Selected Indicators Used in Cephalometric Analysis and Their Predictive Value in Defining Sagittal Discrepancy Malocclusions: A Comparative Study
Abstract
1. Introduction
2. Material and Methods
2.1. Ethical Considerations
2.2. Study Conditions and Inclusion and Exclusion Criteria
Inclusion and Exclusion Criteria from the Study
- (a)
- patients of Caucasian race aged 12–18 years
- (b)
- patients prior to orthodontic treatment
- (c)
- patients with various skeletal categories of class I, II and III
- (d)
- patients characterized by various angles of maxillary base inclination
- (e)
- generally healthy patients
- (f)
- patients without developmental defects
- (g)
- patients without symptoms of untreated dental caries and periodontal disease.
- (a)
- patients aged 0–12 and over 18 years
- (b)
- patients of a race other than Caucasian
- (c)
- patients who had started or completed orthodontic treatment
- (d)
- asymmetry interpreted as a discrepancy between the contours of the right and left side of the mandibular body greater than 8 mm
- (e)
- a projection error or incorrect contrast preventing the identification of reference points
- (f)
- shifts in bilateral anatomical structures relative to each other
- (g)
- patients with congenital defects
- (h)
- patients with disease burdens, including systemic diseases
- (i)
- patients with a high frequency of caries, periodontal disease or cavities after losing teeth, identified in a clinical examination.
2.3. Methods
2.4. Statistical Analysis
- An assessment of the precision of individual cephalometric analyses relative to each other;
- A comparison of the reliability of classifying patients into individual skeletal classes using individual cephalometric analyses.
2.5. Analysis of the Predictive Value and the Fleiss Kappa Index
- <0.00: No agreement
- 0.00–0.20: Poor agreement
- 0.21–0.40: Moderate agreement
- 0.41–0.60: Moderate agreement
- 0.61–0.80: Considerable agreement
- 0.81–1.00: Almost perfect agreement.
3. Results
- Sensitivity = 86/99.4/88.1/87.4/82.4%.
- Positive predictive value = 70.2/50.6/68.8/68.7/70.7%.
- Odds ratio (OR—Likelihood Ratio) = 28.0/169/29.9/28.3/23
- Sensitivity = 70.8/57.5/72.5/87.4/73.7%.
- Positive predictive value = 88.4/94.7/89.0/68.7/89.6%.
- Odds ratio (OR—Likelihood Ratio) = 31.7/53.4/35.4/28.3/40.0.
4. Discussion
4.1. Limitations
4.2. Future Directions of Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 2D | two-dimensional graphics |
| 3D | three-dimensional graphics |
| AI | artificial intelligence |
| OSA | obstructive speech apnea |
| OSD | obstructive sleep disorder |
| OBS | obstructive sleep breathing |
| RODO | General Data Protection Regulation |
| PESEL | the 11-digit identification number assigned to every person residing in Poland and used for unambiguous identification |
| PPV | positive predictive value |
| p | significance level |
| OR | odds ratio |
| CI | confidence level |
References
- Forsyth, D.B.; Shaw, W.C.; Richmond, S.; Roberts, C.T. Digital imaging of cephalometric radiographs, Part 2: Image quality. Angle Orthod. 1996, 66, 43–50. [Google Scholar] [PubMed]
