Validation of the OPTIMAL-Confidence Questionnaire in Patients with Chronic Low Back Pain
Abstract
1. Introduction
- -
- The first objective was to evaluate the reliability and validity of the confidence subscale of the OPTIMAL instrument in individuals with chronic low back pain. This involved a thorough psychometric analysis, including assessments of internal consistency and construct validity through comparisons with established measures;
- -
- The second objective was to describe the levels of confidence in movement capacity within this population. This descriptive analysis aimed to provide a comprehensive characterization of the population’s confidence levels, enhancing the understanding of movement-related confidence in individuals with chronic low back pain.
2. Material and Methods
2.1. Design
2.2. Study Setting and Sample
2.3. Inclusion and Exclusion Criteria
2.4. Instruments
2.5. Data Collection
2.6. Data Analysis
2.7. Ethical Considerations
3. Results
3.1. Characteristics of the Sample
3.2. Psychometric Properties of the OPTIMAL-Confidence
4. Discussion
4.1. Limitations
4.2. Recommendations of Further Research
4.3. Implications for Policy and Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef]
- Merskey, H.; Albe-Fessard, D.G.; Bonica, J.J. International Association for the Study of Pain. Pain Terms: A list with definitions and notes on usage. Pain 1979, 6, 205–208. [Google Scholar]
- GBD 2021 Low Back Pain Collaborators. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e316–e329. [Google Scholar] [CrossRef]
- Soriano, J.B.; Rojas-Rueda, D.; Alonso, J.; Antó, J.M.; Cardona, P.-J.; Fernández, E.; Garcia-Basteiro, A.L.; Glenn, S.D.; Krish, V.; Lazarus, J.V.; et al. The burden of disease in Spain: Results from the Global Burden of Disease 2016. Med. Clin. 2018, 151, 171–190. [Google Scholar] [CrossRef]
- Moix-Queraltó, M.-J.; Vidal-Fernández, J. Aetiology, chronification, and treatment of low back pain. Clínica Salud 2008, 19, 379–392. [Google Scholar]
- George, S.Z.; Fritz, J.M.; Silfies, S.P.; Michael Schneider, D.C.; Lentz, T.A.; Gilliam, J.R. Low Back Pain Decision Tree. Orthop. Phys. Ther. Pract. 2022, 34, 262–267. [Google Scholar]
- Morlion, B.; Coluzzi, F.; Aldington, D.; Kocot-Kepska, M.; Pergolizzi, J.; Mangas, A.C.; Ahlbeck, K.; Kalso, E. Pain chronification: What should a non-pain medicine specialist know? Curr. Med. Res. Opin. 2018, 34, 1169–1178. [Google Scholar] [CrossRef] [PubMed]
