Long-Term Mortality after Transcatheter Edge-to-Edge Mitral Valve Repair Significantly Decreased over the Last Decade: Comparison between Initial and Current Experience from the MiTra Ulm Registry
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Outcomes and Definitions
2.3. Statistics
3. Results
3.1. Baseline Characteristics
3.2. Echocardiographic and Invasive Hemodynamic Assessment
3.3. Short-Term Outcomes
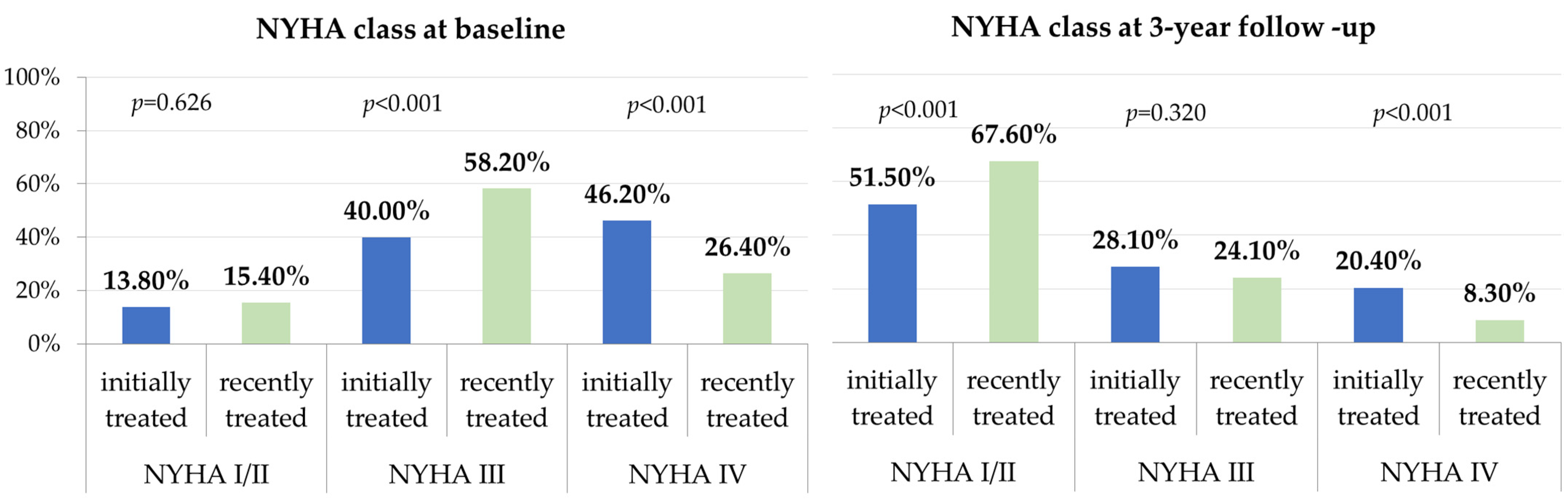
3.4. Functional Outcomes in the First vs. Current M-TEER Experience
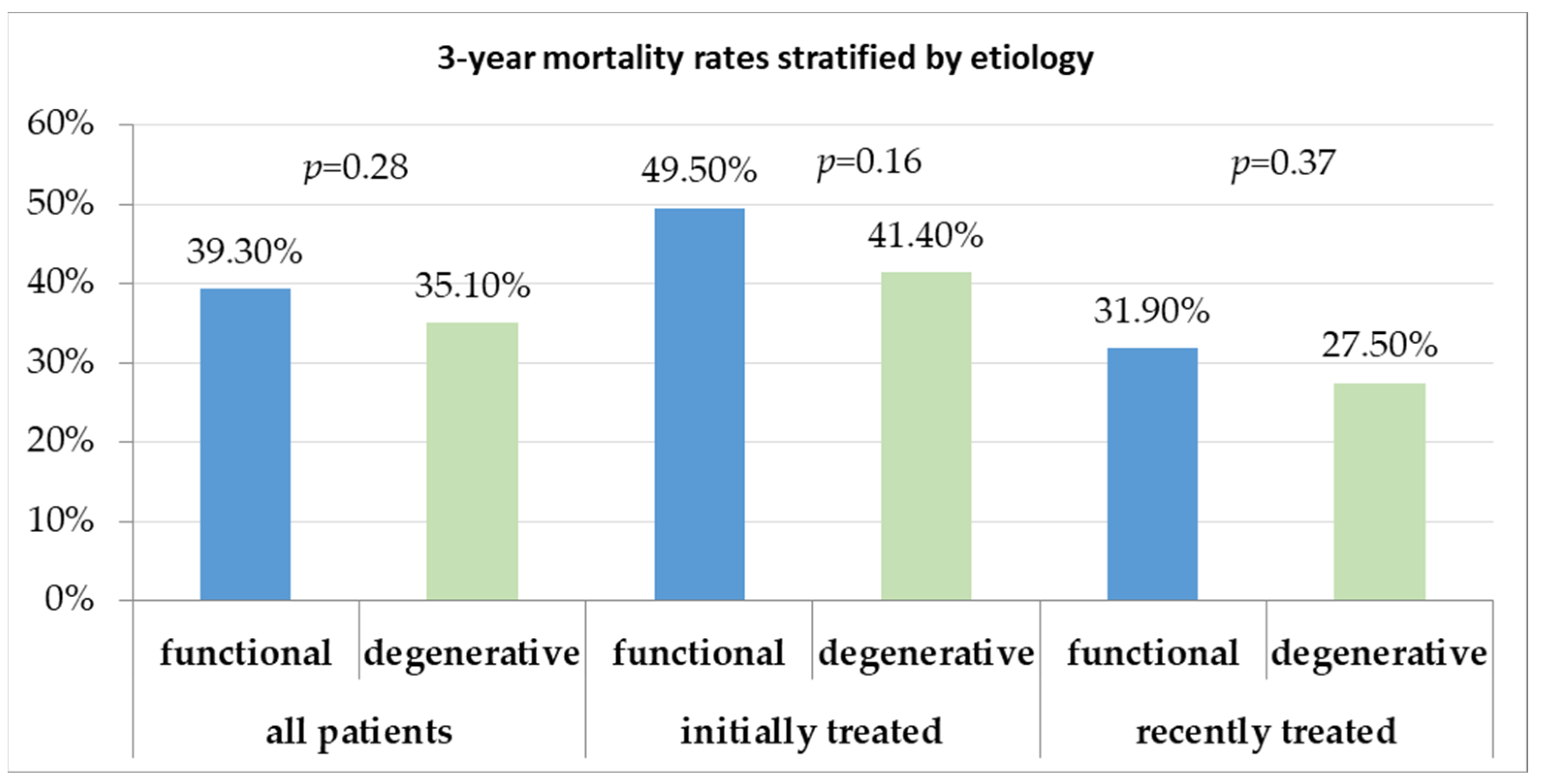
3.5. Trends in Long-Term Follow-Up over the Last Decade
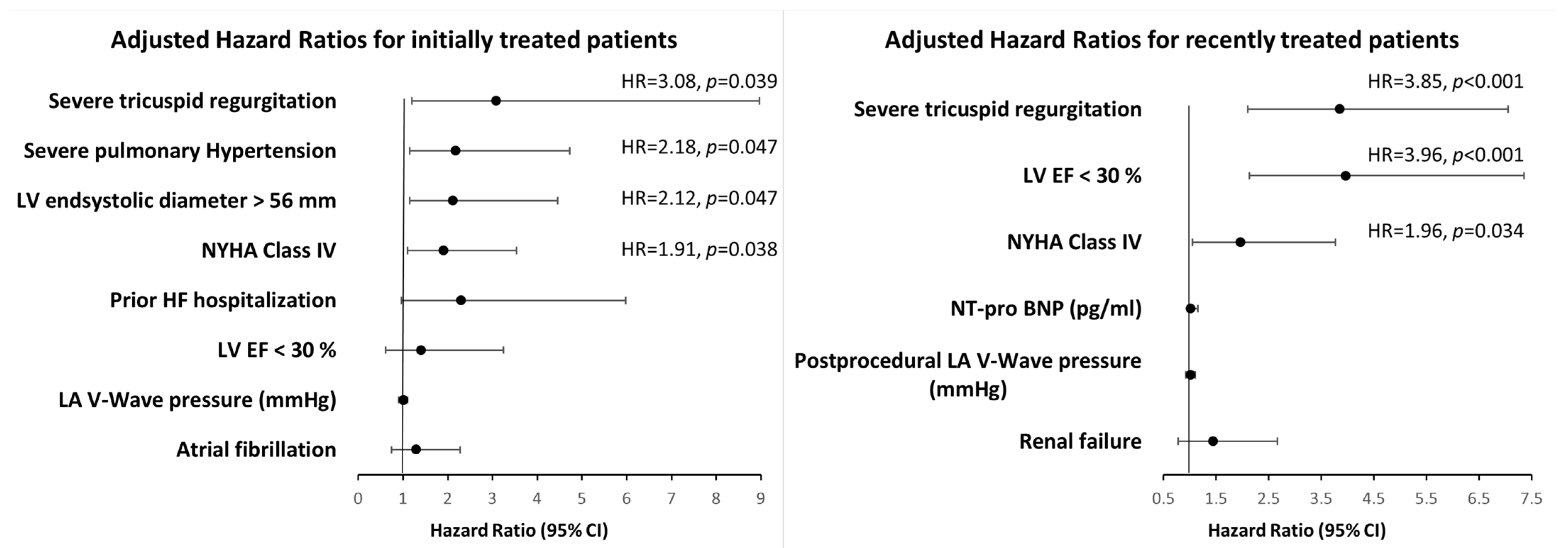
3.6. Predictors of Long-Term Mortality over the Last Decade
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; et al. Percutaneous Repair or Surgery for Mitral Regurgitation. N. Engl. J. Med. 2011, 364, 1395–1406. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Grayburn, P.A.; Rinaldi, M.; Kapadia, S.R.; et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N. Engl. J. Med. 2018, 379, 2307–2318. [Google Scholar] [CrossRef] [PubMed]
- Puls, M.; Lubos, E.; Boekstegers, P.; von Bardeleben, R.S.; Ouarrak, T.; Butter, C.; Zuern, C.S.; Bekeredjian, R.; Sievert, H.; Nickenig, G.; et al. One-Year Outcomes and Predictors of Mortality after MitraClip Therapy in Contemporary Clinical