Sagittal Balance Parameters and Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Selection Criteria
2.3. Quality Assessment
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
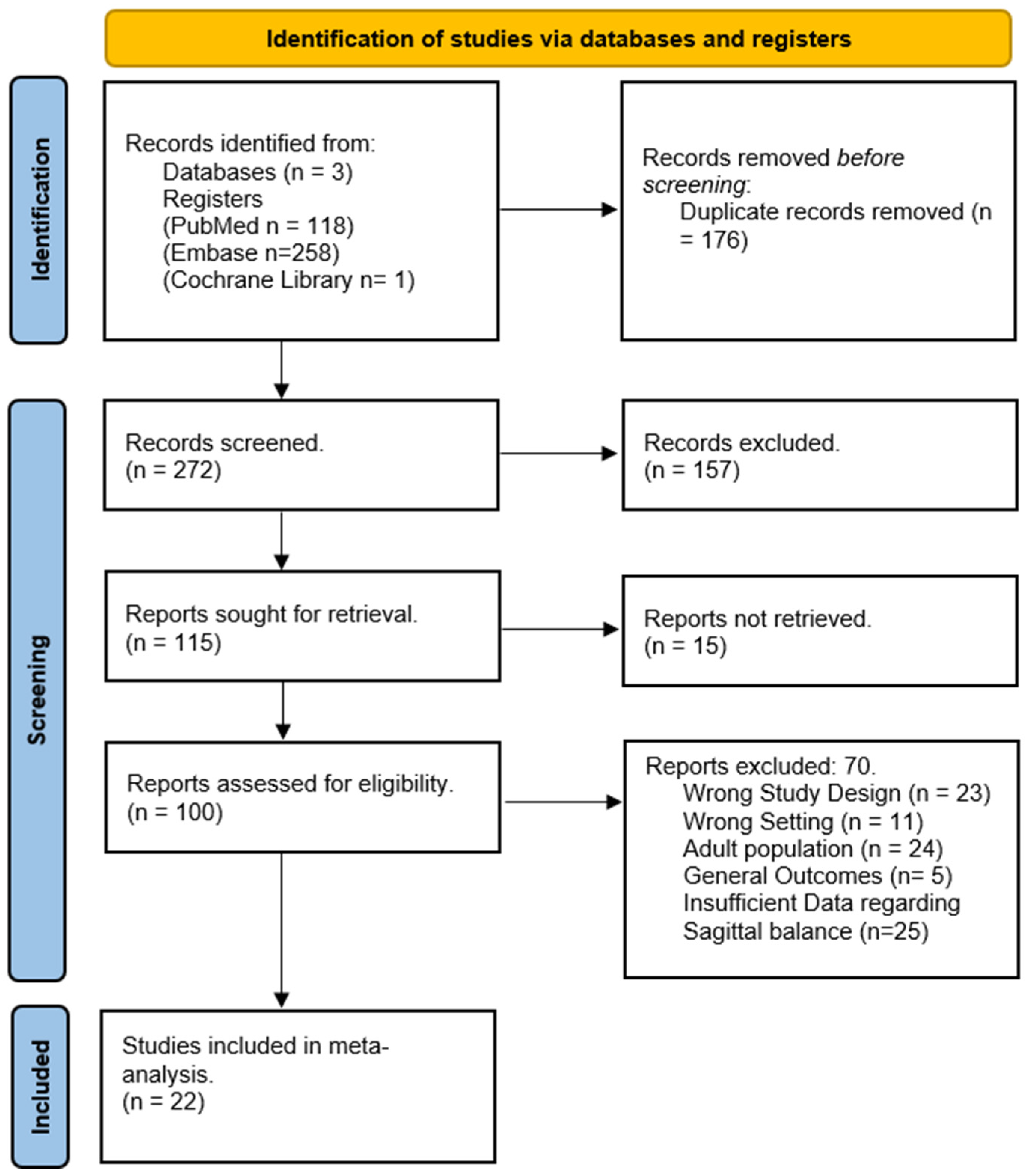
3.1. Literature Search Results
3.2. Demographic Characteristics
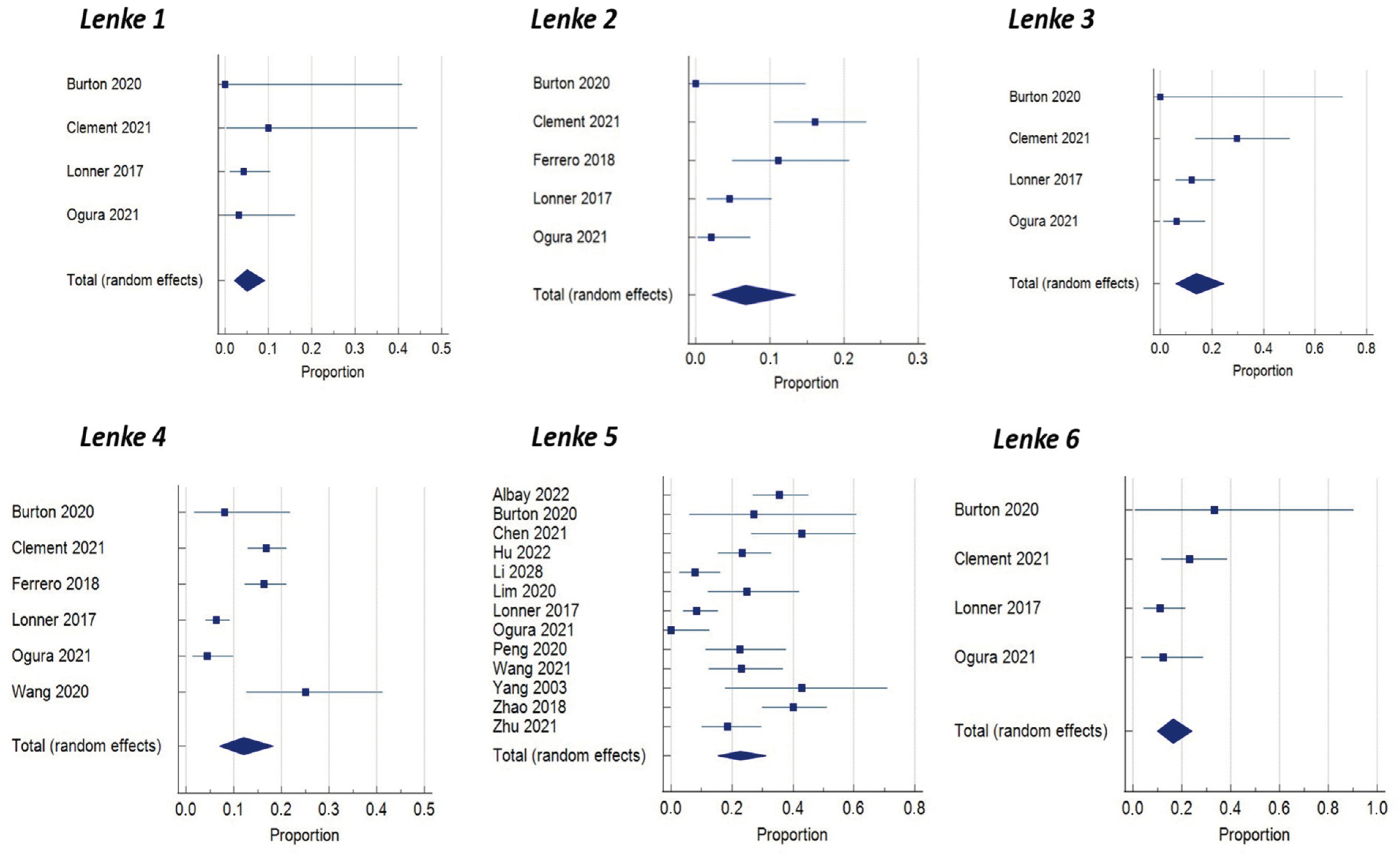
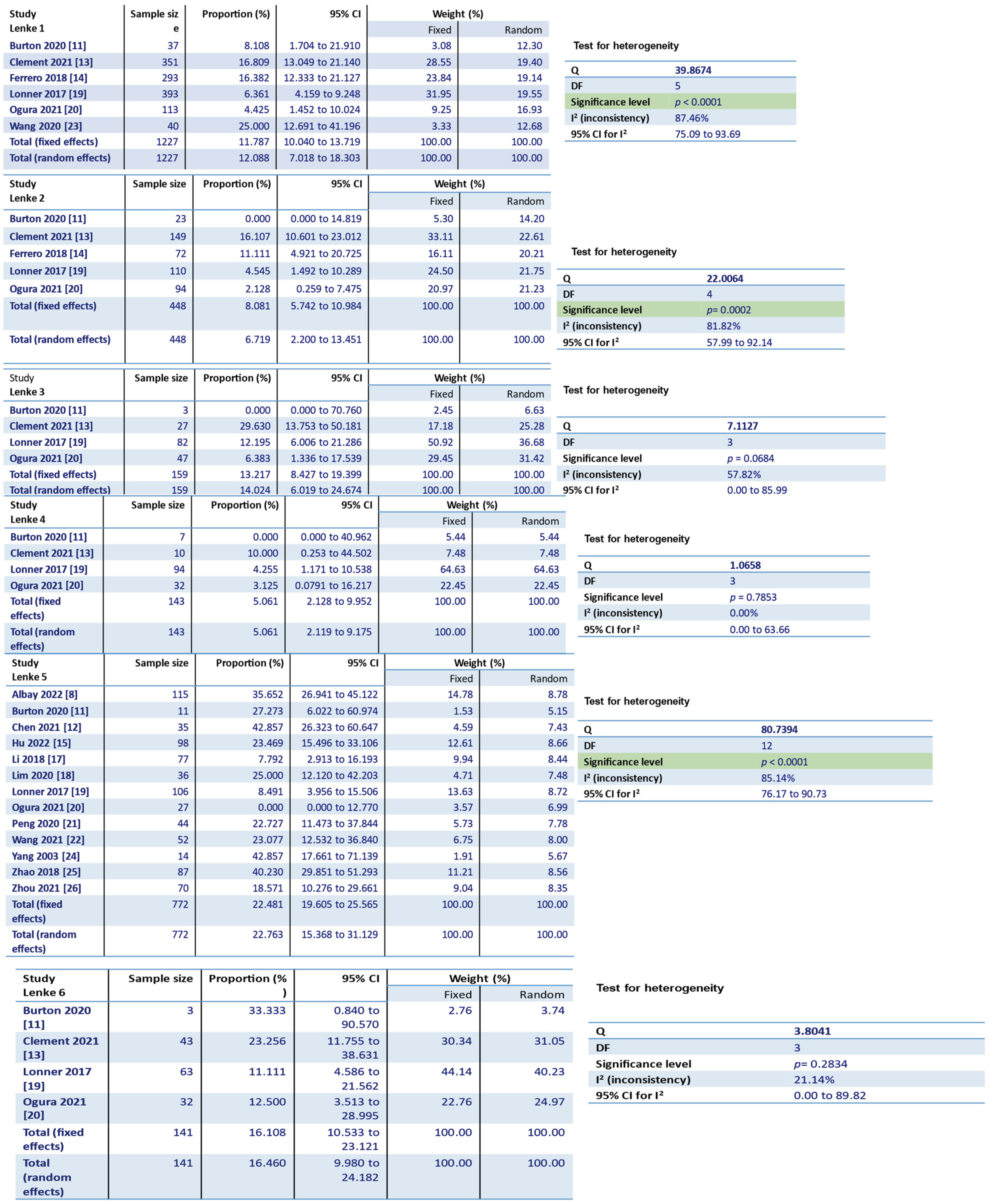
Lenke Classification
3.3. Pre-Operative Sagittal Balance Parameters
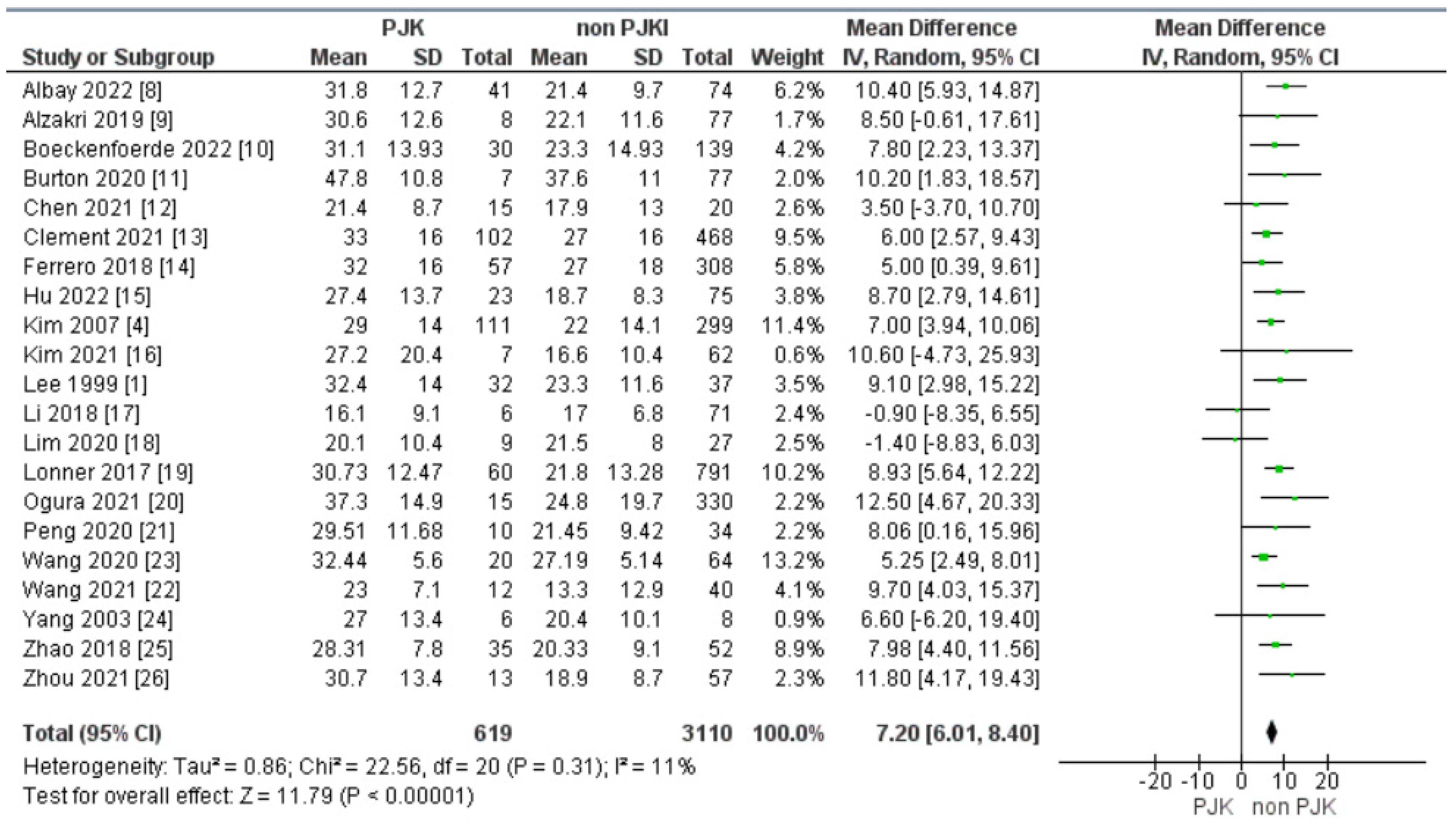
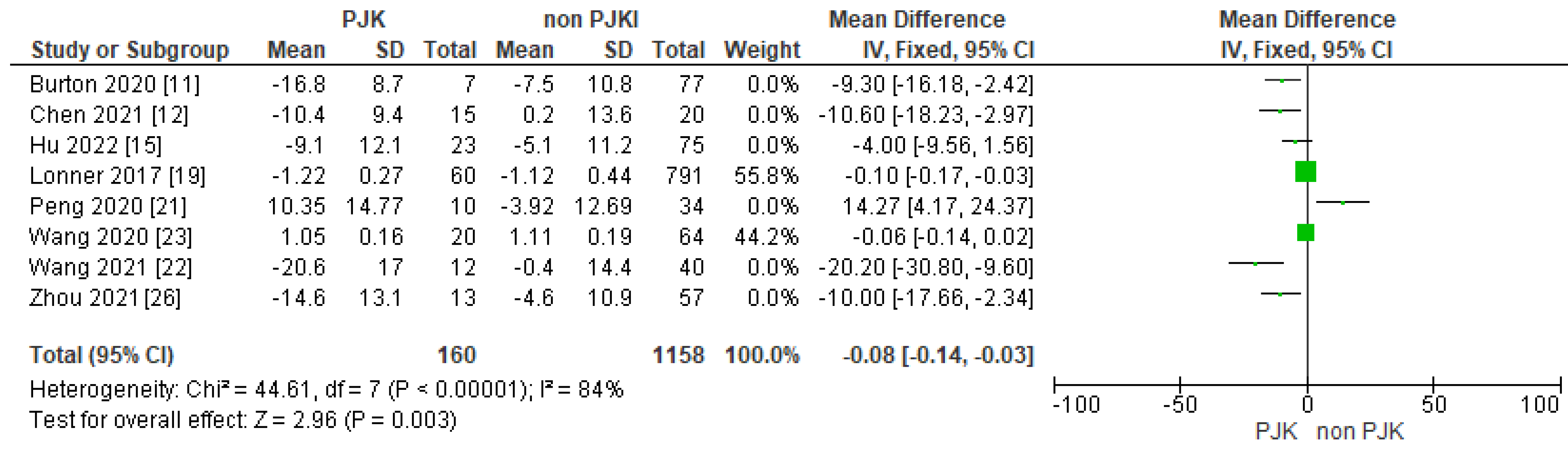
3.3.1. Pre-Operative Thoracic Kyphosis
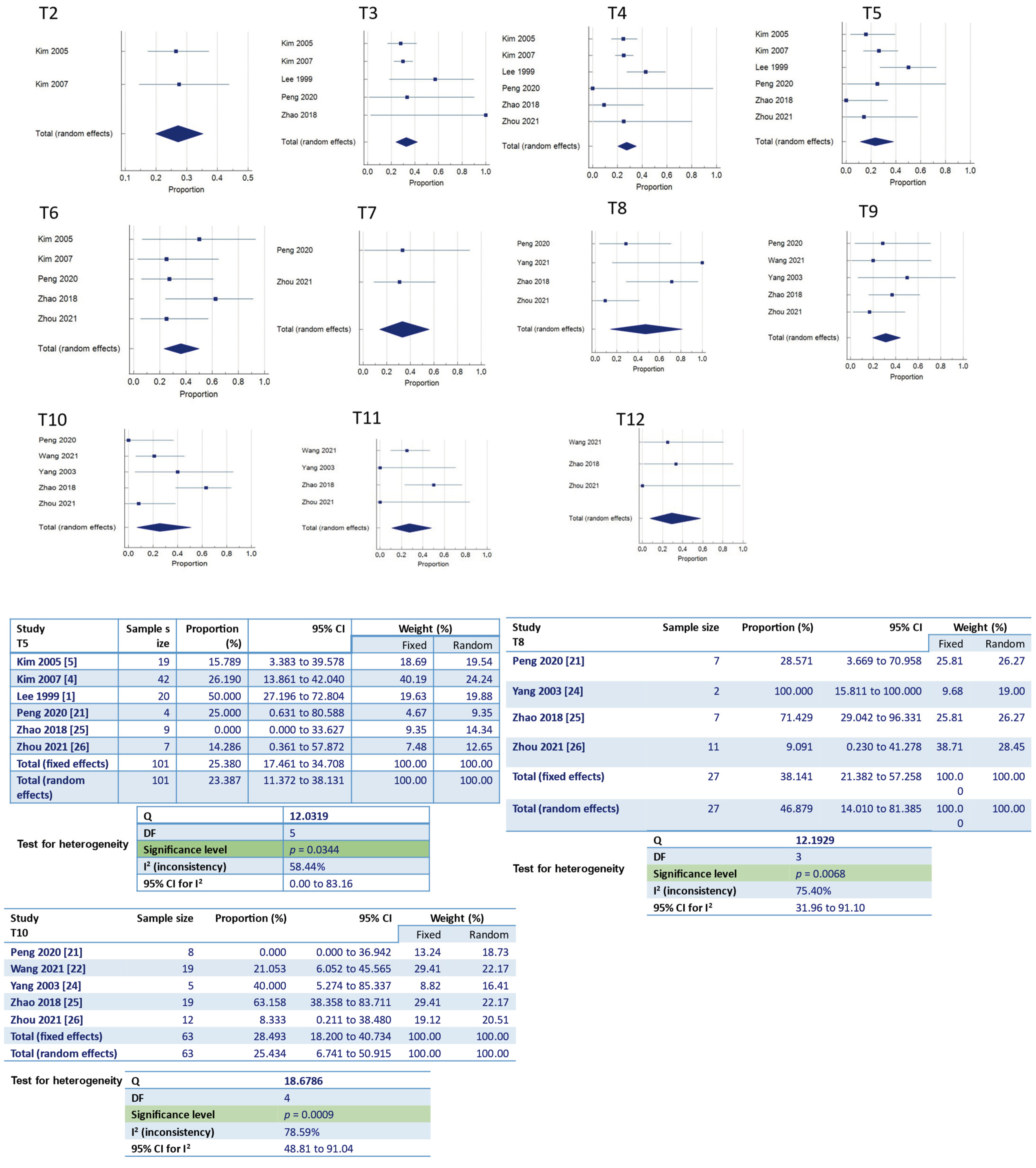
3.3.2. Pre-Operative Lumbar Lordosis
3.3.3. Pre-Operative SVA and PI/LL
3.4. Post-Operative Sagittal Balance Parameters
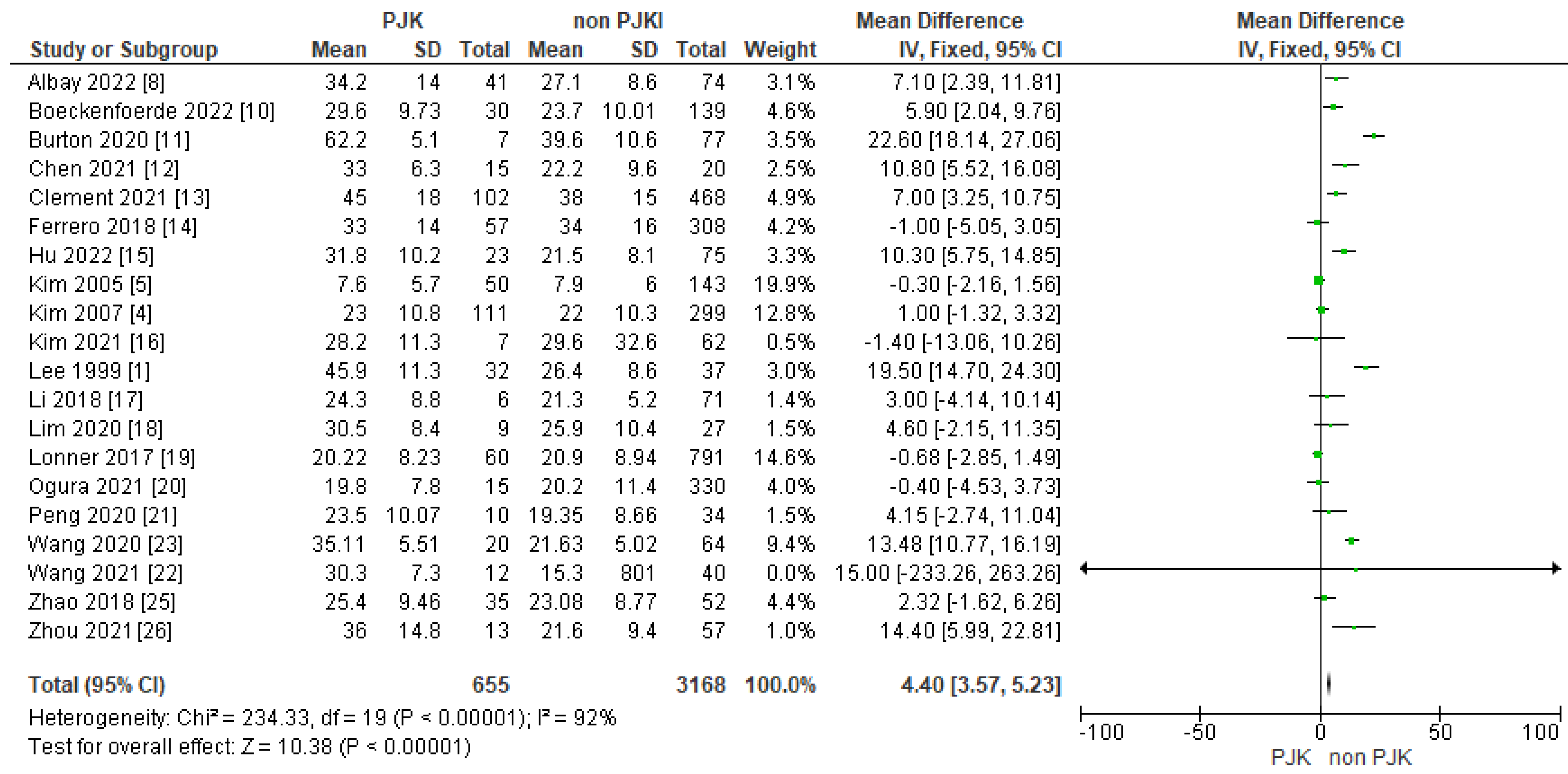
3.4.1. Post-Operative Thoracic Kyphosis
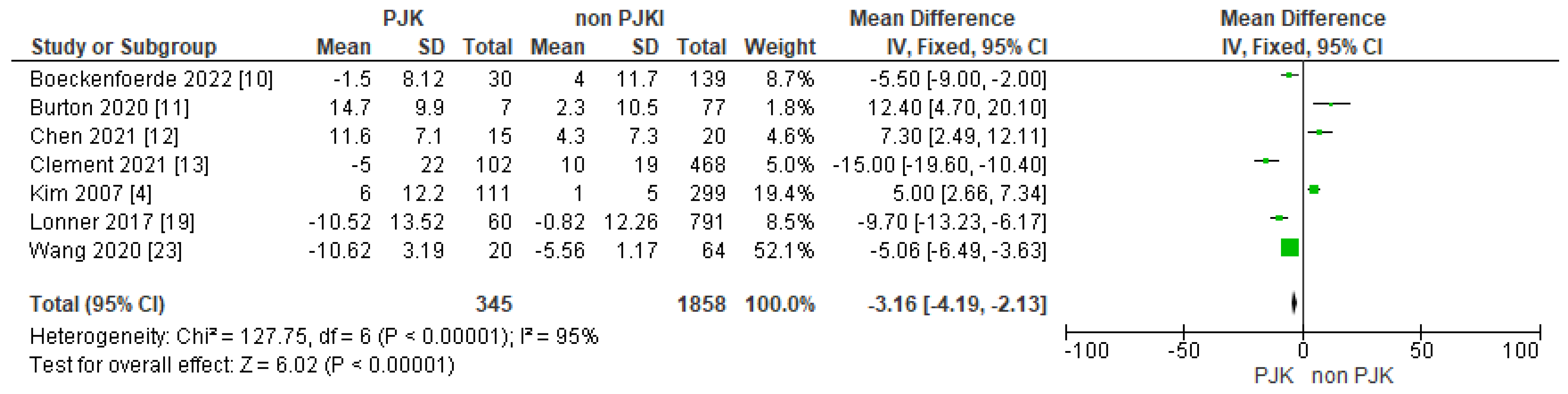
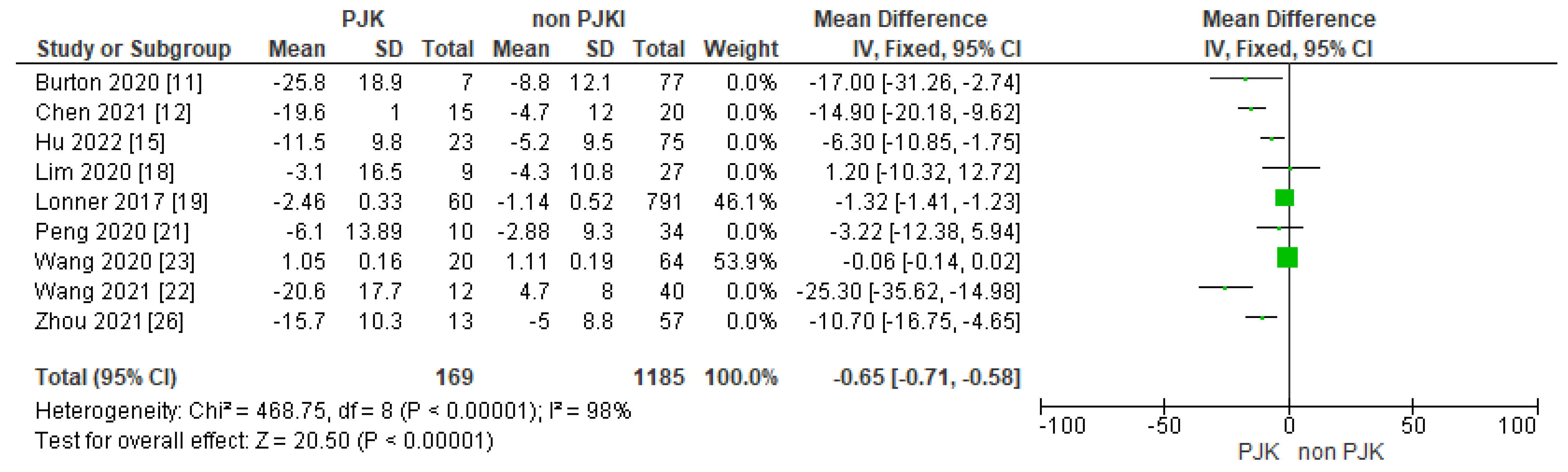
3.4.2. Thoracic Kyphosis Change
3.4.3. Post-Operative Lumbar Lordosis (Post-Op. LL)
3.4.4. Post-Operative SVA, PI and PI/LL
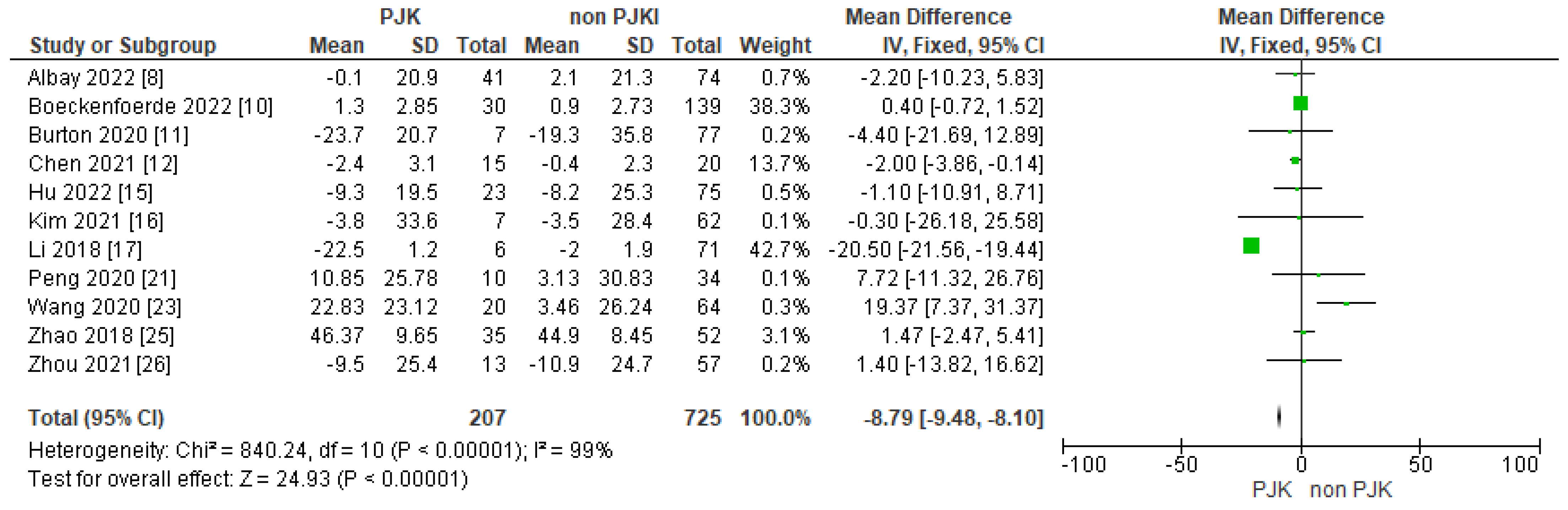
3.4.5. Post-Operative Proximal Junctional Angle/Rod Contour Angle (PJA/RCA)
3.5. Peri-Operative Factors
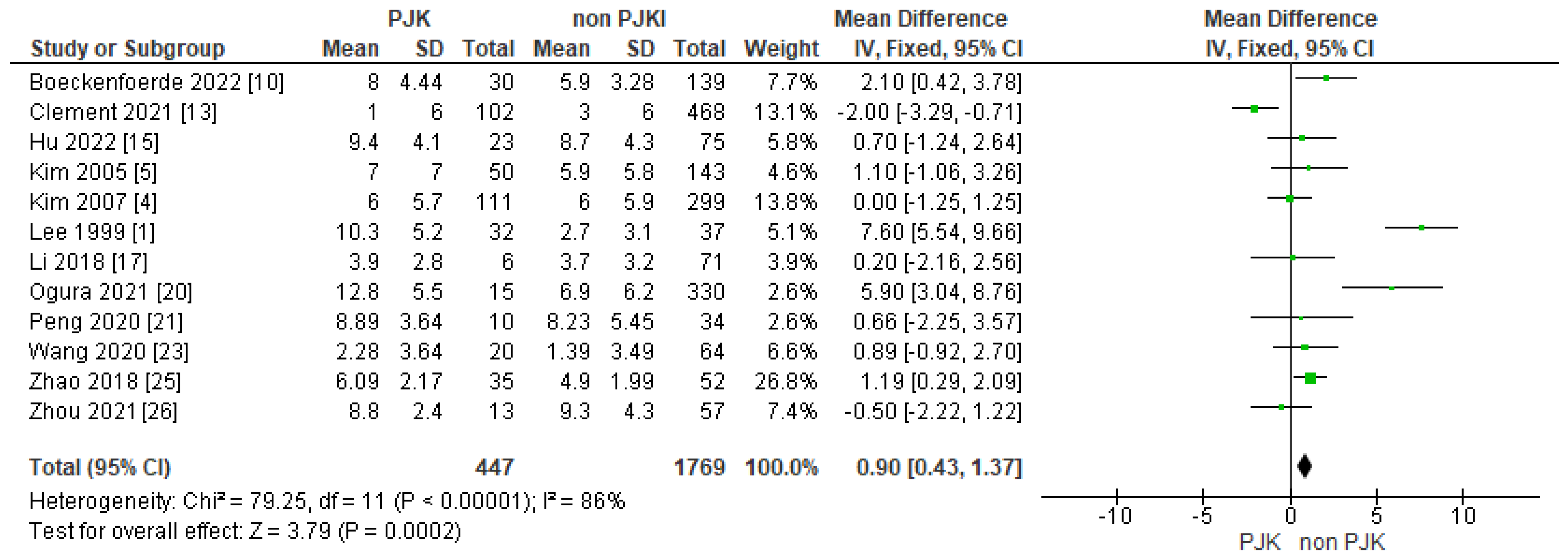