- Matheve, T.; Coluzzi, F.; Aldington, D.; Kocot-Kepska, M.; Pergolizzi, J.; Mangas, A.C.; Ahlbeck, K.; Kalso, E. The Relationship Between Pain-Related Psychological Factors and Maximal Physical Performance in Low Back Pain: A Systematic Review and Meta-Analysis. J. Pain 2022, 23, 2036–2051. [Google Scholar] [CrossRef]
- Pinho, H.; Neves, M.; Costa, F.; Silva, A.G. Associations between pain intensity, pain sensitivity, demographics, psychological factors, disability, physical activity, pain phenotype and COVID-19 history in low back pain: An observational study. Physiother. Res. Int. 2024, 29, e2094. [Google Scholar] [CrossRef]
- Gilliam, J.R.; Sahu, P.K.; Vendemia, J.M.C.; Silfies, S.P. Association between seated trunk control and cortical sensorimotor white matter brain changes in patients with chronic low back pain. PLoS ONE 2024, 19, e0309344. [Google Scholar] [CrossRef] [PubMed]
- de Góes Salvetti, M.; de Mattos Pimenta, C.A. Chronic pain and the belief in self-efficacy. Rev. Esc. Enferm. USP 2007, 41, 135–140. [Google Scholar] [CrossRef]
- Coyne, N.C.; Baez, S.; Murro, M.; Derrico, D.; Mancinelli, C.A.; Jochimsen, K.N. Pain Self-efficacy Is Associated With Patient-Reported Function in Individuals With Chronic Hip Pain. JOSPT Open 2024, 2, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Cameron, N.; Kool, M.; Estévez-López, F.; López-Chicheri, I.; Geenen, R. The potential buffering role of self-efficacy and pain acceptance against invalidation in rheumatic diseases. Rheumatol. Int. 2018, 38, 283–291. [Google Scholar] [CrossRef]
- Guccione, A.A.; Mielenz, T.J.; DeVellis, R.F.; Goldstein, M.S.; Freburger, J.K.; Pietrobon, R.; Miller, S.C.; Callahan, L.F.; Harwood, K.; Carey, T.S. Development and testing of a self-report instrument to measure actions: Outpatient physical therapy improvement in movement assessment log (OPTIMAL). Phys. Ther. 2005, 85, 515–530. [Google Scholar] [CrossRef]
- Pinto-Carral, A.; Fernández-Villa, T.; Guccione, A.A.; Cuadrado, F.M.; Cancela, J.M.; Validity, A.J.M. Reliability, and Responsiveness of the Spanish Version of the OPTIMAL Instrument. PM R J. Inj. Funct. Rehabil. 2019, 11, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J. Clin. Epidemiol. 2010, 63, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Delitto, A.; George, S.Z.; Van Dillen, L.; Whitman, J.M.; Sowa, G.; Shekelle, P.; Denninger, T.R.; Godges, J.J.; Beneciuk, J.M.; Bishop, M.D.; et al. Low back pain. J. Orthop. Sports Phys. Ther. 2012, 42, A1–A57. [Google Scholar] [CrossRef] [PubMed]
