Association Between Depression, Anxiety, Quality of Life and Burnout Syndrome with Symptoms of Insomnia in Healthcare Professionals in Montenegro During the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Sample Description
2.2. Data Collection
2.2.1. General Questionnaire
2.2.2. The Athens Insomnia Scale
2.2.3. Health-Related Quality of Life EQ-5D-5L
2.2.4. DASS Scale—The Depression, Anxiety, and Stress Scale
2.2.5. Maslach Burnout Inventory—Human Services Survey
2.3. Statistical Analyses
2.4. Use of Generative AI
3. Results
3.1. Insomnia and Health-Related Quality of Life
3.2. Insomnia and Mental Health Assessment
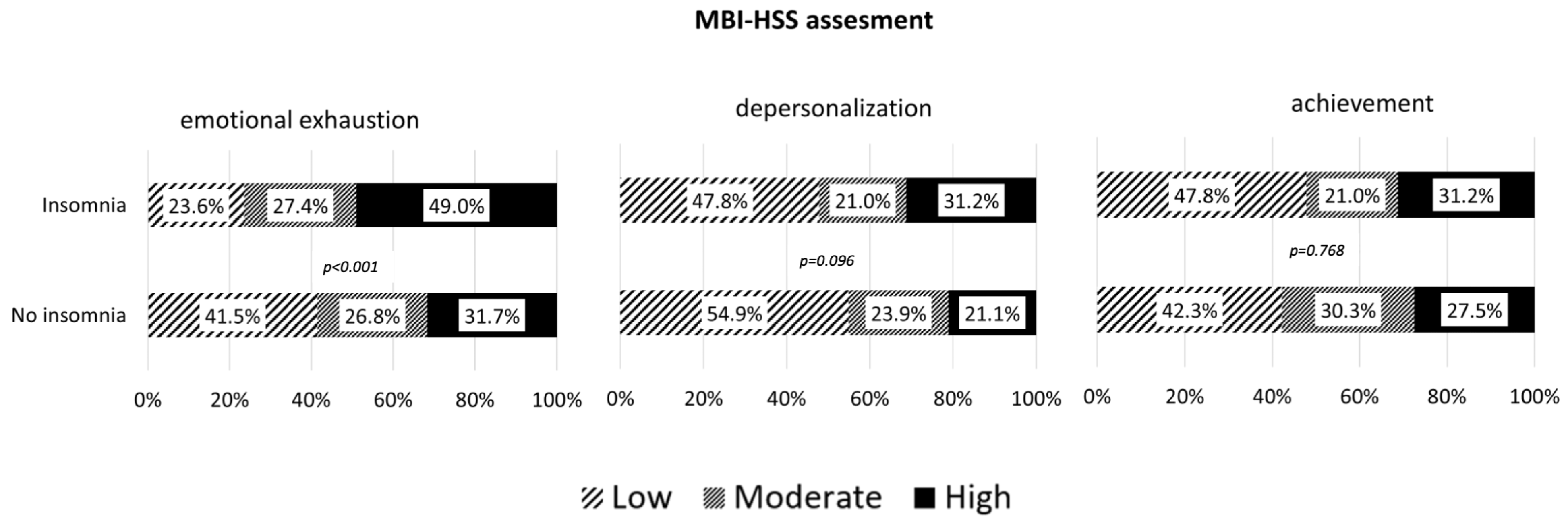
3.3. Insomnia and Burnout Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Verma, A.K.; Prakash, S. Impact of COVID-19 on environment and society. J. Glob. Biosci. 2020, 9, 7352–7363. [Google Scholar]
- Weiss, M.A.; Schwarzenberg, A.B.; Nelson, R.M.; Sutter, K.M.; Sutherland, M.D. Global Economic Effects of COVID-19; Congressional Research Service: Washington, DC, USA, 2020. [Google Scholar]
- Pedrosa, A.L.; Bitencourt, L.; Fróes, A.C.; Cazumbá, M.L.; Campos, R.G.; De Brito, S.B.; Simões e Silva, A.C. Emotional, behavioral, and psychological impact of the COVID-19 pandemic. Front. Psychol. 2020, 11, 566212. [Google Scholar] [CrossRef] [PubMed]
- Dermitzakis, I.; Evangelidis, N.; Evangelidis, P.; Anestis, A. Knowledge, attitudes, and perceptions regarding COVID-19 outbreak in Greece in September 2020: A cross-sectional web-based survey. Hippokratia 2021, 25, 15–21. [Google Scholar] [PubMed]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Khaledi-Paveh, B.; Kazeminia, M.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Eskandari, S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: A systematic review and meta-regression. Hum. Resour. Health 2020, 18, 100. [Google Scholar] [CrossRef]
- Kızılok, G.E.; Tanhan, F. Stress sources and behavioral addiction inclinations of teachers in the COVID-19 outbreak. Res. Educ. Psychol. 2021, 5, 163–185. [Google Scholar] [CrossRef]
- Almeida, G.D.; Souza, H.R.; Almeida, P.C.; Almeida, B.D.; Almeida, G.H. The prevalence of burnout syndrome in medical students. Arch. Clin. Psychiatry 2016, 43, 6–10. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef]
- Spiegelhalder, K.; Scholtes, C.; Riemann, D. The association between insomnia and cardiovascular diseases. Nat. Sci. Sleep 2010, 2, 71–78. [Google Scholar] [CrossRef]
- Palagini, L.; Hertenstein, E.; Riemann, D.; Nissen, C. Sleep, insomnia and mental health. J. Sleep Res. 2022, 31, e13628. [Google Scholar] [CrossRef]
