Sagittal Full-Spine vs. Sectional Cervical Lateral Radiographs: Are the Measurements of Cervical Alignment Interchangeable?
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Data Collection
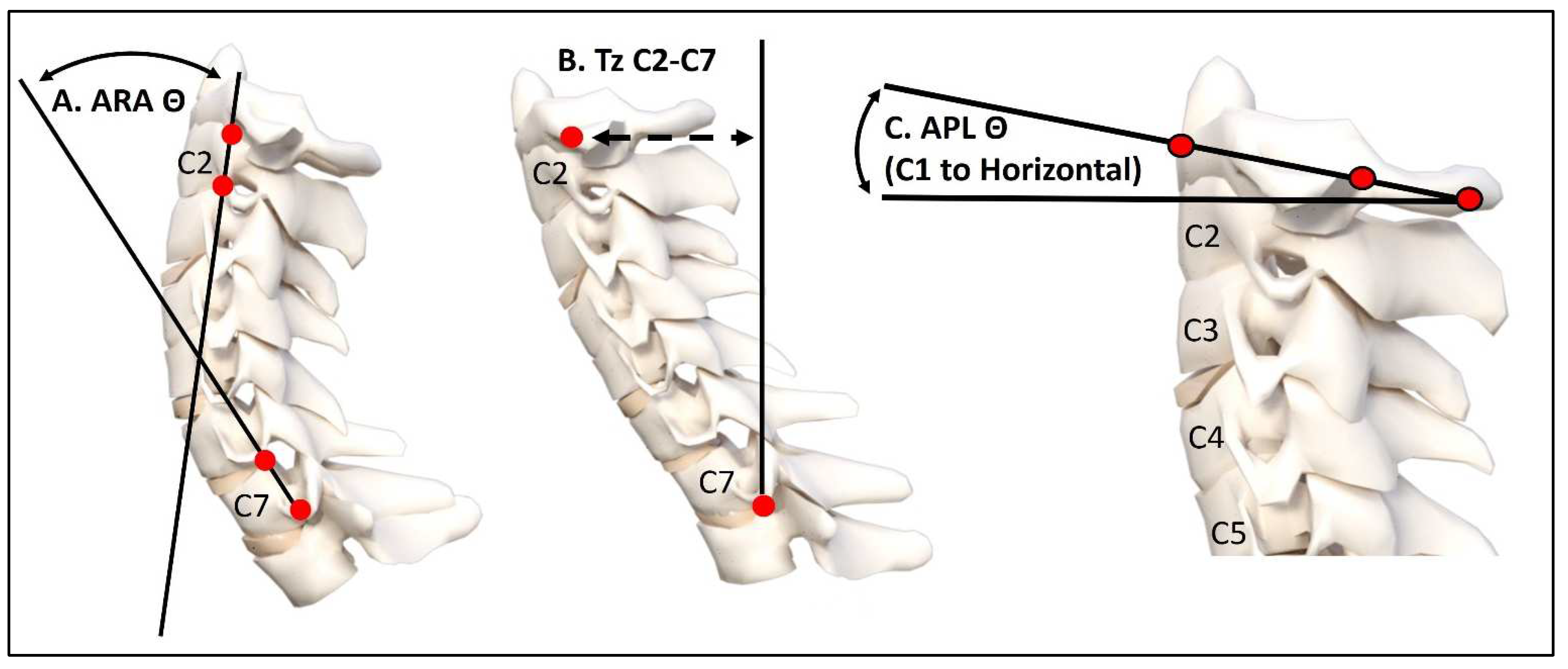
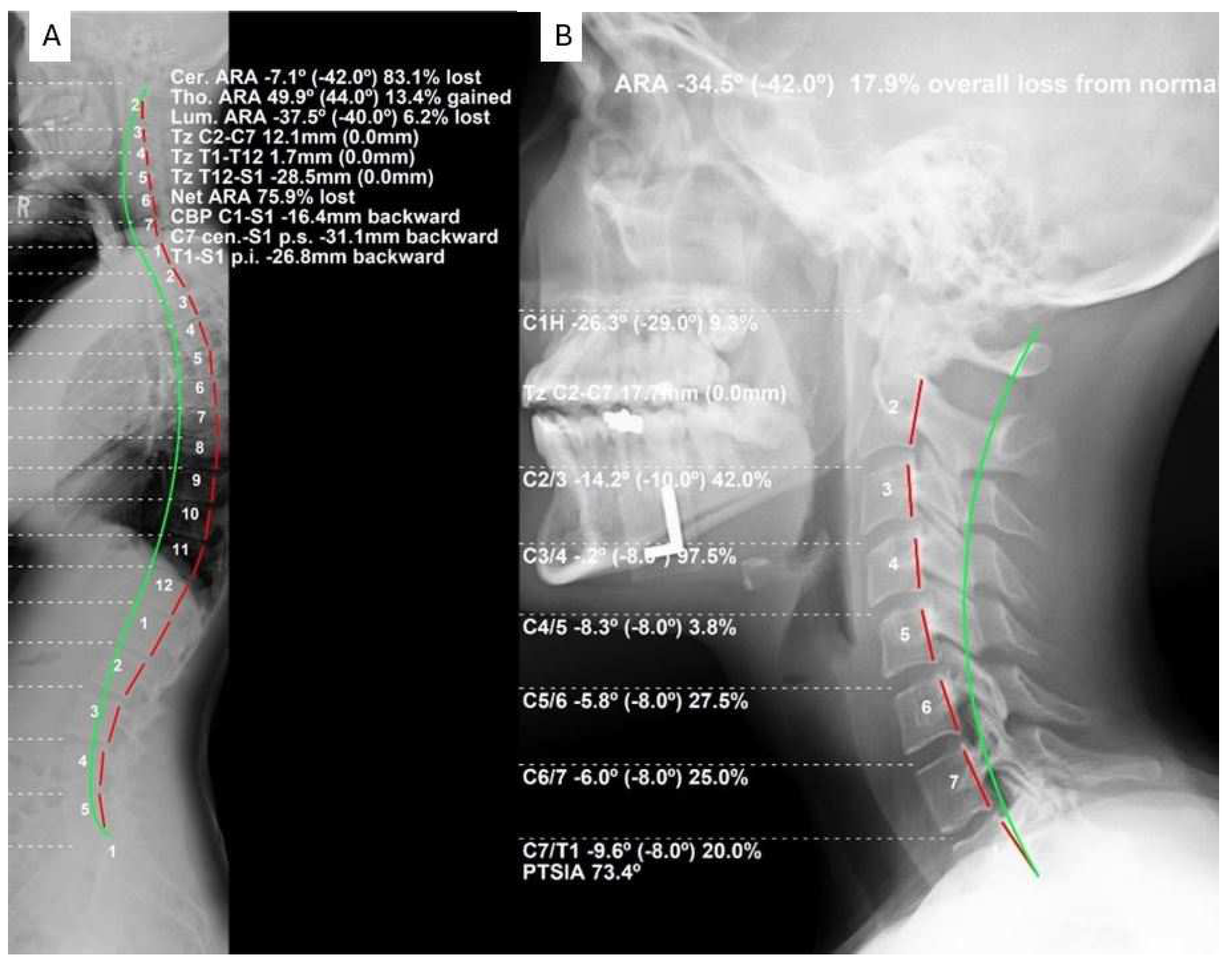
2.2. Radiographic Evaluation Procedure
2.3. Statistical Analytical Methods
3. Results
3.1. Patient Demographics
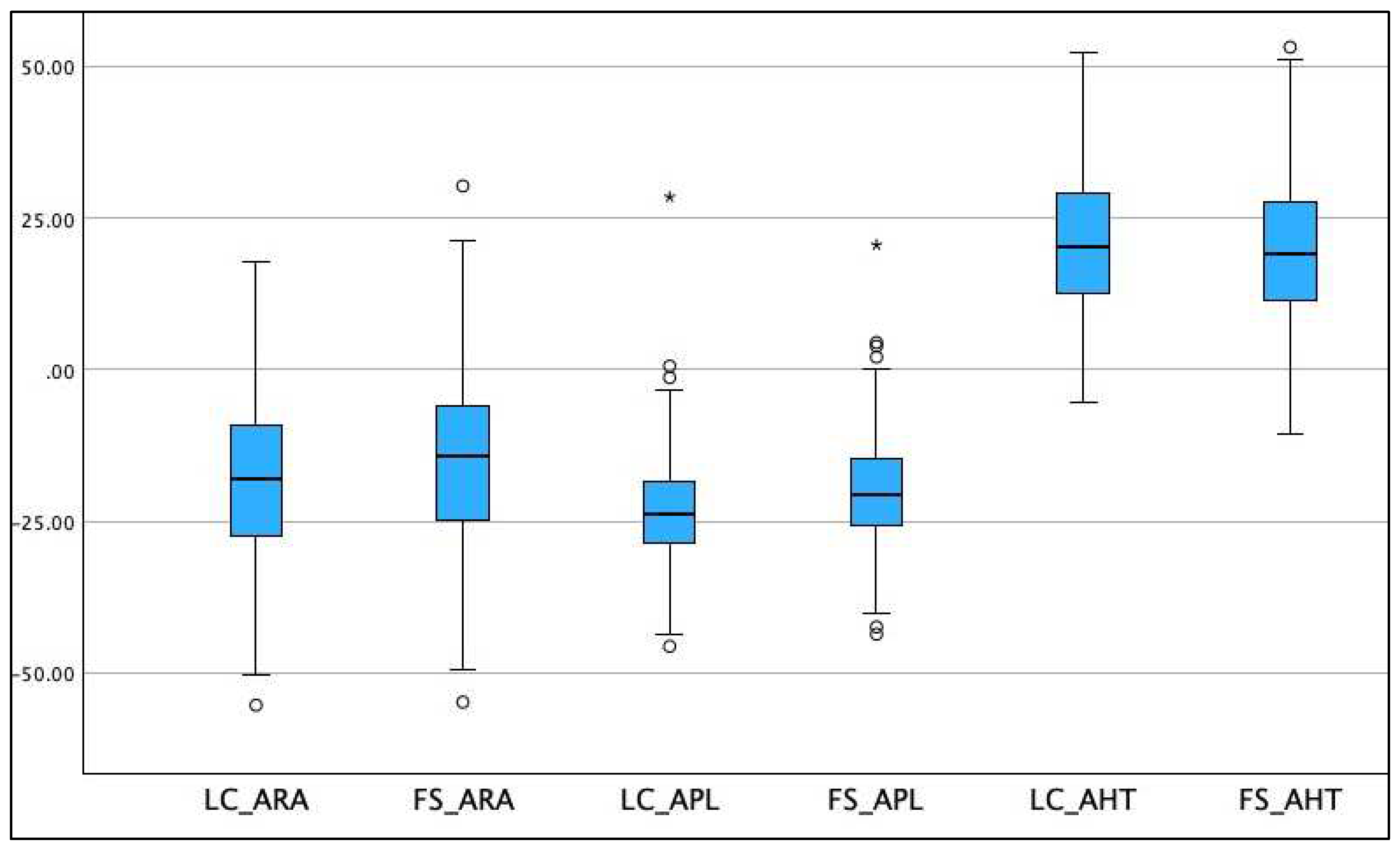
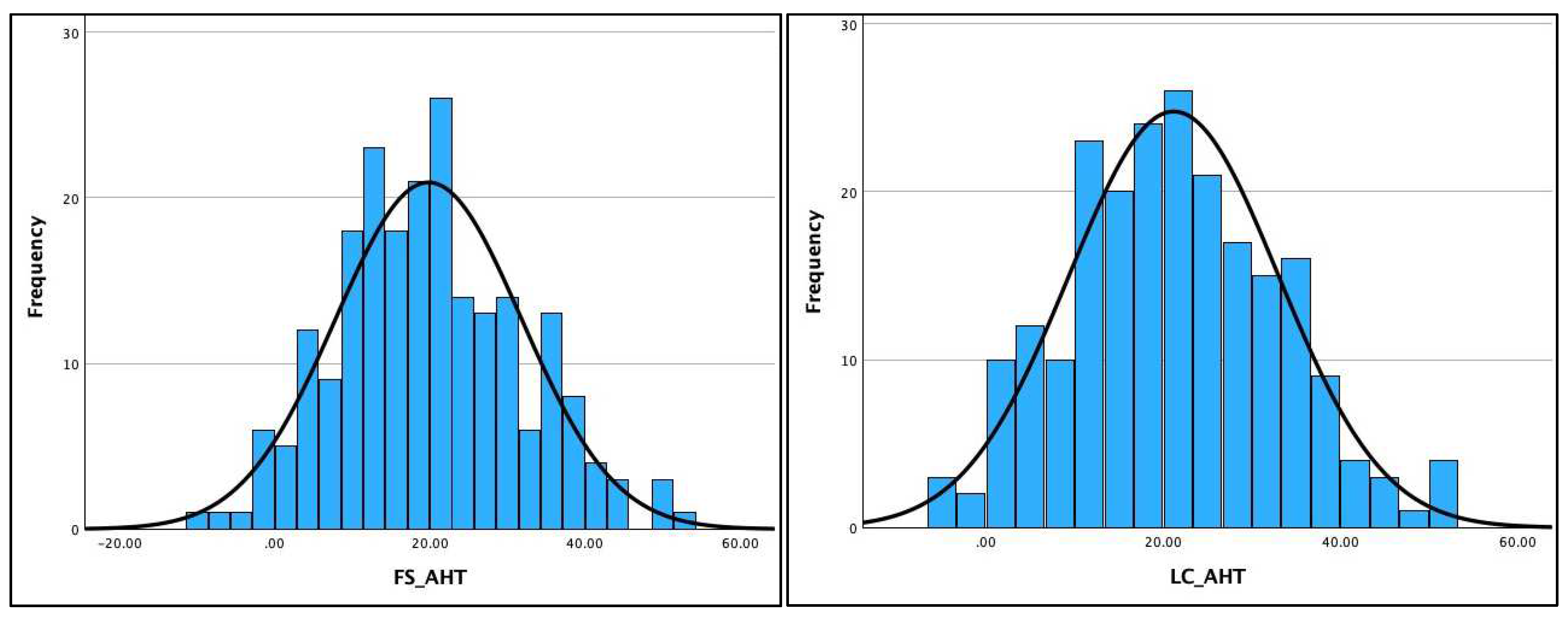
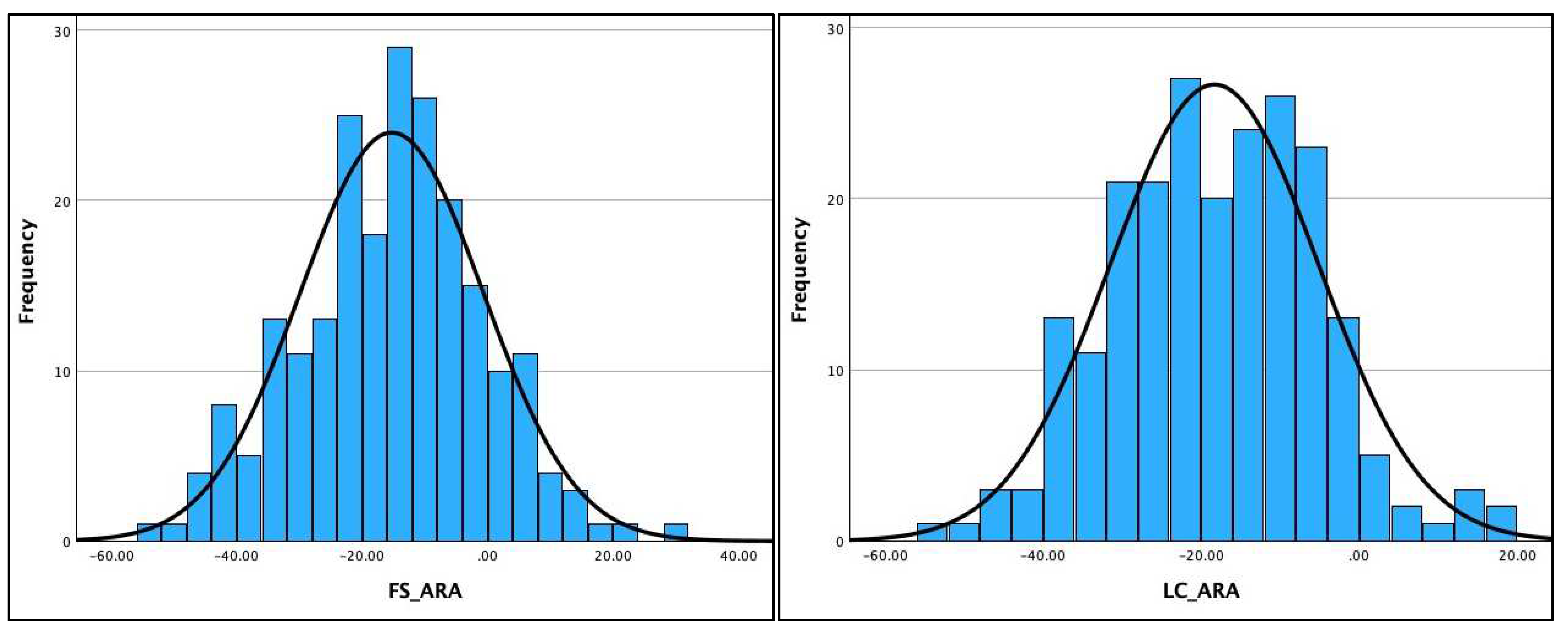
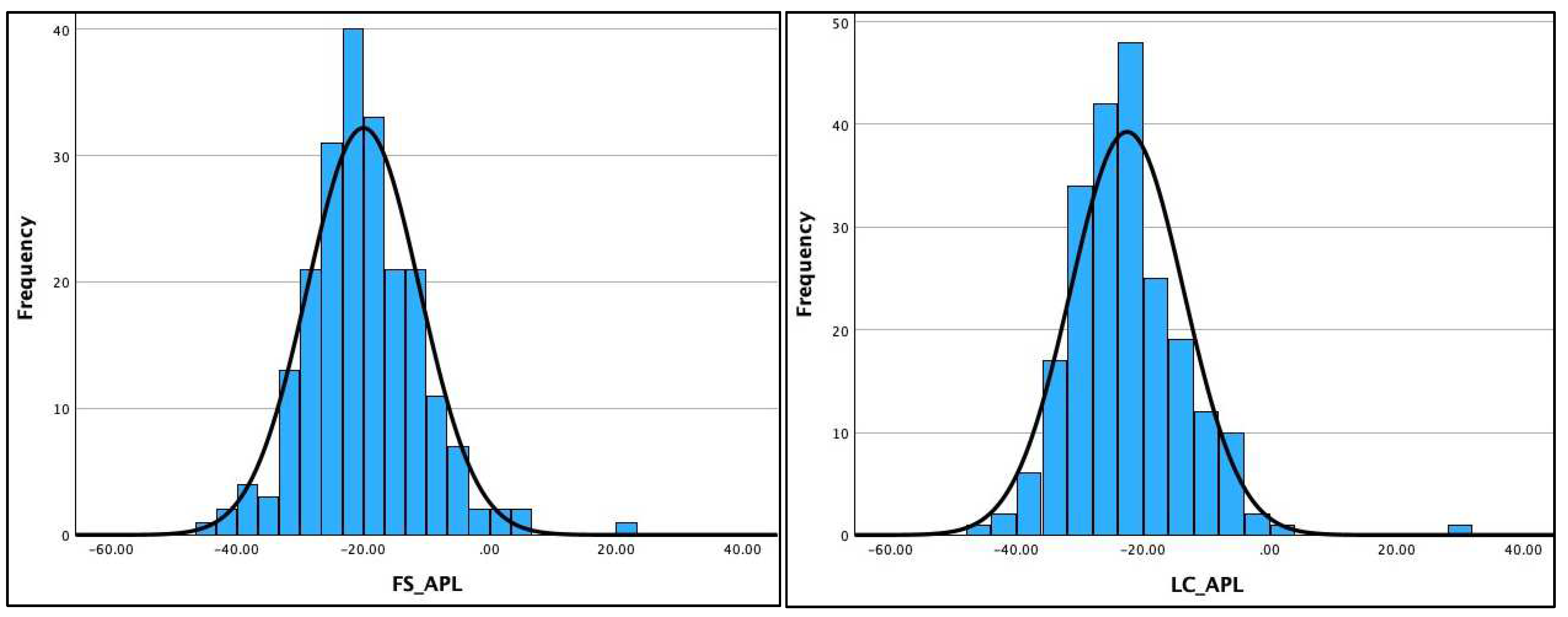
3.2. Normality of Distribution of the Radiographic Data
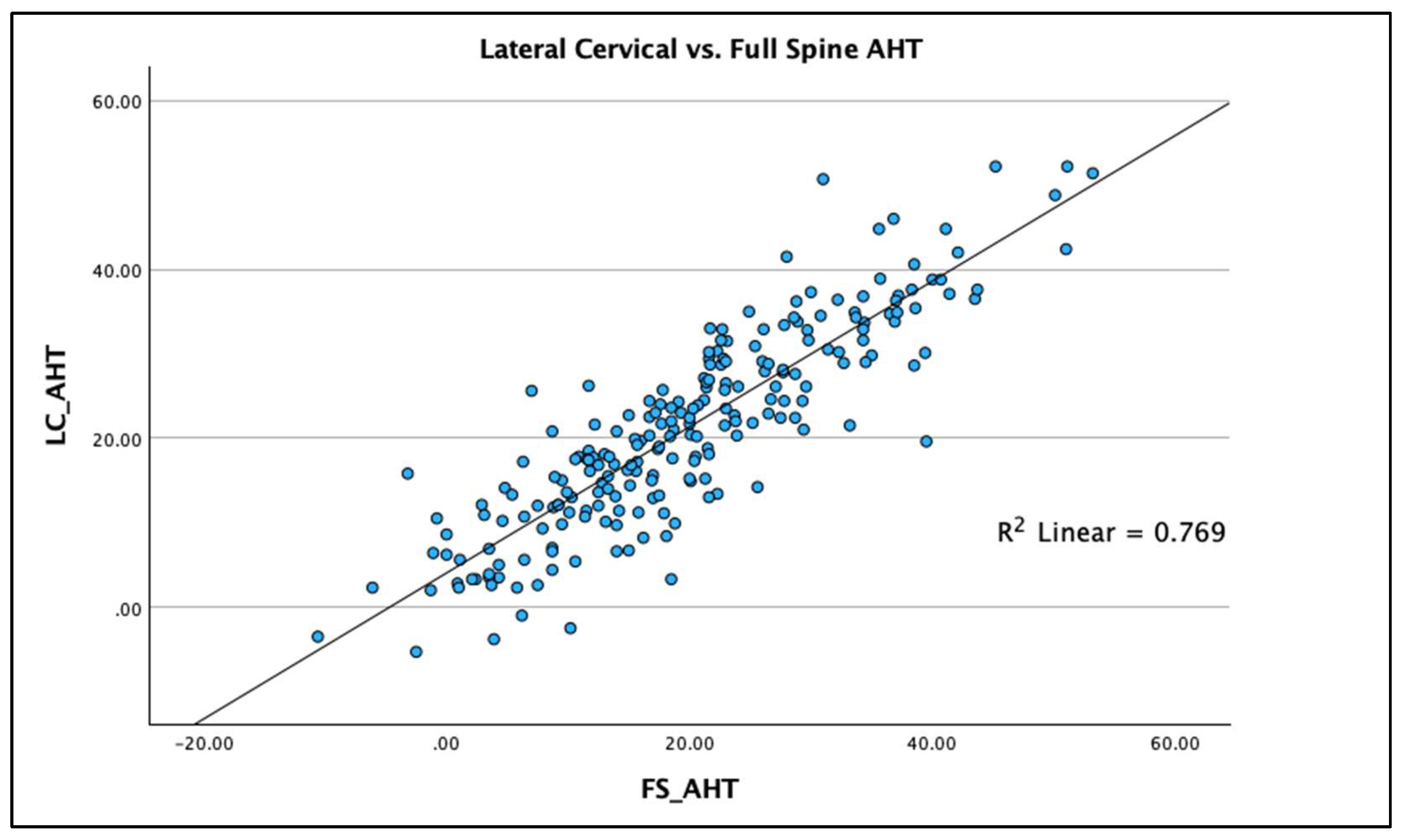
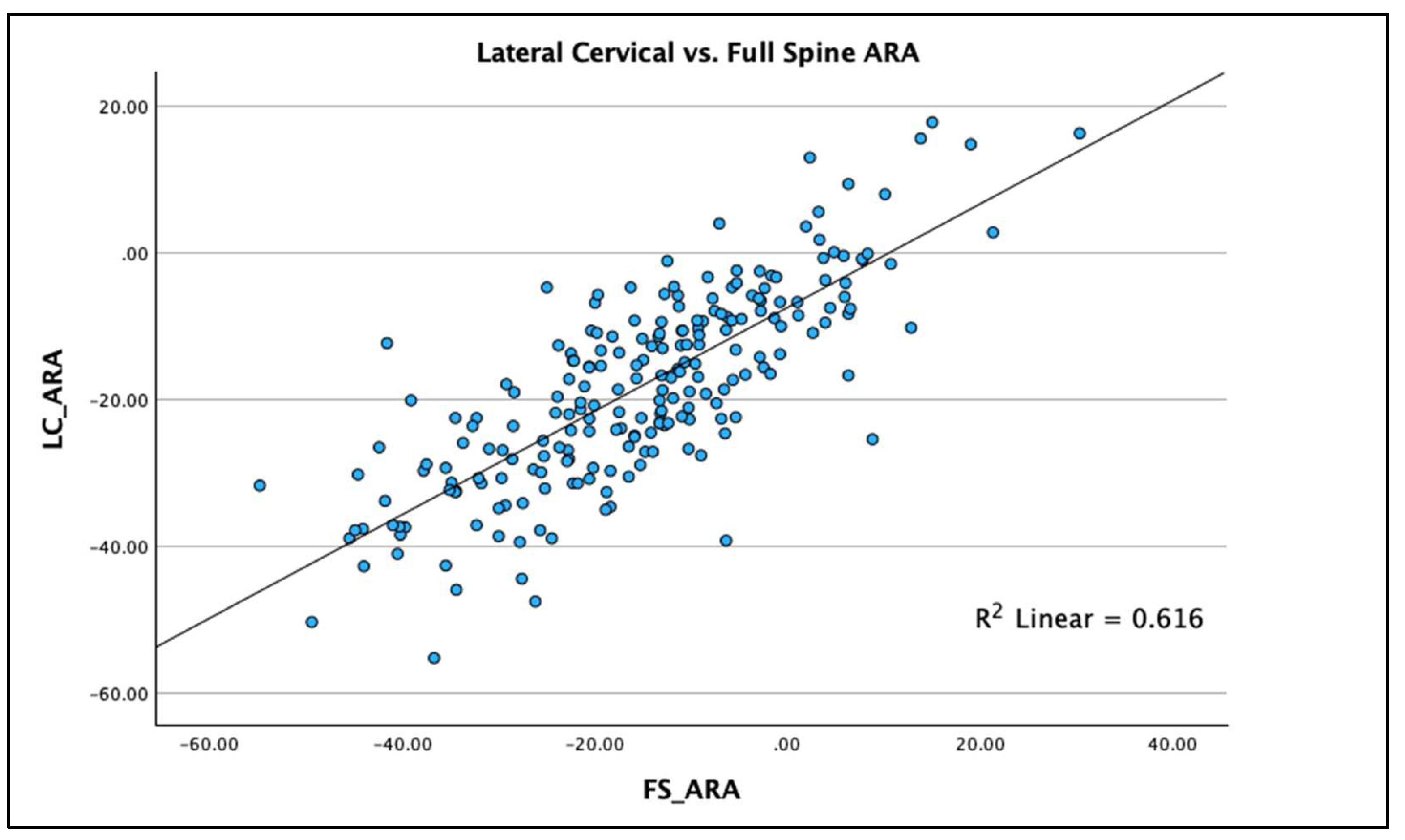
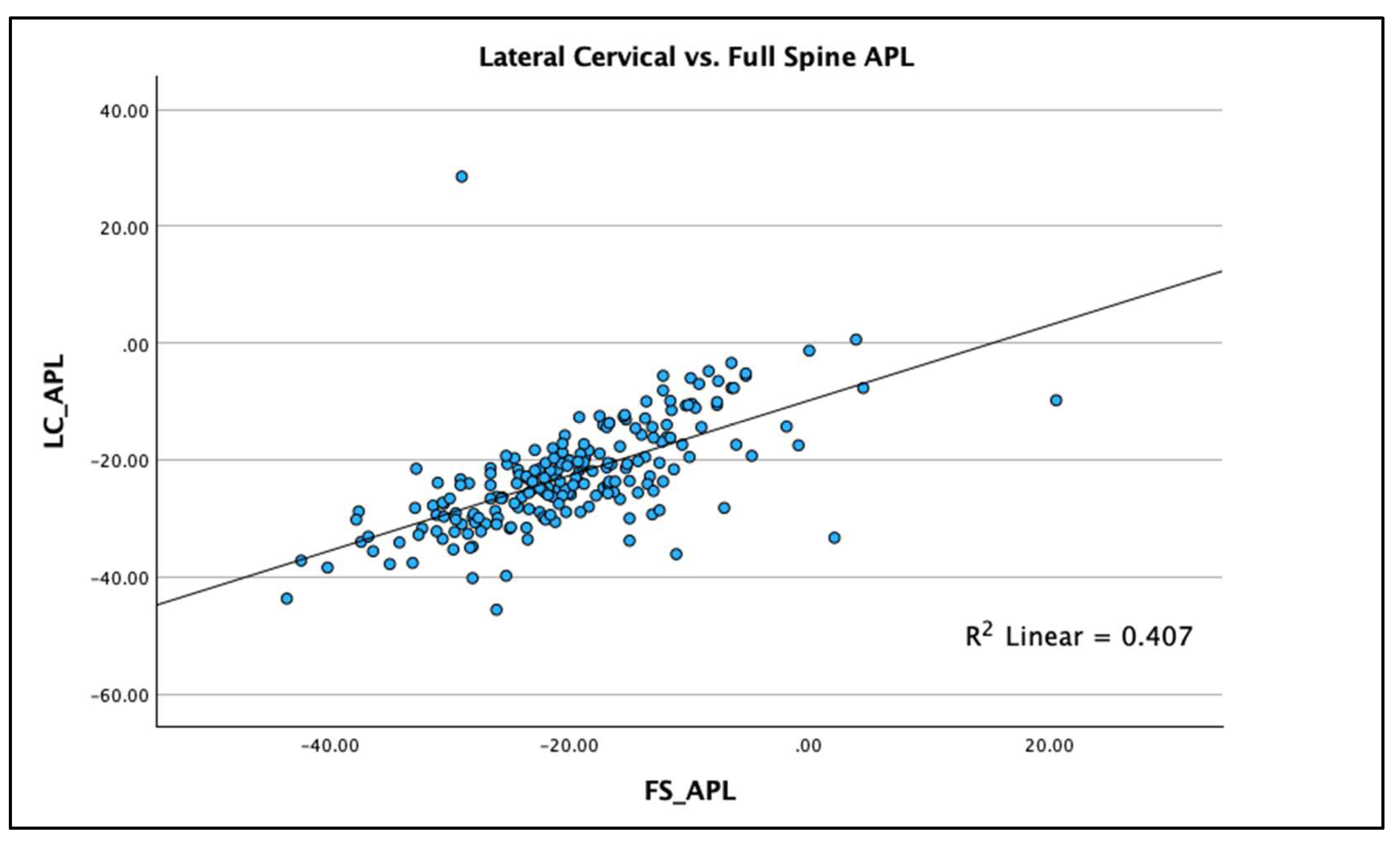
3.3. Regression Analysis with R2
4. Discussion and Clinical Interpretation
4.1. Previous Investigations with Comparison to Current
4.2. Significance of Current Investigation
4.3. Clinical Implications
4.4. Risk–Benefits of a LC and FS Radiograph
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harada, G.K.; Siyaji, Z.K.; Younis, S.; Louie, P.K.; Samartzis, D.; An, H.S. Imaging in Spine Surgery: Current Concepts and Future Directions. Spine Surg. Relat. Res. 2019, 4, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Smith, H.E.; Vaccaro, A.R.; Yuan, P.S.; Papadopoulos, S.; Sasso, R. The use of computerized image guidance in lumbar disk arthroplasty. J. Spinal Disord. Tech. 2006, 19, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Rothenfluh, D.A.; Mueller, D.A.; Rothenfluh, E.; Min, K. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur. Spine J. 2015, 24, 1251–1258. [Google Scholar] [CrossRef] [PubMed]
- Teo, A.Q.A.; Thomas, A.C.; Hey, H.W.D. Sagittal alignment of the cervical spine: Do we know enough for successful surgery? J. Spine Surg. 2020, 6, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, C., 4th; Levin, L.S.; Ondra, S.L.; Shaffrey, C.I.; Morgan, C.J. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: A review and resynthesis of the literature. J. Neurosurg. Spine 2007, 6, 104–112. [Google Scholar] [CrossRef]
- Oakley, P.A.; Ehsani, N.N.; Moustafa, I.M.; Harrison, D.E. Restoring cervical lordosis by cervical extension traction methods in the treatment of cervical spine disorders: A systematic review of controlled trials. J. Phys. Ther. Sci. 2021, 33, 784–794. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Oakley, P.A. An introduction to Chiropractic BioPhysics® (CBP®) technique: A full spine rehabilitation approach to reducing spine deformities. In Complementary Therapies; Bernardo-Filho, M., Ed.; IntechOpen: London, UK, 2022; pp. 1–35. [Google Scholar]
- Shin, D.W.; Shin, J.I.; Koyanagi, A.; Jacob, L.; Smith, L.; Lee, H.; Chang, Y.; Song, T.J. Global, regional, and national neck pain burden in the general population, 1990–2019: An analysis of the global burden of disease study 2019. Front. Neurol. 2022, 13, 955367. [Google Scholar] [CrossRef] [PubMed]