Practice: Results from the German Transcatheter Mitral Valve Interventions Registry. Eur. Heart J. 2016, 37, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Baldus, S.; Schillinger, W.; Franzen, O.; Bekeredjian, R.; Sievert, H.; Schofer, J.; Kuck, K.-H.; Konorza, T.; Möllmann, H.; Hehrlein, C.; et al. MitraClip Therapy in Daily Clinical Practice: Initial Results from the German Transcatheter Mitral Valve Interventions (TRAMI) Registry. Eur. J. Heart Fail. 2012, 14, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. EuroIntervention 2022, 17, e1126–e1196. [Google Scholar] [CrossRef] [PubMed]
- Feldman, T.; Kar, S.; Elmariah, S.; Smart, S.C.; Trento, A.; Siegel, R.J.; Apruzzese, P.; Fail, P.; Rinaldi, M.J.; Smalling, R.W.; et al. Randomized Comparison of Percutaneous Repair and Surgery for Mitral Regurgitation. J. Am. Coll. Cardiol. 2015, 66, 2844–2854. [Google Scholar] [CrossRef] [PubMed]
- Kalbacher, D.; Schäfer, U.; Bardeleben, R.S.v.; Eggebrecht, H.; Sievert, H.; Nickenig, G.; Butter, C.; May, A.E.; Bekeredjian, R.; Ouarrak, T.; et al. Long-Term Outcome, Survival and Predictors of Mortality after MitraClip Therapy: Results from the German Transcatheter Mitral Valve Interventions (TRAMI) Registry. Int. J. Cardiol. 2019, 277, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Obadia, J.