1. Introduction
Meniscal injuries are common conditions accounting for 12% to 14% of all knee injuries, with an incidence of 60–70 cases per 100,000 people [
1].
The menisci are primarily composed of type I collagen fibers within a highly hydrated extracellular matrix [
2] and exhibit a zonal vascularization pattern (red-red, red-white, white-white zones), which critically influences their regenerative capacity and the outcomes of meniscal repair [
3].
The menisci play a crucial role in knee joint homeostasis, preserving tibiofemoral congruency, joint stability, dynamic load distribution, and proprioception [
4]. Notably, meniscal repair, by preserving meniscal tissue, restores biomechanical load distribution in the affected compartment, reducing the risk of early chondral wear and degeneration [
5].
Treatment options for meniscal tears are both non-operative and surgical. The surgical options include meniscectomy and suture repair [
1]. For several years, arthroscopic partial meniscectomy has been the most common orthopedic procedure in the world [
6]. Recent studies suggest that patients treated with meniscectomy may have a substantially higher risk—estimated to be up to 300 times greater—of osteoarthritis progression and subsequent need for total knee arthroplasty compared to those managed with meniscal repair [
7]. This growing body of evidence has contributed to a paradigm shift favoring meniscal preservation, often summarized by the principle ‘save the meniscus’ [
8].
The most common meniscal tear types include horizontal cleavage tears (HCTs), radial tears (RTs), vertical tears, which encompass ramp lesions (MRLs), certain meniscal root tears (MRTs), and longitudinal tears (LTs), and complex meniscal tears (CMTs), which involve a combination of two or more types [
1]. LTs may progress to bucket-handle meniscal tears (BHMTs).
HCTs split the meniscus into a superior and an inferior half, involving the articular surfaces and/or its periphery [
9]. Their incidence is anywhere from 20 to 23% [
10,
11] to 40% [
12] of all meniscal tears. RTs are meniscal tears arising from the central region (white-white) to the periphery (red-red) and can occur in all anteroposterior zones of the medial and lateral meniscus [
13]. They induce increased joint contact pressure, involving a higher risk of chondral damage and meniscal extrusion than other tears. RTs have been reported to account for 10% to 23% of all tears in the adult population [
14], 28% of medial meniscal tears [
13], and 14% of isolated lateral meniscal tears [
15]. LTs are vertical lesions running perpendicular to the tibial plateau and parallel to the long meniscal axis, among the circumferential collagen fibers [
16]. They account for 18.2–37.6% [
8] of all tears. BHMTs are large longitudinal vertical tears with an attached fragment that can be flipped into the intercondylar notch [
17] and have a significant impact on knee biomechanics [
18]. They account for nearly 10% [
19] to 26% [
20,
21] of all meniscal tears. MRLs are vertical peripheral tears involving the posterior horn of the medial meniscus. They may lead to meniscocapsular or meniscotibial disruption [
22]. Their true incidence is unknown due to high rates of mis- or underdiagnosis caused by low imaging sensitivity, poor intraoperative visualization, and surgeon experience [
23]. MRLs are found in 9% [
24] to 42% [
22] of ACL reconstruction procedures, although isolated MRLs may exist in the absence of obvious ACL rupture [
25]. An MRT is a meniscal lesion occurring within 1 cm of the meniscal root attachment, or a complete bony or soft tissue avulsion of the root attachment [
26]. They account for up to 20% of all meniscal tears [
27], although they have been labeled a “silent epidemic” due to their frequent underdiagnoses and the rapid progression of the untreated injuries into osteoarthritis [
28]. Finally, CMTs involve multiplanar disruption of meniscal tissue [
29] by a combination of two or more tear types [
30]. Their incidence is around 15% of all meniscal injuries [
31].
The indications and techniques for surgical repair depend on multiple patient- and lesion-related characteristics [
32]. The type of meniscal tear is critical in guiding treatment decisions [
33]. Second-generation all-inside, inside-out, outside-in [
32], and transtibial pull-out sutures are the most widely used techniques, optimizing the benefits of the surgical treatment and minimizing its drawbacks. Yet, despite advances in repair techniques and devices, failure rates still range from 10% [
1] to 36% [
8].