- Brown, M.; Orth, D. Eight Methods of Analysing a Cephalogram to Establish Anteroposterior Skeletal Discrepancy. Br. J. Orthod. 1981, 8, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Oktay, H. A comparison of ANB, WITS, AF-BF, and APDI measurements. J. Orthod. Dentofac. Orthop. 1991, 99, 122–128. [Google Scholar] [CrossRef]
- Jajoo, A.; Agarkar, S.S.; Sharma, S.; Gadhiya, N.; Sonawane, S.; Narkhede, S. Comparison of Beta and ANB Angles for Evaluation of Sagittal Skeletal Discrepancy: A Cephalometric Study. J. Contemp. Dent. Pract. 2018, 19, 739–742. [Google Scholar] [CrossRef]
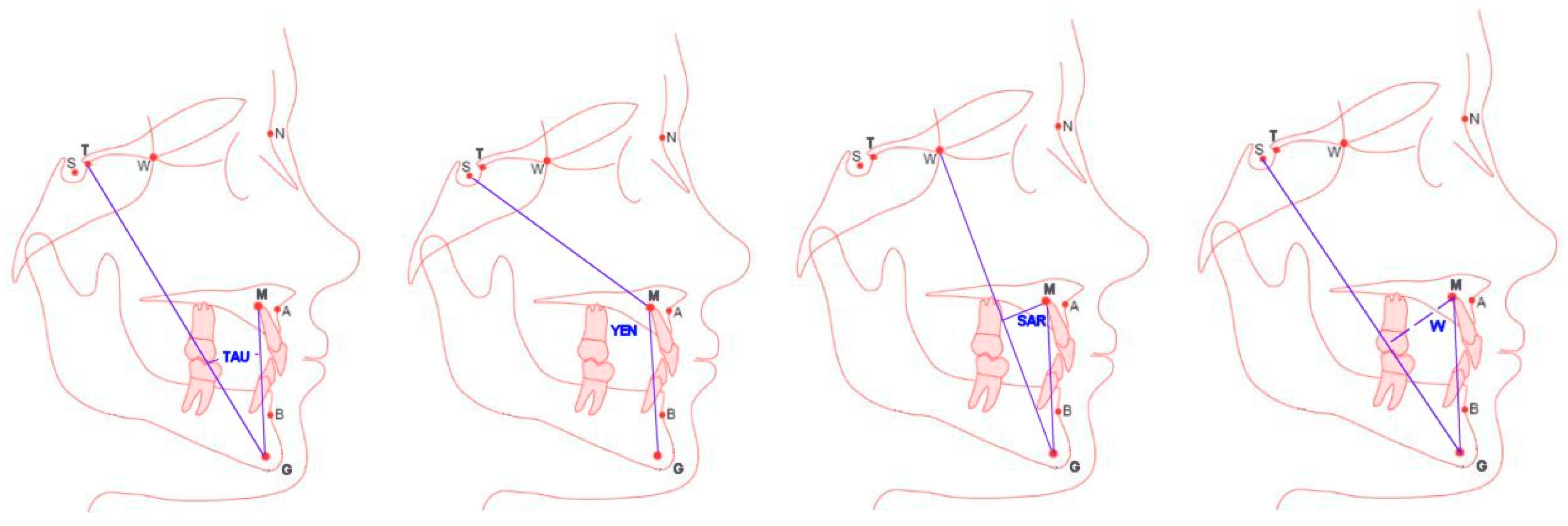
- Kotuła, J.; Kuc, A.E.; Lis, J.; Kawala, B.; Sarul, M. New sagittal and vertical cephalometric analysis methods: A systematic review. Diagnostics 2022, 12, 1723. [Google Scholar] [CrossRef]
- Kotuła, J.; Kuc, A.; Szeląg, E.; Babczyńska, A.; Lis, J.; Matys, J.; Kawala, B.; Sarul, M. Comparison of diagnostic validity of cephalometric analyses of the ANB angle and Tau angle for assessment of the sagittal relationship of jaw and mandible. J. Clin. Med. 2023, 12, 6333. [Google Scholar] [CrossRef]
- Kotuła, J.; Szendoł, K.; Kotuła, K.; Dobrzyński, W.; Lis, J.; Kawala, B.; Sarul, M.; Kuc, A.E. Comparison of the Repeatability and Reproducibility Levels of ANB, Tau and Yen Angle Measurements Used in Cephalometric Diagnostics in the Assessment of Sagittal Discrepancy: A Comparative Study. J. Clin. Med. 2025, 14, 2408. [Google Scholar] [CrossRef]
- Szeląg, E.; Paradowska-Stolarz, A.; Noga, L.; Pietruszka, K.; Szumko, M.; Ogiński, T. Does the Baccetti’s Method of Establishing of Skeletal Age Have Clinical Impotance? Dent. Med. Probl. 2013, 50, 449–453. [Google Scholar]
- Baik, C.Y.; Ververidou, M. A new approach of assessing sagittal discrepancies: The Beta angle. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 100–105. [Google Scholar] [CrossRef]
- Kuijpers-Jagtman, A.M. Reproducibility of cephalometric measurements: Comparison of analog and digital methods. Eur. J. Orthod. 2002, 24, 655–665. [Google Scholar]
- Kumar, V.; Sundareswaran, S. Cephalometric Assessment of Sagittal Dysplasia: A Review of Twenty-One Methods. J. Indian. Orthod. Soc. 2014, 48, 33–41. [Google Scholar] [CrossRef]
- Gupta, P.; Singh, N.; Tripathi, T.; Gopal, R.; Rai, P. Tau angle: A new approach to assessing true sagittal maxillomandibular relationship. Int. J. Clin. Pediatr. Dent. 2020, 13, 497–500. [Google Scholar] [PubMed]
- Jedliński, M.; Janiszewska-Olszowska, J.; Grocholewicz, K. Description of sagittal mandibular relationship in cephalometric analysis—A literature review. Pomer. J. Life Sci. 2020, 66, 25–31. [Google Scholar] [CrossRef]
- Turker, G.; Ozturk, T.; Coban, G.; Isgandarov, E. Evaluation of different sagittal cephalometric measurements in individuals with skeletal class I with different types of vertical facial growth. Ortodon./Orthod. Forum. 2021, 17, 106–113. [Google Scholar] [CrossRef]
- Bruks, A.; Enberg, K.; Nordqvist, I.; Hansson, A.S.; Jansson, L.; Svenson, B. Radiographic studies as an aid in orthodontic diagnosis and treatment planning. Swed. Dent. J. 1999, 23, 77–85. [Google Scholar]
