Sex Disparity in the Association of Metabolic Syndrome with Cognitive Impairment
Abstract
1. Introduction
2. Materials and Methods
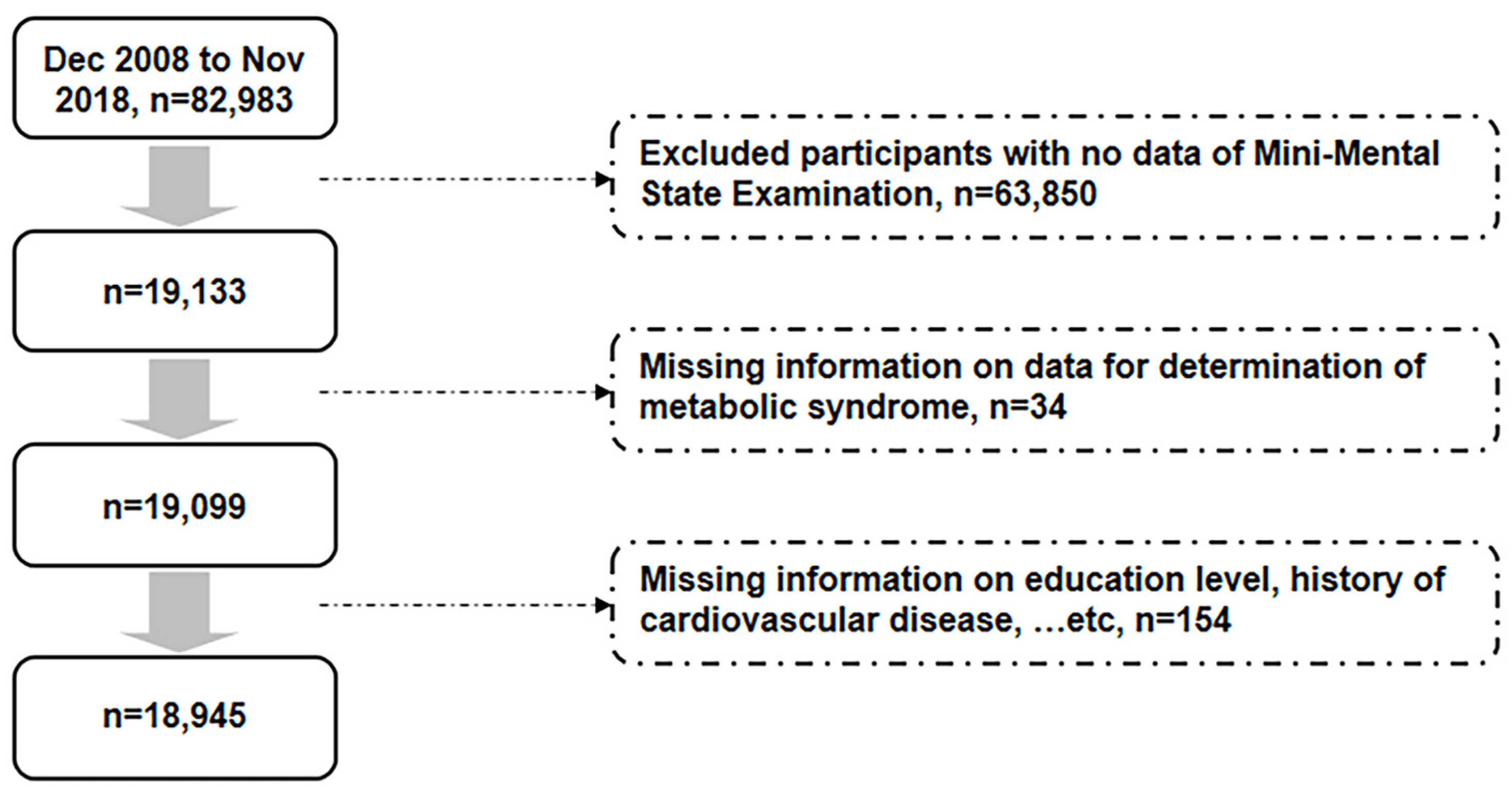
2.1. Study Participants
2.2. Cognitive Assessment and the Definition of Dementia
2.3. Definition of Metabolic Syndrome
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alzheimer’s Disease International. Available online: https://www.alzint.org/u/WorldAlzheimerReport2015.pdf (accessed on 29 July 2022).
- GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Dementia: Number of People Affected to Triple in Next 30 Years. Available online: https://www.who.int/news/item/07-12-2017-dementia-number-of-people-affected-to-triple-in-next-30-years (accessed on 14 June 2022).
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Ancelin, M.L.; Ripoche, E.; Dupuy, A.M.; Barberger-Gateau, P.; Auriacombe, S.; Rouaud, O.; Berr, C.; Carrière, I.; Ritchie, K. Sex differences in the associations between lipid levels and incident dementia. J. Alzheimer’s Dis. 2013, 34, 519–528. [Google Scholar] [CrossRef]
- Power, M.C.; Rawlings, A.; Sharrett, A.R.; Bandeen-Roche, K.; Coresh, J.; Ballantyne, C.M.; Pokharel, Y.; Michos, E.D.; Penman, A.; Alonso, A.; et al. Association of midlife lipids with 20-year cognitive change: A cohort study. Alzheimer’s Dement. 2018, 14, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Witt, B.J.; Howard, D.E.; Erwin, P.J.; Gami, L.A.; Somers, V.K.; Montori, V.M. Metabolic syndrome and risk of incident cardiovascular events and death: A systematic review and meta-analysis of longitudinal studies. J. Am. Coll. Cardiol. 2007, 49, 403–414. [Google Scholar] [CrossRef]
- Komulainen, P.; Lakka, T.A.; Kivipelto, M.; Hassinen, M.; Helkala, E.L.; Haapala, I.; Nissinen, A.; Rauramaa, R. Metabolic syndrome and cognitive function: A population-based follow-up study in elderly women. Dement. Geriatr. Cogn. Disord. 2007, 23, 29–34. [Google Scholar] [CrossRef]
- Reynolds, C.A.; Gatz, M.; Prince, J.A.; Berg, S.; Pedersen, N.L. Serum lipid levels and cognitive change in late life. J. Am. Geriatr. Soc. 2010, 58, 501–509. [Google Scholar] [CrossRef]
- Yaffe, K.; Kanaya, A.; Lindquist, K.; Simonsick, E.M.; Harris, T.; Shorr, R.I.; Tylavsky, F.A.; Newman, A.B. The metabolic syndrome, inflammation, and risk of cognitive decline. JAMA 2004, 292, 2237–2242. [Google Scholar] [CrossRef] [PubMed]
- Yaffe, K.; Haan, M.; Blackwell, T.; Cherkasova, E.; Whitmer, R.A.; West, N. Metabolic syndrome and cognitive decline in elderly Latinos: Findings from the Sacramento Area Latino Study of Aging study. J. Am. Geriatr. Soc. 2007, 55, 758–762. [Google Scholar] [CrossRef]
- Kalmijn, S.; Foley, D.; White, L.; Burchfiel, C.M.; Curb, J.D.; Petrovitch, H.; Ross, G.W.; Havlik, R.J.; Launer, L.J. Metabolic cardiovascular syndrome and risk of dementia in Japanese-American elderly men. The Honolulu-Asia aging study. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 2255–2260. [Google Scholar] [CrossRef]
- Yaffe, K.; Weston, A.L.; Blackwell, T.; Krueger, K.A. The metabolic syndrome and development of cognitive impairment among older women. Arch. Neurol. 2009, 66, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Pal, K.; Mukadam, N.; Petersen, I.; Cooper, C. Mild cognitive impairment and progression to dementia in people with diabetes, prediabetes and metabolic syndrome: A systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zang, B.; Shao, J.; Ning, N.; He, L.; Ma, Y. Predictor of cognitive impairment: Metabolic syndrome or circadian syndrome. BMC Geriatr. 2023, 23, 408. [Google Scholar] [CrossRef] [PubMed]
