Abdominal Arterial Translation in Lower Lumbar Spine Level Due to Positional Change: A Clinical Survey Using Intraoperative Computed Tomography
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
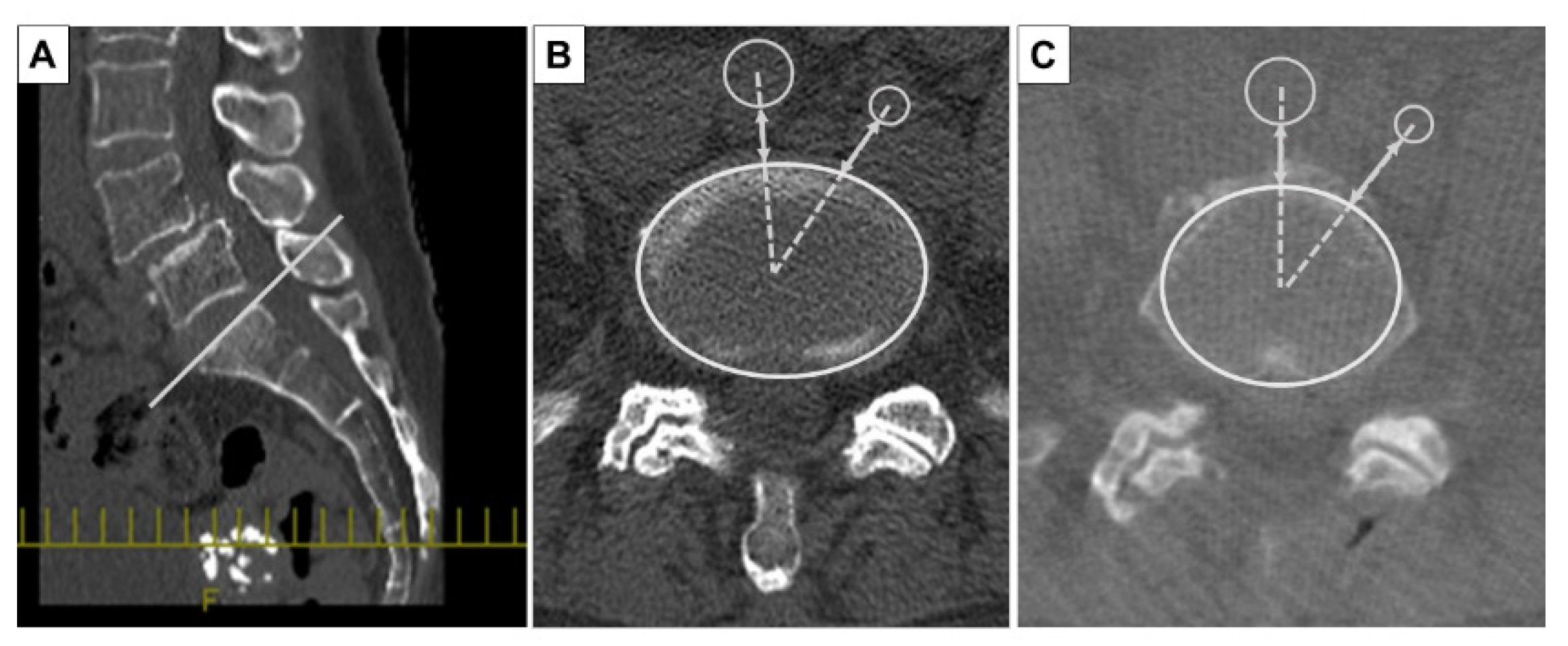
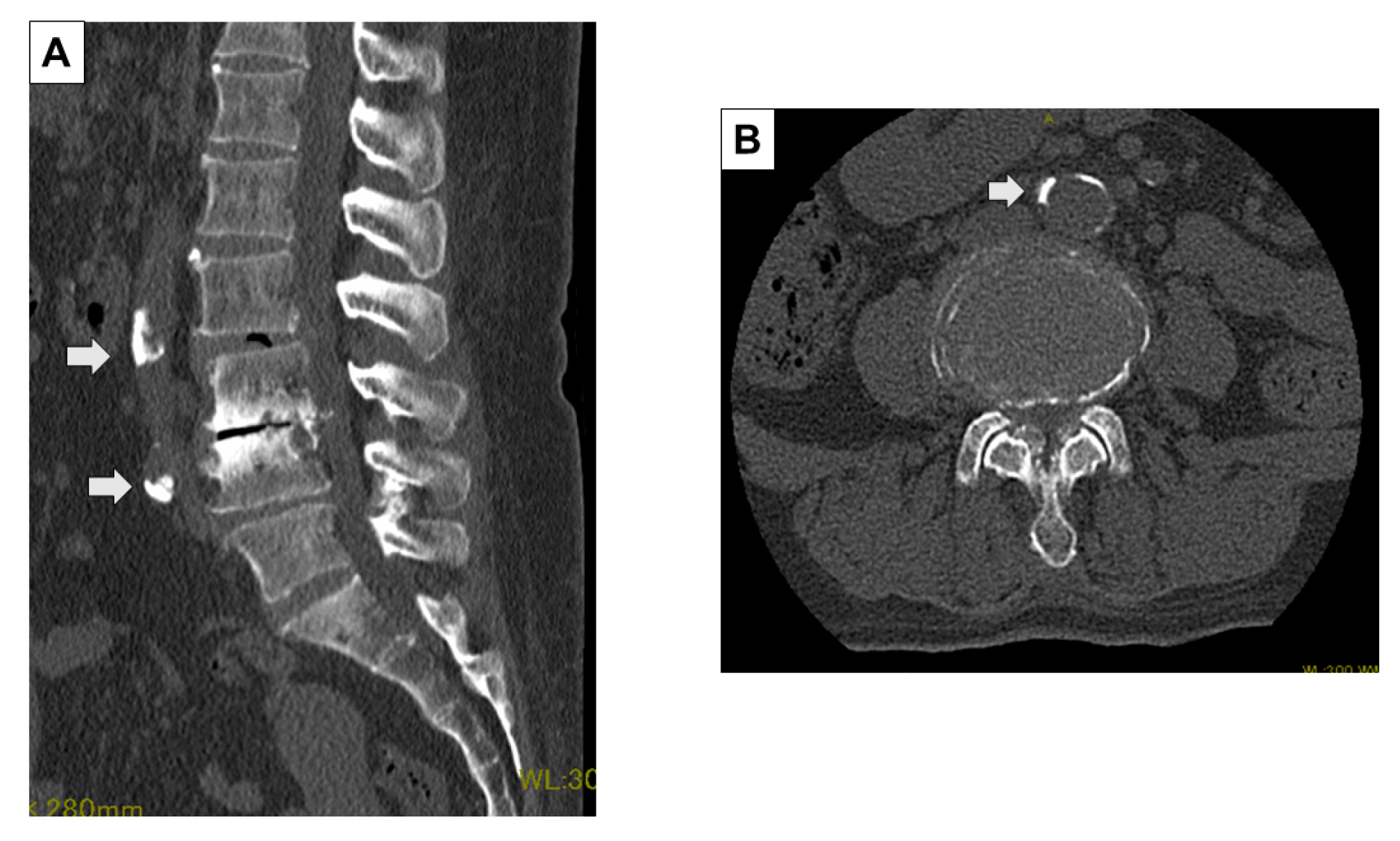
2.2. Evaluation Method of Preoperative and Intraoperative CT Images
2.3. Statistical Analysis
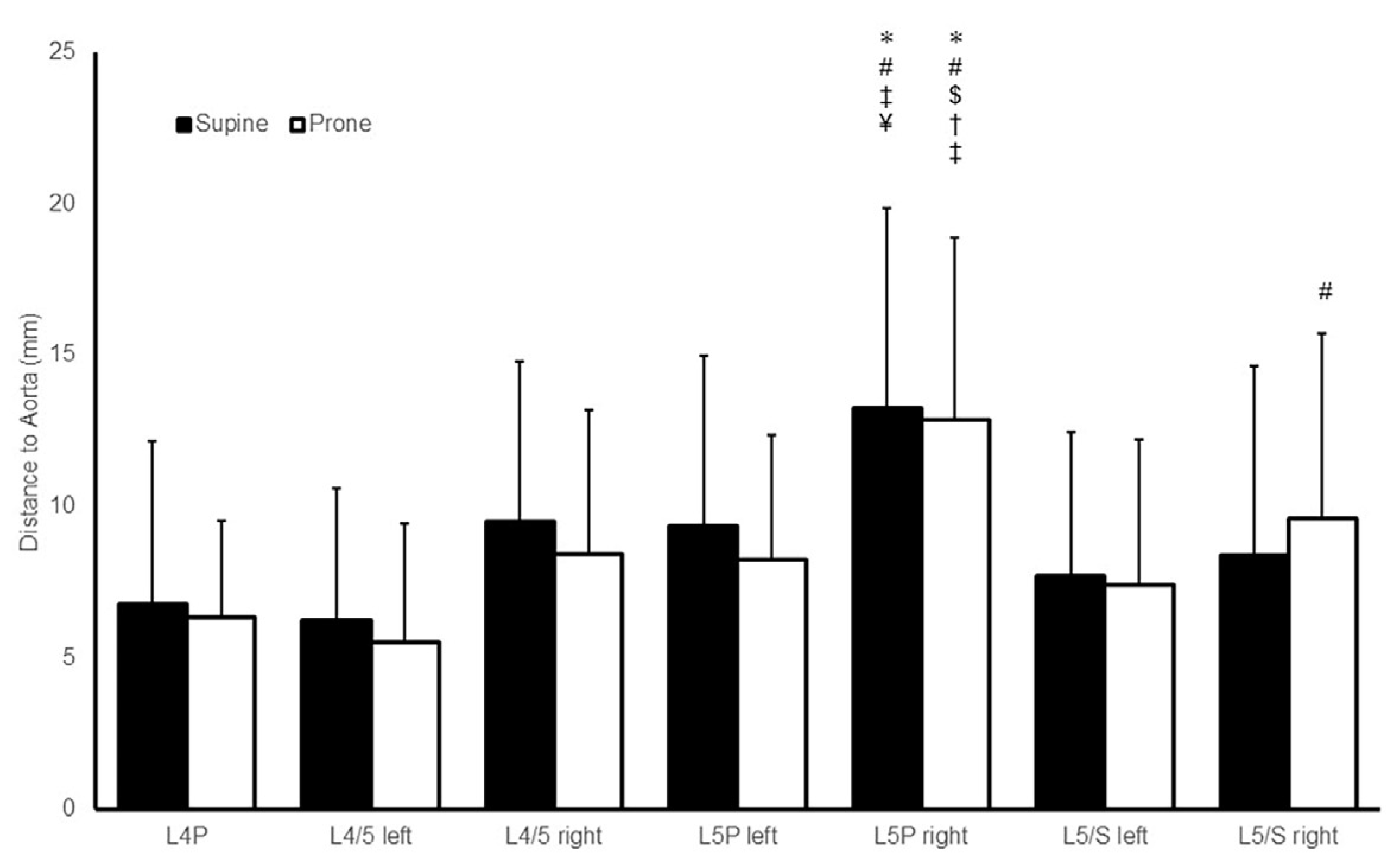
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Love, J. Removal of protruded intervertebral disc without laminectomy. Proc. Staff Meet Mayo Clin. 1939, 14, 800–805. [Google Scholar]
- Cloward, R.B. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J. Neurosurg. 1953, 10, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Wetzel, F.T.; Larocca, H. The failed posterior lumbar interbody fusion. Spine 1991, 16, 839–845. [Google Scholar] [CrossRef]
- Zhou, Z.J.; Xia, P.; Zhao, F.D.; Fang, X.Q.; Fan, S.W.; Zhang, J.F. Endplate injury as a risk factor for cage retropulsion following transforaminal lumbar interbody fusion: An analysis of 1052 cases. Medicine 2021, 100, e24005. [Google Scholar] [CrossRef] [PubMed]
- Tokuhashi, Y.; Ajiro, Y.; Umezawa, N. Subsidence of metal interbody cage after posterior lumbar interbody fusion with pedicle screw fixation. Orthopedics 2009, 32. [Google Scholar]
- Corniola, M.V.; Jägersberg, M.; Stienen, M.N.; Gautschi, O.P. Complete cage migration/subsidence into the adjacent vertebral body after posterior lumbar interbody fusion. J. Clin. Neurosci. 2015, 22, 597–598. [Google Scholar] [CrossRef]
