Effectiveness of Subcutaneous Negative-Suction Drain on Surgical Site Infection After Ileostomy Reversal: A Propensity Score Matching Analysis
Abstract
1. Introduction
2. Methods
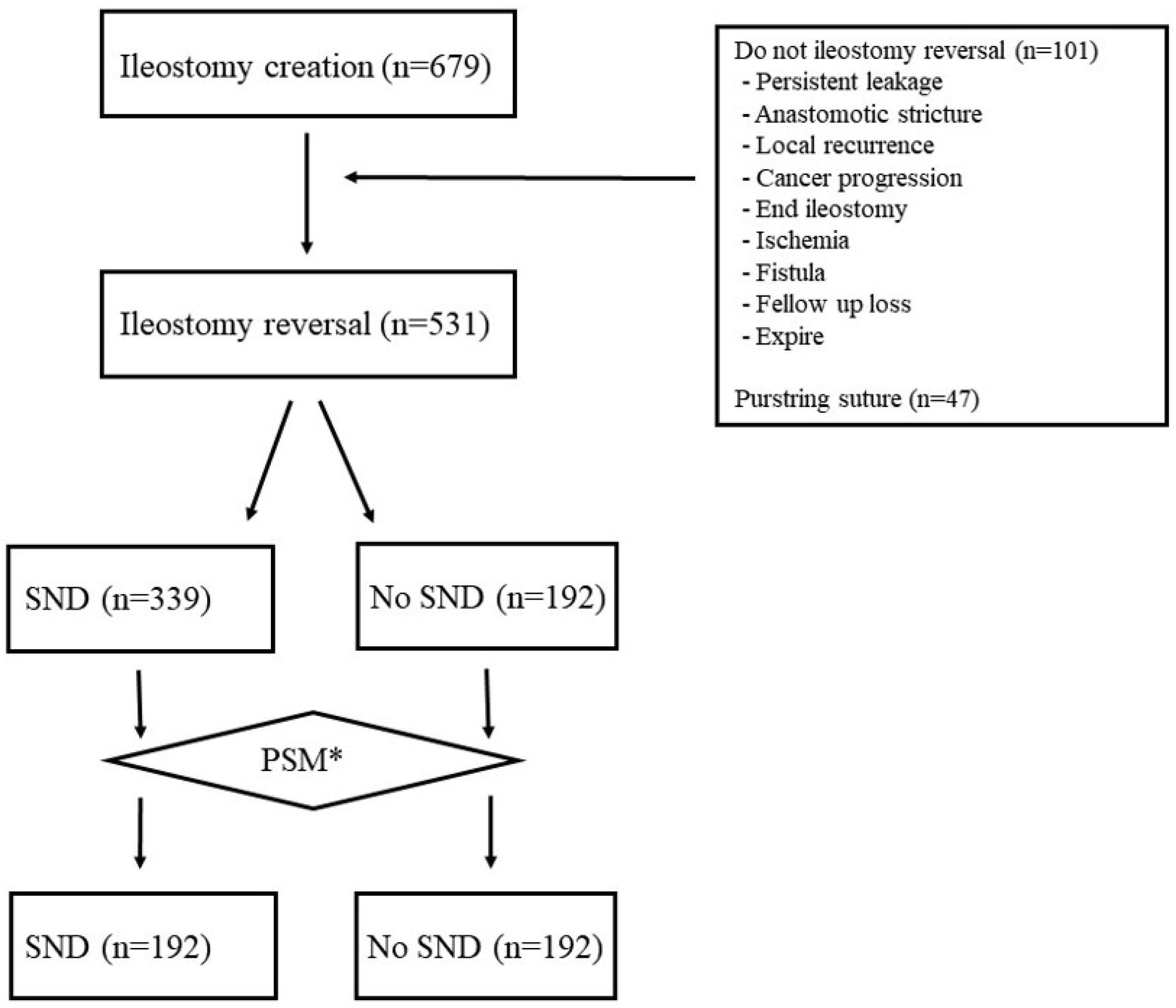
2.1. Study Design
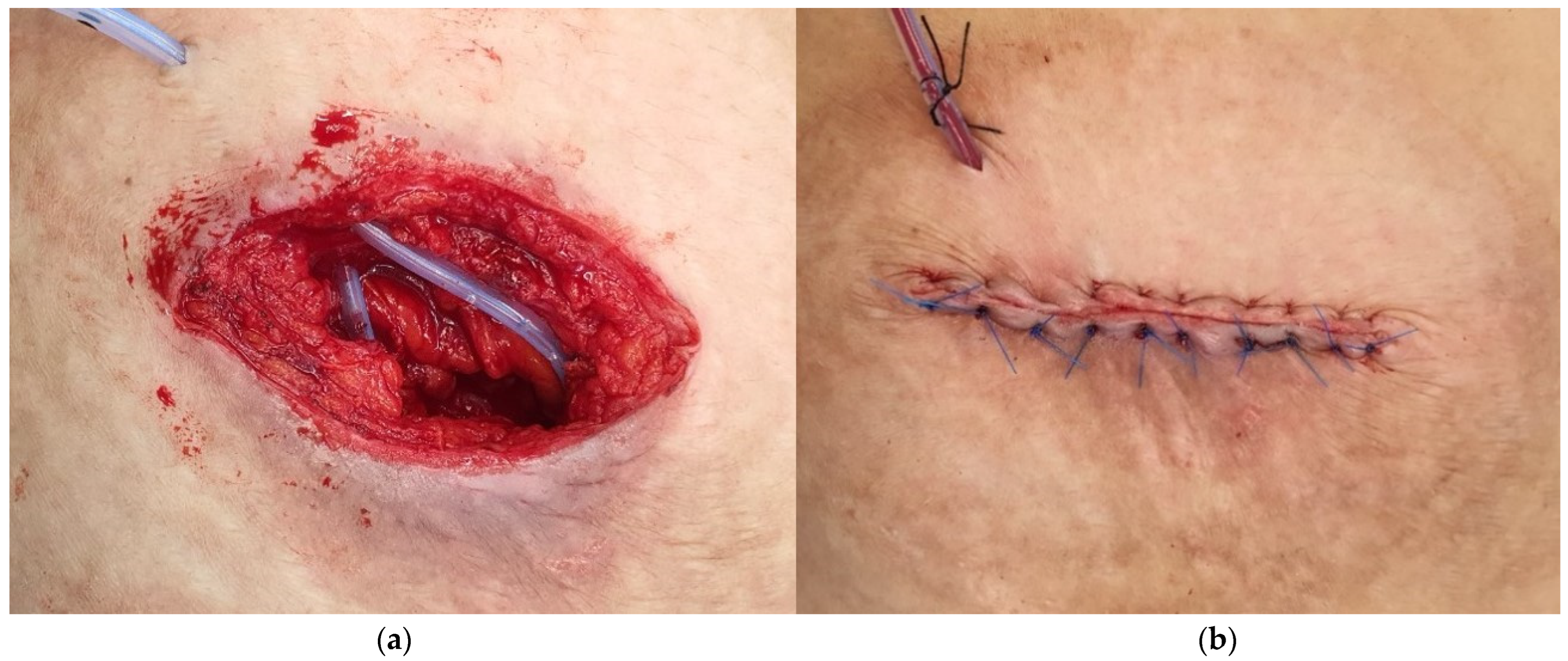
2.2. Surgical Procedure
2.3. Postoperative Care
2.4. Statistics
2.5. Research Ethics
3. Results
4. Discussion
5. Limitations and Strengths
6. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Degiuli, M.; Elmore, U.; De Luca, R.; De Nardi, P.; Tomatis, M.; Biondi, A.; Persiani, R.; Solaini, L.; Rizzo, G.; Soriero, D.; et al. Risk factors for anastomotic leakage after anterior resection for rectal cancer (RALAR study): A nationwide retrospective study of the Italian Society of Surgical Oncology Colorectal Cancer Network Collaborative Group. Color. Dis. 2022, 24, 264–276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Den Dulk, M.; Marijnen, C.A.; Collette, L.; Putter, H.; Påhlman, L.; Folkesson, J.; Bosset, J.-F.; Rödel, C.; Bujko, K.; van de Velde, C.J.H. Multicentre analysis of oncological and survival outcomes following anastomotic leakage after rectal cancer surgery. Br. J. Surg. 2009, 96, 1066–1075. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Ding, F.; Xu, T.; Pan, Z.; Zhuang, J.; Liu, X.; Guan, G. Double-stapled anastomosis without “dog-ears” reduces the anastomotic leakage in laparoscopic anterior resection of rectal cancer: A prospective, randomized, controlled study. Front. Surg. 2022, 9, 1003854. [Google Scholar] [CrossRef] [PubMed]
- Tschann, P.; Weigl, M.P.; Szeverinski, P.; Lechner, D.; Brock, T.; Rauch, S.; Rossner, J.; Eiter, H.; Girotti, P.N.; Jäger, T.; et al. Are risk factors for anastomotic leakage influencing long-term oncological outcomes after low anterior resection of locally advanced rectal cancer with neoadjuvant therapy? A single-Centre cohort study. Langenbecks Arch. Surg. 2022, 407, 2945–2957. [Google Scholar] [CrossRef]
- Law, W.L.; Chu, K.W. Anterior resection for rectal cancer with mesorectal excision: A prospective evaluation of 622 patients. Ann. Surg. 2004, 240, 260–268. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lim, M.; Akhtar, S.; Sasapu, K.; Harris, K.; Burke, D.; Sagar, P.; Finan, P. Clinical and subclinical leaks after low colorectal anastomosis: A clinical and radiologic study. Dis. Colon Rectum 2006, 49, 1611–1619. [Google Scholar] [CrossRef] [PubMed]