Upper Instrumented Vertebra (UIV)
4. Discussion
4.1. Incidence
4.2. Risk Factors
4.2.1. Lenke Classification
4.2.2. Pre-Operative Parameters in Sagittal Balance
Pre-Operative Thoracic Kyphosis
Pre-Operative Lumbar Lordosis, SVA and PI/LL
4.2.3. Post-Operative Sagittal Parameters
Post-Operative Thoracic Kyphosis and Change in Kyphotic Angle
Post-Operative Lumbar Lordosis, SVA and PI/LL Mismatch
Post-Operative PJA-RCA and Rod Contour Angle
Upper Instrumented Vertebra (UIV)
Minimizing the Risk of PJK in AIS: Clinical Suggestions
- Careful pre-operative planning is needed when AIS correction is considered. Measuring the pre-operative thoracic kyphosis, lumbar lordosis, SVA and PI/LL mismatch are valuable to plan and achieve the optimal sagittal alignment for each patient postoperatively. Patient-specific thoracic kyphosis (“PSTK = 2(PT + LL − PI)”) tends to be the target postoperative thoracic kyphosis after AIS correction. The extent of instrumentation, the surgical approach, the UIV and the rod contour is suggested to be decided in line with the PSTK.
- Careful selection of fusion levels, type of instrumentation especially at the upper end of the construct, surgical technique and sparing of the spinous processes, their posterior ligaments and posterior facet capsules of the upper instrumented levels (UIV, UIV + 1) could add to diminish the prevalence of PJK after AIS correction.
- Rod contouring is crucial to minimize the risk of PJK. The maintenance of an individual’s coronal and sagittal spinal alignment post-operatively is the key for avoidance of PJK.
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, G.A.; Betz, R.R.; Clements, D.H., 3rd; Huss, G.K. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine 1999, 24, 795–799. [Google Scholar] [CrossRef]
- Glattes, R.C.; Bridwell, K.H.; Lenke, L.G.; Kim, Y.J.; Rinella, A.; Edwards, C., 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine 2005, 30, 1643–1649. [Google Scholar] [CrossRef]
- Helgeson, M.D.; Shah, S.A.; Newton, P.O.; Clements, D.H., 3rd; Betz, R.R.; Marks, M.C.; Bastrom, T.; Harms Study, G. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 2010, 35, 177–181. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lenke, L.G.; Bridwell, K.H.; Kim, J.; Cho, S.K.; Cheh, G.; Yoon, J. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: Incidence and risk factor analysis of 410 cases. Spine 2007, 32, 2731–2738. [Google Scholar] [CrossRef]
