Exploring Quality of Life and Mortality in Pertrochanteric Fragility Hip Fractures in Northern Greece: A Single Tertiary Center Study
Abstract
1. Introduction
2. Materials and Methods
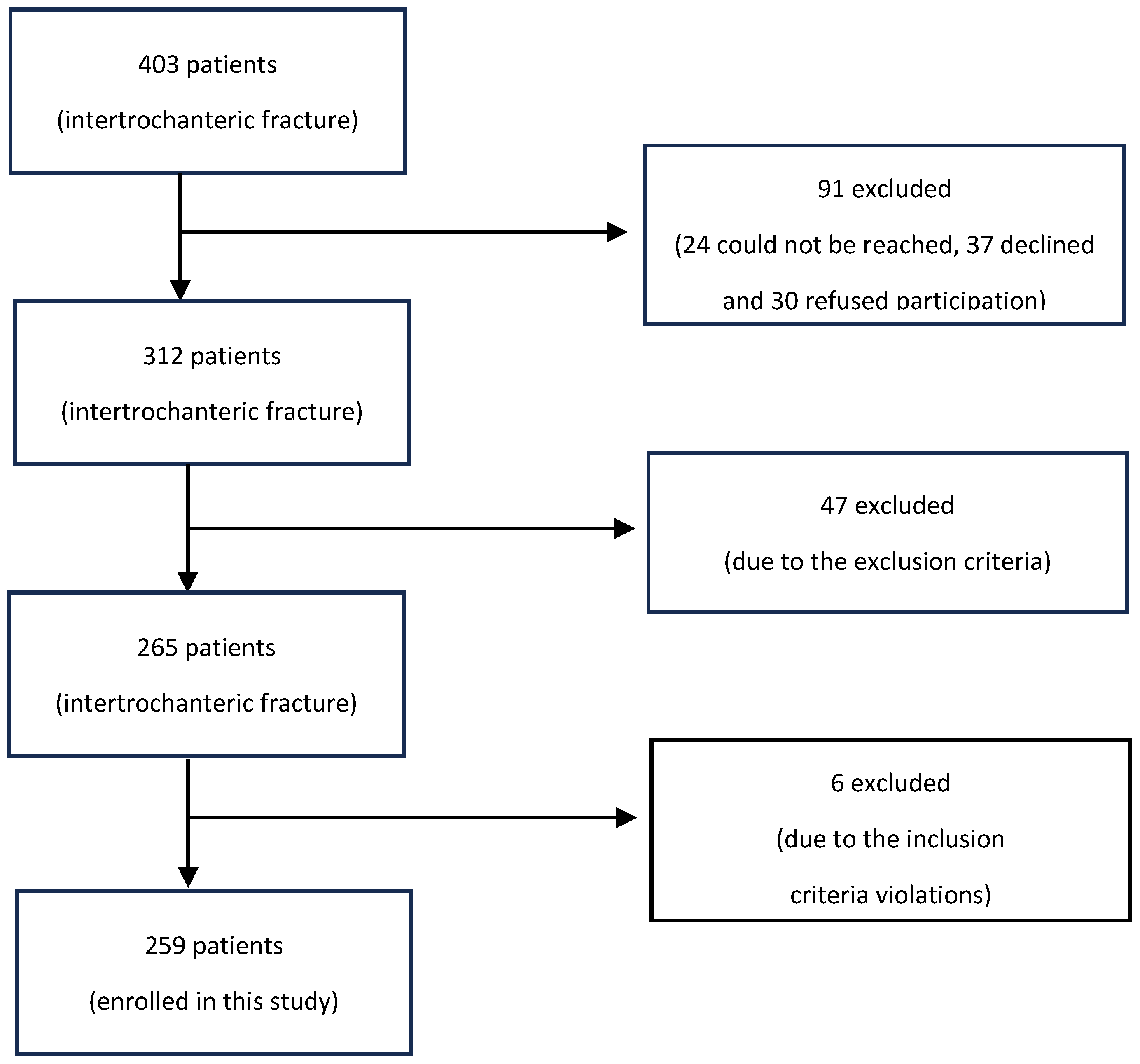
2.1. Study Design and Patients
2.2. Data Collection
2.3. Surgical Technique
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Health-Related Quality of Life
3.3. Mortality
3.4. Transfusion
3.5. Mobility Six Months Post-Op
4. Discussion
4.1. HRQoL Measured by EQ-5D
4.2. HRQoL Measured by SF-12
4.3. Factors Correlated to EQ-5D and SF-12
4.4. Mortality and Mobility
4.5. Factors Correlated to Mortality
4.6. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Walter, N.; Szymski, D.; Kurtz, S.M.; Lowenberg, D.W.; Alt, V.; Lau, E.C.; Rupp, M. Epidemiology and Treatment of Proximal Femoral Fractures in the Elderly U.S. Population. Sci. Rep. 2023, 13, 12734. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Maggi, S. Epidemiology and Social Costs of Hip Fracture. Injury 2018, 49, 1458–1460. [Google Scholar] [CrossRef] [PubMed]
- Anglen, J.O.; Weinstein, J.N. Nail or Plate Fixation of Intertrochanteric Hip Fractures: Changing Pattern of Practice. A Review of the American Board of Orthopaedic Surgery Database. J. Bone Jt. Surg. Am. 2008, 90, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Williamson, S.; Landeiro, F.; McConnell, T.; Fulford-Smith, L.; Javaid, M.K.; Judge, A.; Leal, J. Costs of Fragility Hip Fractures Globally: A Systematic Review and Meta-Regression Analysis. Osteoporos. Int. 2017, 28, 2791–2800. [Google Scholar] [CrossRef] [PubMed]
- Mundi, S.; Pindiprolu, B.; Simunovic, N.; Bhandari, M. Similar Mortality Rates in Hip Fracture Patients over the Past 31 Years. Acta Orthop. 2014, 85, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Haentjens, P.; Autier, P.; Barette, M.; Boonen, S. Predictors of Functional Outcome Following Intracapsular Hip Fracture in Elderly Women. A One-Year Prospective Cohort Study. Injury 2005, 36, 842–850. [Google Scholar] [CrossRef] [PubMed]