- Neela, P.K.; Mascarenhas, R.; Husain, A. A new index of sagittal dysplasia: The YEN angle. World J. Orthod. 2009, 10, 147–151. [Google Scholar]
- Kumar, S.; Valiathan, A.; Gautam, P.; Chakravarthy, K.; Jayaswal, P. Ocena analizy Pi w ocenie relacji przednio-tylnej szczęki. J. Orthod. 2012, 39, 262–269. [Google Scholar] [CrossRef]
- Bhad, W.A.; Nayak, S.; Doshi, U.H. A new approach to assessing sagittal dysplasia: The W angle. Eur. J. Orthod. 2013, 35, 66–70. [Google Scholar] [CrossRef]
- Sonahita, A.; Jitendra, B.; Praveen, M.; Sudhir, K.; Kumar, J.R. SAR angle: A contemporary marker of sagittal mandibular dysplasia. Orthod. J. Nepal. 2014, 4, 16–20. [Google Scholar]
- Hatewar, S.K.; Reddy, G.H.; Singh, J.R.; Jain, M.; Munje, S.; Khandelwal, P. A new dimension of cephalometry: The D. W. plane. J. Indian. Orthod. Soc. 2015, 49, 206–212. [Google Scholar] [CrossRef]
- Rizwan, M.; Mascarenhas, R. A new parameter for assessing vertical skeletal discrepancies: The R angle. Rev. Latinoam. Ortodon. Odontop. 2013, 16, 200102C5997. [Google Scholar]
- Kattan, E.E.; Kattan, M.H.; Elhiny, O.A. A new horizontal plane of head. Open Access Maced. J. Med. Sci. 2018, 6, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Park, J.A.; Lee, J.S.; Koh, K.S.; Song, W.C. The use of the zygomatic arch as a reference line in clinical applications and anthropological research. Surg. Radiol. Anat. 2019, 41, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Smołka, P.; Nelke, K.; Struzik, N.; Wiśniewska, K.; Kiryk, S.; Kensy, J.; Dobrzyński, W.; Kiryk, J.; Matys, J.; Dobrzyński, M. Discrepancies in the results of cephalometric analysis between orthodontists and radiologists and artificial intelligence: A systematic review. Appl. Sci. 2024, 14, 4972. [Google Scholar] [CrossRef]
- Starch-Jensen, T.; Hernández-Alfaro, F.; Kesmez, Ö.; Gorgis, R.; Valls-Ontañón, A. Accuracy of orthognathic surgery planning using three-dimensional virtual techniques compared with conventional two-dimensional techniques: A systematic review. J. Oral. Maxillofac. Res. 2023, 14, 14101. [Google Scholar]
- AlBarakati, S.F.; Kula, K.S.; Ghoneima, A.A. Reliability and repeatability of cephalometric measurements: A comparison of conventional and digital methods. Dentomaxillofac. Radiol. 2012, 41, 11–17. [Google Scholar] [CrossRef]
- Devereux, L.; Moles, D.; Cunningham, S.J.; McKnight, M. How important are lateral cephalometric radiographs in orthodontic treatment planning? Am. J. Orthod. Dentofac. Orthop. 2011, 139, 175–181. [Google Scholar] [CrossRef]
- Nijkamp, P.; Habets, L.; Aartman, I.; Zentner, A. The influence of cephalometry on orthodontic treatment planning. Eur. J. Ortoda. 2008, 30, 630–635. [Google Scholar] [CrossRef]
- Durão, A.R.; Pittayapat, P.; Rockenbach, M.I.B. Validity of 2D lateral cephalometry in orthodontics: A systematic review. Prog. Ortoda. 2013, 14, 31. [Google Scholar] [CrossRef]
- Ahmed, M.; Shaikh, A.; Fida, M. Diagnostic performance of various cephalometric parameters for the assessment of vertical growth pattern. Dent. Press. J. Orthod. 2016, 21, 41–49. [Google Scholar] [CrossRef]
- Jarosz-Nowak, J. Models for assessing the degree of agreement between two experts using kappa coefficients. Appl. Math. 2007, 8, 126–154. [Google Scholar]