- Kim, Y.J.; Bridwell, K.H.; Lenke, L.G.; Kim, J.; Cho, S.K. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: Minimum 5-year follow-up. Spine 2005, 30, 2045–2050. [Google Scholar] [CrossRef]
- Rhee, J.M.; Bridwell, K.H.; Won, D.S.; Lenke, L.G.; Chotigavanichaya, C.; Hanson, D.S. Sagittal plane analysis of adolescent idiopathic scoliosis: The effect of anterior versus posterior instrumentation. Spine 2002, 27, 2350–2356. [Google Scholar] [CrossRef]
- Wang, J.; Zhao, Y.; Shen, B.; Wang, C.; Li, M. Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury 2010, 41, 415–420. [Google Scholar] [CrossRef]
- Albay, C.; Kaygusuz, M.A.; Kargin, D.; Oner, A. Correlations of proximal junctional kyphosis with radiographic measurements, spinopelvic parameters, and health-related quality of life in Lenke type V adolescent idiopathic scoliosis. Jt. Dis. Relat. Surg. 2022, 33, 162–171. [Google Scholar] [CrossRef]
- Alzakri, A.; Vergari, C.; Van den Abbeele, M.; Gille, O.; Skalli, W.; Obeid, I. Global Sagittal Alignment and Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis. Spine Deform. 2019, 7, 236–244. [Google Scholar] [CrossRef]