- Cornwall, R.; Gilbert, M.S.; Koval, K.J.; Strauss, E.; Siu, A.L. Functional Outcomes and Mortality Vary among Different Types of Hip Fractures: A Function of Patient Characteristics. Clin. Orthop. Relat. Res. 2004, 425, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Buecking, B.; Bliemel, C.; Struewer, J.; Eschbach, D.; Ruchholtz, S.; Müller, T. Use of the Gamma3TM Nail in a Teaching Hospital for Trochanteric Fractures: Mechanical Complications, Functional Outcomes, and Quality of Life. BMC Res. Notes 2012, 5, 651. [Google Scholar] [CrossRef] [PubMed]
- Ju, J.B.; Zhang, P.X.; Jiang, B.G. Risk Factors for Functional Outcomes of the Elderly with Intertrochanteric Fracture: A Retrospective Cohort Study. Orthop. Surg. 2019, 11, 643. [Google Scholar] [CrossRef]
- Giessauf, C.; Glehr, M.; Bernhardt, G.A.; Seibert, F.J.; Gruber, K.; Sadoghi, P.; Leithner, A.; Gruber, G. Quality of Life after Pertrochanteric Femoral Fractures Treated with a γ Nail: A Single Center Study of 62 Patients. BMC Musculoskelet. Disord. 2012, 13, 214. [Google Scholar] [CrossRef]
- Gjertsen, J.E.; Baste, V.; Fevang, J.M.; Furnes, O.; Engesæter, L.B. Quality of Life Following Hip Fractures: Results from the Norwegian Hip Fracture Register. BMC Musculoskelet. Disord. 2016, 17, 265. [Google Scholar] [CrossRef] [PubMed]
- Marks, L.; Pass, B.; Knobe, M.; Volland, R.; Eschbach, D.; Lendemans, S.; Aigner, R.; Schoeneberg, C. Quality of Life, Walking Ability and Change of Living Situation after Trochanteric Femur Fracture in Geriatric Patients-Comparison between Sliding Hip Screw and Cephalomedullary Nails from the Registry for Geriatric Trauma. Injury 2021, 52, 1793–1800. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Roudijk, B.; Ludwig, K.; Devlin, N.; Roudijk, B.; Ludwig, K.; Devlin, N. EQ-5D-5L Value Set Summaries. In Value Sets for EQ-5D-5L; Springer: Cham, Switzerland, 2022; pp. 55–212. [Google Scholar] [CrossRef]