- Okuyama, T.; Tagaya, N.; Sugamata, Y.; Hirano, K.; Saito, K.; Yamagata, Y.; Sameshima, S.; Noie, T.; Oya, M. Laparoscopic surgery to remove a cage that migrated to the retroperitoneal space during posterior lumbar interbody fusion: A case report. Asian J. Endosc. Surg. 2018, 11, 75–78. [Google Scholar] [CrossRef]
- Goodkin, R.; Laska, L.L. Vascular and visceral injuries associated with lumbar disc surgery: Medicolegal implications. Surg. Neurol. 1998, 49, 358–370; discussion 370. [Google Scholar] [CrossRef]
- Papadoulas, S.; Konstantinou, D.; Kourea, H.P.; Kritikos, N.; Haftouras, N.; Tsolakis, J.A. Vascular injury complicating lumbar disc surgery. A systematic review. Eur. J. Vasc. Endovasc. Surg. 2002, 24, 189–195. [Google Scholar] [CrossRef]
- Postacchini, R.; Cinotti, G.; Postacchini, F. Injury to major abdominal vessels during posterior lumbar interbody fusion. A case report and review of the literature. Spine J. 2013, 13, e7–e11. [Google Scholar] [CrossRef] [PubMed]
- Forbang, N.I.; Nguyen, T.; Ix, J.H.; Criqui, M.H.; Allison, M.A. The downward shift of the aortic bifurcation, a possible marker for vascular aging. J. Surg. Radiol. 2011, 2, 372–377. [Google Scholar]
- Rusconi, A.; Peron, S.; Roccucci, P.; Stefini, R. The internal carotid artery and the atlas: Anatomical relationship and implications for C1 lateral mass fixation. Surg. Radiol. Anat. 2021, 43, 87–92. [Google Scholar] [CrossRef]