-F.; Messika-Zeitoun, D.; Leurent, G.; Iung, B.; Bonnet, G.; Piriou, N.; Lefèvre, T.; Piot, C.; Rouleau, F.; Carrié, D.; et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N. Engl. J. Med. 2018, 379, 2297–2306. [Google Scholar] [CrossRef] [PubMed]
- Iung, B.; Armoiry, X.; Vahanian, A.; Boutitie, F.; Mewton, N.; Trochu, J.; Lefèvre, T.; Messika-Zeitoun, D.; Guerin, P.; Cormier, B.; et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation: Outcomes at 2 Years. Eur. J. Heart Fail. 2019, 21, 1619–1627. [Google Scholar] [CrossRef] [PubMed]
- Mack, M.J.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.K.; Grayburn, P.A.; Rinaldi, M.J.; Kapadia, S.R.; et al. 3-Year Outcomes of Transcatheter Mitral Valve Repair in Patients with Heart Failure. J. Am. Coll. Cardiol. 2021, 77, 1029–1040. [Google Scholar] [CrossRef] [PubMed]
- Nita, N.; Schneider, L.; Dahme, T.; Markovic, S.; Keßler, M.; Rottbauer, W.; Tadic, M. Trends in Transcatheter Edge-to-Edge Mitral Valve Repair Over a Decade: Data From the MiTra ULM Registry. Front. Cardiovasc. Med. 2022, 9, 850356. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Muñoz, D.R.; et al. 2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Rev. Española De Cardiol. (Engl. Ed.) 2018, 71, 110. [Google Scholar] [CrossRef]
