1. Introduction
There is a pressing need for strategies that optimize the management of heart failure (HF), a common condition that is the leading cause of premature death worldwide [
1]. The disease burden is very high, and its prevalence is progressively increasing for reasons that include, among others, the aging of the population and the greater coexistence of risk factors [
2]. In Spain, the estimated prevalence of HF is 2% according to recently published studies, but this rate is increasing every year [
3]. This disease is also a major contributor to cardiovascular-related hospitalizations and deaths [
4]. It is the principal cause of hospital admissions in people older than 65 years [
5] and 50% of patients die in the first five years after diagnosis [
4]. In terms of economic impact, HF accounts for 2% of Spanish health expenditure [
6], but this figure could rise as prevalence increases.
The CARABELA-HF initiative addresses the improvement areas in the management of HF in the healthcare system in Spain. CARABELA initiatives are led by scientific societies and AstraZeneca to analyze and tackle the current situation and needs in chronic conditions with the aim of driving a holistic transformation toward systemic and practical improvement. CARABELA-HF is therefore a transversal initiative that seeks to reduce existing management inequalities and inefficiencies, improve the quality of care, and optimize the routine management of HF, taking into account the various realities and care models present in Spain [
7]. A recent publication introduced CARABELA-HF as a joint collaboration between scientific societies and AstraZeneca and described the care of patients with HF in Spain as a circular multidisciplinary process where primary care, internal medicine and cardiology go hand-in-hand, in a patient-centered approach [
8].
We report here the results obtained during the CARABELA-HF initiative, which aimed to analyze current HF management models in Spain in order to develop healthcare quality indicators for detecting improvement areas and defining lines of action.
2. Methods
CARABELA-HF Design and Participants
This initiative has been developed and coordinated throughout Spain by the main scientific societies involved in the management of HF in Spain: Spanish Society of Cardiology (SEC), Spanish Society of Internal Medicine (SEMI), Spanish Society of Quality of Care (SECA), and Spanish Society of Health Managers (SEDISA). A total of 10 pilot centers participated in the characterization phase. The overall structure and methodological foundation of the CARABELA initiative has been detailed previously [
7]. In the case of CARABELA-HF, the project was organized into four phases:
Phase 1: Characterization and evaluation of HF healthcare models in Spanish hospitals.
The characterization phase was grounded in the concept of HF care as a cyclical and multidisciplinary process [
8]. The current models of HF clinical management were analyzed in the 10 pilot centers and presented in sessions in which healthcare professionals from each center participated. Data collection at each center was conducted via structured working sessions involving multidisciplinary clinical teams. Information was gathered regarding coordination practices, resource availability, and professional roles in HF management. In these meetings, a total of 9 variables were selected by the Scientific Committee based on clinical relevance and feasibility of collection. These helped to categorize the different models of patient care and define the type and degree of coordination between the medical specialties involved in HF care, the roles of implicated professionals, and the availability of certain resources: coordination between cardiology and internal medicine; availability of skilled nursing staff; availability of nurse consultations; responsibility for drug titration; availability of case managers; use of HF protocols and circuits; role of other specialties; existence of multidisciplinary committees; and presence of a day hospital. The identification and classification of the four HF care models was based on the comparative analysis of these variables across centers. Data on these nine variables were collected through structured working sessions held with multidisciplinary teams from each pilot center, including cardiologists, internists, and nursing staff.
A set of healthcare quality indicators was created to assess each identified model and to establish a reference framework for future monitoring, through iterative consensus among the CARABELA-HF scientific committee, using structured expert meetings, as well as national and regional workshops. These indicators were subsequently piloted in the participating pilot centers and were divided by type into three main clusters: structure, quality of care, and transformation.
Phase 2 (validation), Phase 3 (cocreation), and Phase 4 (dissemination and implementation).
During Phase 2, the identified models and the interpretation of the data collected during Phase 1, were reviewed and used to identify improvement areas and potential solutions that were subsequently validated by members of the Spanish HF health ecosystem during the National CARABELA-HF Conference through a structured consensus process.
Finally, all the results obtained were synthesized and the regional refinement of solutions to address improvement areas in the HF care process was drawn up during the co-creation Phase 3. In Phase 4, the analyses and potential solutions were disseminated to as many Spanish healthcare centers as possible. These results were included in a digital questionnaire in the form of a playbook.