- Yoshida, M.; Neo, M.; Fujibayashi, S.; Nakamura, T. Comparison of the anatomical risk for vertebral artery injury associated with the C2-pedicle screw and atlantoaxial transarticular screw. Spine 2006, 31, E513–E517. [Google Scholar] [CrossRef]
- Neo, M.; Fujibayashi, S.; Miyata, M.; Takemoto, M.; Nakamura, T. Vertebral artery injury during cervical spine surgery: A survey of more than 5600 operations. Spine 2008, 33, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Currier, B.L.; Maus, T.P.; Eck, J.C.; Larson, D.R.; Yaszemski, M.J. Relationship of the internal carotid artery to the anterior aspect of the C1 vertebra: Implications for C1-C2 transarticular and C1 lateral mass fixation. Spine 2008, 33, 635–639. [Google Scholar] [CrossRef] [PubMed]
- Vanden Bogaerde, M.V.; Viaene, P.; Thijs, V. Iatrogenic perforation of the internal carotid artery by a transarticular screw: An unusual case of repetitive ischemic stroke. Clin. Neurol. Neurosurg. 2007, 109, 466–469. [Google Scholar] [CrossRef] [PubMed]
- Tschoeke, S.K.; Gahr, P.; Krug, L.; Kasper, A.S.; Heyde, C.E.; Ertel, W. Late diagnosis of pedicle screw malplacement with perforation of the thoracic aorta after posterior stabilization in a patient with multiple myeloma: Case report. Spine 2011, 36, E886–E890. [Google Scholar] [CrossRef] [PubMed]
- Sevuk, U.; Mesut, A.; Kiraz, I.; Kose, K.; Ayaz, F.; Erkul, A. Delayed presentation of aortic injury by a thoracic pedicle screw. J. Card. Surg. 2016, 31, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Mani, K.; Rantatalo, M.; Bjurholm, A.; Thelin, S.; Eriksson, L.G.; Wanhainen, A. Aortic rupture after spinal correction for scoliosis in the presence of a thoracic stent graft. J. Vasc. Surg. 2010, 52, 1653–1657. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Plataniotis, N.; Evangelopoulos, D.S.; Katzouraki, G.; Pneumaticos, S. The effect of patient positioning on the relative position of the aorta to the thoracic spine. Eur. Spine J. 2019, 28, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, C.; Petrus, L.; Ross, I.B. Regarding the possibility of anterior vascular injury from the posterior approach to the lumbar disc space: An anatomical study. Spine 2012, 37, E1371–E1375. [Google Scholar] [CrossRef] [PubMed]
- Ni, L.; Fan, Y.; Bian, J.; Deng, X.; Ma, Y. Effect of body mass on oxygenation and intra-abdominal pressure when using a Jackson surgical table in the prone position during lumbar surgery. Spine 2018, 43, 965–970. [Google Scholar] [CrossRef] [PubMed]
| Total | Calcification (−) | Calcification (+) | p-Value | |
|---|---|---|---|---|
| Sample number | 30 | 11 | 19 | |
| Age | 65.3 ± 10.0 | 58.2 ± 7.9 | 69.5 ± 8.8 | 0.002 |
| Female | 20 (66.7%) | 10 (90.9%) | 10 (52.6%) | 0.049 |
| Height | 155.9 ± 7.8 | 154.7 ± 5.2 | 156.7 ± 9.1 | 0.672 |
| Body weight | 65.1 ± 11.7 | 69.5 ± 10.0 | 62.6 ± 12.2 | 0.103 |
| Body mass index | 26.7 ± 4.1 | 29.0 ± 3.8 | 25.4 ± 3.9 | 0.016 |
| Calcification (−) | Calcification (+) | |||||||
|---|---|---|---|---|---|---|---|---|
| Supine | Prone | p-Value | AAT | Supine | Prone | p-Value | AAT | |