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.M.; Kolahi, A.A.; Safiri, S. Neck pain: Global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.T.; Aris, I.M.; Snyder, B.D.; Harris, M.B.; Kang, J.D.; Murray, M.; Rodriguez, E.K.; Nazarian, A. Musculoskeletal health: An ecological study assessing disease burden and research funding. Lancet Reg. Health Am. 2024, 29, 100661. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Park, S.; Kim, D.G.; Hwang, C.J.; Lee, C.S.; Hwang, E.S.; Cho, J.H. Cervical spine lateral radiograph versus whole spine lateral radiograph: A retrospective comparative study to identify a better modality to assess cervical sagittal alignment. Medicine 2021, 100, e25987. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Moon, S.H.; Kim, T.H.; Oh, J.K.; Kang, H.J.; Riew, K.D. Radiographic Comparison between Cervical Spine Lateral and Whole-Spine Lateral Standing Radiographs. Glob. Spine J. 2016, 6, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Ogura, Y.; Dimar, J.R.; Djurasovic, M.; Carreon, L.Y. Etiology and treatment of cervical kyphosis: State of the art review-a narrative review. J. Spine Surg. 2021, 7, 422–433. [Google Scholar] [CrossRef]
- Nugent, S.M.; Lovejoy, T.I.; Shull, S.; Dobscha, S.K.; Morasco, B.J. Associations of Pain Numeric Rating Scale Scores Collected during Usual Care with Research Administered Patient Reported Pain Outcomes. Pain Med. 2021, 22, 2235–2241. [Google Scholar] [CrossRef] [PubMed]
- Sy, E.; Samboju, V.; Mukhdomi, T. X-ray Image Production Procedures. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022; [Updated 17 October 2022]. Available online: https://ncbi.nlm.nih.gov/books/NBK564352/ (accessed on 2 January 2024).
- Harrison, D.E.; Harrison, D.D.; Cailliet, R.; Troyanovich, S.J.; Janik, T.J.; Holland, B. Cobb method or Harrison posterior tangent method: Which to choose for lateral cervical radiographic analysis. Spine 2000, 25, 2072–2078. [Google Scholar] [CrossRef] [PubMed]
- Pivotto, L.R.; Navarro, I.J.R.L.; Candotti, C.T. Radiography and photogrammetry-based methods of assessing cervical spine posture in the sagittal plane: A systematic review with meta-analysis. Gait Posture 2021, 84, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Maher, J.M.; Markey, J.C.; Ebert-May, D. The other half of the story: Effect size analysis in quantitative research. CBE Life Sci. Educ. 2013, 12, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-M.; Song, K.-S.; Park, S.-H.; Kang, H.; Riew, K.D. Does whole-spine lateral radiograph with clavicle positioning reflect the correct cervical sagittal alignment? Eur. Spine J. 2015, 24, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, Y.; Shigematsu, H.; Iwata, E.; Tanaka, M.; Okuda, A.; Masuda, K.; Yamamoto, Y.; Takeshima, T.; Nakagawa, Y.; Tanaka, Y. Evaluating