Currently, the literature includes numerous studies that analyze individual meniscal lesions in detail, focusing on incidence, classification, diagnosis, treatment, outcomes, and failure rates. Similarly, several works provide a general overview encompassing the most common meniscal injuries; however, these often lack specific and clinically relevant details for each lesion. To date, a descriptive study addressing the most frequent meniscal tears, highlighting intraoperative findings and short-term treatment evolution, is still missing.
We describe meniscal repair as it occurred in our high-volume meniscal suture center and analyze the most common meniscal lesions with emphasis on their features and treatment. The primary aim of the study is to assess the frequency, site (medial/lateral), radial location (anterior horn, body/posterior horn, root), and surgical management of each type. The secondary aim is to analyze total and lesion-specific failure rates with a focus on the suture techniques related to higher failure rates. In light of the current literature and of lesion characteristics, we hypothesize that failure rates differ across lesions and that certain repair patterns may be at a higher risk of failure than others.
2. Materials and Methods
2.1. Study Design and Patient Selection
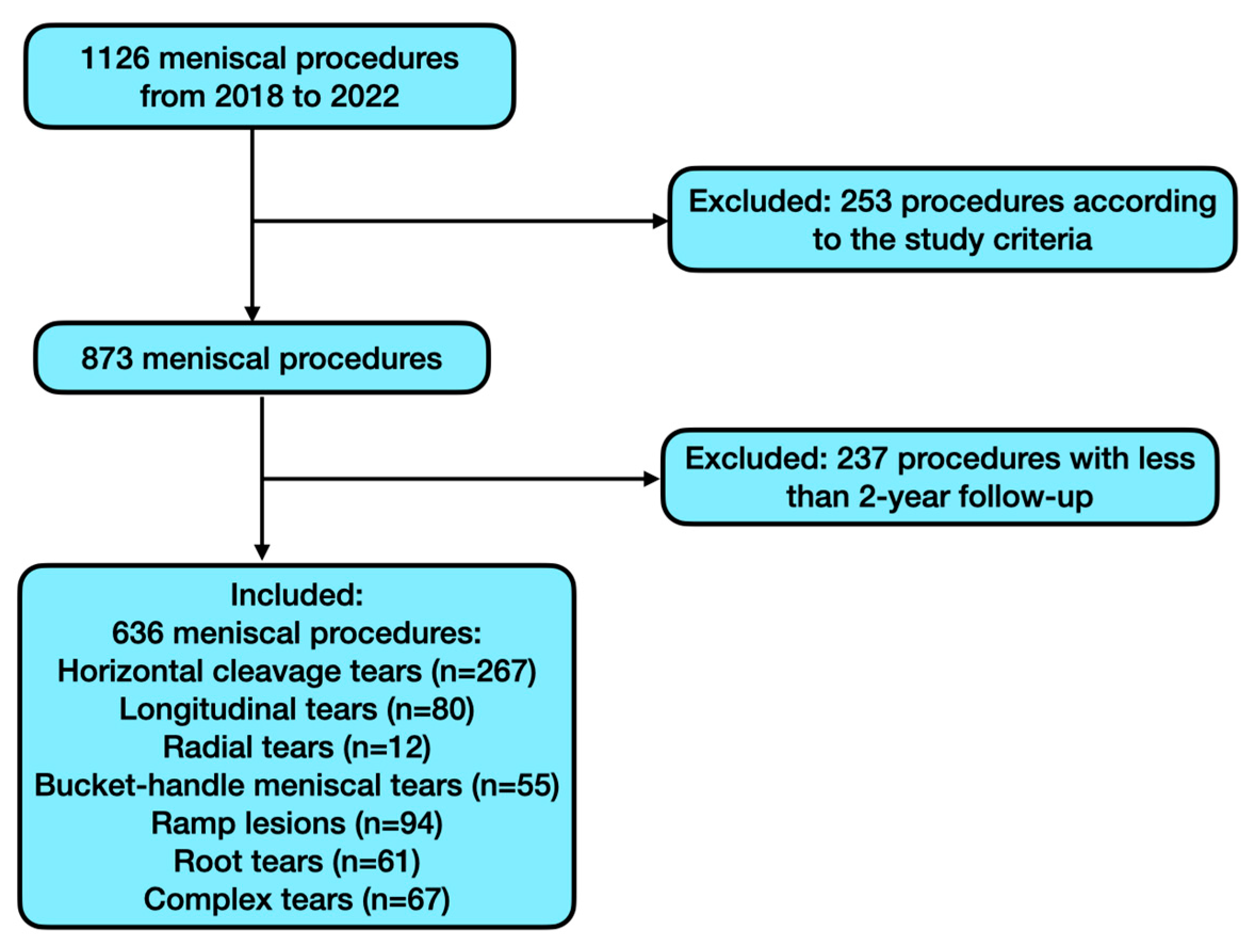
The present retrospective observational study is on a consecutive cohort of patients undergoing meniscal repair.