- Alsuwaidi, H.N.; Ahmed, A.I.; Alkorbi, H.A.; Ali, S.M.; Altarawneh, L.N.; Uddin, S.I.; Roueentan, S.R.; Alhitmi, A.A.; Djouhri, L.; Chivese, T. Association Between Metabolic Syndrome and Decline in Cognitive Function: A Cross-Sectional Study. Diabetes Metab. Syndr. Obes. 2023, 16, 849–859. [Google Scholar] [CrossRef] [PubMed]
- Rochlani, Y.; Pothineni, N.V.; Mehta, J.L. Metabolic Syndrome: Does it Differ Between Women and Men? Cardiovasc. Drugs Ther. 2015, 29, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Kaylor, M.B.; Johannsson, M.; Bay, C.; Churilla, J.R. Prevalence of metabolic syndrome and individual criterion in US adolescents: 2001–2010 National Health and Nutrition Examination Survey. Metab. Syndr. Relat. Disord. 2014, 12, 527–532. [Google Scholar] [CrossRef]
- Song, Q.B.; Zhao, Y.; Liu, Y.Q.; Zhang, J.; Xin, S.J.; Dong, G.H. Sex difference in the prevalence of metabolic syndrome and cardiovascular-related risk factors in urban adults from 33 communities of China: The CHPSNE study. Diabetes Vasc. Dis. Res. 2015, 12, 189–198. [Google Scholar] [CrossRef]
- Wang, W.S.; Wahlqvist, M.L.; Hsu, C.C.; Chang, H.Y.; Chang, W.C.; Chen, C.C. Age- and gender-specific population attributable risks of metabolic disorders on all-cause and cardiovascular mortality in Taiwan. BMC Public Health 2012, 12, 111. [Google Scholar] [CrossRef] [PubMed]
- Beam, C.R.; Kaneshiro, C.; Jang, J.Y.; Reynolds, C.A.; Pedersen, N.L.; Gatz, M. Differences Between Women and Men in Incidence Rates of Dementia and Alzheimer’s Disease. J. Alzheimer’s Dis. 2018, 64, 1077–1083. [Google Scholar] [CrossRef]
- Fratiglioni, L.; Viitanen, M.; von Strauss, E.; Tontodonati, V.; Herlitz, A.; Winblad, B. Very old women at highest risk of dementia and Alzheimer’s disease: Incidence data from the Kungsholmen Project, Stockholm. Neurology 1997, 48, 132–138. [Google Scholar] [CrossRef]
- Andersen, K.; Launer, L.J.; Dewey, M.E.; Letenneur, L.; Ott, A.; Copeland, J.R.; Dartigues, J.F.; Kragh-Sorensen, P.; Baldereschi, M.; Brayne, C.; et al. Gender differences in the incidence of AD and vascular dementia: The EURODEM Studies. Neurology 1999, 53, 1992–1997. [Google Scholar] [CrossRef] [PubMed]
- Lidfeldt, J.; Nyberg, P.; Nerbrand, C.; Samsioe, G.; Scherstén, B.; Agardh, C.D. Socio-demographic and psychosocial factors are associated with features of the metabolic syndrome. The Women’s Health in the Lund Area (WHILA) study. Diabetes Obes. Metab. 2003, 5, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Buring, J.E.; Cook, N.R.; Grodstein, F. The relation of education and income to cognitive function among professional women. Neuroepidemiology 2006, 26, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.C.; Chen, L.K.; Hsiao, W.W.; Fan, C.T.; Ko, M.L. Next Chapter of the Taiwan Biobank: Sustainability and Perspectives. Biopreservation Biobanking 2019, 17, 189–197. [Google Scholar] [CrossRef]