- Boeckenfoerde, K.; Schulze Boevingloh, A.; Gosheger, G.; Bockholt, S.; Lampe, L.P.; Lange, T. Risk Factors of Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis-The Spinous Processes and Proximal Rod Contouring. J. Clin. Med. 2022, 11, 6098. [Google Scholar] [CrossRef]
- Burton, D.A.; Karkenny, A.J.; Schulz, J.F.; Hanstein, R.; Gomez, J.A. Sagittal spinopelvic changes after posterior spinal fusion in adolescent idiopathic scoliosis. J. Child. Orthop. 2020, 14, 544–553. [Google Scholar] [CrossRef]
- Chen, J.; Fan, H.; Sui, W.; Yang, J.; Deng, Y.; Huang, Z.; Yang, J. Risk and Predictive Factors for Proximal Junctional Kyphosis in Patients Treated by Lenke Type 5 Adolescent Idiopathic Scoliosis Correction. World Neurosurg. 2021, 147, e315–e323. [Google Scholar] [CrossRef]
- Clement, J.L.; Pesenti, S.; Ilharreborde, B.; Morin, C.; Charles, Y.P.; Parent, H.F.; Violas, P.; Szadkowski, M.; Boissiere, L.; Solla, F. Proximal junctional kyphosis is a rebalancing spinal phenomenon due to insufficient postoperative thoracic kyphosis after adolescent idiopathic scoliosis surgery. Eur. Spine J. 2021, 30, 1988–1997. [Google Scholar] [CrossRef]