- Kuc, A.E.; Kotuła, J.; Nawrocki, J.; Szeląg, E.; Kawala, B.; Lis, J.; Sarul, M. Morphological evaluation of the incisal canal in the aspect of diagnosis and planning of orthodontic treatment—CBCT study. Appl. Sci. 2023, 13, 12010. [Google Scholar] [CrossRef]
- Chen, Z.; Mo, S.; Fan, X.; You, Y.; Guanrong, Y.; Zhou, N. A meta-analysis and systematic review comparing the effectiveness of traditional and virtual surgical planning for orthognathic surgery: Based on randomized clinical trials. J. Oral. Maxillofac. Surg. 2021, 79, 471.e1–471.e19. [Google Scholar] [CrossRef]
- Lin, L.O.; Kalmar, C.L.; Vu, G.H.; Zimmerman, C.E.; Humphries, L.S.; Swanson, J.W.; Bartlett, S.P.; Taylor, J.A. Value-based analysis of virtual versus traditional surgical planning for orthognathic surgery. J. Craniofacial Surg. 2020, 31, 1238–1242. [Google Scholar] [CrossRef]
- Bogusiak, K.; Kociński, M.; Łutkowski, A.; Materka, A.; Arkuszewski, P. Changes in measurements of Segner-Hasund analysis in patients with mandibular prognathism after orthognathic surgery. Dent. Med. Probl. 2016, 53, 13–21. [Google Scholar] [CrossRef]
- Bansal, N.; Singla, J.; Gera, G.; Gupta, M.; Kaur, G. Reliability of natural head position in orthodontic diagnosis: A cephalometric study. Contemp. Clin. Dent. 2012, 3, 180–183. [Google Scholar] [CrossRef]
- Wang, C.W.; Huang, C.T.; Hsieh, M.C.; Li, C.H.; Chang, S.W.; Li, W.C.; Vandaele, R.; Marée, R.; Jodogne, S.; Geurts, P.; et al. Evaluation and comparison of anatomical landmark detection methods for cephalometric X-ray Images: A grand challenge. IEEE Trans. Med. Imaging 2015, 34, 1890–1900. [Google Scholar] [CrossRef]
- Barrera-Chaparro, J.P.; Plaza-Ruíz, S.P.; Parra, K.L.; Quintero, M.; Velasco, M.D.P.; Molinares, M.C.; Álvarez, C. The need for orthodontic treatment, types of braces, and quality of life related to oral health. Dent. Med. Probl. 2023, 60, 287–294. [Google Scholar] [CrossRef]
- Lagravère, M.O.; Low, C.; Flores-Mir, C.; Chung, R.; Carey, J.P.; Heo, G.; Major, P.W. Intraexaminer and interexaminer reliabilities of landmark identification on digitized lateral cephalograms and formatted 3-dimensional cone-beam computerized tomography images. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 598–604. [Google Scholar] [CrossRef]
- Frongia, G.; Piancino, M.G.; Bracco, A.A.; Crincoli, V.; Debernardi, C.L.; Bracco, P. Assessment of the reliability and repeatability of landmarks using 3-D cephalometric software. Cranio® 2012, 30, 255–263. [Google Scholar] [CrossRef]
- De Oliveira Lisboa, C.; Masterson, D.; Motta, A.F.J.; Motta, A.T. Reliability and reproducibility of three-dimensional cephalometric landmarks using CBCT: A systematic review. J. Appl. Oral. Sci. 2015, 23, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Chien, P.C.; Parks, E.T.; Eraso, F.; Hartsfield, J.K.; Roberts, W.E.; Ofner, S. Comparison of reliability in anatomical landmark identification using two-dimensional digital cephalometrics and three-dimensional Cone Beam Computed Tomography in vivo. Dentomaxillofacial Radiol. 2009, 38, 262–273. [Google Scholar] [CrossRef] [PubMed]