- Ohayon, M.M. Epidemiological overview of sleep disorders in the general population. Sleep Med. Res. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Hartstein, L.E.; Mathew, G.M.; Reichenberger, D.A.; Rodriguez, I.; Allen, N.; Chang, A.M.; Chaput, J.P.; Christakis, D.A.; Garrison, M.; Gooley, J.J.; et al. The impact of screen use on sleep health across the lifespan: A national sleep foundation consensus statement. Sleep Health 2024, 10, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Martínez-Jarreta, B.; Rapisarda, V.; Ledda, C. Occupational risks of healthcare personnel. Front. Public Health 2022, 10, 1022327. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Lemoine, P.; Arnaud-Briant, V.; Dreyfus, M. Prevalence and consequences of sleep disorders in a shift worker population. J. Psychosom. Res. 2002, 53, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Vandekerckhove, M.; Cluydts, R. The emotional brain and sleep: An intimate relationship. Sleep Med. Rev. 2010, 14, 219–226. [Google Scholar] [CrossRef]
- Sharifi, M.; Asadi-Pooya, A.A.; Mousavi-Roknabadi, R.S. Burnout among healthcare providers of COVID-19; A systematic review of epidemiology and recommendations. Arch. Acad. Emerg. Med. 2020, 9, e7. [Google Scholar]
- Doleman, G.; De Leo, A.; Bloxsome, D. The impact of pandemics on healthcare providers’ workloads: A scoping review. J. Adv. Nurs. 2023, 79, 4434–4454. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Ielapi, N.; Andreucci, M.; Bracale, U.M.; Costa, D.; Bevacqua, E.; Bitonti, A.; Mellace, S.; Buffone, G.; Candido, S.; Provenzano, M.; et al. Insomnia Prevalence among Italian Night-Shift Nurses. Nurs. Rep. 2021, 11, 530–535. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Balai, M.K.; Avasthi, R.D.; Raghu, V.A.; Jonwal, A. Psychological impacts among healthcare personnel during COVID-19 pandemic: A systematic review. J. Caring Sci. 2022, 11, 118–125. [Google Scholar] [CrossRef]
- Chen, S.; Cheng, C. Unveiling Coronasomnia: Pandemic Stress and Sleep Problems During the COVID-19 Outbreak. Nat. Sci. Sleep 2024, 12, 543–553. [Google Scholar] [CrossRef]
- Olson, E.J.; Drage, L.A.; Auger, R.R. Sleep deprivation, physician performance, and patient safety. Chest 2009, 136, 1389–1396. [Google Scholar] [CrossRef] [PubMed]
- Backović, D.; Jovanović, D.; Bukmirić, Z.; Kusturica, M.; Asotić, M. Burnout syndrome among employees in a clinical center in Montenegro during COVID-19. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 10126–10132. [Google Scholar] [PubMed]
- Jovanović, D.; Backović, D.; Tomas, A.; Bukumirić, Z.; Koprivica, B. Predisposition and Working Conditions for the Occurrence of Lumbar Syndrome in Medical Workers of the Clinical Center of Montenegro during the COVID-19 Pandemic. J. Clin. Med. 2024, 13, 2431. [Google Scholar] [CrossRef] [PubMed]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. The diagnostic validity of the Athens Insomnia Scale. J. Psychosom. Res. 2003, 55, 263–267. [Google Scholar] [CrossRef]
- Parkitny, L.; McAuley, J. The Depression Anxiety Stress Scale (DASS). J. Physiother. 2010, 56, 204. [Google Scholar] [CrossRef]