| L4P | 7.5 ± 8.4 | 5.5 ± 3.8 | 0.248 | −2.0 ± 5.3 | 6.4 ± 2.6 | 6.8 ± 2.7 | 0.355 | 0.4 ± 1.8 |
| L4/5 left | 4.9 ± 5.0 | 5.2 ± 4.9 | 0.248 | 0.3 ± 2.4 | 7.0 ± 4.0 | 5.7 ± 3.5 | 0.334 | −1.3 ± 3.5 |
| L4/5 right | 9.7 ± 6.0 | 9.3 ± 5.2 | 0.799 | −0.4 ± 1.9 | 9.4 ± 5.0 | 8.0 ± 4.6 | 0.133 | −1.4 ± 3.7 |
| L5P left | 7.7 ± 7.4 | 6.4 ± 3.7 | 0.929 | −1.3 ± 5.7 | 10.3 ± 4.3 | 9.3 ± 4.1 | 0.107 | −1.0 ± 3.7 |
| L5P right | 11.5 ± 7.1 | 10.7 ± 5.6 | 0.657 | −0.8 ± 7.0 | 14.3 ± 6.2 | 14.2 ± 5.9 | 0.601 | −0.1 ± 4.3 |
| L5/S left | 5.7 ± 3.5 | 7.5 ± 6.2 | 0.248 | 1.7 ± 4.1 | 8.8 ± 5.1 | 7.4 ± 3.9 | 0.159 | −1.4 ± 3.8 |
| L5/S right | 7.6 ± 5.7 | 8.5 ± 5.3 | 0.213 | 1.0 ± 3.1 | 8.9 ± 6.7 | 10.3 ± 6.5 | 0.445 | 1.4 ± 6.5 |
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Supine | Prone | p-Value | Supine | Prone | p-Value | |
| L4P | 7.9 ± 2.6 | 8.0 ± 2.6 | 0.799 | 6.2 ± 6.3 | 5.5 ± 3.2 | 0.940 |
| L4/5 left | 8.0 ± 4.4 | 6.8 ± 3.8 | 0.646 | 5.3 ± 4.2 | 4.9 ± 4.0 | 0.940 |
| L4/5 right | 11.0 ± 5.0 | 9.4 ± 4.8 | 0.203 | 8.7 ± 5.4 | 7.9 ± 4.8 | 0.231 |
| L5P left | 10.3 ± 5.7 | 10.0 ± 4.8 | 0.878 | 8.9 ± 5.7 | 7.4 ± 3.6 | 0.156 |
| L5P right | 15.7 ± 7.4 | 17.3 ± 6.1 | 0.575 | 12.0 ± 5.9 | 10.7 ± 4.7 | 0.502 |
| L5/S left | 8.6 ± 6.4 | 5.6 ± 3.4 | 0.037 | 7.2 ± 3.8 | 8.3 ± 5.2 | 0.145 |
| L5/S right | 10.0 ± 8.3 | 12.0 ± 7.7 | 0.575 | 7.6 ± 5.0 | 8.4 ± 4.9 | 0.332 |
| Calcification of Aorta At | β | p-Value | R2 |
|---|---|---|---|
| L4P | 0.215 | 0.379 | 0.109 |