Following review board approval, the institutional electronic database was mined for the meniscal arthroscopic repair procedures performed by the same senior surgeon from January 2018 to September 2022 at the Orthopedic Department of IRCCS Sacro Cuore-Don Calabria Hospital (Negrar di Valpolicella, Italy), reference center for orthopedic surgery, with a high annual volume of procedures in the field of sports medicine.
2.2. Inclusion and Exclusion Criteria
Procedures involving the seven most common types of meniscal lesions—HCTs, RTs, LTs, BHMTs, MRLs, MRTs, and CMTs—that were treated with all-inside, outside-in, inside-out, and transtibial pull-out suture techniques were included. In particular, only patients who had a follow-up of at least 2 years were selected. The study excluded lesions treated solely with regularization; lesions requiring treatments other than those listed above (e.g., meniscal transplantation or anchor-based sutures) or additional biological treatments; cases with less than 2-year follow-up; patients with prior knee infections or discoid meniscus; other less frequent meniscal lesion types; and any procedures whose description in the surgical records was unclear. Finally, patients with confounders such as comorbidities that potentially impair meniscal healing following repair procedures (rheumatic diseases, tumors, or coagulative disorders) or chondral damage >2 according to the International Cartilage Repair Society classification were excluded from the study.
2.3. Minimizing Bias
Several strategies were employed to minimize bias in this retrospective study, particularly considering the non-randomized nature of treatment allocation due to the distinct types of meniscal lesions. Despite the lack of randomization, treatments were systematically selected based on the type and location of the lesion, which could help reduce selection bias that may influence the results. Data were collected using a standardized protocol for all cases, and all patients were evaluated using the same criteria to determine meniscal repair failure. The patient cohort included a wide range of characteristics, both in terms of meniscal type and surgical treatment. Additionally, diagnostic criteria for each type of lesion and the definition of failure were clearly defined in advance to minimize discrepancies between clinicians. To further reduce information bias, a double data review was conducted: an independent evaluation by two authors (F.Q. and L.D.B.), with any ambiguous cases resolved by a third, experienced author (D.S.). Finally, all surgeries were performed by a single surgeon, which helped minimize inter-surgeon bias that could affect the outcomes.
2.4. Data Collection
We abstracted the following demographic and preoperative data from the dataset: gender, age at surgery, and affected knee (left/right). We recorded the following intraoperative data: tear type, based on the intraoperative arthroscopic findings, instead of the preoperative diagnosis; tear laterality (medial/lateral); tear site (anterior horn, body/posterior horn, root); repair technique (all-inside, inside-out, outside-in, pull-out); number and combination of sutures used; and presence of a meniscal lesion in the contralateral meniscus.
We also recorded treatment failures, defined as the need for further surgery in case of tear persistence [
34], to calculate the overall failure rate of the cohort and of each type of tear and repair technique.
2.5. Tear Types: Classification and Diagnosis
2.5.1. Horizontal Cleavage Tears
HCTs are graded on a 1 to 3 scale based on magnetic resonance imaging (MRI) scans according to Stoller et al. [
35]. In this classification, grade 1 involves irregularly marginated intrameniscal signal; grade 2 involves primarily linear signal that does not communicate with an articular margin; and grade 3 involves signal intensity that communicates with an articular margin. On MRI, HCTs usually appear as an area where signal alteration extends horizontally along the meniscus parallel to the tibial plateau.