- Tsai, C.F.; Lee, W.J.; Wang, S.J.; Shia, B.C.; Nasreddine, Z.; Fuh, J.L. Psychometrics of the Montreal Cognitive Assessment (MoCA) and its subscales: Validation of the Taiwanese version of the MoCA and an item response theory analysis. Int. Psychogeriatr. 2012, 24, 651–658. [Google Scholar] [CrossRef]
- Tsai, J.C.; Chen, C.W.; Chu, H.; Yang, H.L.; Chung, M.H.; Liao, Y.M.; Chou, K.R. Comparing the Sensitivity, Specificity, and Predictive Values of the Montreal Cognitive Assessment and Mini-Mental State Examination When Screening People for Mild Cognitive Impairment and Dementia in Chinese Population. Arch. Psychiatr. Nurs. 2016, 30, 486–491. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Shigemori, K.; Ohgi, S.; Okuyama, E.; Shimura, T.; Schneider, E. The factorial structure of the Mini-Mental State Examination (MMSE) in Japanese dementia patients. BMC Geriatr. 2010, 10, 36. [Google Scholar] [CrossRef]
- Stone, N.J.; Bilek, S.; Rosenbaum, S. Recent National Cholesterol Education Program Adult Treatment Panel III update: Adjustments and options. Am. J. Cardiol. 2005, 96, 53E–59E. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J.; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef] [PubMed]
- Nagai, M.; Hoshide, S.; Kario, K. Hypertension and dementia. Am. J. Hypertens. 2010, 23, 116–124. [Google Scholar] [CrossRef]
- Ott, A.; Stolk, R.P.; van Harskamp, F.; Pols, H.A.; Hofman, A.; Breteler, M.M. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology 1999, 53, 1937–1942. [Google Scholar] [CrossRef] [PubMed]
- Dimache, A.M.; Șalaru, D.L.; Sascău, R.; Stătescu, C. The Role of High Triglycerides Level in Predicting Cognitive Impairment: A Review of Current Evidence. Nutrients 2021, 13, 2118. [Google Scholar] [CrossRef]
- Watson, L.S.; Wilken-Resman, B.; Williams, A.; DiLucia, S.; Sanchez, G.; McLeod, T.L.; Sims-Robinson, C. Hyperinsulinemia alters insulin receptor presentation and internalization in brain microvascular endothelial cells. Diabetes Vasc. Dis. Res. 2022, 19, 14791641221118626. [Google Scholar] [CrossRef]
- de la Monte, S.M. Contributions of brain insulin resistance and deficiency in amyloid-related neurodegeneration in Alzheimer’s disease. Drugs 2012, 72, 49–66. [Google Scholar] [CrossRef]
- Reitz, C. Dyslipidemia and dementia: Current epidemiology, genetic evidence, and mechanisms behind the associations. J. Alzheimer’s Dis. 2012, 30 (Suppl. 2), S127–S145. [Google Scholar] [CrossRef]
- Yaghi, S.; Elkind, M.S. Lipids and Cerebrovascular Disease: Research and Practice. Stroke 2015, 46, 3322–3328. [Google Scholar] [CrossRef] [PubMed]
- Iadecola, C.; Yaffe, K.; Biller, J.; Bratzke, L.C.; Faraci, F.M.; Gorelick, P.B.; Gulati, M.; Kamel, H.; Knopman, D.S.; Launer, L.J.; et al. Impact of Hypertension on Cognitive Function: A Scientific Statement From the American Heart Association. Hypertension 2016, 68, e67–e94. [Google Scholar] [CrossRef]