Cervical Sagittal Alignment in Cervical Myelopathy: Are Sitting Cervical Radiographs and Standing Whole-Spine Radiographs Equally Useful? Glob. Spine J. 2019, 9, 591–597. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, H.J.; Kim, J.H.; Kim, I.S.; Hong, J.T. Physiologic Cervical Alignment Change Between Whole Spine Radiographs and Normal Standing Cervical Radiographs. World Neurosurg. 2019, 122, e1222–e1227. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Colloca, C.J.; Betz, J.; Janik, T.J.; Holland, B. Repeatability over time of posture, radiograph positioning, and radiograph line drawing: An analysis of six control groups. J. Manip. Physiol. Ther. 2003, 26, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.P.; Kanemura, T.; Kawakami, N.; Hales, C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine 2000, 25, 575–586. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.S.; Notz, W.I.; Flinger, M.A. The Basic Practice of Statistics, 6th ed.; W. H. Freeman and Company: New York, NY, USA, 2013; p. 138. [Google Scholar]
- Harrison, D.D.; Janik, T.J.; Troyanovich, S.J.; Holland, B. Comparisons of lordotic cervical spine curvatures to a theoretical ideal model of the static sagittal cervical spine. Spine 1996, 21, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Janik, T.J.; Holland, B.; Siskin, L.A. Slight head