, L.; Jiménez-Moleón, J.J. Influence of cognitive impairment on mobility recovery of patients with hip fracture. Am. J. Phys. Med. Rehabil. 2017, 96, 109–115. [Google Scholar] [CrossRef]
- Jones, C.A.; Jhangri, G.S.; Feeny, D.H.; Beaupre, L.A. Cognitive status at hospital admission: Postoperative trajectory of functional recovery for hip fracture. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 61–67. [Google Scholar] [CrossRef]
- Uriz-Otano, F.; Uriz-Otano, J.I.; Malafarina, V. Factors associated with short-term functional recovery in elderly people with a hip fracture. Influence of cognitive impairment. J. Am. Med. Dir. Assoc. 2015, 16, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, M.; Goto, E.; Shin, J.H.; Imanaka, Y. Regional disparities in Dementia-free Life Expectancy in Japan: An ecological study, using the Japanese long-term care insurance claims database. PLoS ONE 2023, 18, e0280299. [Google Scholar] [CrossRef] [PubMed]
- Tolea, M.I.; Morris, J.C. Trajectory of mobility decline by type of dementia, Galvin JE. Alzheimer Dis. Assoc. Disord. 2016, 30, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Lynds, M.E.; Arnold, C.M. Fall risk screening and assessment for people living with dementia: A scoping review. J. Appl. Gerontol. 2023, 42, 2025–2035. [Google Scholar] [CrossRef]
- Rm, A.M.; Ekholm, A.; Zander, V. Preventing falls and malnutrition among older adults in municipal residential care in Sweden: A registry study. Sage Open Nurs. 2021, 7, 23779608211026161. [Google Scholar] [CrossRef]

| Score | |||
|---|---|---|---|
| Items | 0 | 1 | 2 |
| Follow bed rest instructions | Able | Unable | |
| Follow instructions to raise hands | Able | Unable | |
| Turnover | Able | Partially able | Able |
| Sit up | Able | Unable | |
| Keep a sitting position | Able | Partially able | Able |
| Transfer | Able | Partially able | Able |
| Independent walking (with/without aids) | Able | Unable | |
| Oral care | Able | Unable | |
| Food intake | Able | Partially able | Able |
| Change clothes | Able | Partially able | Able |
| Communication | Able | Partially able | Able |
| Therapeutic instructions | Able | Unable | |
| Deviant behaviours | No | Yes | |
| Total | 19 points | ||
| Variables | ||
|---|---|---|
| Number of patients | 269 | |
| Median age (range) | 85 (43–101) | |
| Female, n (%) | 197 (73.2%) | |
| Fracture type, n (%) | ||
| Trochanteric fracture (AO/OTA 31-A) | 142 (52.7%) | |
| Neck fracture (AO/OTA 31-B) | 127 (47.3%) | |
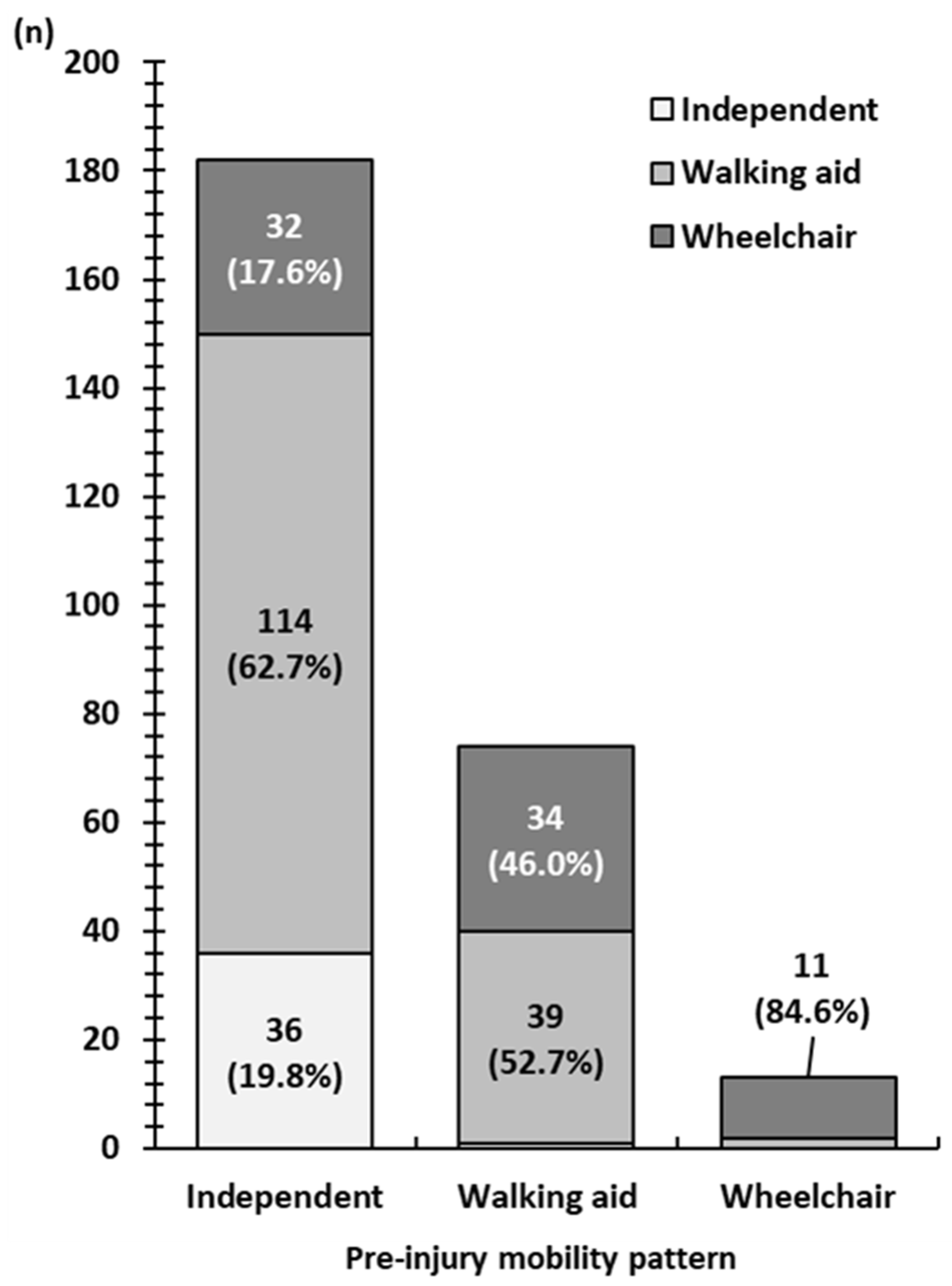
| Pre-injury mobility pattern, n (%) | ||
| Independent | 182 (67.7%) | |
| Walking aid | 74 (27.5%) | |
| Wheelchair | 13 (4.8%) | |
| Surgical method, n (%) | ||
| Osteosynthesis | 94 (34.9) | |
| Bipolar head arthroplasty | 175 (65.1) | |
| Median pre-surgical days (range) | 6 (0–49) | |
| Median hospital days (range) | ||