- Sam, A.; Currie, K.; Oh, H.; Flores-Mir, C.; Lagravére-Vich, M. Reliability of different three-dimensional cephalometric landmarks in cone-beam computed tomography: A systematic review. Angle Orthod. 2019, 89, 317–332. [Google Scholar] [CrossRef]
- Kuc, A.E.; Kotuła, J.; Nawrocki, J.; Kulgawczyk, M.; Kawala, B.; Lis, J.; Sarul, M. Maxillary bone remodeling after incisor retraction during orthodontic treatment with premolar extraction based on CBCT imaging: A systematic review. J. Clin. Med. 2024, 13, 1503. [Google Scholar] [CrossRef]
- Kuc, A.E.; Kotuła, J.; Nahajowski, M.; Warnecki, M.; Lis, J.; Amm, E.; Kawala, B.; Sarul, M. Methods of anterior torque control during retraction: A systematic review. Diagnostics 2022, 12, 1611. [Google Scholar] [CrossRef]
- Minch, L.; Marzec, A.M.; Nowak, R.; Pieńkowska, K. Orthodontic-surgical treatment of a female patient with skeletal class III malocclusion due to maxillary deficiency—Case report. Forum Ortodon./Orthod. Forum 2021, 17, 301–311. [Google Scholar] [CrossRef]
- Szarmach, I.; Kaczyńska, J.; Łukasiewicz, D.; Szarmach, J. Long-term observation of class III malocclusion. Forum Ortodon. 2008, 4, 129–140. [Google Scholar]
- Lin, J.H.; Wang, S.; Abdullah, U.A.; Le, A.D.; Chung, C.H.; Chenshuang, L. Sagittal and vertical changes of the maxilla after surgically assisted rapid palatal expansion: A systematic review and meta-analysis. J. Clin. Med. 2023, 12, 3488. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Gallo, S.; Pascadopoli, M.; Gandini, P.; Roncoroni, C.; Scribante, A. Upper airway dimensions among different skeletal malocclusions: A retrospective observational study using cephalometric analysis. Dent. J. 2024, 12, 12. [Google Scholar] [CrossRef]
- Sarul, M.; Nahajowski, M.; Gawin, G.; Antoszewska-Smith, J. Does the duration of daily wearing of Twin Block reliably predict its efficacy in class II treatment? J. Orofac. Orthop. 2022, 83, 195–204. [Google Scholar] [CrossRef]
- Kartbak, S.B.A.; Özel, M.B.; Kocakaya, D.N.C.; Çakmak, M.; Sinanoğlu, E.A. Classification of intraoral photographs using deep learning algorithms trained according to cephalometric measurements. Diagnostics 2025, 15, 1059. [Google Scholar] [CrossRef]
- Ribas-Sabartés, J.; Sánchez-Molins, M.; d’Oliveira, N.G. Accuracy of algorithms applied by artificial intelligence in the detection of cephalometric points: A systematic review. Bioengineering 2024, 11, 1286. [Google Scholar] [CrossRef] [PubMed]
- Khabadze, Z.; Mordanov, O.; Shilyaeva, E. Comparative analysis of 3D cephalometry using artificial intelligence and manual tracking. Diagnostics 2024, 14, 2524. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.K.; Alftaikhah, S.A.A.; Issrani, R.; Ronsivalle, V.; Lo Giudice, A.; Cicciù, M.; Minervini, G. Applications of Artificial Intelligence in the Utilisation of Imaging Modalities in Dentistry: A Systematic Review and Meta-Analysis of in-Vitro Studies. Heliyon 2024, 10, e24221. [Google Scholar] [CrossRef]
- Miryala, A.G.; Miryala, G.; Khan, Y.; Ramalingam, N.T.; Sevugaperumal, B.; Soman, M.; Padmanabhan, A. Revolutionizing Dental Imaging: A Comprehensive Study on the Integration of Artificial Intelligence in Dental and Maxillofacial Radiology. Cureus 2023, 15, e50292. [Google Scholar]