- McEvoy, L.K.; Laughlin, G.A.; Barrett-Connor, E.; Bergstrom, J.; Kritz-Silverstein, D.; Der-Martirosian, C.; von Mühlen, D. Metabolic syndrome and 16-year cognitive decline in community-dwelling older adults. Ann. Epidemiol. 2012, 22, 310–317. [Google Scholar] [CrossRef]
- Dearborn, J.L.; Knopman, D.; Sharrett, A.R.; Schneider, A.L.; Jack, C.R., Jr.; Coker, L.H.; Alonso, A.; Selvin, E.; Mosley, T.H.; Wagenknecht, L.E.; et al. The metabolic syndrome and cognitive decline in the Atherosclerosis Risk in Communities study (ARIC). Dement. Geriatr. Cogn. Disord. 2014, 38, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Raffaitin, C.; Féart, C.; Le Goff, M.; Amieva, H.; Helmer, C.; Akbaraly, T.N.; Tzourio, C.; Gin, H.; Barberger-Gateau, P. Metabolic syndrome and cognitive decline in French elders: The Three-City Study. Neurology 2011, 76, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Yaffe, K. Metabolic syndrome and cognitive decline. Curr. Alzheimer Res. 2007, 4, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Schuur, M.; Henneman, P.; van Swieten, J.C.; Zillikens, M.C.; de Koning, I.; Janssens, A.C.; Witteman, J.C.; Aulchenko, Y.S.; Frants, R.R.; Oostra, B.A.; et al. Insulin-resistance and metabolic syndrome are related to executive function in women in a large family-based study. Eur. J. Epidemiol. 2010, 25, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Galobardes, B.; Shaw, M.; Lawlor, D.A.; Lynch, J.W.; Davey Smith, G. Indicators of socioeconomic position (part 1). J. Epidemiol. Community Health 2006, 60, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Crum, R.M.; Anthony, J.C.; Bassett, S.S.; Folstein, M.F. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA 1993, 269, 2386–2391. [Google Scholar] [CrossRef] [PubMed]
- Peeters, G.; Kenny, R.A.; Lawlor, B. Late life education and cognitive function in older adults. Int. J. Geriatr. Psychiatry 2020, 35, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Marseglia, A.; Darin-Mattsson, A.; Skoog, J.; Rydén, L.; Hadarsson-Bodin, T.; Kern, S.; Rydberg Sterner, T.; Shang, Y.; Zettergren, A.; Westman, E.; et al. Metabolic Syndrome Is Associated with Poor Cognition: A Population-Based Study of 70-Year-Old Adults without Dementia. J. Gerontol. A Biol. Sci. Med. Sci. 2021, 76, 2275–2283. [Google Scholar] [CrossRef]
- Ng, T.P.; Feng, L.; Nyunt, M.S.; Feng, L.; Gao, Q.; Lim, M.L.; Collinson, S.L.; Chong, M.S.; Lim, W.S.; Lee, T.S.; et al. Metabolic Syndrome and the Risk of Mild Cognitive Impairment and Progression to Dementia: Follow-up of the Singapore Longitudinal Ageing Study Cohort. JAMA Neurol. 2016, 73, 456–463. [Google Scholar] [CrossRef]
- Koepsell, T.D.; Monsell, S.E. Reversion from mild cognitive impairment to normal or near-normal cognition: Risk factors and prognosis. Neurology 2012, 79, 1591–1598. [Google Scholar] [CrossRef]
- Chanti-Ketterl, M.; Stebbins, R.C.; Obhi, H.K.; Belsky, D.W.; Plassman, B.L.; Yang, Y.C. Sex Differences in the Association between Metabolic Dysregulation and Cognitive Aging: The Health and Retirement Study. J. Gerontol. A Biol. Sci. Med. Sci. 2022, 77, 1827–1835. [Google Scholar] [CrossRef] [PubMed]