- Kaistha, S.; Panwar, R.; Pal, S.; Dash, N.R.; Sahni, P.; Chattopadhyay, T.K. Wound Infection After Ileostomy Closure: An Interim Analysis of a Prospective Randomized Study Comparing Primary Versus Circumferential Subcuticular Closure Techniques. Surg. Infect. 2023, 24, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Emile, S.H.; Horesh, N.; Garoufalia, Z.; Gefen, R.; Ray-Offor, E.; Wexner, S.D. Outcomes of Early Versus Standard Closure of Diverting Ileostomy After Proctectomy: Meta-analysis and Meta-regression Analysis of Randomized Controlled Trials. Ann. Surg. 2024, 279, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Chow, A.; Tilney, H.S.; Paraskeva, P.; Jeyarajah, S.; Zacharakis, E.; Purkayastha, S. The morbidity surrounding reversal of defunctioning ileostomies: A systematic review of 48 studies including 6,107 cases. Int. J. Color. Dis. 2009, 24, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Kaidar-Person, O.; Person, B.; Wexner, S.D. Complications of construction and closure of temporary loop ileostomy. J. Am. Coll. Surg. 2005, 201, 759–773. [Google Scholar] [CrossRef]
- Wong, K.-S.; Remzi, F.H.; Gorgun, E.; Arrigain, S.; Church, J.M.; Preen, M.; Fazio, V.W. Loop ileostomy closure after restorative proctocolectomy: Outcome in 1504 patients. Dis Colon Rectum 2005, 48, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Ohara, Y.; Owada, Y.; Kim, J.; Moue, S.; Akashi, Y.; Ogawa, K.; Takahashi, K.; Shimomura, O.; Furuya, K.; Hashimoto, S.; et al. Clinical Benefits of Reducing Dead Space Using a Closed Suction Drain and Subcutaneous Large-bite Buried Suture Technique to Prevent Superficial Surgical-site Infections Following Primary Closure of a Diverting Stoma. J. Anus Rectum Colon 2024, 8, 70–77. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tiang, T.; Behrenbruch, C.; Noori, J.; Lam, D.; Bhamidipaty, M.; Johnston, M.; Woods, R.; D’Souza, B. Prophylactic negative pressure wound therapy to improve wound healing rates following ileostomy closure: A randomized controlled trial. ANZ J. Surg. 2024, 94, 1627–1633. [Google Scholar] [CrossRef] [PubMed]
- Jeong, Y.S.; Cho, S.H.; Park, B.S.; Son, G.M.; Kim, H.S. Role of subcutaneous closed suction drain in the prevention of incisional surgical site infection after loop ileostomy reversal with purse-string skin closure: A retrospective observational study. BMC Surg. 2024, 24, 252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chu, D.I.; Schlieve, C.R.; Colibaseanu, D.T.; Simpson, P.J.; Wagie, A.E.; Cima, R.R.; Habermann, E.B. Surgical site infections (SSIs) after stoma reversal (SR): Risk factors, implications, and protective strategies. J. Gastrointest. Surg. 2015, 19, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.D.; Wang, L.; Peng, Y.F.; Li, M.; Yao, Y.F.; Zhao, J.; Zhan, T.