- Clinical Trial Design Principles and Endpoint Definitions for Transcatheter Mitral Valve Repair and Replacement: Part 2: Endpoint Definitions: A Consensus Document from the Mitral Valve Academic Research Consortium–PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/26184623/ (accessed on 22 April 2022).
- Kar, S.; Feldman, T.; Qasim, A.; Trento, A.; Kapadia, S.; Pedersen, W.; Lim, D.S.; Kipperman, R.; Smalling, R.W.; Bajwa, T.; et al. Five-Year Outcomes of Transcatheter Reduction of Significant Mitral Regurgitation in High-Surgical-Risk Patients. Heart 2019, 105, 1622–1628. [Google Scholar] [CrossRef] [PubMed]
- Orban, M.; Karam, N.; Lubos, E.; Kalbacher, D.; Braun, D.; Deseive, S.; Neuss, M.; Butter, C.; Praz, F.; Kassar, M.; et al. Impact of Proportionality of Secondary Mitral Regurgitation on Outcome After Transcatheter Mitral Valve Repair. JACC Cardiovasc. Imaging 2021, 14, 715–725. [Google Scholar] [CrossRef] [PubMed]
- Maor, E.; Raphael, C.E.; Panaich, S.S.; Reeder, G.S.; Nishimura, R.A.; Nkomo, V.T.; Rihal, C.S.; Eleid, M.F. Acute Changes in Left Atrial Pressure after MitraClip Are Associated with Improvement in 6-Minute Walk Distance. Circ Cardiovasc. Interv. 2017, 10, e004856. [Google Scholar] [CrossRef] [PubMed]
- Predictors of Left Ventricular Reverse Remodeling after Percutaneous Therapy for Mitral Regurgitation with the MitraClip System–PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/32104977/ (accessed on 22 April 2022).