2.5.2. Radial Lesions
The latest RTs classification, proposed by Chahla et al. [
5] and adopted in this study, divides them into partial stable RTs extending to the white-white zone (type I); partial unstable RTs extending to the red-white zone (type II); complete RTs without gapping (type III), complete RTs with 3 mm gapping (type IV), and complete RTs with >3 mm gapping (type V). We adopted the MRI-based criteria described by Harper et al. [
36], where on MRI scans the posterior and anterior meniscal horns appear as low-signal triangles on sagittal scans. In contrast, the body has a triangular shape on coronal images. All RTs shared the truncated triangle sign (abrupt termination of the triangular meniscal contour at its tip on sagittal or coronal images) and the cleft sign (linear, vertical high signal extending through the meniscus on coronal or sagittal images). They also shared the marching cleft sign, where a cleft running in central or peripheral direction is detected on consecutive sagittal or coronal images.
2.5.3. Longitudinal Lesions
There is no universally accepted classification for LTs. Two widely used systems are based on circumferential zones [
37] or meniscal radial zones [
4]. Circumferential zones consist of zone 0, the meniscosynovial junction; zone 1, the outer third; zone 2, the middle third; and zone 3, the inner third. Radial zones categorize LTs based on their extension into the posterior, midbody, or anterior zones. MRI findings for LTs [
38] are linear hyperintensity on T2-weighted images; disruption of meniscal morphology with alterations running parallel to the circumferential fibers; meniscal extrusion (≥3 mm beyond the tibial plateau); and associated joint effusion.
2.5.4. Bucket-Handle Meniscal Tears
BHMTs can be classified according to Lim et al. [
39] based on reducibility and tear type into 3 types: type 1 rotates upward, type 2 rotates downward (both are easily reduced), whereas in type 3 the displaced central fragment is rotated by 180° or more and is difficult to reduce. MRI scans are evaluated in the sagittal plane for subchondral edema, the double posterior cruciate ligament sign [
20], the flipped meniscus sign, the absent bow sign, the disproportionate posterior horn sign, and/or the double anterior horn sign [
40]. In the coronal plane, they are examined for the intercondylar notch sign [
41] and in the axial plane for the V-sign and/or the double anterior cruciate ligament (ACL) sign [
40].
2.5.5. Meniscal Ramp Lesions
The most recent MRL classification, and the one adopted herein, is by Pimprikar and Patil [
42]. Type 1 involves injury only to the meniscocapsular junction without meniscotibial ligament (MTL) disruption and may only affect the synovium. Type 2 involves the meniscocapsular ligament (MCL) and the MTL, causing the posteromedial capsule to peel off from the inferior surface of the meniscus. Type 3 involves meniscal tissue, MCL, and MTL. MRLs can be detected on routine MRI. The most obvious finding is an irregularity or a longitudinal vertical tear in the peripheral zone of the posterior horn of the medial meniscus, with interposed thin fluid signal between the posterior horn of the medial meniscus and the posteromedial capsule [
43]. Additionally, there may be soft tissue edema between the meniscus and the collateral ligament, bone bruising in the posteromedial tibia from pivot shift, countercoup injury in the medial compartment, and anterior translation of the medial plateau in relation to the femoral condyle [
22].
2.5.6. Meniscal Root Tears
We have adopted the classification of LaPrade et al. [
44], which divides tears into five categories based on location and quality. Type 1: isolated, partial, and, therefore, stable root tears; type 2: complete root tear; type 3: tear with a concomitant longitudinal/circumferential tear (i.e., BHMT); type 4: oblique meniscal tear extending into the root, resulting in complete root detachment; type 5: complete bony avulsion fracture of the root from its attachment. Unlike other classifications, the LaPrade system applies to both the anterior and posterior roots [
28]. MRI is the most reliable non-invasive modality for MRT diagnosis [
28]. Specific signs include increased signal due to fluid collection near the roots, the ghost sign (sagittal cuts where the meniscus is not identifiable in its normal position), and meniscal extrusion >3 mm from the tibial articular cartilage in coronal views. A further sign is subchondral insufficiency fracture of the knee, i.e., bony edema of the femoral condyles or tibial plateau that seems to be caused by increased point-loading due to lack of meniscal support [
26].
2.5.7. Complex Meniscal Tears
There is currently no classification for CMTs. MRI is the diagnostic gold standard, the signal being dependent on the imaging patterns of each simple lesion within the CMT.
2.6. Types of Repair
The main exposure in this study refers to the type of meniscal repair technique employed, specifically the all-inside, inside-out, outside-in, and pull-out. The suture techniques employed to repair meniscal tears are based on lesion type and location. The four most widely used approaches are also those applied in the cases reviewed here.