- Downie, W.W.; Leatham, P.A.; Rhind, V.M.; Wright, V.; Branco, J.A.; Anderson, J.A. Studies with pain rating scales. Ann. RheumDis. 1978, 378–381. [Google Scholar] [CrossRef]
- Allen, D.D. Validity and reliability of the movement ability measure: A self-report instrument proposed for assessing movement across diagnoses and ability levels. Phys. Ther. 2007, 87, 899–916. [Google Scholar] [CrossRef]
- Anderson, K.O.; Dowds, B.N.; Pelletz, R.; Edwards, T.; Peeters-Asdourian, C. Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain. Pain 1995, 63, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Martín-Aragón, M.; Pastor, M.A.; Rodríguez-Marín, J.; March, M.J.; Lledó, A. Percepción de autoeficacia en dolor crónico. Adaptación y validación de la chronic pain self efficacy scale. J. Health Psychol. 1999, 11, 53–75. [Google Scholar]
- Mishra, P.; Pandey, C.M.; Singh, U.; Gupta, A.; Sahu, C.; Keshri, A. Descriptive Statistics and Normality Tests for Statistical Data. Ann. Card. Anaesth. 2019, 22, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Vrbin, C.M. Parametric or nonparametric statistical tests: Considerations when choosing the most appropriate option for your data. Cytopathology 2022, 33, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Vaske, J.J.; Beaman, J.; Sponarski, C.C. Rethinking Internal Consistency in Cronbach’s Alpha. Leis. Sci. 2017, 39, 163–173. [Google Scholar] [CrossRef]
- Karasawa, Y.; Yamada, K.; Iseki, M.; Yamaguchi, M.; Murakami, Y.; Tamagawa, T.; Kadowaki, F.; Hamaoka, S.; Ishii, T.; Kawai, A.; et al. Association between change in self-efficacy and reduction in disability among patients with chronic pain. PLoS ONE 2019, 14, e0215404. [Google Scholar] [CrossRef]
- Raman, S.; Sharma, P. Self—Efficacy as a mediator of the relationship between pain and disability in chronic pain patients: A narrative review. Bull. Fac. Phys. Ther. 2022, 27, 42. [Google Scholar] [CrossRef]