- Grayburn, P.A.; Foster, E.; Sangli, C.; Weissman, N.J.; Massaro, J.; Glower, D.G.; Feldman, T.; Mauri, L. Relationship between the Magnitude of Reduction in Mitral Regurgitation Severity and Left Ventricular and Left Atrial Reverse Remodeling after MitraClip Therapy. Circulation 2013, 128, 1667–1674. [Google Scholar] [CrossRef] [PubMed]
- Grasso, C.; Popolo Rubbio, A.; Capodanno, D.; Buccheri, S.; Di Salvo, M.E.; Cannata, S.; Scandura, S.; Mangiafico, S.; Farruggio, S.; Salerno, T.; et al. Incidence, Timing, Causes and Predictors of Early and Late Re-Hospitalization in Patients Who Underwent Percutaneous Mitral Valve Repair with the MitraClip System. Am. J. Cardiol. 2018, 121, 1253–1259. [Google Scholar] [CrossRef] [PubMed]

| All (n = 677) | Initially Treated (n = 340) | Recently Treated (n = 337) | p-Value | |
|---|---|---|---|---|
| Age (years) | 76 ± 8 | 76 ± 8 | 76 ± 9 | 0.683 |
| Male (%) | 402 (59.4) | 208 (61.1) | 194 (57.6) | 0.342 |
| Functional MR (%) | 429 (63.3) | 233 (68.4) | 196 (58.2) | 0.004 |
| NYHA class | ||||
| I–II (%) | 99 (14.7) | 47 (13.8) | 52 (15.4) | 0.626 |
| III (%) | 332 (49.0) | 136 (40.0) | 196 (58.2) | <0.001 |
| IV (%) | 246 (36.3) | 157(46.2) | 89 (26.4) | <0.001 |
| Prior heart failure hospitalization | 338 (49.9) | 200 (58.8) | 138 (40.9) | <0.001 |
| Interventions and surgeries | ||||
| PCI (%) | 308 (45.5) | 143(42.1) | 165 (48.9) | 0.060 |
| CABG (%) | 108 (16) | 60 (17.7) | 48 (14.2) | 0.273 |
| Valve surgery (%) | 40 (5.9) | 22 (6.4) | 18 (5.3) | 0.566 |
| Comorbidities | ||||
| Previous MI (%) | 159 (23.5) | 70 (20.6) | 89 (26.4) | 0.103 |
| CAD (%) | 469 (69.3) | 246 (72.5) | 223 (66.1) | 0.064 |
| DCM (%) | 123 (18.2) | 59(17.4) | 64(18.9) | 0.605 |
| Hypertension (%) | 544 (80.4) | 280 (82.3) | 264 (78.3) | 0.185 |
| Diabetes (%) | 192 (28.3) | 112 (33) | 80 (23.7) | 0.177 |
| Atrial fibrillation (%) | 441 (65.1) | 228 (67.1) | 213 (63.2) | 0.273 |
| Peripheral artery disease (%) | 60 (8.9) | 31 (9.4) | 29 (8.6) | 0.676 |
| COPD (%) | 84 (12.4) | 47 (13.7) | 37 (10.9) | 0.299 |
| Chronic renal failure (%) | 365 (53.9) | 190 (56) | 175 (52) | 0.252 |
| Previous cancer (%) | 116 (17.2) | 61 (18) | 55 (16.3) | 0.203 |
| Antiarrhythmia devices | ||||
| CRT (%) | 66 (9.8) | 36 (10.7) | 30 (8.9) | 0.369 |
| ICD (%) | 97 (14.3) | 68 (20) | 29 (8.6) | 0.022 |
| Pacemaker (%) | 62 (9.2) | 36 (9.9) | 26 (8.7) | 0.505 |
| Euro Score II | 8.4 ± 8.2 | 9.6 ± 8.1 | 7.8 ± 8.2 | <0.001 |
| Therapy | ||||