extension: Does it change the sagittal cervical curve? Eur. Spine J. 2001, 10, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Lan, Z.; Wu, Z.; Xu, W.; Huang, Y. Analysis of a radiographic parameter K-line tilt following adjacent two-level anterior cervical discectomy and fusion: A retrospective study. J. Orthop. Surg. Res. 2020, 15, 131. [Google Scholar] [CrossRef] [PubMed]
- Ruiz Santiago, F.; Láinez Ramos-Bossini, A.J.; Wáng, Y.X.J.; López Zúñiga, D. The role of radiography in the study of spinal disorders. Quant. Imaging Med. Surg. 2020, 10, 2322–2355. [Google Scholar] [CrossRef]
- Hornung, A.L.; Hornung, C.M.; Mallow, G.M.; Barajas, J.N.; Rush, A., 3rd; Sayari, A.J.; Galbusera, F.; Wilke, H.J.; Colman, M.; Phillips, F.M.; et al. Artificial intelligence in spine care: Current applications and future utility. Eur Spine J. 2022, 31, 2057–2081. [Google Scholar] [CrossRef] [PubMed]
- Čeko, M.; Lindquist, M.A.; Grotzinger, A.D.; Keller, M.C.; Friedman, N.P.; Wager, T.D. Genetic risk shared across 24 chronic pain conditions: Identification and characterization with genomic structural equation modeling. Pain 2023, 164, 2239–2252. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.; Das, J.M. Anatomy, Head and Neck: Cervical Spine. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023; [Updated 28 August 2023]. Available online: https://ncbi.nlm.nih.gov/books/NBK557516/ (accessed on 2 January 2024).