- Alvani, E.; Sheikhi, B.; Letafatkar, A.; Rossettini, G. Effects of pain neuroscience education combined with neuromuscular exercises on pain, functional disability and psychological factors in chronic low back pain: A study protocol for a single-blind randomized controlled trial. PLoS ONE 2024, 19, e0309679. [Google Scholar] [CrossRef]
- Benedict, T.M.; Nitz, A.J.; Gambrel, M.K.; Louw, A. Pain neuroscience education improves post-traumatic stress disorder, disability, and pain self-efficacy in veterans and service members with chronic low back pain: Preliminary results from a randomized controlled trial with 12-month follow-up. Mil. Psychol. 2024, 36, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Touche, R.L.; Grande-Alonso, M.; Arnés-Prieto, P.; Paris-Alemany, A. How does self-efficacy influence pain perception, postural stability and range of motion in individuals with chronic low back pain? Pain Physician 2019, 22, E1–E13. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, T.; Göz, E.; Genç, A. The association between self-reported low back pain and lower limb disability as well as the association between neck pain and upper limb disability. Agri. Agri. (Algoloji) Dernegi’nin Yayin. Organidir J. Turk. Soc. Algol. 2017, 29, 1–8. [Google Scholar] [CrossRef]
- Sugavanam, T.; Sannasi, R.; Anand, P.A.; Javia, P.A. Postural asymmetry in low back pain—A systematic review and meta-analysis of observational studies. Disabil. Rehabil. 2024, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Tikhile, P.; Patil, D.S.; Jaiswal, P.R. Management of Low Back Pain With Concurrent Hamstring Tightness: A Case Report Highlighting the Efficacy of Proprioceptive Neuromuscular Facilitation, Mulligan’s Two-Leg Rotation Technique, and Exercise Regimen. Cureus 2024, 16, e58705. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, R.; Parhampour, B.; Pourahmadi, M.R.; Fazeli, S.H.; Takamjani, I.E.; Akbari, M.; Dadgoo, M. The Effect of Core Stabilization Exercises on Trunk-Pelvis Three-Dimensional Kinematics During Gait in Non-Specific Chronic Low Back Pain. Spine 2019, 44, 927–936. [Google Scholar] [CrossRef]
- Suh, J.H.; Kim, H.; Jung, G.P.; Ko, J.Y.; Ryu, J.S. The effect of lumbar stabilization and walking exercises on chronic low back pain. Medicine 2019, 98, e16173. [Google Scholar] [CrossRef]
- Zhang, Z.; Zou, J.; Lu, P.; Hu, J.; Cai, Y.; Xiao, C.; Li, G.; Zeng, Q.; Zh eng, M.; Huang, G. Analysis of lumbar spine loading during walking in patients with chronic low back pain and healthy controls: An OpenSim-Based study. Front. Bioeng. Biotechnol. 2024, 12, 1377767. [Google Scholar] [CrossRef]