- Tabatabaian, F.; Vora, S.R.; Mirabbasi, S. Applications, Functions, and Accuracy of Artificial Intelligence in Restorative Dentistry: A Literature Review. J. Esthet. Restor. Dent. 2023, 35, 842–859. [Google Scholar] [CrossRef]
- Kiełczykowski, M.; Kamiński, K.; Perkowski, K.; Zadurska, M.; Czochrowska, E. Application of Artificial Intelligence (AI) in a Cephalometric Analysis: A Narrative Review. Diagnostics 2023, 13, 2640. [Google Scholar] [CrossRef]
- Alessandri-Bonetti, A.; Sangalli, L.; Salerno, M.; Gallenzi, P. Reliability of Artificial Intelligence-Assisted Cephalometric Analysis. A Pilot Study. BioMedInformatics 2023, 3, 44–53. [Google Scholar] [CrossRef]
- Segner, D.; Hasund, A. Indywidualna Kefalometria; MedTourPress: Otwock, Poland, 1996; ISBN 8390359049. [Google Scholar]
- WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Participants—WMA—The World Medical Association. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki/?utm_source=newsletter&utm_medium=email&utm_campaign=revised_declaration_of_helsinki_adopted_by_the_global_medical_community_strengthening_ethical_standards_in_clinical_research_involving_humans&utm_term=2024-10-23 (accessed on 30 November 2024).
- Altman, D.G.; Bland, J.M. Diagnostic tests 2: Predictive values. BMJ 1994, 309, 102. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Fleiss, J.L. Measuring normal scale agreement among many raters. Psychol. Bull. 1971, 76, 378–382. [Google Scholar] [CrossRef]
- Nahajowski, M.; Lis, J.; Kawala, B.; Sarul, M. Effectiveness of different protocols of Class II treatment: A retrospective study. Forum Ortodon./Orthod. Forum 2022, 18, 127–143. [Google Scholar] [CrossRef]
| Skeletal Class II Tau Angle | Skeletal Class II ANB: >4° (Distoclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 3933 | No N = 7947 | ||||
| Tau > 33.3° | 3384 (86.0) | 1434 (18.0) | <0.001 | 28.0 [25.2–31.2] | Sens. = 0.860 |
| Tau ≤ 33.3° | 549 (14.0) | 6513 (82.0) | 1.00 (ref.) | PPV = 0.702 | |
| Skeletal Class II Yen Angle | Skeletal Class II ANB: >4° (Distoclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 3933 | No N = 7947 | ||||
| Yen < 129.0° | 3908 (99.4) | 3816 (48.0) | <0.001 | 169 [114–251] | Sens. = 0.994 |
| Yen ≥ 129.0° | 25 (0.6) | 4131 (52.0) | 1.00 (ref.) | PPV = 0.506 | |
| Skeletal Class II W Angle | Skeletal Class II ANB: >4° (Distoclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 3933 | No N = 7947 | ||||
| W < 54.1° | 3439 (87.4) | 1570 (19.8) | <0.001 | 28.3 [25.3–31.5] | Sens. = 0.874 |
| W ≥ 54.1° | 494 (12.6) | 6377 (80.2) | 1.00 (ref.) | PPV = 0.687 | |
| Skeletal Class II Sar Angle | Skeletal Class II ANB: >4° (Distoclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 3933 | No N = 7947 | ||||
| Sar < 56.6° | 3464 (88.1) | 1574 (19.8) | <0.001 | 29.9 [26.8–33.4] | Sens. = 0.881 |
| Sar ≥ 56.6° | 469 (12.6) | 6373 (80.2) | 1.00 (ref.) | PPV = 0.688 | |
| Skeletal Class II Wits | Skeletal Class II ANB: >4° (Distoclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 3933 | No N = 7947 | ||||
| Wits > 1.0 mm | 3240 (82.4) | 1341 (16.9) | <0.001 | 23.0 [20.8–25.5] | Sens. = 0.824 |