-C.; Du, C.-Z.; Gu, J. Subcutaneous vacuum drains reduce surgical site infection after primary closure of defunctioning ileostomy. Int. J. Color. Dis. 2015, 30, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Lauscher, J.C.; Schneider, V.; Lee, L.D.; Stroux, A.; Buhr, H.J.; Kreis, M.E.; Ritz, J.P. Necessity of subcutaneous suction drains in ileostomy reversal (DRASTAR)-a randomized, controlled bi-centered trial. Langenbecks Arch. Surg. 2016, 401, 409–418. [Google Scholar] [CrossRef]
- Watanabe, J.; Ota, M.; Kawamoto, M.; Akikazu, Y.; Suwa, Y.; Suwa, H.; Momiyama, M.; Ishibe, A.; Watanabe, K.; Masui, H.; et al. A randomized controlled trial of subcutaneous closed-suction Blake drains for the prevention of incisional surgical site infection after colorectal surgery. Int. J. Color. Dis. 2017, 32, 391–398. [Google Scholar] [CrossRef]
- Mirande, M.D.; McKenna, N.P.; Bews, K.A.; Shawki, S.F.; Cima, R.R.; Brady, J.T.; Colibaseanu, D.T.; Mathis, K.L.; Kelley, S.R. Risk factors for surgical site infections and trends in skin closure technique after diverting loop ileostomy reversal: A multi-institutional analysis. Am. J. Surg. 2023, 226, 703–708. [Google Scholar] [CrossRef]
- ACS NSQIP Surgical Risk Calculator. American College of Surgeons National Surgical Quality Improvement Program. Available online: https://riskcalculator.facs.org/RiskCalculator/ (accessed on 23 April 2022).
- Amodu, L.I.; Hakmi, H.; Sohail, A.H.; Akerman, M.; Petrone, P.; Halpern, D.K.; Sonoda, T. Laparoscopic Hartmann’s procedure for complicated diverticulitis is associated with lower superficial surgical site infections compared to open surgery with similar other outcomes: A NSQIP-based, propensity score matched analysis. Eur. J. Trauma Emerg. Surg. 2024, 50, 2097–2103. [Google Scholar] [CrossRef] [PubMed]
- Nasseri, Y.; Liu, A.; Kasheri, E.; Oka, K.; Langenfeld, S.; Smiley, A.; Cohen, J.; Ellenhorn, J.; Barnajian, M. Hartmann’s reversal is associated with worse outcomes compared to elective left colectomy: A NSQIP analysis of 36,794 cases. Am. J. Surg. 2022, 224, 1351–1355. [Google Scholar] [CrossRef] [PubMed]
- Aimaq, R.; Akopian, G.; Kaufman, H.S. Surgical site infection rates in laparoscopic versus open colorectal surgery. Am. Surg. 2011, 77, 1290–1294. [Google Scholar] [CrossRef] [PubMed]