- Kontodimopoulos, N.; Pappa, E.; Niakas, D.; Tountas, Y. Validity of SF-12 Summary Scores in a Greek General Population. Health Qual. Life Outcomes 2007, 5, 55. [Google Scholar] [CrossRef] [PubMed]
- Kontodimopoulos, N.; Pappa, E.; Niakas, D.; Yfantopoulos, J.; Dimitrakaki, C.; Tountas, Y. Validity of the EuroQoL (EQ-5D) Instrument in a Greek General Population. Value Health 2008, 11, 1162–1169. [Google Scholar] [CrossRef]
- Amarilla-Donoso, F.J.; Roncero-Martin, R.; Lavado-Garcia, J.M.; Toribio-Felipe, R.; Moran-Garcia, J.M.; Lopez-Espuela, F. Quality of Life after Hip Fracture: A 12-Month Prospective Study. PeerJ 2020, 2020, e9215. [Google Scholar] [CrossRef]
- Amarilla-Donoso, F.J.; López-Espuela, F.; Roncero-Martín, R.; Leal-Hernandez, O.; Puerto-Parejo, L.M.; Aliaga-Vera, I.; Toribio-Felipe, R.; Lavado-García, J.M. Quality of Life in Elderly People after a Hip Fracture: A Prospective Study. Health Qual. Life Outcomes 2020, 18, 71. [Google Scholar] [CrossRef] [PubMed]
- Moerman, S.; Vochteloo, A.J.H.; Tuinebreijer, W.E.; Maier, A.B.; Mathijssen, N.M.C.; Nelissen, R.G.H.H. Factors Associated with the Course of Health-Related Quality of Life after a Hip Fracture. Arch. Orthop. Trauma. Surg. 2016, 136, 935–943. [Google Scholar] [CrossRef]
- Deutschbein, J.; Lindner, T.; Möckel, M.; Pigorsch, M.; Gilles, G.; Stöckle, U.; Müller-Werdan, U.; Schenk, L. Health-Related Quality of Life and Associated Factors after Hip Fracture. Results from a Six-Month Prospective Cohort Study. PeerJ 2023, 11, e14671. [Google Scholar] [CrossRef]
- Mak, P.H.K.; Campbell, R.C.H.; Irwin, M.G. The ASA Physical Status Classification: Inter-Observer Consistency. Anaesth. Intensive Care 2002, 30, 633–640. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Census Results—ELSTAT. Hellenic Statistical Authority. Available online: https://elstat-outsourcers.statistics.gr/Booklet_AποτελεσματαΠληθυσμου2023_II GR_FINAL2_WEB.pdf (accessed on 14 March 2024).