2.6.1. All-Inside Technique
All-inside repair was performed through standard arthroscopic portals using the FAST-FIXTM Meniscal Repair System (Smith & Nephew, Andover, MD, USA) according to the manufacturer’s recommendations. Briefly, each FAST-FIX contains two 5 mm polymer-integrated bio-inert anchors (PEEK-OPTIMA® from Invibio®, Lancashire, UK) with a pretied, self-sliding knot comprising a 2-0, non-absorbable, UHMW polyethylene ULTRABRAIDTM suture. The entire system is packaged in an easy-to-insert integrated delivery needle. Sutures were placed until the desired stability was achieved.
2.6.2. Inside-Out Technique
A long and straight needle loaded with 2-0 non-absorbable sutures is inserted through an arthroscopic cannula and passed from the intra-articular side through the meniscus toward the outer capsule using a dedicated inside-out meniscal repair device. Sutures are placed approximately 1–2 mm from the tear margin to ensure optimal stabilization. To prevent iatrogenic injury, a small incision is made on the medial or lateral aspect of the knee at the level of the meniscus, and a spoon-shaped retractor is introduced to shield neurovascular structures. Once the sutures are successfully passed, both ends are retrieved through the extra-articular incision, where they are securely tied under direct visualization, ensuring adequate compression of the meniscal tissue while avoiding excessive tension that could compromise vascular supply.
2.6.3. Outside-In Technique
The outside-in technique involved using a 22G sterile lumbar spinal needle and slowly absorbable suture material (PDS 0). To prevent cheese-wiring, the second suture was crossed over the first.
2.6.4. Transtibial Pull-Out Technique
The transtibial tunnel pull-out technique is principally used for MRTs. A 3 cm incision is made adjacent to the tibial tubercle on the side of the tear. A tibial tunnel guide, opened at 60°, is used to ream the tunnel. Anatomical positioning of the tunnels in the posterior root attachment site should be visualized arthroscopically. Two simple sutures are passed through the meniscal root and shuttled down the tibial tunnel. After root reduction, the sutures through the tibial tunnel are tied over a button on the anterior tibia to avoid suture cut-in [
28].
2.7. Surgical Procedure
The patient in supine position was examined under anesthesia. The limb was placed in standard arthroscopic position with padding of all bony prominences. Following spinal anesthesia, tourniquet placement, and a time-out, standard medial and lateral transpatellar portals were opened, and diagnostic arthroscopy was performed to confirm the preoperative diagnosis. Once it was established that the tear was amenable to repair, its edges were freshened up using a shaver. One of the four repair techniques described above was then applied depending on lesion type and location. Regardless of repair type, sutures were placed along the tear at 5–7 mm intervals [
45,
46] until achievement of stability to probing. The knee was then copiously irrigated and closed in standard layered fashion.
2.8. Postoperative Rehabilitation
All patients followed the same rehabilitation protocol, designed to maximize healing and functional recovery and to eliminate an important potential confounder. Weight bearing was not allowed for three weeks, followed by progressive partial load for the next two weeks. Crutches must be used for six weeks after surgery. Patients wore a brace locked in extension for the first ten days, unlocking to 0–60° in the following week, and to 0–90° in the subsequent week. Once adequate quadriceps strength was achieved, typically around four to five weeks, the immobilizer brace was discontinued, with a progressive increase in flexion. Initially, exercises focused on quadriceps sets, straight-leg raises, heel slides, and patellar mobilization. Subsequently, closed-chain exercises, lunges (0–90°), leg presses (0–90°), proprioceptive training, and a stationary bike were gradually introduced. From weeks 12 to 16, patients progressed to further strengthening exercises, including single-leg strengthening, jogging, and a gradual transition to running. Sport-specific exercises were incorporated as recovery progressed.
2.9. Statistical Analysis
We used Microsoft Excel (version 16.75.2, Redmond, WA, USA) in conjunction with the XLSTAT resource pack (XLSTAT-Premium, Addinsoft Inc., New York, NY, USA) for all analyses. All continuous data are expressed as mean and standard deviation (SD), whereas categorical variables are expressed as frequency and percentages. The Chi-square test or Fisher’s exact test was used for categorical data as appropriate. A p-value < 0.05 was statistically significant.