- Merz, A.A.; Cheng, S. Sex differences in cardiovascular ageing. Heart 2016, 102, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Kwan, A.C.; Chen, M.T.; Ouyang, D.; Ebinger, J.E.; Bell, S.P.; Niiranen, T.J.; Bello, N.A.; Cheng, S. Sex Differences in Myocardial and Vascular Aging. Circ. Res. 2022, 130, 566–577. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.H.; Kim, H.S. Menopause-Associated Lipid Metabolic Disorders and Foods Beneficial for Postmenopausal Women. Nutrients 2020, 12, 202. [Google Scholar] [CrossRef] [PubMed]
- Berg, G.A.; Siseles, N.; González, A.I.; Ortiz, O.C.; Tempone, A.; Wikinski, R.W. Higher values of hepatic lipase activity in postmenopause: Relationship with atherogenic intermediate density and low density lipoproteins. Menopause 2001, 8, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Proudler, A.J.; Felton, C.V.; Stevenson, J.C. Ageing and the response of plasma insulin, glucose and C-peptide concentrations to intravenous glucose in postmenopausal women. Clin. Sci. 1992, 83, 489–494. [Google Scholar] [CrossRef] [PubMed]
- Gouni-Berthold, I.; Berthold, H.K.; Mantzoros, C.S.; Böhm, M.; Krone, W. Sex disparities in the treatment and control of cardiovascular risk factors in type 2 diabetes. Diabetes Care 2008, 31, 1389–1391. [Google Scholar] [CrossRef] [PubMed]
- Dove, A.; Shang, Y.; Xu, W.; Grande, G.; Laukka, E.J.; Fratiglioni, L.; Marseglia, A. The impact of diabetes on cognitive impairment and its progression to dementia. Alzheimer’s Dement. 2021, 17, 1769–1778. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, A.M.; Sharrett, A.R.; Schneider, A.L.; Coresh, J.; Albert, M.; Couper, D.; Griswold, M.; Gottesman, R.F.; Wagenknecht, L.E.; Windham, B.G.; et al. Diabetes in midlife and cognitive change over 20 years: A cohort study. Ann. Intern. Med. 2014, 161, 785–793. [Google Scholar] [CrossRef]
- Xia, W.; Zhang, B.; Yang, Y.; Wang, P.; Yang, Y.; Wang, S. Poorly controlled cholesterol is associated with cognitive impairment in T2DM: A resting-state fMRI study. Lipids Health Dis. 2015, 14, 47. [Google Scholar] [CrossRef]
- Obisesan, T.O. Hypertension and cognitive function. Clin. Geriatr. Med. 2009, 25, 259–288. [Google Scholar] [CrossRef] [PubMed]
| Variables | Males | Females | p |
|---|---|---|---|
| Number of participants | 7399 | 11546 | |
| Age, years | 64.2 (64.1, 64.2) | 63.7 (63.7, 63.8) | <0.001 |
| Body mass index, kg/m2 | 25.0 (24.9, 25.0) | 24.0 (23.9, 24.1) | <0.001 |
| Waist circumference, cm | 88.1 (87.9, 88.3) | 83.3 (83.1, 83.4) | <0.001 |
| Systolic blood pressure, mm Hg | 132.4 (132.0, 132.8) | 127.8 (127.5, 128.1) | <0.001 |
| Diastolic blood pressure, mm Hg | 78.1 (77.9, 78.3) | 72.6 (72.4, 72.7) | <0.001 |
| Smoking, n (%) | 1012 (13.7) | 120 (1.0) | <0.001 |
| Hypertension, n (%) | 3688 (49.8) | 4397 (38.1) | <0.001 |
| Diabetes mellitus, n (%) | 1612 (21.8) | 1859 (16.1) | <0.001 |