- Kinman, G. Maslach Burnout Inventory. Occup. Med. 2024, 74, 630–631. [Google Scholar]
- Sahebi, A.; Abdi, K.; Moayedi, S.; Torres, M.; Golitaleb, M. The prevalence of insomnia among health care workers amid the COVID-19 pandemic: An umbrella review of meta-analyses. J. Psychosom. Res. 2021, 149, 110597. [Google Scholar] [CrossRef]
- Garcia, A.N.; Salloum, I.M. Polysomnographic Sleep Disturbances in Nicotine, Caffeine, Alcohol, Cocaine, Opioid, and Cannabis Use: A Focused Review. Am. J. Addict. 2015, 24, 590–598. [Google Scholar] [CrossRef]
- Silva, F.C.T.; Neto, M.L.R. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: A systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2020, 104, 110057. [Google Scholar] [CrossRef]
- Sasaki, N.; Kuroda, R.; Tsuno, K.; Kawakami, N. The deterioration of mental health among healthcare workers during the COVID-19 outbreak: A population-based cohort study of workers in Japan. Scand. J. Work Environ. Health 2020, 46, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Metlaine, A.; Sauvet, F.; Gomez-Merino, D.; Boucher, T.; Elbaz, M.; Delafosse, J.Y.; Leger, D.; Chennaoui, M. Sleep and biological parameters in professional burnout: A psychophysiological characterization. PLoS ONE 2018, 13, e0190607. [Google Scholar] [CrossRef] [PubMed]
- Medisauskaite, A.; Kamau, C. Does occupational distress raise the risk of alcohol use, binge-eating, ill health, and sleep problems among medical doctors? A UK cross-sectional study. BMJ Open 2019, 9, e027362. [Google Scholar] [CrossRef]
- Amini-Rarani, M.; Azami-Aghdash, S.; Mousavi Isfahani, H.; Mohseni, M. Estimation of the prevalence of anxiety during the COVID-19 pandemic: A meta-analysis of meta-analyses. BMC Public Health 2024, 24, 2831. [Google Scholar] [CrossRef]
- Bianchi, R.; Schonfeld, I.S. Beliefs about burnout. Work Stress 2024, 38, 1–19. [Google Scholar] [CrossRef]
- Lavoie-Tremblay, M.; Gélinas, C.; Aubé, T.; Nguemeleu, É.T.; Tremblay, D.; Gagnon, M.; Côté, J. Influence of Caring for COVID-19 Patients on Nurse’s Turnover, Work Satisfaction and Quality of Care. J. Nurs. Manag. 2021, 30, 33. [Google Scholar] [CrossRef]
- Evans, E.J.; Noureddine, N.; Curry, S.R.; Nam, K. COVID-19 Impacts on Social Work and Nursing Now and into the Future: National Administration Plans. Health Soc. Work 2021, 46, 152. [Google Scholar] [CrossRef]
- Mensinger, J.L.; Brom, H.; Havens, D.S.; Costello, A.; D’Annunzio, C.; Durning, J.D.; Bradley, P.K.; Copel, L.C.; Maldonado, L.; Smeltzer, S.C.; et al. Psychological Responses of Hospital-Based Nurses Working during the COVID-19 Pandemic in the United States: A Cross-Sectional Study. Appl. Nurs. Res. 2021, 63, 151517. [Google Scholar] [CrossRef]