- Alexiou, K.I.; Roushias, A.; Evaritimidis, S.; Malizos, K.N. Quality of Life and Psychological Consequences in Elderly Patients after a Hip Fracture: A Review. Clin. Interv. Aging 2018, 13, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Peeters, C.M.M.; Visser, E.; Van De Ree, C.L.P.; Gosens, T.; Den Oudsten, B.L.; De Vries, J. Quality of Life after Hip Fracture in the Elderly: A Systematic Literature Review. Injury 2016, 47, 1369–1382. [Google Scholar] [CrossRef] [PubMed]
- Parsons, N.; Griffin, X.L.; Achten, J.; Chesser, T.J.; Lamb, S.E.; Costa, M.L. Modelling and Estimation of Health-Related Quality of Life after Hip Fracture: A Re-Analysis of Data from a Prospective Cohort Study. Bone Jt. Res. 2018, 7, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Jürisson, M.; Pisarev, H.; Kanis, J.; Borgström, F.; Svedbom, A.; Kallikorm, R.; Lember, M.; Uusküla, A. Quality of Life, Resource Use, and Costs Related to Hip Fracture in Estonia. Osteoporos. Int. 2016, 27, 2555–2566. [Google Scholar] [CrossRef] [PubMed]
- Van De Ree, C.L.P.; Landers, M.J.F.; Kruithof, N.; De Munter, L.; Slaets, J.P.J.; Gosens, T.; Jongh, M.A.C. Effect of Frailty on Quality of Life in Elderly Patients after Hip Fracture: A Longitudinal Study. BMJ Open 2019, 9, e025941. [Google Scholar] [CrossRef]
- Milte, R.; Crotty, M.; Miller, M.D.; Whitehead, C.; Ratcliffe, J. Quality of Life in Older Adults Following a Hip Fracture: An Empirical Comparison of the ICECAP-O and the EQ-5D-3 L Instruments. Health Qual. Life Outcomes 2018, 16, 173. [Google Scholar] [CrossRef]
- Buecking, B.; Struewer, J.; Waldermann, A.; Horstmann, K.; Schubert, N.; Balzer-Geldsetzer, M.; Dodel, R.; Bohl, K.; Ruchholtz, S.; Bliemel, C. What Determines Health-Related Quality of Life in Hip Fracture Patients at the End of Acute Care?—A Prospective Observational Study. Osteoporos. Int. 2014, 25, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Ostendorf, M.; van Stel, H.F.; Buskens, E.; Schrijvers, A.J.P.; Marting, L.N.; Verbout, A.J.; Dhert, W.J.A. Patient-Reported Outcome in Total Hip Replacement. A Comparison of Five Instruments of Health Status. J. Bone Jt. Surg. Br. 2004, 86, 801–808. [Google Scholar] [CrossRef]
- Amphansap, T.; Sujarekul, P. Quality of Life and Factors That Affect Osteoporotic Hip Fracture Patients in Thailand. Osteoporos. Sarcopenia 2018, 4, 140. [Google Scholar] [CrossRef]
- Sprague, S.; Bhandari, M.; Heetveld, M.J.; Liew, S.; Scott, T.; Bzovsky, S.; Heels-Ansdell, D.; Zhou, Q.; Swiontkowski, M.; Schemitsch, E.H. Factors Associated with Health-Related Quality of Life, Hip Function, and Health Utility after Operative Management of Femoral Neck Fractures. Bone Jt. J. 2018, 100-B, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Roche, J.J.W.; Wenn, R.T.; Sahota, O.; Moran, C.G. Effect of Comorbidities and Postoperative Complications on Mortality after Hip Fracture in Elderly People: Prospective Observational Cohort Study. BMJ 2005, 331, 1374–1376. [Google Scholar] [CrossRef] [PubMed]