- McCracken, E.K.E.; Mureebe, L.; Blazer, D.G., 3rd. Minimally Invasive Surgical Site Infection in Procedure-Targeted ACS NSQIP Pancreaticoduodenectomies. J. Surg. Res. 2019, 233, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Ortega, G.; Rhee, D.S.; Papandria, D.J.; Yang, J.; Ibrahim, A.M.; Shore, A.D.; Makary, M.A.; Abdullah, F. An evaluation of surgical site infections by wound classification system using the ACS-NSQIP. J. Surg. Res. 2012, 174, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Manigrasso, M.; Degiuli, M.; Maione, F.; Venetucci, P.; Roviello, F.; De Palma, G.D.; Milone, M.; SICO-CCN Collaborative Group. Is proctoscopy sufficient for the evaluation of colorectal anastomosis prior to ileostomy reversal? A nationwide retrospective analysis of the Italian Society of Surgical Oncology Colorectal Cancer Network Collaborative group (SICO-CCN). Color. Dis. 2024, 26, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.; El-Hussuna, A.; Gallo, G.; Keatley, J.; Kelly, M.E.; Minaya-Bravo, A.; Ovington, L.; Pata, F.; Pellino, G.; Pinkney, T.; et al. An international assessment of surgeon practices in abdominal wound closure and surgical site infection prevention by the European Society for Coloproctology. Color. Dis. 2023, 25, 1014–1025. [Google Scholar] [CrossRef] [PubMed]
- Vermulst, N.; Vermeulen, J.; Hazebroek, E.J.; Coene, P.P.; van der Harst, E. Primary closure of the skin after stoma closure. Management of wound infections is easy without (long-term) complications. Dig. Surg. 2006, 23, 255–258. [Google Scholar] [CrossRef] [PubMed]
- Lahat, G.; Tulchinsky, H.; Goldman, G.; Klauzner, J.M.; Rabau, M. Wound infection after ileostomy closure: A prospective randomized study comparing primary vs. delayed primary closure techniques. Tech. Coloproctol. 2005, 9, 206–208. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, D.P.; Carter, M.; Wijewardene, D.; Burton, M.; Waldron, D.; Condon, E.; Coffey, J.C.; Peirce, C. The effect of purse-string approximation versus linear approximation of ileostomy reversal wounds on morbidity rates and patient satisfaction: The ’STOMA’ trial. Tech. Coloproctol. 2017, 21, 863–868. [Google Scholar] [CrossRef] [PubMed]
- Ban, K.A.; Minei, J.P.; Laronga, C.; Harbrecht, B.G.; Jensen, E.H.; Fry, D.E.; Itani, K.M.; Dellinger, E.P.; Ko, C.Y.; Duane, T.M. Executive summary of the American college of surgeons/surgical infection society surgical site infection guidelines-2016 update. Surg. Infect. 2017, 18, 379–382. [Google Scholar] [CrossRef]