All collected information was descriptive and qualitative, aimed at capturing the organizational features of each center rather than obtaining quantitative measurements or collecting patient-level clinical outcome data such as mortality or readmission rates. No formal measurement scales or standardized instruments were used, nor were formal statistical analyses applied.
3. Results
3.1. Coordination Models for the Management of HF in Spanish Hospitals
During the pilot phase, a total of four care models of the HF patient were identified which mainly differed on the degree of coordination and communication between the departments involved in patient management. The availability of resources for HF management among the models were notably different. An overview of the four models is shown in
Figure 1 and in the
Supplementary Materials.
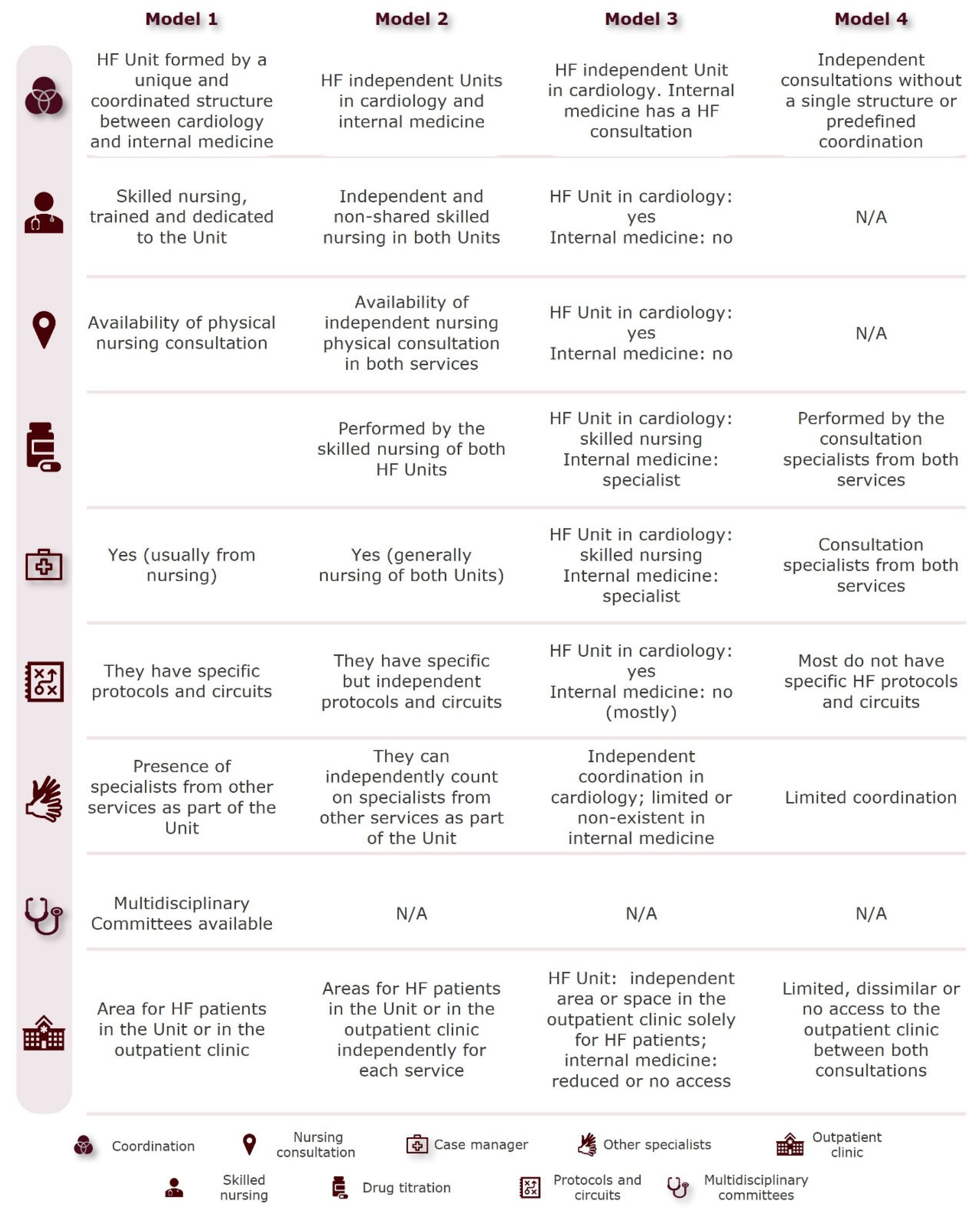
Model 1 consists of a single HF unit integrating cardiology and internal medicine, with equal resource access, a skilled and trained nursing team, a dedicated consultation room, a designated person responsible for drug titrations, and a case manager overseeing patient transitions in and out of the hospital. The unit applies specific protocols and circuits and has multidisciplinary committees and specialists from other departments. Model 2 consists of two independent HF units within cardiology and internal medicine, with unequal access to resources, a lower level of coordination than Model 1 and no predetermined multidisciplinary committees discussing patient management. Model 3 consists of an HF unit in the cardiology department, while internal medicine relies on external HF consultations, and has less access to resources. Only the HF unit within cardiology has a specific protocol and circuit for HF care and an independent area within the day hospital. Model 4 lacks structured HF units relying on independent consultations for HF patient management without interdepartmental coordination or access to resources, and specialists from each department are responsible for tasks such as drug titration and case management. This model lacks skilled nursing staff, specific protocols and circuits are rare, and coordination with other specialties is limited. Access to the day hospital is scant and varies between departments. Model characteristics are compared in
Figure 2.
3.2. Indicators to Evaluate Care Models
HF units must be assessed from different perspectives. Care models must therefore be analyzed on the basis of three indicator types (structure, quality of care, and transformation) that have been previously described in detail [
7]. Conclusions can be drawn about the model by gathering and evaluating predetermined indicators of each type.