| Cardiovascular disease, n (%) | 596 (8.1) | 288 (2.5) | <0.001 |
| Education level, n (%) | <0.001 | ||
| ≤6 years | 735 (9.9) | 2441 (21.1) | |
| >6 years | 6664 (90.1) | 9105 (78.9) | |
| Fasting plasma glucose, mg/dL | 103.9 (103.3, 104.4) | 99.3 (98.9, 99.7) | <0.001 |
| HDL cholesterol, mg/dL | 48.4 (48.2, 48.7) | 57.9 (57.7, 58.2) | <0.001 |
| Triglycerides, mg/dL | 124.7 (122.8, 126.5) | 116.8 (115.4, 118.2) | <0.001 |
| MMSE | 27.5 (27.5, 27.6) | 27.2 (27.2, 27.3) | <0.001 |
| MMSE < 24, n (%) | 400 (5.4) | 1042 (9.0) | <0.001 |
| Metabolic syndrome, n (%) | 2245 (30.3) | 3514 (30.4) | 0.905 |
| Large waist circumference, n (%) | 3033 (41.0) | 7222 (62.5) | <0.001 |
| High blood pressure, n (%) | 4115 (55.6) | 5155 (44.6) | <0.001 |
| High fasting glucose, n (%) | 3000 (40.5) | 3417 (29.6) | <0.001 |
| Low HDL cholesterol, n (%) | 1645 (22.2) | 3343 (29.0) | <0.001 |
| High triglyceride, n (%) | 1870 (25.3) | 2495 (21.6) | <0.001 |
| Univariate Analysis | Multivariate Analysis a | ||||
|---|---|---|---|---|---|
| Independent Variable: Metabolic Syndrome | OR (95% CI) | p | OR (95% CI) | p | p for Interaction |
| Overall population | 1.30 (1.15, 1.46) | <0.001 | 1.27 (1.13, 1.43) | <0.001 | |
| Males | 1.05 (0.84, 1.30) | 0.685 | 1.02 (0.82, 1.27) | 0.867 | 0.005 |
| Females | 1.54 (1.34, 1.78) | <0.001 | 1.48 (1.29, 1.71) | <0.001 | |
| Education level ≤ 6 years | 1.21 (1.03, 1.42) | 0.018 | 1.21 (1.03, 1.41) | 0.020 | 0.331 |
| Education level > 6 years | 1.08 (0.89, 1.30) | 0.448 | 1.06 (0.87, 1.27) | 0.579 | |
| Male | Female | ||||
|---|---|---|---|---|---|
| Independent Variables | OR (95% CI) a | p | OR (95% CI) a | p | p for Interaction |
| Large waist circumference | 1.14 (0.92, 1.41) | 0.226 | 1.25 (1.08, 1.46) | 0.003 | 0.466 |
| High blood pressure | 1.01 (0.81, 1.25) | 0.940 | 1.09 (0.95, 1.25) | 0.235 | 0.562 |
| High fasting glucose | 0.89 (0.72, 1.11) | 0.307 | 1.16 (1.00, 1.34) | 0.046 | 0.054 |
| Low HDL cholesterol | 1.05 (0.82, 1.34) | 0.711 | 1.16 (1.00, 1.34) | 0.049 | 0.503 |
| High triglyceride | 0.90 (0.70, 1.16) | 0.415 | 1.10 (0.94, 1.29) | 0.251 | 0.187 |
| Males | Females | ||||
|---|---|---|---|---|---|
| Independent Variables | OR (95% CI) a | p | OR (95% CI) a | p | p for Interaction |
| Impaired orientation | |||||
| Metabolic syndrome | 0.96 (0.79, 1.16) | 0.661 | 1.21 (1.07, 1.37) | 0.003 | 0.039 |
| Large waist circumference | 1.02 (0.85, 1.21) | 0.868 | 1.19 (1.05, 1.36) | 0.007 | 0.124 |
| High blood pressure | 0.92 (0.78, 1.10) | 0.381 | 1.13 (1.00, 1.27) | 0.044 | 0.066 |
| High fasting glucose | 1.00 (0.84, 1.19) | 0.980 | 1.18 (1.04, 1.34) | 0.009 | 0.122 |
| Low HDL cholesterol | 1.02 (0.83, 1.25) | 0.880 | 1.14 (1.00, 1.29) | 0.050 | 0.362 |
| High triglyceride | 0.93 (0.76, 1.14) | 0.513 | 1.23 (1.08, 1.42) | 0.003 | 0.025 |
| Impaired memory | |||||
| Metabolic syndrome | 0.93 (0.82, 1.06) | 0.289 | 1.12 (1.01, 1.25) | 0.034 | 0.023 |