- Marcomini, I.; Agus, C.; Milani, L.; Sfogliarini, R.; Bona, A.; Castagna, M. COVID-19 and Post-Traumatic Stress Disorder among Nurses: A Descriptive Cross-Sectional Study in a COVID Hospital. Med. Lav. 2021, 112, 241. [Google Scholar] [CrossRef]
- Sørengaard, T.A.; Olsen, A.; Langvik, E.; Saksvik-Lehouillier, I. Associations between Sleep and Work-Related Cognitive and Emotional Functioning in Police Employees. Saf. Health Work 2021, 12, 359. [Google Scholar] [CrossRef]
- Kyle, S.D.; Morgan, K.; Espie, C.A. Insomnia and Health-Related Quality of Life: A Clinical Review. Sleep Med. Rev. 2010, 14, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Daley, M.; Morin, C.M.; LeBlanc, M.; Grégoire, J.P.; Savard, J.; Baillargeon, L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009, 10, 427–438. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://apps.who.int/gb/ebwha/pdf_files/wha69/a69_39-en.pdf (accessed on 28 April 2025).
- Grover, S.; Fitzpatrick, A.; Azim, F.T.; Ariza-Vega, P.; Bellwood, P.; Burns, J.; Burton, E.; Fleig, L.; Clemson, L.; Hoppmann, C.A.; et al. Defining and implementing patient-centered care: An umbrella review. Patient Educ. Couns. 2022, 105, 1679–1688. [Google Scholar] [CrossRef] [PubMed]
- Karazivan, P.; Dumez, V.; Flora, L.; Pomey, M.P.; Del Grande, C.; Ghadiri, D.P.; Fernandez, N.; Jouet, E.; Las Vergnas, O.; Lebel, P. The patient-as-partner approach in health care: A conceptual framework for a necessary transition. Acad. Med. 2015, 90, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Lefurgey, S.; Detillieux, S.; Shaheen, A.; Daigle, P.; Nolan, D.; Rudnick, A. Person-Centered Care: Learning from the Evolution of Mental Health Care. Encyclopedia 2025, 5, 29. [Google Scholar] [CrossRef]
- Jørgensen, K.; Lerbæk, B.; Frederiksen, J.; Watson, E.; Karlsson, B. Patient Participation in Mental Health Care–Perspectives of Healthcare Professionals and Patients: A Scoping Review. Issues Ment. Health Nurs. 2024, 45, 794–810. [Google Scholar] [CrossRef]
- Edvardsson, D.; Fetherstonhaugh, D.; Nay, R.; Gibson, S. Development and initial testing of the Person-centered Care Assessment Tool (P-CAT). Int. Psychogeriatr. 2010, 22, 101–108. [Google Scholar] [CrossRef]
- Edvardsson, D.; Innes, A. Measuring person-centered care: A critical comparative review of published tools. Gerontologist 2010, 50, 834–846. [Google Scholar] [CrossRef]
- Bru-Luna, L.M.; Martí-Vilar, M.; Merino-Soto, C.; Livia-Segovia, J.; Garduño-Espinosa, J.; Toledano-Toledano, F. Person-centered care assessment tool with a focus on quality healthcare: A systematic review of psychometric properties. BMC Psychol. 2024, 12, 217. [Google Scholar] [CrossRef]
- Esparza-Reig, J.; Martí-Vilar, M.; González-Sala, F.; Merino-Soto, C.; Toledano-Toledano, F. Social Support and Resilience as Predictors of Prosocial Behaviors before and during COVID-19. Healthcare 2022, 10, 1669. [Google Scholar] [CrossRef]