- Cheng, J.; Liu, P.; Sun, D.; Ma, Z.; Liu, J.; Wang, Z.; Mou, J. Correlation of cervical and thoracic inlet sagittal parameters by MRI and radiography in patients with cervical spondylosis. Medicine 2019, 98, e14393. [Google Scholar] [CrossRef] [PubMed]
- Torlincasi, A.M.; Waseem, M. Cervical Injury. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022; [Updated 22 August 2022]. Available online: https://ncbi.nlm.nih.gov/books/NBK448146/ (accessed on 2 January 2024).
- Goo, B.W.; Oh, J.H.; Kim, J.S.; Lee, M.Y. Effects of cervical stabilization with visual feedback on craniovertebral angle and proprioception for the subjects with forward head posture. Medicine 2024, 103, e36845. [Google Scholar] [CrossRef] [PubMed]
- Kang, X.; Qian, M.; Qin, T.; Liu, M.; Xu, H.; Xu, B. Increased Expression of Inflammatory Cytokines and Discogenic Neck Pain. Orthop. Surg. 2024, 16, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Fakhoury, J.; Dowling, T.J. Cervical Degenerative Disc Disease. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023; [Updated 14 August 2023]. Available online: https://ncbi.nlm.nih.gov/books/NBK560772/ (accessed on 2 January 2024).
- Alghamdi, M.S.; Alghamdi, A.F.; Almalawi, A.M.; Alsulami, R.A.; Hazazi, H.A.; Al Ghashmari, A.A.; Al Dawais, A.S.; Salawati, E. The Association Between Neck Pain and Psychological Distress Experienced by King Abdulaziz University Students: A Cross-Sectional Study. Cureus 2023, 15, e35685. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Oakley, P.A.; Moustafa, I.M. Don’t Throw the ‘Bio’ out of the Bio-Psycho-Social Model: Editorial for Spine Rehabilitation in 2022 and Beyond. J. Clin. Med. 2023, 12, 5602. [Google Scholar] [CrossRef] [PubMed]
- Mulloy, D.F.; Hughes, R.G. Wrong-site surgery: A preventable medical error. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Chapter 36; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008. [Google Scholar]
- Cobb, T.K. Wrong site surgery—Where are we and what is the next step? Hand 2012, 7, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Seiden, S.C.; Barach, P. Wrong-side/wrong-site, wrong-procedure, and wrong-patient adverse events: Are they preventable? Arch. Surg. 2006, 141, 931–939. [Google Scholar] [CrossRef] [PubMed]
- DeVine, J.; Chutkan, N.; Norvell, D.C.; Dettori, J.R. Avoiding wrong site surgery: A systematic review. Spine 2010, 35, S28–S36. [Google Scholar] [CrossRef] [PubMed]
- Hsiang, J. Wrong-level surgery: A unique problem in spine surgery. Surg. Neurol. Int. 2011, 2, 47. [Google Scholar] [CrossRef] [PubMed]
- Sebaaly, A.; Lahoud, M.J.; Rizkallah, M.; Kreichati, G.; Kharrat, K. Etiology, Evaluation, and Treatment of Failed Back Surgery Syndrome. Asian Spine J. 2018, 12, 574–585. [Google Scholar] [CrossRef] [PubMed]
- Miękisiak, G. Failed Back Surgery Syndrome: No Longer a Surgeon’s Defeat-A Narrative Review. Medicina 2023, 59, 1255. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.M.; Weinberg, B.D.; Hoch, M.J. CT Myelography: Clinical Indications and Imaging Findings. Radiographics 2020, 40, 470–484. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Zhao, W.-K.; Li, M.; Wang, S.-B.; Sun, Y.; Jiang, L.; Wei, F.; Liu, X.-G.; Zeng, L.; Liu, Z.-J. Analysis of cervical and global spine alignment under Roussouly sagittal classification in Chinese cervical spondylotic patients and asymptomatic subjects. Eur. Spine J. 2015, 24, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Son, E.S.; Seo, E.M.; Suk, K.S.; Kim, K.T. Factors determining cervical spine sagittal balance in asymptomatic adults: Correlation with spinopelvic balance and thoracic inlet alignment. Spine J. 2015, 15, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Ames, C.P.; Blondel, B.; Scheer, J.K.; Schwab, F.J.; Le Huec, J.-C.; Massicotte, E.M.; Patel, A.A.; Traynelis, V.C.; Kim, H.J.; Shaffrey, C.I.; et al. Cervical radiographical alignment: Comprehensive assessment techniques and potential importance in cervical myelopathy. Spine 2013, 38 (Suppl. 1), S149–S160. [Google Scholar] [CrossRef] [PubMed]
- Abelin-Genevois, K.; Idjerouidene, A.; Roussouly, P.; Vital, J.M.; Garin, C. Cervical spine alignment in the pediatric population: A radiographic normative study of 150 asymptomatic patients. Eur. Spine J. 2014, 23, 1442–1448. [Google Scholar] [CrossRef] [PubMed]
- Le Huec, J.C.; Demezon, H.; Aunoble, S. Sagittal parameters of global cervical balance using EOS imaging: Normative values from a prospective cohort of asymptomatic volunteers. Eur. Spine J. 2015, 24, 63–71. [Google Scholar] [CrossRef]
- Ha, Y.; Schwab, F.; Lafage, V.; Mundis, G.; Shaffrey, C.; Smith, J.; Bess, S.; Ames, C. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur. Spine J. 2014, 23, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Norton, T.C.; Oakley, P.A.; Haas, J.W.; Harrison, D.E. Positive Outcomes Following Cervical Acceleration-Deceleration (CAD) Injury Using Chiropractic BioPhysics® Methods: A Pre-Auto Injury and Post-Auto Injury Case Series. J. Clin. Med. 2023, 12, 6414. [Google Scholar] [CrossRef] [PubMed]
- Oakley, P.A.; Moustafa, I.M.; Harrison, D.E. Restoration of cervical and lumbar lordosis: CBP® methods overview. In Spinal Deformities in Adolescents, Adults and Older Adults; Bettany-Saltikov, J., Ed.; IntechOpen Publisher: London, UK, 2019; pp. 1–19. [Google Scholar]
- Oakley, P.A.; Kallan, S.Z.; Harrison, D.E. Structural rehabilitation of the cervical lordosis and forward head posture: A selective review of Chiropractic BioPhysics® case reports. J. Phys. Ther. Sci. 2022, 34, 759–771. [Google Scholar] [CrossRef] [PubMed]
- Oakley, P.; Kallan, S.; Harrison, D. Improving the pediatric cervical lordosis: A review of Chiropractic Biophysics® case reporting. J. Contemp. Chiropr. 2022, 5, 190–195. [Google Scholar]