- Ferrero, E.; Bocahut, N.; Lefevre, Y.; Roussouly, P.; Pesenti, S.; Lakhal, W.; Odent, T.; Morin, C.; Clement, J.L.; Compagnon, R.; et al. Proximal junctional kyphosis in thoracic adolescent idiopathic scoliosis: Risk factors and compensatory mechanisms in a multicenter national cohort. Eur. Spine J. 2018, 27, 2241–2250. [Google Scholar] [CrossRef]
- Hu, B.; Wang, L.; Song, Y.; Yang, X.; Liu, L.; Zhou, C. Postoperative proximal junctional kyphosis correlated with thoracic inlet angle in Lenke 5c adolescent idiopathic scoliosis patients following posterior surgery. BMC Musculoskelet. Disord. 2022, 23, 919. [Google Scholar] [CrossRef]
- Kim, H.J.; Yang, J.H.; Chang, D.G.; Suk, S.I.; Suh, S.W.; Kim, J.S.; Kim, S.I.; Song, K.S.; Cho, W. Incidence and Radiological Risk Factors of Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis Following Pedicle Screw Instrumentation with Rod Derotation and Direct Vertebral Rotation: A Minimum 5-Year Follow-Up Study. J. Clin. Med. 2021, 10, 5351. [Google Scholar] [CrossRef]
- Li, J.; Zhao, Z.; Tseng, C.; Zhu, Z.; Qiu, Y.; Liu, Z. Selective Fusion in Lenke 5 Adolescent Idiopathic Scoliosis. World Neurosurg. 2018, 118, e784–e791. [Google Scholar] [CrossRef]