| Large waist circumference | 1.01 (0.90, 1.14) | 0.845 | 1.07 (0.96, 1.19) | 0.229 | 0.438 |
| High blood pressure | 1.06 (0.94, 1.19) | 0.320 | 1.00 (0.90, 1.10) | 0.943 | 0.467 |
| High fasting glucose | 0.88 (0.78, 0.99) | 0.033 | 1.09 (0.98, 1.22) | 0.113 | 0.006 |
| Low HDL cholesterol | 1.02 (0.89, 1.18) | 0.740 | 1.13 (1.01, 1.26) | 0.035 | 0.270 |
| High triglyceride | 0.93 (0.82, 1.07) | 0.317 | 1.07 (0.95, 1.21) | 0.285 | 0.138 |
| Impaired attention and calculation | |||||
| Metabolic syndrome | 0.96 (0.83, 1.12) | 0.597 | 1.09 (0.99, 1.21) | 0.084 | 0.173 |
| Large waist circumference | 1.04 (0.90, 1.19) | 0.599 | 1.04 (0.94, 1.15) | 0.464 | 0.983 |
| High blood pressure | 0.92 (0.80, 1.05) | 0.208 | 1.09 (0.99, 1.20) | 0.068 | 0.038 |
| High fasting glucose | 1.06 (0.93, 1.22) | 0.384 | 1.13 (1.02, 1.25) | 0.017 | 0.502 |
| Low HDL cholesterol | 1.10 (0.93, 1.29) | 0.257 | 1.04 (0.94, 1.15) | 0.487 | 0.536 |
| High triglyceride | 1.03 (0.88, 1.21) | 0.699 | 1.11 (0.99, 1.24) | 0.081 | 0.503 |
| Impaired language | |||||
| Metabolic syndrome | 1.08 (0.94, 1.25) | 0.275 | 1.09 (0.97, 1.21) | 0.142 | 0.767 |
| Large waist circumference | 1.29 (1.13, 1.48) | <0.001 | 1.14 (1.02, 1.27) | 0.022 | 0.246 |
| High blood pressure | 1.00 (0.87, 1.15) | 0.974 | 1.00 (0.90, 1.11) | 0.949 | 0.938 |
| High fasting glucose | 1.03 (0.90, 1.18) | 0.692 | 1.16 (1.04, 1.30) | 0.008 | 0.109 |
| Low HDL cholesterol | 1.33 (1.14, 1.56) | <0.001 | 1.14 (1.02, 1.27) | 0.023 | 0.142 |
| High triglyceride | 0.94 (0.80, 1.10) | 0.414 | 0.98 (0.86, 1.11) | 0.715 | 0.605 |
| Impaired design copying | |||||
| Metabolic syndrome | 1.13 (0.90, 1.42) | 0.283 | 1.41 (1.23, 1.62) | <0.001 | 0.093 |
| Large waist circumference | 1.05 (0.84, 1.30) | 0.679 | 1.31 (1.13, 1.52) | <0.001 | 0.075 |
| High blood pressure | 1.02 (0.82, 1.27) | 0.857 | 1.14 (1.00, 1.31) | 0.051 | 0.344 |
| High fasting glucose | 1.25 (1.01, 1.55) | 0.043 | 1.30 (1.13, 1.50) | <0.001 | 0.692 |
| Low HDL cholesterol | 1.09 (0.85, 1.39) | 0.516 | 1.18 (1.03, 1.37) | 0.021 | 0.515 |
| High triglyceride | 1.00 (0.78, 1.28) | 0.996 | 1.19 (1.01, 1.39) | 0.032 | 0.236 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-M.; Lee, C.-L.; Wang, J.-S. Sex Disparity in the Association of Metabolic Syndrome with Cognitive Impairment. J. Clin. Med. 2024, 13, 2571. https://doi.org/10.3390/jcm13092571
Chang Y-M, Lee C-L, Wang J-S. Sex Disparity in the Association of Metabolic Syndrome with Cognitive Impairment. Journal of Clinical Medicine. 2024; 13(9):2571. https://doi.org/10.3390/jcm13092571
Chicago/Turabian StyleChang, Yi-Min, Chia-Lin Lee, and Jun-Sing Wang. 2024. "Sex Disparity in the Association of Metabolic Syndrome with Cognitive Impairment" Journal of Clinical Medicine 13, no. 9: 2571. https://doi.org/10.3390/jcm13092571
APA StyleChang, Y.-M., Lee, C.-L., & Wang, J.-S. (2024). Sex Disparity in the Association of Metabolic Syndrome with Cognitive Impairment. Journal of Clinical Medicine, 13(9), 2571. https://doi.org/10.3390/jcm13092571