| Wits ≤ 1.0 mm | 693 (16.6) | 6606 (83.1) | 1.00 (ref.) | PPV = 0.707 | |
| Skeletal Class III Tau Angle | Skeletal Class III ANB: <2° (Mesiocclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 5166 | No N = 6714 | ||||
| Tau < 29.9° | 3660 (70.8) | 478 (7.1) | <0.001 | 31.7 [28.4–35.4] | Sens. = 0.708 |
| Tau ≥ 29.9° | 1506 (29.2) | 6236 (92.9) | 1.00 (ref.) | PPV = 0.884 | |
| Skeletal Class III Yen Angle | Skeletal Class III ANB: <2° (Mesiocclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 5166 | No N = 6714 | ||||
| Yen > 127.2° | 2972 (57.5) | 166 (2.5) | <0.001 | 53.4 [45.4–62.9] | Sens. = 0.575 |
| Yen ≤ 127.2° | 2194 (42.5) | 6548 (97.5) | 1.00 (ref.) | PPV = 0.947 | |
| Skeletal Class III W Angle | Skeletal Class III ANB: <2° (Mesiocclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 5166 | No N = 6714 | ||||
| W > 57.5° | 3575 (69.2) | 384 (5.7) | <0.001 | 37.0 [32.9–41.7] | Sens. = 0.692 |
| W ≤ 57.5° | 1591 (30.8) | 6330 (94.3) | 1.00 (ref.) | PPV = 0.903 | |
| Skeletal Class III Sar Angle | Skeletal Class III ANB: <2° (Mesiocclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 5166 | No N = 6714 | ||||
| Sar > 59.6° | 3743 (72.5) | 464 (6.9) | <0.001 | 35.4 [31.7–39.6] | Sens. = 0.725 |
| Sar ≤ 59.6° | 1423 (27.5) | 6250 (93.1) | 1.00 (ref.) | PPV = 0.890 | |
| Skeletal Class III Wits | Skeletal Class III ANB: <2° (Mesiocclusion) | p-Value | OR [95% CI] | Test Quality Indicators | |
|---|---|---|---|---|---|
| Yes N = 5166 | No N = 6714 | ||||
| Wits < −0.8 mm | 3809 (73.7) | 440 (6.5) | <0.001 | 40.0 [35.7–44.9] | Sens. = 0.737 |
| Wits ≥ −0.8 mm | 1357 (26.3) | 6274 (93.5) | 1.00 (ref.) | PPV = 0.896 | |
| Tau (°) | Yen (°) | W (°) | Sar (°) | Wits (mm) | |
|---|---|---|---|---|---|
| ANB (°) | 0.540 | 0.345 | 0.542 | 0.553 | 0.546 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotuła, J.; Kotuła, K.; Kotarska, M.; Lis, J.; Kawala, B.; Sarul, M.; Kuc, A.E. Selected Indicators Used in Cephalometric Analysis and Their Predictive Value in Defining Sagittal Discrepancy Malocclusions: A Comparative Study. J. Clin. Med. 2025, 14, 3429. https://doi.org/10.3390/jcm14103429
Kotuła J, Kotuła K, Kotarska M, Lis J, Kawala B, Sarul M, Kuc AE. Selected Indicators Used in Cephalometric Analysis and Their Predictive Value in Defining Sagittal Discrepancy Malocclusions: A Comparative Study. Journal of Clinical Medicine. 2025; 14(10):3429. https://doi.org/10.3390/jcm14103429
Chicago/Turabian StyleKotuła, Jacek, Krzysztof Kotuła, Małgorzata Kotarska, Joanna Lis, Beata Kawala, Michał Sarul, and Anna Ewa Kuc. 2025. "Selected Indicators Used in Cephalometric Analysis and Their Predictive Value in Defining Sagittal Discrepancy Malocclusions: A Comparative Study" Journal of Clinical Medicine 14, no. 10: 3429. https://doi.org/10.3390/jcm14103429
APA StyleKotuła, J., Kotuła, K., Kotarska, M., Lis, J., Kawala, B., Sarul, M., & Kuc, A. E. (2025). Selected Indicators Used in Cephalometric Analysis and Their Predictive Value in Defining Sagittal Discrepancy Malocclusions: A Comparative Study. Journal of Clinical Medicine, 14(10), 3429. https://doi.org/10.3390/jcm14103429