- Lim, J.L.; Hey, H.W.D.; Kumar, N.; Teo, A.Q.A.; Lau, L.L.; Hee, H.T.; Ruiz, J.N.; Kumar, N.S.; Thambiah, J.S.; Liu, G.K.; et al. A 10-Year Radiographic Study Comparing Anterior Versus Posterior Instrumented Spinal Fusion in Patients with Lenke Type 5 Adolescent Idiopathic Scoliosis. Spine 2020, 45, 612–620. [Google Scholar] [CrossRef]
- Lonner, B.S.; Ren, Y.; Newton, P.O.; Shah, S.A.; Samdani, A.F.; Shufflebarger, H.L.; Asghar, J.; Sponseller, P.; Betz, R.R.; Yaszay, B. Risk Factors of Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis-The Pelvis and Other Considerations. Spine Deform. 2017, 5, 181–188. [Google Scholar] [CrossRef]
- Ogura, Y.; Glassman, S.D.; Sucato, D.; Hresko, M.T.; Carreon, L.Y. Incidence of Proximal Junctional Kyphosis with Pedicle Screws at Upper Instrumented Vertebrae in Posterior Spinal Fusion for Adolescent Idiopathic Scoliosis. Glob. Spine J. 2021, 11, 1019–1024. [Google Scholar] [CrossRef]
- Peng, L.; Lan, L.; Xiu, P.; Zhang, G.; Hu, B.; Yang, X.; Song, Y.; Yang, X.; Gu, Y.; Yang, R.; et al. Prediction of Proximal Junctional Kyphosis After Posterior Scoliosis Surgery with Machine Learning in the Lenke 5 Adolescent Idiopathic Scoliosis Patient. Front. Bioeng. Biotechnol. 2020, 8, 559387. [Google Scholar] [CrossRef]