The structure indicator category focuses on the organization of HF management in the center and covers four areas: hospital environment; resources in the HF unit; origin and characteristics of patients with HF; and care process. Within this category, the analysis defined indicators such as the number of HF patients in the unit, the number of different healthcare professionals, indicators related to the proportion of time invested on consultation, diagnostic tests, and patient education, the percentage of referrals from primary care or other specialties and waiting lists. All structure indicators are listed in
Table 1.
Healthcare quality indicators were categorized based on the phases of the care process: suspicion (i.e., >70% of patients with HF suspicion are referred with a digitized electrocardiogram), diagnosis (i.e., virtual consultation between primary care and specialists), treatment (i.e., treatment adherence programs), and follow-up (i.e., skilled HF nursing staff) (
Table 2).
Likewise, the scientific committee defined three types of transformation indicators to evaluate the care model evolution: transformation of the structure; transformation of the process; and health outcomes (
Table 3).
This subdivision included the presence of a cardiac intensive care unit, a person in the hospital who is responsible for the centralization of patient transitions, the percentage of confirmed diagnosed patients referred from primary care, and the average length of stay in the cardiology or internal medicine ward of patients admitted with a HF diagnosis, among others.
3.3. The Future of HF: Improvement Areas for the Evolution of Care Models, Barriers, and Potential Solutions
The in-depth analysis of the identified care models led to the recognition of 13 areas of improvement associated with the distinct phases of the HF care process (suspicion, diagnosis, treatment, and follow-up) that were validated during the National CARABELA-HF Conference. These improvement areas would be addressed in the future for the design of an integrated care model. The initial management of patients with HF suspicion was identified as an improvement area at the clinical suspicion level, along with the development of an integrated model for HF management at diagnosis level, the standardization of patient management irrespective of the responsible department at treatment level and the implementation of a coordinated management model between different care levels with standardized follow-up of HF patients at follow-up level.
Finally, after characterizing the different care models in place throughout Spain, identifying the areas of improvement with the greatest potential impact both nationally and regionally, and gathering the perspectives of healthcare professionals through meetings conducted as part of the CARABELA-HF initiative, we identified key solutions that should be pursued to develop a comprehensive and integrated HF care model: (1) coordination and protocols, (2) a virtual care model and digital transformation, (3) roles and functions of the nursing team, (4) professional training and patient education on HF, (5) access to resources, (6) accredited care models, and (7) registries and data evaluation.