- Reid, M.C.; Williams, C.S.; Gill, T.M. The relationship between psychological factors and disabling musculoskeletal pain in community-dwelling older persons. J. Am. Geriatr. Soc. 2003, 51, 1092–1098. [Google Scholar] [CrossRef]
- LaPlante, M.P.; Kaye, H.S. Demographics and trends in wheeled mobility equipment use and accessibility in the community. Assist. Technol. Off. J. RESNA 2010, 22, 3–17, quiz 19. [Google Scholar] [CrossRef] [PubMed]
- Edwards, R.R.; Dworkin, R.H.; Sullivan, M.D.; Turk, D.C.; Wasan, A.D. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. J. Pain 2016, 17, T70-92. [Google Scholar] [CrossRef]
- Shigetoh, H.; Abiko, T.; Ohyama, M.; Sakata, E.; Murata, S. Associations of Central Sensitization-Related Symptoms with Low Back Pain-Related Factors and Work Status in Caregivers. Int. J. Environ. Res. Public Health 2022, 19, 10135. [Google Scholar] [CrossRef] [PubMed]
- Elston, B.; Goldstein, M.; Makambi, K.H. Item response theory analysis of the Outpatient Physical Therapy Improvement in Movement Assessment Log (OPTIMAL). Phys. Ther. 2013, 93, 661–671. [Google Scholar] [CrossRef]
- Sidiq, M.; Muzaffar, T.; Janakiraman, B.; Masoodi, S.; Vasanthi, R.K.; Ramachandran, A.; Bansal, N.; Chahal, A.; Kashoo, F.Z.; Rizvi, M.R.; et al. Effects of pain education on disability, pain, quality of life, and self-efficacy in chronic low back pain: A randomized controlled trial. PLoS ONE 2024, 19, e0294302. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.J.; Hur, Y.; Lee, B. A study of the relationship among fear-avoidance beliefs, pain and disability index in patients with low back pain. J. Exerc. Rehabil. 2013, 9, 532–535. [Google Scholar] [CrossRef] [PubMed]
| Low Back Pain (N = 122) n (%) | CI § 95% | Healthy Population (N = 30) n (%) | CI § 95% | p-Value | |
|---|---|---|---|---|---|
| Age † | 58.61 ± 13.08 | 55.10 ± 13.06 | 0.19 | ||
| Gender | 0.67 | ||||
| Men | 50(41) | (32.2–50.3) | 11(36.7) | (19.9–56.1) | |
| Women | 72(59) | (49.7–67.8) | 19(63.3) | (43.9–80.1) | |
| BMI † | 27.62 ± 4.96 | 25.68 ± 3.90 | 0.05 | ||
| Area of residence | 0.03 | ||||
| Rural | 46(37.7) | (29.1–46.9) | 5(16.7) | (5.6–34.7) | |
| Urban | 76(62.3) | (53.1–70.9) | 25(83.3) | (65.3–94.4) | |