- Ngobeni, R. Mortality in Elderly Patients with Intertrochanteric Fractures: Three Years’ Experience. SA Orthop. J. 2010, 9, 55–60. [Google Scholar]
- Wang, T.; Guo, J.; Long, Y.; Hou, Z. Incidence and Risk Factors of Mortality in Nonagenarians and Centenarians after Intertrochanteric Fracture: 2-Year Follow-Up. Clin. Interv. Aging 2022, 17, 369. [Google Scholar] [CrossRef] [PubMed]
- Boukebous, B.; Maillot, C.; Neouze, A.; Esnault, H.; Gao, F.; Biau, D.; Rousseau, M.A. Excess Mortality after Hip Fracture during COVID-19 Pandemic: More about Disruption, Less about Virulence-Lesson from a Trauma Center. PLoS ONE 2022, 17, e0263680. [Google Scholar] [CrossRef] [PubMed]
- Stitkitti, N.; Amphansap, T.; Therdyothin, A. Mortality and Outcome in Fragility Hip Fracture Care during COVID-19 Pandemic in Police General Hospital, Thailand. Osteoporos. Sarcopenia 2023, 9, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Vochteloo, A.J.H.; Moerman, S.; Tuinebreijer, W.E.; Maier, A.B.; de Vries, M.R.; Bloem, R.M.; Nelissen, R.G.H.H.; Pilot, P. More than Half of Hip Fracture Patients Do Not Regain Mobility in the First Postoperative Year. Geriatr. Gerontol. Int. 2013, 13, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Greve, K.; Modig, K.; Talbäck, M.; Bartha, E.; Hedström, M. No Association between Waiting Time to Surgery and Mortality for Healthier Patients with Hip Fracture: A Nationwide Swedish Cohort of 59,675 Patients. Acta Orthop. 2020, 91, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Leer-Salvesen, S.; Engesæter, L.B.; Dybvik, E.; Furnes, O.; Kristensen, T.B.; Gjertsen, J.E. Does Time from Fracture to Surgery Affect Mortality and Intraoperative Medical Complications for Hip Fracture Patients? An Observational Study of 73 557 Patients Reported to the Norwegian Hip Fracture Register. Bone Jt. J. 2019, 101-B, 1129–1137. [Google Scholar] [CrossRef]
- Greenhalgh, M.S.; Gowers, B.T.V.; Iyengar, K.P.; Adam, R.F. Blood Transfusions and Hip Fracture Mortality—A Retrospective Cohort Study. J. Clin. Orthop. Trauma 2021, 21, 101506. [Google Scholar] [CrossRef]
- Howell, J.; Xu, M.; Duncan, C.P.; Masri, B.A.; Garbuz, D.S. A Comparison between Patient Recall and Concurrent Measurement of Preoperative Quality of Life Outcome in Total Hip Arthroplasty. J. Arthroplast. 2008, 23, 843–849. [Google Scholar] [CrossRef]
- Moldovan, F. Sterile Inflammatory Response and Surgery-Related Trauma in Elderly Patients with Subtrochanteric Fractures. Biomedicines 2024, 12, 354. [Google Scholar] [CrossRef]
- Salman, L.A.; Al-Ani, A.; Radi, M.F.A.; Abudalou, A.F.; Baroudi, O.M.; Ajaj, A.A.; Alkhayarin, M.; Ahmed, G. Open versus Closed Intramedullary Nailing of Femur Shaft Fractures in Adults: A Systematic Review and Meta-Analysis. Int. Orthop. 2023, 47, 3031–3041. [Google Scholar] [CrossRef]
| (a) | ||||
| Patients Characteristics | All Patients | Female | Male | p |