- Calabrese, E.J. On the origins of the linear no-threshold (LNT) dogma by means of untruths, artful dodges and blind faith. Environ. Res. 2015, 142, 432–442. [Google Scholar] [CrossRef] [PubMed]
- Mainprize, J.G.; Yaffe, M.J.; Chawla, T.; Glanc, P. Effects of ionizing radiation exposure during pregnancy. Abdom. Radiol. 2023, 48, 1564–1578. [Google Scholar] [CrossRef] [PubMed]
- Larson, D.B.; Rader, S.B.; Forman, H.P.; Fenton, L.Z. Informing parents about CT radiation exposure in children: It’s OK to tell them. AJR Am. J. Roentgenol. 2007, 189, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Oakley, P.A.; Harrison, D.E. Radiophobia: 7 Reasons Why Radiography Used in Spine and Posture Rehabilitation Should Not Be Feared or Avoided. Dose Response 2018, 16, 1559325818781445. [Google Scholar] [CrossRef] [PubMed]
- Cuttler, J.M. Application of Low Doses of Ionizing Radiation in Medical Therapies. Dose Response 2020, 18, 1559325819895739. [Google Scholar] [CrossRef] [PubMed]
- Selby, P.B.; Calabrese, E.J. How self-interest and deception led to the adoption of the linear non-threshold dose response (LNT) model for cancer risk assessment. Sci. Total Environ. 2023, 898, 165402. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, E.J.; Agathokleous, E.; Giordano, J.; Selby, P.B. Manhattan Project genetic studies: Flawed research discredits LNT recommendations. Environ. Pollut. 2023, 319, 120902. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, E.J.; Agathokleous, E. Is LNT anti-evolution dose response model? Arch. Toxicol. 2022, 96, 3141–3142. [Google Scholar] [CrossRef] [PubMed]
- Doss, M. The Conclusion of the BEIR VII Report Endorsing the Linear No-Threshold Model Is No Longer Valid Due to Advancement of Knowledge. J. Nucl. Med. 2018, 59, 1777. [Google Scholar] [CrossRef] [PubMed]
- Oakley, P.A.; Harrison, D.E. Death of the ALARA Radiation Protection Principle as Used in the Medical Sector. Dose Response 2020, 18, 1559325820921641. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, E.J.; Giordano, J. How did Hermann Muller publish a paper absent any data in the journal Science? Ethical questions and implications of Muller’s Nobel Prize. Chem. Biol. Interact. 2022, 368, 110204. [Google Scholar] [CrossRef]
- Calabrese, E.J. Confirmation that Hermann Muller was dishonest in his Nobel Prize Lecture. Arch. Toxicol. 2023, 97, 2999–3003. [Google Scholar] [CrossRef] [PubMed]
- Schultz, C.H.; Fairley, R.; Murphy, L.S.; Doss, M. The Risk of Cancer from CT Scans and Other Sources of Low-Dose Radiation: A Critical Appraisal of Methodologic Quality. Prehosp. Disaster Med. 2020, 35, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Horton, W.C.; Brown, C.W.; Bridwell, K.H.; Glassman, S.D.; Suk, S.I.; Cha, C.W. Is there an optimal patient stance for obtaining a lateral 36” radiograph? A critical comparison of three techniques. Spine 2005, 30, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Marks, M.; Stanford, C.; Newton, P. Which lateral radiographic positioning technique provides the most reliable and functional representation of a patient’s sagittal balance? Spine 2009, 34, 949–954. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± SD | |||
|---|---|---|---|---|
| Age (years) | 43 ± 12.5 | |||
| Weight (kg) | 74.9 ± 16.5 | |||
| Height (cm) | 169.77 ± 10.76 | |||
| Neck pain intensity (NRS) | 3.29 ± 2.08 | |||
| Gender (%) | ||||
| Male | 36.9 | |||
| Female | 63.1 | |||
| Radiographic Variables | Full Spine | Lateral Cervical | p-value | Cohen’s d c |
| AHT Tz C2-C7 (mm) | 19.84 ± 11.98 | 21.18 ± 11.8 | <0.001 a | 0.228 (0.094, 0.362) |
| ARA C2-C7 (°) | −15.3 ± 14.63 | −18.32 ± 13.16 | <0.001 a | −0.327 (−0.463, −0.191) |
| Atlas Plane Line (APL) (°) | −19.99 ± 8.88 | −22.56 ± 8.93 | <0.001 b | −0.352 (−0.489, −0.214) |
| View and Variable | Kolmogorov–Smirnov a | Shapiro–Wilk | ||||
|---|---|---|---|---|---|---|
| Statistic | df | Sig. | Statistic | df | Sig. | |
| LC_ARA | 0.034 | 215 | 0.200 * | 0.994 | 215 | 0.568 |
| FS_ARA | 0.045 | 215 | 0.200 * | 0.996 | 215 | 0.850 |
| LC_APL | 0.084 | 215 | <0.001 | 0.949 | 215 | <0.001 |
| FS_APL | 0.052 | 215 | 0.200 * | 0.980 | 215 | 0.004 |
| LC_AHT | 0.041 | 215 | 0.200 * | 0.992 | 215 | 0.253 |
| FS_AHT | 0.056 | 215 | 0.200 * | 0.992 | 215 | 0.277 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haas, J.W.; Oakley, P.A.; Betz, J.W.; Miller, J.E.; Jaeger, J.O.; Moustafa, I.M.; Harrison, D.E. Sagittal Full-Spine vs. Sectional Cervical Lateral Radiographs: Are the Measurements of Cervical Alignment Interchangeable? J. Clin. Med. 2024, 13, 2502. https://doi.org/10.3390/jcm13092502
Haas JW, Oakley PA, Betz JW, Miller JE, Jaeger JO, Moustafa IM, Harrison DE. Sagittal Full-Spine vs. Sectional Cervical Lateral Radiographs: Are the Measurements of Cervical Alignment Interchangeable? Journal of Clinical Medicine. 2024; 13(9):2502. https://doi.org/10.3390/jcm13092502
Chicago/Turabian StyleHaas, Jason W., Paul A. Oakley, Joseph W. Betz, Jason E. Miller, Jason O. Jaeger, Ibrahim M. Moustafa, and Deed E. Harrison. 2024. "Sagittal Full-Spine vs. Sectional Cervical Lateral Radiographs: Are the Measurements of Cervical Alignment Interchangeable?" Journal of Clinical Medicine 13, no. 9: 2502. https://doi.org/10.3390/jcm13092502
APA StyleHaas, J. W., Oakley, P. A., Betz, J. W., Miller, J. E., Jaeger, J. O., Moustafa, I. M., & Harrison, D. E. (2024). Sagittal Full-Spine vs. Sectional Cervical Lateral Radiographs: Are the Measurements of Cervical Alignment Interchangeable? Journal of Clinical Medicine, 13(9), 2502. https://doi.org/10.3390/jcm13092502