| Marital status | 0.37 | ||||
| Married | 79(64.8) | (55.6–73.2) | 18(60.0) | (40.6–77.3) | |
| Single | 22(18) | (11.7–26) | 9(30.0) | (14.7–49.4) | |
| Divorced | 13(10.7) | (5.8–17.5) | 1(3.3) | (0.1–17.2) | |
| Widowed | 8(6.6) | (2.9–12.5) | 2(6.7) | (0.8–22.1) | |
| Education | 0.05 | ||||
| Primary | 43(35.2) | (26.8–44.4) | 3(10.0) | (2.1–26.5) | |
| High School/Vocational Training | 58(47.2) | (38.4–56.8) | 19(63.3) | (43.9–80.1) | |
| University | 21(17.2) | (11–25.1) | 8(26.7) | (13.3–45.9) | |
| Employment | 0.50 | ||||
| Active | 66(54.1) | (44.8–63.2) | 16(53.3) | (34.3–71.7) | |
| Unemployed | 8(6.6) | (2.9–12.5) | 3(10.0) | (2.1–26.5) | |
| Retired | 31(25.4) | (18–34.1) | 10(33.3) | (17.3–52.8) | |
| Student | 0(0) | (0–3) | 0(0.0) | (0.0–11.6) | |
| Disabled | 5(4.1) | (1.3–9.3) | 0(0.0) | (0.0–11.6) | |
| Household chores | 12(9.8) | (5.2–16.6) | 1(3.3) | (0.1–17.2) | |
| Chronic diseases | <0.001 | ||||
| No disease | 32(26.2) | (18.7–35.0) | 22(73.3) | (54.1–87.7) | |
| One disease | 32(26.2) | (18.7–35.0) | 6(20.0) | (7.7–38.6) | |
| Two or more diseases | 58(47.5) | (38.4–56.8) | 2(6.7) | (0.8–22.1) | |
| Treatments performed for pain | 0.10 | ||||
| No drug | 5(4.1) | (1.3–9.3) | 4(13.3) | (3.8–30.7) | |
| One drug | 27(22.1) | (15.1–30.5) | 4(13.3) | (3.8–30.7) | |
| Two or more drugs | 90(73.8) | (65–81.3) | 22(73.3) | (54.1–87.7) | |
| Frequency of physical activity | 0.90 | ||||
| Less than 4 h/week | 53(43.4) | (34.5–52.7) | 13(43.3) | (25.5–62.6) | |
| Between 4 and 10 h/week | 49(40.2) | (31.4–49.4) | 13(43.3) | (25.5–62.6) | |
| More than 10 h/week | 20(16.4) | (10.3–24.2) | 4(13.3) | (3.8–30.7) | |
| Use of walking aid | 0.15 | ||||
| Yes | 15(12.3) | (7–19.5) | 1(3.3) | (0.1–17.2) | |
| No | 107(87.7) | (80.5–93) | 29(96.7) | (82.8–99.9) | |
| Pain localisation | |||||
| Localised pain | 44(36.1) | (27.6–45.3) | |||
| Referred/irradiated pain | 45(36.9) | (28.3–46.1) | |||
| Generalised pain | 33(27) | (19.4–35.8) |
| Scales | Mean ± SD | Median (Q1–Q3) |
|---|---|---|
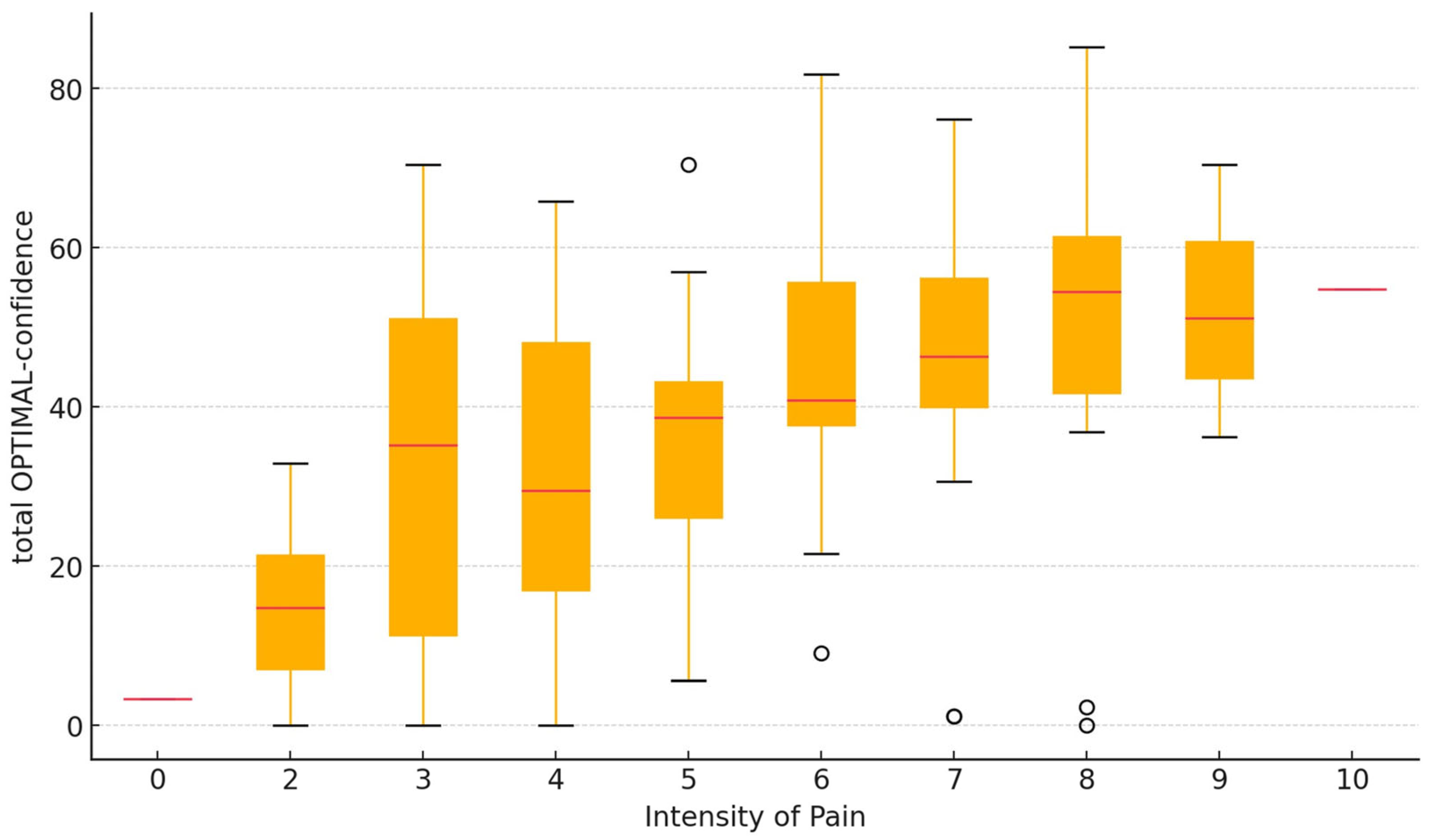
| Intensity of pain (0–10 scale) | 5.61 ± 1.95 | 6 (4–7) |
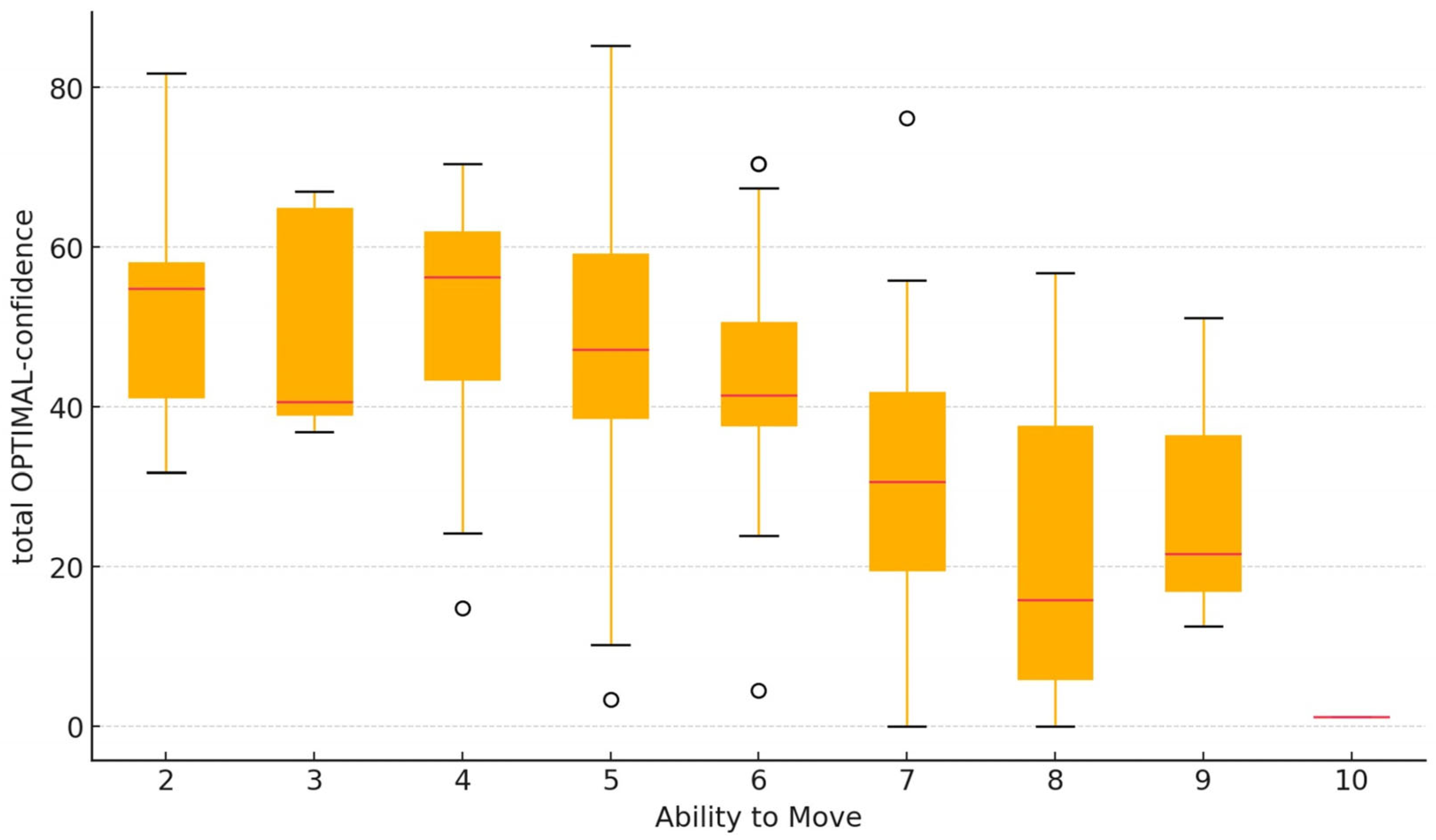
| Ability to move (0–10 scale) | 5.77 ± 1.78 | 6 (5–7) |
| Total OPTIMAL-confidence § | 39.56 ± 20.70 | 40.90 (24.09–55.04) |
| Trunk subscale | 32.61 ± 23.11 | 32.14 (13.39–50) |