- Peltrini, R.; Ferrara, F.; Parini, D.; Pacella, D.; Vitiello, A.; Scognamillo, F.; Pilone, V.; Pietroletti, R.; De Nardi, P.; Stoma Closure Collaborative Group. Current approach to loop ileostomy closure: A nationwide survey on behalf of the Italian Society of ColoRectal Surgery (SICCR). Updates Surg. 2024; Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Wierdak, M.; Pisarska-Adamczyk, M.; Wysocki, M.; Major, P.; Kołodziejska, K.; Nowakowski, M.; Vongsurbchart, T.; Pędziwiatr, M. Prophylactic negative-pressure wound therapy after ileostomy reversal for the prevention of wound healing complications in colorectal cancer patients: A randomized controlled trial. Tech. Coloproctol. 2021, 25, 185–193. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Okuya, K.; Takemasa, I.; Tsuruma, T.; Noda, A.; Sasaki, K.; Ueki, T.; Mukaiya, M.; Saito, K.; Okita, K.; Nishidate, T.; et al. Evaluation of negative-pressure wound therapy for surgical site infections after ileostomy closure in colorectal cancer patients: A prospective multicenter study. Surg. Today 2020, 50, 1687–1693. [Google Scholar] [CrossRef] [PubMed]
- Curchod, P.; Clerc, D.; Jurt, J.; Hubner, M.; Hahnloser, D.; Demartines, N.; Grass, F. Closed-wound negative pressure therapy dressing after loop ostomy closure: A retrospective comparative study. Sci. Rep. 2022, 12, 7790. [Google Scholar] [CrossRef] [PubMed]
- Brook, A.J.; Mansfield, S.D.; Daniels, I.R.; Smart, N.J. Incisional hernia following closure of loop ileostomy: The main predictor is the patient, not the surgeon. Surgeon 2018, 16, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Barranquero, A.G.; Tobaruela, E.; Bajawi, M.; Muñoz, P.; Die Trill, J.; Garcia-Perez, J.C. Incidence and risk factors for incisional hernia after temporary loop ileostomy closure: Choosing candidates for prophylactic mesh placement. Hernia 2020, 24, 93–98. [Google Scholar] [CrossRef] [PubMed]
| Before Propensity Score Matching | After Propensity Score Matching | |||||
|---|---|---|---|---|---|---|
| SND (n = 339) | No SND (n = 192) | p-Value | SND (n = 192) | No SND (n = 192) | p-Value | |
| Sex | 0.815 | 0.317 | ||||
| Male | 223 (65.8%) | 129 (67.2%) | 139 (72.4%) | 129 (67.2%) | ||
| Female | 116 (34.2%) | 63 (32.8%) | 53 (27.6%) | 63 (32.8%) | ||
| Age (years) | 63.1 ± 12.5 | 60.6 ± 11.0 | 0.023 | 60.8 ± 11.9 | 60.6 ± 11.0 | 0.859 |
| BMI * (kg/m2) | 23.8 ± 3.1 | 24.0 ± 3.4 | 0.454 | 23.8 ± 3.0 | 24.0 ± 3.4 | 0.434 |
| ASA classification + | 1.000 | 0.638 | ||||
| 1 and 2 | 324 (95.6%) | 184 (95.8%) | 181 (94.3%) | 184 (95.8%) | ||