- Latif, A.; Yaqub, S.; Dar, A.Q.; Awan, S.U.; Khokhar, A.M. Stress, resilience and moral distress among health care providers during COVID-19 pandemic. J. Health Res. 2023, 8, 1–4. [Google Scholar] [CrossRef]
- Goudarzian, A.H.; Nikbakht Nasrabadi, A.; Sharif-Nia, H.; Farhadi, B.; Navab, E. Exploring the concept and management strategies of caring stress among clinical nurses: A scoping review. Front. Psychiatry 2024, 15, 1337938. [Google Scholar] [CrossRef] [PubMed]
- Urtubia-Herrera, V.; Navarta-Sánchez, M.V.; Palmar-Santos, A.M.; Pedraz-Marcos, A.; García-Gomez, A.; Luis, E.O.; Bermejo-Martins, E. The relationship between sense of coherence and emotional intelligence as individual health assets for mental health promotion in students and healthcare professionals: A scoping review. Front. Public Health 2024, 12, 1304310. [Google Scholar] [CrossRef] [PubMed]
- Saparniene, D.; Strukcinskiene, B.; Mineviciute, G.; Cizauskaite, A.; Rapoliene, L.; Grigoliene, R.; Pacauskiene, I.; Malcikaite, D.; Kairys, J.; Savickas, S. Post-traumatic stress symptoms among healthcare professionals involved in COVID-19 response: Findings from a cross-sectional study. Int. J. Environ. Res. Public Health 2023, 20, 1765. [Google Scholar]
- Koka, S.; Lê, J.L.; Salgado, J.; Martinez, G.; Popper, J. Emotional and psychological impact of COVID-19 on healthcare workers in Europe: A systematic review. Eur. J. Public Health 2021, 31, 16–21. [Google Scholar]
| Characteristics | No Insomnia n (%) | Insomnia n (%) | p-Value |
|---|---|---|---|
| Sex | |||
| Male | 51 (35.9) | 55 (35.0) | 0.873 |
| Female | 91 (64.1) | 102 (65.0) | |
| Age | 36.79 ± 11.278 | 38.57 ± 11.567 | 0.180 |
| Marital status | 0.914 | ||
| Single | 62 (43.7) | 70 (44.6) | |
| Married | 68 (47.9) | 72 (45.9) | |
| Divorced | 12 (8.5) | 15 (6.6) | |
| Number of children | 0.487 | ||
| 0 | 73 (51.8) | 72 (45.9) | |
| 1 | 15 (10.6) | 20 (12.7) | |
| 2 | 27 (19.1) | 39 (24.8) | |
| 3 | 21 (14.9) | 19 (12.1) | |
| 4 | 5 (3.5) | 7 (4.5) | |
| Alcohol consumption | 0.007 | ||
| No | 122 (85.9) | 115 (73.2) | |
| Yes | 20 (14.1) | 42 (26.8) | |
| Cigarette consumption | 0.006 | ||
| No | 83 (58.5) | 67 (42.7) | |
| Yes | 59 (41.5) | 90 (57.3) | |
| Consuming a sedative | 0.038 | ||
| No | 141 (99.3) | 149 (94.9) | |
| Yes | 1 (0.7) | 8 (5.1) | |
| Occupation | 0.698 | ||
| A doctor | 39 (27.5) | 44 (28.0) | |
| Nurse | 79 (55.6) | 81 (51.6) | |
| Other medical staff | 24 (16.9) | 32 (20.4) | |
| Working hours | 0.107 | ||
| Only in one shift | 28 (19.7) | 21 (13.4) | |
| In two shifts | 29 (20.4) | 21 (13.4) | |
| In shifts 12 h | 54 (38.0) | 75 (47.8) | |
| Morning + 24 h | 31 (21.8) | 40 (25.5) | |
| Overtime | 0.321 | ||
| No | 47 (33.3) | 44 (28.0) | |
| Yes | 94 (66.7) | 113 (72.0) |
| Characteristics | No Insomnia n (%) | Insomnia n (%) | p-Value |
|---|---|---|---|