| Number (%) | 259 (100) | 212 (81.9) | 47 (18.1) | |
| Age, mean (range) | 83.6 (60–99) | 84.0 (60–99) | 81.7 (62–95) | 0.626 |
| ASA score, mean (range) | 3 (2–4) | 3.0 (2–4) | 3.11 (2–4) | 0.961 |
| CCI, mean (SD) | 5.7 (2–13) | 5.7 (2–13) | 6.0 (3–13) | 0.245 |
| Smoking (%) | 42 (16.2) | 24 (11.3) | 18 (38.3) | <0.001 |
| Non smoking | 217 (83.8) | 188 (88.7) | 29 (61.7) | <0.001 |
| Living in home pre Fx (%) | 245 (94.6) | 199 (93.9) | 46 (97.9) | 0.204 |
| Living in facilities (%) | 14 (5.4) | 13 (6.1) | 1 (2.1) | 0.835 |
| Osteoprotective Treatment pre-Fx (%) | 10 (3.9) | 10 (4.7) | 0 (0.0) | - |
| Days to operation, mean (range) | 2.7 (0–11) | 2.6 (0–9) | 3.1 (0–11) | 0.047 |
| Mean hospitalization time, Days (range) | 7.5 (1–23) | 7.4 (1–23) | 8.3 (2–17) | 0.538 |
| (b) | ||||
| Patients Characteristics | All Patients | Pre-COVID-19 Era | Post-COVID-19 Era | p |
| Number (%) | 259 (100) | 101 (39%) | 158 (61%) | |
| Age, mean (range) | 83.6 (60–99) | 83.9 (63–98) | 83.3 (60–99) | 0.790 |
| ASA score, mean (range) | 3 (2–4) | 2.9 (2–4) | 3.1 (2–4) | 0.989 |
| CCI, mean (range) | 5.7 (2–13) | 5.8 (3–13) | 5.7 (2–13) | 0.487 |
| Smoking (%) | 42 (16.2) | 12 (12.0) | 30 (19.0) | 0.361 |
| Non smoking | 217 (83.8) | 89 (88.0) | 128 (81.0) | 0.02 |
| Living in home pre Fx (%) | 245 (94.6) | 98 (97.0) | 147 (93.0) | 0.159 |
| Living in facilities (%) | 14 (5.4) | 3 (3.0) | 11 (7.0) | 0.604 |
| Osteoprotective Treatment pre-Fx (%) | 10 (3.9) | 3 (3.0) | 7 (4.4) | 0.928 |
| Days to operation, mean (range) | 2.7 (0–11) | 3.3 (0–11) | 2.3 (0–9) | 0.284 |
| Mean hospitalization time, Days (range) | 7.5 (1–23) | 8.5 (4–17) | 7.4 (1–23) | 0.049 |
| Rehabilitation Centre post op (%) | 179 (69.1) | 75 (74.3) | 104 (65.8) | 0.01 |
| No rehab-centre post-op (%) | 80 (30.9) | 26 (25.7) | 54 (34.2) | 0.11 |
| (a) | ||||
| Pre-Fracture | 6 Months Post-Op | p | Effect Size | |
| EQ-5D index | 0.74 | 0.39 | <0.001 | 1.11 |
| EQ-5D VAS | 69.7 | 42.4 | <0.001 | 2.46 |
| SF-12 PCS | 34.2 | 27.6 | <0.001 | 1.21 |
| SF-12 MCS | 54.49 | 38.6 | <0.001 | 1.02 |
| (b) | ||||
| EQ-5D | SF-12 | |||
| Age | Spearman r | 0.077 | 0.156 | |
| p | 0.438 | 0.116 | ||
| ASA score | Spearman r | 0.134 | 0.232 | |
| p | 0.178 | 0.018 | ||
| CCI * | Spearman r | 0.080 | −0.018 | |
| p | 0.419 | 0.857 | ||
| Own home | U | 1009.5 | 1091.0 | |
| p | 0.543 | 0.977 | ||
| Rehabilitation Center | U | 864.0 | 944.5 | |
| p | 0.224 | 0.540 | ||
| All Patients | Female | Male | p | Pre-Pandemic | Pandemic | p | |
|---|---|---|---|---|---|---|---|
| 30-days mortality (%) | 24 (9.3) | 16 (7.5) | 8 (17.0) | 0.087 | 5 (5.0) | 19 (12.0) | 0.003 |
| 1-year mortality (%) | 84 (32.4) | 71 (33.5) | 13 (27.7) | 0.21 | 28 (27.7) | 56 (35.4) | 0.196 |
| 30 Days Mortality | ||
| x2 | p | |
| ASA | 8.546 | 0.014 |
| CCI | 7.590 | 0.669 |
| Gender | 2.932 | 0.087 |
| Transfusion | 1.289 | 0.256 |
| 1 Year Mortality | ||
| x2 | p | |
| ASA | 4.305 | 0.116 |