| Acute care hospital | 20 (4–77) | |
| Rehabilitation hospitals | 52 (5–154) | |
| Total hospitals | 73 (20–186) | |
| Pre-injury dementia, n (%) | 147 (54.6) | |
| Nursing Needs Score, median (range) | ||
| Acute care hospital | 6 (0–18) | |
| Rehabilitation hospitals | 1 (0–19) | |
| Variable | Ambulatory Group (n = 192) | Non-Ambulatory Group (n = 77) | p-Value |
|---|---|---|---|
| Median age (range) | 83 (43–101) | 88 (71–100) | <0.01 |
| Female, n (%) | 145 (53.9%) | 52 (19.3%) | 0.24 |
| Pre-injury mobility (wheelchair), n (%) | 2 (1.0%) | 11 (14.3%) | <0.01 |
| Pre-injury dementia (dementia), n (%) | 57 (29.7%) | 65 (84.4%) | <0.01 |
| Fracture type (neck), n (%) | 96 (0.5%) | 31 (40.3%) | 0.21 |
| Surgical method (BHA), n (%) | 72 (37.5%) | 22 (28.6%) | 0.21 |
| Pre-surgical days (range) | 6 (0–49) | 7 (0–49) | 0.31 |
| Acute care hospital days (range) | 20 (4–67) | 21 (7–77) | 0.46 |
| Rehabilitation hospital days (range) | 51 (9–138) | 56 (5–154) | 0.58 |
| Total hospital days (range) | 72 (21–158) | 79 (20–186) | 0.49 |
| Acute care hospital NNS (range) | 5 (0–16) | 11 (3–18) | <0.01 |
| Rehabilitation hospital NNS (range) | 0 (0–19) | 6 (0–19) | <0.01 |
| Acute care hospital discharge mobility (wheelchair), n (%) | 144 (75.0%) | 73 (94.8%) | <0.01 |
| Acute care hospital discharge dementia, n (%) | 111 (57.8%) | 71 (92.2%) | <0.01 |
| Rehabilitation hospital discharge dementia, n (%) | 101 (52.6%) | 73 (94.8%) | <0.01 |
| Odds Ratio | 95% Confidence Interval | p-Value | |
|---|---|---|---|
| Age | 0.95 | 0.90–1.00 | 0.06 |
| Pre-injury mobility | 2.99 | 1.67–5.34 | <0.01 |
| Pre-surgical days | 1.01 | 0.97–1.05 | 0.54 |
| Acute care hospital Nursing Needs Score | 0.72 | 0.64–0.80 | <0.01 |
| Acute care hospital discharge dementia | 1.84 | 0.62–5.51 | 0.27 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takahashi, A.; Naruse, H.; Hasegawa, D.; Nakajima, H.; Matsumine, A. Functional Recovery Predictors in Hip Fractures: Insights from a Community Clinical Pathway. J. Clin. Med. 2025, 14, 3430. https://doi.org/10.3390/jcm14103430
Takahashi A, Naruse H, Hasegawa D, Nakajima H, Matsumine A. Functional Recovery Predictors in Hip Fractures: Insights from a Community Clinical Pathway. Journal of Clinical Medicine. 2025; 14(10):3430. https://doi.org/10.3390/jcm14103430
Chicago/Turabian StyleTakahashi, Ai, Hiroaki Naruse, Daiki Hasegawa, Hideaki Nakajima, and Akihiko Matsumine. 2025. "Functional Recovery Predictors in Hip Fractures: Insights from a Community Clinical Pathway" Journal of Clinical Medicine 14, no. 10: 3430. https://doi.org/10.3390/jcm14103430
APA StyleTakahashi, A., Naruse, H., Hasegawa, D., Nakajima, H., & Matsumine, A. (2025). Functional Recovery Predictors in Hip Fractures: Insights from a Community Clinical Pathway. Journal of Clinical Medicine, 14(10), 3430. https://doi.org/10.3390/jcm14103430