| COVID-19 work | 0.386 | ||
| Not at all or continuously | 111 (78.2) | 129 (82.2) | |
| Intermintently | 31 (21.8) | 28 (17.8) | |
| COVID-19 engagement | 0.097 | ||
| No | 29 (20.4) | 27 (17.2) | |
| I was engaged for 1 to 3 months | 26 (18.3) | 18 (11.5) | |
| I was engaged for more than 3 months | 87 (61.3) | 112 (71.3) | |
| COVID-19 impacted my employment | 0.607 | ||
| I don’t agree at all | 55 (39.0) | 58 (37.4) | |
| I don’t agree | 42 (29.8) | 41 (26.5) | |
| I agree | 26 (18.4) | 37 (23.9) | |
| I completely agree | 18 (12.8) | 19 (12.3) | |
| I had increase workload and excessive engagement | 0.017 | ||
| I don’t agree at all | 22 (15.6) | 9 (5.7) | |
| I don’t agree | 38 (27.0) | 30 (19.1) | |
| I agree | 52 (36.9) | 87 (55.4) | |
| I completely agree | 29 (20.6) | 31 (19.7) | |
| I had adequate protective equipment | 0.066 | ||
| I don’t agree at all | 6 (4.2) | 42(1.3) | |
| I don’t agree | 30 (21.1) | 41 (26.1) | |
| I agree | 74 (52.1) | 100 (63.7) | |
| I completely agree | 32 (22.5) | 14 (8.9) | |
| I had enough knowledge on COVID-19 | 0.426 | ||
| I don’t agree at all | 8 (5.6) | 8 (5.1) | |
| I don’t agree | 36 (25.4) | 39 (24.8) | |
| I agree | 48 (33.8) | 68 (43.3) | |
| I completely agree | 50 (35.2) | 42 (26.8) | |
| COVID-19 negatively impacted my finances | 0.194 | ||
| I don’t agree at all | 31 (21.68) | 28 (17.9) | |
| I don’t agree | 48 (33.8) | 42 (26.9) | |
| I agree | 39 (27.5) | 61 (39.1) | |
| I completely agree | 24 (16.9) | 25 (16.0) | |
| Quarantine during COVID-19 | 0.008 | ||
| No | 66 (46.5) | 49 (31.4) | |
| Yes | 76 (53.5) | 107 (68.6) | |
| COVID-19 infection | 0.001 | ||
| No | 90 (63.4) | 69(43.9) | |
| Yes | 52 (36.6) | 88 (56.1) |
| Dimension | No Insomnia n (%) | Insomnia n (%) | p-Value |
|---|---|---|---|
| EQ-5D-5L Mobility | <0.001 | ||
| I have no problems in walking about | 111 (88.8) | 68 (54.4) | |
| I have slight problems in walking about | 10 (8.0) | 32 (25.6) | |
| I have moderate problems in walking about | 2 (1.6) | 10 (8.0) | |
| I have severe problems in walking about | 0 (0.0) | 13 (10.4) | |
| I am unable to walk about | 2 (1.6) | 2 (1.6) | |
| EQ-5D-5L Self-care | <0.001 | ||
| I have no problems washing or dressing myself θ | 119 (95.2) | 98 (78.4) | |
| I have slight problems washing or dressing myself θ | 3 (2.4) | 11 (8.8) | |
| I have moderate problems washing or dressing myself | 1 (0.8) | 16 (12.8) | |
| I have severe problems washing or dressing myself | 2 (1.6) | 0 (0.0) | |
| EQ-5D-5L Usual activities | <0.001 | ||
| I have no problems doing my usual activities | 116 (92.8) | 77 (61.6) | |
| I have slight problems doing my usual activities | 4 (3.2) | 30 (24.0) | |
| I have moderate problems doing my usual activities | 5 (4.0) | 16 (12.8) | |
| I have severe problems doing my usual activities | 0 (0.0) | 2 (1.6) | |