| 3 | 15 (4.4%) | 8 (4.2%) | 11 (5.7%) | 8 (4.2%) | ||
| Estimated SSI risk by ACS NSQIP § risk calculator (%) | 5.4 ± 1.1 | 5.6 ± 1.1 | 0.224 | 5.5 ± 1.1 | 5.6 ± 1.1 | 0.870 |
| Diagnosis | 0.851 | 0.659 | ||||
| T-colon ca. € | 1 (0.3%) | 0 (0.0%) | 1 (0.5%) | 0 (0.0%) | ||
| S-colon ca. ¥ | 14 (4.1%) | 8 (4.2%) | 10 (5.2%) | 8 (4.2%) | ||
| RS colon ca. $ | 1 (0.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Rectal ca. £ | 320 (94.4%) | 183 (95.3%) | 179 (93.2%) | 183 (95.3%) | ||
| FAP ♀ | 3 (0.9%) | 1 (0.5%) | 2 (1.0%) | 1 (0.5%) | ||
| Reversal interval (days) | 168.0 ± 128.9 | 151.5 ± 141.0 | 0.173 | 193.3 ± 151.6 | 151.5 ± 141.0 | 0.005 |
| Parastomal hernia | 49 (14.5%) | 16 (8.3%) | 0.054 | 16 (8.3%) | 16 (8.3%) | 1.000 |
| Before Propensity Score Matching | After Propensity Score Matching | |||||
|---|---|---|---|---|---|---|
| SND (n = 339) | No SND (n = 192) | p-Value | SND (n = 192) | No SND (n = 192) | p-Value | |
| Short-term Morbidity | 19 (5.6%) | 27 (14.1%) | 0.002 | 17 (8.9%) | 27 (14.1%) | 0.199 |
| SSI * | 12 (3.5%) | 25 (13.0%) | <0.001 | 10 (5.2%) | 25 (13.0%) | 0.013 |
| Ileus | 6 (1.8%) | 4 (2.1%) | 0.320 | 6 (3.1%) | 4 (2.1%) | 0.254 |
| Etc. | 2 (0.6%) | 1 (0.5%) | 0.752 | 2 (1.0%) | 1 (0.5%) | 0.701 |
| Incisional hernia | 3 (0.9%) | 8 (4.2%) | 0.025 | 3 (1.6%) | 7 (3.6%) | 0.336 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.M.; Kim, J.H.; Kim, M.J.; Lim, C.D.; Lee, Y.S. Effectiveness of Subcutaneous Negative-Suction Drain on Surgical Site Infection After Ileostomy Reversal: A Propensity Score Matching Analysis. J. Clin. Med. 2025, 14, 236. https://doi.org/10.3390/jcm14010236
Song JM, Kim JH, Kim MJ, Lim CD, Lee YS. Effectiveness of Subcutaneous Negative-Suction Drain on Surgical Site Infection After Ileostomy Reversal: A Propensity Score Matching Analysis. Journal of Clinical Medicine. 2025; 14(1):236. https://doi.org/10.3390/jcm14010236
Chicago/Turabian StyleSong, Ju Myung, Ji Hoon Kim, Moon Jin Kim, Chae Dong Lim, and Yoon Suk Lee. 2025. "Effectiveness of Subcutaneous Negative-Suction Drain on Surgical Site Infection After Ileostomy Reversal: A Propensity Score Matching Analysis" Journal of Clinical Medicine 14, no. 1: 236. https://doi.org/10.3390/jcm14010236
APA StyleSong, J. M., Kim, J. H., Kim, M. J., Lim, C. D., & Lee, Y. S. (2025). Effectiveness of Subcutaneous Negative-Suction Drain on Surgical Site Infection After Ileostomy Reversal: A Propensity Score Matching Analysis. Journal of Clinical Medicine, 14(1), 236. https://doi.org/10.3390/jcm14010236