| CCI | 9.986 | 0.442 |
| Gender | 1.573 | 0.21 |
| Transfusion | 0.939 | 0.319 |
| Characteristics | Mortality Group (n = 84) | Survival Group (n = 175) | p | Effect Size |
|---|---|---|---|---|
| Age, years (range) | 86.7 (66–99) | 82.0 (60–98) | <0.001 | 0.62 |
| Hemoglobin | ||||
| In Admission (g/dL) | 11.5 (7–15.2) | 12.0 (7.5–16.1) | <0.001 | 0.28 |
| On Discharge (g/dL) | 10.2 (7.5–12.4) | 10.0 (8–13.5) | <0.001 | 0.1 |
| Delay to operate (in days) | 2.8 (0–8) | 2.6 (0–11) | =0.091 | 0.09 |
| Characteristics | Non Transfused (n = 87) | Transfused (n = 172) | p | Effect Size |
|---|---|---|---|---|
| Age, years (range) | 81.3 (62–97) | 84.7 (60–99) | <0.001 | 0.44 |
| Hemoglobin | ||||
| Admision (g/gL) | 12.9 (7.9–16.1) | 11.4 (7–15.2) | <0.001 | 0.9 |
| Discharge (g/dL) | 10.7 (8.4–13.5) | 9.8 (7.5–12.5) | <0.001 | 0.45 |
| Delay to operate in days | 2.6 (0–8) | 2.7 (0–11) | 0.093 | 0.045 |
| Post-Op Mobility | ||||||
|---|---|---|---|---|---|---|
| 1/5 | 2/5 | 3/5 | 4/5 | 5/5 | ||
| Pre-FX mobility | 1/5 | 100.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| 2/5 | 40.0% | 40.0% | 0.0% | 20.0% | 0.0% | |
| 3/5 | 14.8% | 44.4% | 37.0% | 3.7% | 0.0% | |
| 4/5 | 9.5% | 19.0% | 57.1% | 14.3% | 0.0% | |
| 5/5 | 16.7% | 4.2% | 33.3% | 37.5% | 8.3% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konstantinou, P.; Kostretzis, L.; Fragkiadakis, G.; Touchtidou, P.; Mavrovouniotis, A.; Davitis, V.; Ditsiou, A.Z.; Gigis, I.; Nikolaides, A.P.; Niakas, D.; et al. Exploring Quality of Life and Mortality in Pertrochanteric Fragility Hip Fractures in Northern Greece: A Single Tertiary Center Study. J. Clin. Med. 2024, 13, 2478. https://doi.org/10.3390/jcm13092478
Konstantinou P, Kostretzis L, Fragkiadakis G, Touchtidou P, Mavrovouniotis A, Davitis V, Ditsiou AZ, Gigis I, Nikolaides AP, Niakas D, et al. Exploring Quality of Life and Mortality in Pertrochanteric Fragility Hip Fractures in Northern Greece: A Single Tertiary Center Study. Journal of Clinical Medicine. 2024; 13(9):2478. https://doi.org/10.3390/jcm13092478
Chicago/Turabian StyleKonstantinou, Panagiotis, Lazaros Kostretzis, Georgios Fragkiadakis, Panagiota Touchtidou, Argyrios Mavrovouniotis, Vasileios Davitis, Athina Zacharoula Ditsiou, Ioannis Gigis, Anastasios P. Nikolaides, Dimitris Niakas, and et al. 2024. "Exploring Quality of Life and Mortality in Pertrochanteric Fragility Hip Fractures in Northern Greece: A Single Tertiary Center Study" Journal of Clinical Medicine 13, no. 9: 2478. https://doi.org/10.3390/jcm13092478
APA StyleKonstantinou, P., Kostretzis, L., Fragkiadakis, G., Touchtidou, P., Mavrovouniotis, A., Davitis, V., Ditsiou, A. Z., Gigis, I., Nikolaides, A. P., Niakas, D., Papadopoulos, P., & Ditsios, K. (2024). Exploring Quality of Life and Mortality in Pertrochanteric Fragility Hip Fractures in Northern Greece: A Single Tertiary Center Study. Journal of Clinical Medicine, 13(9), 2478. https://doi.org/10.3390/jcm13092478