| EQ-5D-5L Pain discomfort | <0.001 | ||
| I have no pain or discomfort | 98 (78.4) | 49 (39.2) | |
| I have slight pain or discomfort | 20 (16.0) | 40 (32.0) | |
| I have moderate pain or discomfort | 6 (4.8) | 27 (21.6) | |
| I have severe pain or discomfort | 1 (0.8) | 9 (7.2) | |
| EQ-5D-5L Anxiety and depression | <0.001 | ||
| I am not anxious or depressed | 116 (92.8) | 62 (49.6) | |
| I am slightly anxious or depressed | 7 (5.6) | 43 (34.4) | |
| I am moderately anxious or depressed | 2 (1.6) | 15 (12.0) | |
| I am severely anxious or depressed | 0 (0.0) | 5 (4.0) | |
| EQ-5D-5L Health condition | 89.26 ± 11.949 | 73.82 ± 18.799 | <0.001 |
| EQ-5D-5L Index | 0.97 ± 0.85 | 0.89 ± 0.13 | <0.001 |
| Characteristics | No Insomnia n (%) | Insomnia n (%) | p-Value |
|---|---|---|---|
| ASS21 stress level | <0.001 | ||
| Normal | 115 (81.0) | 97 (61.8) | |
| Mild | 13 (9.2) | 21 (13.4) | |
| Moderate | 10 (7.0) | 26 (16.6) | |
| Severe | 3 (2.1) | 11 (7.0) | |
| Extremely severe | 1 (0.7) | 2 (1.3) | |
| ASS21 anxiety level | <0.001 | ||
| Normal | 103(72.5) | 78 (49.7) | |
| Mild | 6 (4.2) | 10 (6.4) | |
| Moderate | 21 (14.8) | 27 (17.2) | |
| Severe | 4 (2.8) | 20 (12.7) | |
| Extremely severe | 8 (5.6) | 22 (14.0) | |
| ASS21 degree of depression | <0.001 | ||
| Normal | 117 (82.4) | 97 (61.8) | |
| Mild | 14 (9.9) | 20 (12.7) | |
| Moderate | 10 (7.0) | 29 (18.5) | |
| Severe | 1(0.7) | 9 (5.7) | |
| Extremely severe | 0 (0.0) | 2 (1.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Backović, D.; Jovanović, D.; Tomas, A.; Bukumirić, Z.; Tomović, K. Association Between Depression, Anxiety, Quality of Life and Burnout Syndrome with Symptoms of Insomnia in Healthcare Professionals in Montenegro During the COVID-19 Pandemic. J. Clin. Med. 2025, 14, 3374. https://doi.org/10.3390/jcm14103374
Backović D, Jovanović D, Tomas A, Bukumirić Z, Tomović K. Association Between Depression, Anxiety, Quality of Life and Burnout Syndrome with Symptoms of Insomnia in Healthcare Professionals in Montenegro During the COVID-19 Pandemic. Journal of Clinical Medicine. 2025; 14(10):3374. https://doi.org/10.3390/jcm14103374
Chicago/Turabian StyleBacković, Dragana, Dragana Jovanović, Ana Tomas, Zoran Bukumirić, and Kristina Tomović. 2025. "Association Between Depression, Anxiety, Quality of Life and Burnout Syndrome with Symptoms of Insomnia in Healthcare Professionals in Montenegro During the COVID-19 Pandemic" Journal of Clinical Medicine 14, no. 10: 3374. https://doi.org/10.3390/jcm14103374
APA StyleBacković, D., Jovanović, D., Tomas, A., Bukumirić, Z., & Tomović, K. (2025). Association Between Depression, Anxiety, Quality of Life and Burnout Syndrome with Symptoms of Insomnia in Healthcare Professionals in Montenegro During the COVID-19 Pandemic. Journal of Clinical Medicine, 14(10), 3374. https://doi.org/10.3390/jcm14103374