| L4/5 left | −0.521 | 0.026 | 0.325 |
| L4/5 right | −0.156 | 0.548 | 0.072 |
| L5P left | −0.247 | 0.281 | 0.232 |
| L5P right | −0.29 | 0.157 | 0.397 |
| L5/S left | −0.253 | 0.203 | 0.426 |
| L5/S right | −0.020 | 0.933 | 0.172 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asari, T.; Wada, K.; Sasaki, E.; Kumagai, G.; Tanaka, S.; Ishibashi, Y. Abdominal Arterial Translation in Lower Lumbar Spine Level Due to Positional Change: A Clinical Survey Using Intraoperative Computed Tomography. J. Clin. Med. 2024, 13, 1897. https://doi.org/10.3390/jcm13071897
Asari T, Wada K, Sasaki E, Kumagai G, Tanaka S, Ishibashi Y. Abdominal Arterial Translation in Lower Lumbar Spine Level Due to Positional Change: A Clinical Survey Using Intraoperative Computed Tomography. Journal of Clinical Medicine. 2024; 13(7):1897. https://doi.org/10.3390/jcm13071897
Chicago/Turabian StyleAsari, Toru, Kanichiro Wada, Eiji Sasaki, Gentaro Kumagai, Sunao Tanaka, and Yasuyuki Ishibashi. 2024. "Abdominal Arterial Translation in Lower Lumbar Spine Level Due to Positional Change: A Clinical Survey Using Intraoperative Computed Tomography" Journal of Clinical Medicine 13, no. 7: 1897. https://doi.org/10.3390/jcm13071897
APA StyleAsari, T., Wada, K., Sasaki, E., Kumagai, G., Tanaka, S., & Ishibashi, Y. (2024). Abdominal Arterial Translation in Lower Lumbar Spine Level Due to Positional Change: A Clinical Survey Using Intraoperative Computed Tomography. Journal of Clinical Medicine, 13(7), 1897. https://doi.org/10.3390/jcm13071897