4. Discussion
The need for collaborative HF management is well known. In fact, the SEC and the SEMI have been promoting the establishment of specialized units in Spanish hospitals for years [
9], and the European Society of Cardiology (ESC) recommends that patients with HF should be treated in multidisciplinary units to reduce hospitalizations and mortality [
10]. This is partly because in the management of HF, the role of the internist is crucial, as many patients present with multiple comorbidities that are treated by internal medicine. Furthermore, HF units should be run systematically, as proposed in a scientific consensus published by the SEC in 2016. This document defined both quality standards and methods for the accreditation of HF units [
11]. Further down the line, we must now assess the implementation of these quality-of-care programs and produce an overview of how HF is managed in Spanish centers nowadays. For this reason, the CARABELA-HF initiative has focused on defining the shared model between cardiology and internal medicine and on identifying the use of resources and the management characteristics. Only in this way can limitations be detected, and solutions designed.
This detailed characterization process implemented in 10 centers nationwide has identified that while the range of available resources determines the type and quality of care provided to patients, the main differentiating factor in the type of care received is the coordination and communication between cardiology and internal medicine. Inadequate coordination or delayed referral, more characteristic of Models 3 and 4, can hinder timely optimization of pharmacological therapy, which has been linked to increased morbidity and higher readmission rates [
2,
10]. Equitable access to the center’s resources is clearly key in generating a model of coordination and optimal communication between units in the care of patients with HF, while the collaboration and integration of other specialties into the unit offers a 360° vision. The effectiveness of implementing multidisciplinary HF management programs with an equal allocation of assets between units has been proven in other countries [
12]. Another conclusion was that periodically convening multidisciplinary clinical case committees is useful for improving the care of patients with HF. Considering the impact of HF on the Spanish population [
5,
13], the early optimization and use of disease-modifying drugs is deficient. Prompt horizontal introduction of these therapies, rather than a staggered approach, would avoid a delay in the administration of highly effective therapies. All centers recognize the need to generate rapid care circuits for HF patients, including medical record flagging to streamline their journey throughout the care process. In terms of resources, the centers generally do not have a professional with predefined roles and functions who is responsible for the management of internal/external patient transitions throughout the care process. Furthermore, the availability of specialized, fully dedicated nurses with their own consulting room appears to be key to improving patient care both during treatment and at follow-up. This type of organizational structure, characterized by strong coordination between specialties, equitable access to resources, and the involvement of HF-specialized nurses, has been associated with better clinical outcomes. For instance, accredited HF units in Spain, which share many features with Model 1, have demonstrated improved adherence to guideline-directed medical therapy and more systematic follow-up strategies, contributing to higher quality of care [
9].
Although CARABELA-HF was conducted within the specific organizational framework of the Spanish healthcare system, several principles identified may be broadly applicable across different countries, despite differences in healthcare structures and financing models. These include the critical role of structured multidisciplinary collaboration, the early initiation and optimization of disease-modifying therapies, the importance of consistent follow-up strategies, and the equitable allocation of healthcare resources. Moreover, disease management programs and multidisciplinary care approaches have shown to reduce hospital readmissions and improve survival and patient quality of life [
2,
14]. Prioritizing models with stronger integration and resource access, and adapting these principles to local contexts, may contribute to improved HF care delivery and outcomes worldwide. This approach aligns with the ESC guidelines, which recommend early optimization of pharmacological treatment, patient education, and care integration as essential strategies to improve long-term outcomes in HF [
10].
The main limitation of this initiative is its lack of quantitative methodology, but notwithstanding, the use of the healthcare quality indicators described in this document as an instrument for evaluating care models was fundamental for analyzing the efficacy of our processes in terms of organization, structure, resources, and patient empowerment. The previous literature has reported that a system of indicators to measure intervention outcomes and to ensure continuous improvement in the quality of care is essential for the success of disease management programs [
14]. To that end, indicators must be synthesized and endorsed at a national level, as isolated databases are insufficient. The CARABELA-HF initiative has established a system of indicators that covers all aspects of the care process and can be used systematically at a national level.
CARABELA-HF offers the added value of a public and private multidisciplinary collaboration involving numerous national experts and several scientific societies focused on the quality management of HF. We have included not only entities with a clinical perspective, but also institutions from the healthcare management field, as the latter are indispensable for the organization of healthcare provision. Strengthening collaboration with primary care is assuredly the great improvement area for the near future [
9], and ongoing initiative within the CARABELA “fleet” are focused on this approach.