| Lower extremity subscale | 44.00 ± 23.51 | 46.68 (30.23–63.88) |
| Upper extremity subscale | 41.15 ± 24.10 | 41.66 (25–61.53) |
| Total Self-efficacy † | 65.70 ± 17.38 | 68.42 (54.47–79.60) |
| Symptom Management | 67.61 ± 16.86 | 68.75 (58.75–81.25) |
| Physical Functioning | 74.78 ± 21.52 | 79.16 (63.33–91.66) |
| Pain Management | 51.77 ± 21.99 | 56 (35.50–68) |
| Analysis Group | OPTIMAL-Confidence Median (Q1–Q3) | p-Value |
|---|---|---|
| Age (N = 122) | ||
| ≤50 years (n = 37) | 26.14(3.98–48.29) | 0.009 ** |
| 51–61 years (n = 24) | 40.91 (23.86–55.64) | |
| 62–67 years (n = 31) | 42.05(31.82–56.82) | |
| ≥68 years (n = 30) | 44.70(38.35–55.96) | |
| Use of walking aid (N = 122) | ||
| Yes (n = 15) | 55.68(39.77–64.77) | 0.009 * |
| No (n = 107) | 39.77(22.73–53.41) | |
| Pain localisation (N = 122) | ||
| Localised pain (n = 44) | 36.60(19.88–51.41) | 0.147 ** |
| Referred/irradiated pain (n = 45) | 42.05(30.68–58.52) | |
| Generalised pain (n = 33) | 43.95(27.84–56.90) | |
| Low back pain | ||
| Yes (n = 122) | 40.91(24.09–55.01) | 0.001 * |
| No (n = 30) | 10.23(0.85–23.01) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nieto-Marcos, S.; Álvarez-Álvarez, M.J.; Ramón-Insunza, I.A.; García-Solís, L.; Calvo-Arias, M.M.; Pinto-Carral, A. Validation of the OPTIMAL-Confidence Questionnaire in Patients with Chronic Low Back Pain. J. Clin. Med. 2025, 14, 221. https://doi.org/10.3390/jcm14010221
Nieto-Marcos S, Álvarez-Álvarez MJ, Ramón-Insunza IA, García-Solís L, Calvo-Arias MM, Pinto-Carral A. Validation of the OPTIMAL-Confidence Questionnaire in Patients with Chronic Low Back Pain. Journal of Clinical Medicine. 2025; 14(1):221. https://doi.org/10.3390/jcm14010221
Chicago/Turabian StyleNieto-Marcos, Sonia, María José Álvarez-Álvarez, Iván Antonio Ramón-Insunza, Leonor García-Solís, María Mar Calvo-Arias, and Arrate Pinto-Carral. 2025. "Validation of the OPTIMAL-Confidence Questionnaire in Patients with Chronic Low Back Pain" Journal of Clinical Medicine 14, no. 1: 221. https://doi.org/10.3390/jcm14010221
APA StyleNieto-Marcos, S., Álvarez-Álvarez, M. J., Ramón-Insunza, I. A., García-Solís, L., Calvo-Arias, M. M., & Pinto-Carral, A. (2025). Validation of the OPTIMAL-Confidence Questionnaire in Patients with Chronic Low Back Pain. Journal of Clinical Medicine, 14(1), 221. https://doi.org/10.3390/jcm14010221