| Loop diuretics (%) | 523 (77.3) | 264 (77.7) | 259 (76.8) | 0.757 |
| ACEI (%) | 319 (47.1) | 173 (51) | 146 (43) | 0.034 |
| ARB (%) | 185 (27.3) | 82 (24.1) | 103 (31) | 0.037 |
| ARNI (%) | 78(11.5) | 8(2.3) | 70 (20.7) | 0.001 |
| Beta-blockers (%) | 586 (86.6) | 292 (86) | 294 (87.2) | 0.501 |
| Aldosterone antagonists (%) | 304 (44.9) | 121 (41) | 183 (54) | 0.032 |
| Laboratory | ||||
| GFR (mL/min/1.73 m2) | 47 ± 19 | 46 ± 18 | 49 ± 20 | 0.137 |
| Troponin T (ng/L) | 87 ± 144 | 139 ± 211 | 43 ± 98 | 0.021 |
| NT-pro-BNP (pg/mL) | 6601 ± 7238 | 7264 ± 7011 | 5995 ± 7398 | 0.001 |
| All (n = 677) | Initially Treated (n = 340) | Recently Treated (n = 337) | p-Value | |
|---|---|---|---|---|
| Echocardiography | ||||
| LVEF (%) | 44 ± 17 | 43 ± 17 | 44 ± 17 | 0.434 |
| LVEDD (mm) | 60 ± 11 | 62 ± 12 | 58 ± 10 | 0.017 |
| LVESD (mm) | 47 ± 15 | 49 ± 16 | 43 ± 13 | 0.007 |
| Interventricular septum thickness (mm) | 11 ± 4.8 | 10.5 ± 2.4 | 11.3 ± 6 | 0.039 |
| LA (mm) | 57 ± 10 | 58 ± 12 | 55 ± 8 | 0.045 |
| sPAP | 59 ± 17 | 62 ± 20 | 57 ± 15 | 0.047 |
| EROA | 0.43 ± 0.35 | 0.48 ± 0.4 | 0.4 ± 0.31 | 0.003 |
| Carpentier Type I | 205(30.1) | 111(32.7) | 94(27.6) | 0.139 |
| Carpentier Type II | 141(20.9) | 67(19.7) | 74(21.7) | 0.553 |
| Carpentier Type IIIa | 109(16.3) | 42(12.3) | 67(20.4) | 0.002 |
| Carpentier Type IIIb | 222(32.7) | 120(35.3) | 102(30.3) | 0.147 |
| Severe TR (grade III/IV) | 253(37.3) | 161(47.3) | 92 (27.3) | <0.001 |
| Catheterization | ||||
| Heart rate (beat/min) | 72 ± 15 | 72 ± 14 | 71 ± 17 | 0.241 |
| Mean RA pressure (mmHg) | 11 ± 7 | 11 ± 6 | 10 ± 7 | 0.102 |
| Mean RV pressure (mmHg) | 26 ± 28 | 32 ± 32 | 13 ± 8 | <0.001 |
| Systolic PA pressure (mmHg) | 55 ± 19 | 57 ± 21 | 50 ± 15 | 0.011 |
| Diastolic PA pressure (mmHg) | 23 ± 14 | 25 ± 15 | 19 ± 8 | 0.041 |
| Mean PA pressure (mmHg) | 34 ± 14 | 35 ± 15 | 32 ± 11 | 0.015 |
| Mean LA pressure (mmHg) | 27± 18 | 28 ± 18 | 22 ± 18 | 0.016 |
| V wave LA pressure | 32± 16 | 37 ± 18 | 30 ± 15 | 0.003 |
| SVR (dynes/seconds/cm−5) | 2019 ± 2201 | 2812 ± 529 | 1996 ± 2227 | 0.009 |
| Cardiac index (L/min/m2) | 2.08 ± 0.55 | 2.06 ± 0.57 | 2.13 ± 0.50 | 0.143 |
| All (n = 677) | Initially Treated (n = 340) | Recently Treated (n = 337) | p-Value | |
|---|---|---|---|---|
| Time after procedure (days) | 6.7 ± 5.6 | 7.69 ± 5.6 | 5.7 ± 5.3 | <0.001 |
| ICU length (days) | 1.0 ± 3.9 | 1.05 ± 3.9 | 0.94 ± 3.9 | <0.001 |
| Fluoroscopy time (min) | 29 ± 17 | 30 ± 17 | 27 ± 17 | <0.001 |
| Number of clips implanted | 1.3 ±0.7 | 1.3 ±0.5 | 1.41 ±0.9 | 0.281 |
| MVARC device success | 635 (93.8) | 317 (93.3) | 318 (94.3) | 0.660 |
| Post-procedural mean LA pressure (mmHg) | 15 ± 6 | 16 ± 6 | 12 ± 4 | <0.001 |
| Post-procedural v wave LA pressure | 22 ± 11 | 24 ± 9 | 19 ± 11 | <0.001 |
| Grade of MR after procedure | 1.5 ± 0.7 | 1.6 ± 0.7 | 1.5 ± 0.6 | 0.093 |
| Transmitral mean gradient after procedure | 3.4 ± 1.90 | 3.4 ± 2.2 | 3.5 ± 1.7 | 0.224 |
| Periprocedural mortality | 21 (3.1) | 10 (2.9) | 11 (3.2) | 0.848 |
| 30-day rehospitalization | 26 (3.9) | 13 (3.8) | 13 (3.9) | 0.920 |
| 30-day all-cause mortality | 27 (4) | 12 (3.5) | 15 (4.5) | 0.470 |
| 30-day MACCE | 51 (7.6) | 27 (8) | 24 (7.1) | 0.703 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nita, N.; Tadic, M.; Mörike, J.; Paukovitsch, M.; Felbel, D.; Keßler, M.; Gröger, M.; Schneider, L.-M.; Rottbauer, W. Long-Term Mortality after Transcatheter Edge-to-Edge Mitral Valve Repair Significantly Decreased over the Last Decade: Comparison between Initial and Current Experience from the MiTra Ulm Registry. J. Clin. Med. 2024, 13, 2172. https://doi.org/10.3390/jcm13082172
Nita N, Tadic M, Mörike J, Paukovitsch M, Felbel D, Keßler M, Gröger M, Schneider L-M, Rottbauer W. Long-Term Mortality after Transcatheter Edge-to-Edge Mitral Valve Repair Significantly Decreased over the Last Decade: Comparison between Initial and Current Experience from the MiTra Ulm Registry. Journal of Clinical Medicine. 2024; 13(8):2172. https://doi.org/10.3390/jcm13082172
Chicago/Turabian StyleNita, Nicoleta, Marijana Tadic, Johannes Mörike, Michael Paukovitsch, Dominik Felbel, Mirjam Keßler, Matthias Gröger, Leonhard-Moritz Schneider, and Wolfgang Rottbauer. 2024. "Long-Term Mortality after Transcatheter Edge-to-Edge Mitral Valve Repair Significantly Decreased over the Last Decade: Comparison between Initial and Current Experience from the MiTra Ulm Registry" Journal of Clinical Medicine 13, no. 8: 2172. https://doi.org/10.3390/jcm13082172
APA StyleNita, N., Tadic, M., Mörike, J., Paukovitsch, M., Felbel, D., Keßler, M., Gröger, M., Schneider, L.-M., & Rottbauer, W. (2024). Long-Term Mortality after Transcatheter Edge-to-Edge Mitral Valve Repair Significantly Decreased over the Last Decade: Comparison between Initial and Current Experience from the MiTra Ulm Registry. Journal of Clinical Medicine, 13(8), 2172. https://doi.org/10.3390/jcm13082172