- Wang, G.; Li, Y.; Liu, P.; Sun, J. Pelvic incidence correlates to sagittal spinal morphology in lenke 5 adolescent idiopathic scoliosis and influences the proximal junctional kyphosis rate after correction surgery. Eur. Spine J. 2021, 30, 2457–2466. [Google Scholar] [CrossRef]
- Wang, J.; Yang, N.; Luo, M.; Xia, L.; Li, N. Large Difference between Proximal Junctional Angle and Rod Contouring Angle is a Risk Factor for Proximal Junctional Kyphosis. World Neurosurg. 2020, 136, e683–e689. [Google Scholar] [CrossRef]
- Yang, S.H.; Chen, P.Q. Proximal kyphosis after short posterior fusion for thoracolumbar scoliosis. Clin. Orthop. Relat. Res. 2003, 411, 152–158. [Google Scholar] [CrossRef]
- Zhao, J.; Yang, M.; Yang, Y.; Chen, Z.; Li, M. Proximal junctional kyphosis following correction surgery in the Lenke 5 adolescent idiopathic scoliosis patient. J. Orthop. Sci. 2018, 23, 744–749. [Google Scholar] [CrossRef]
- Zhou, Q.; Hu, B.; Yang, X.; Song, Y.; Liu, L.; Wang, L.; Wang, L.; Zhou, C.; Zhou, Z.; Xiu, P.; et al. Proximal junctional kyphosis in Lenke 5 AIS patients: The important factor of pelvic incidence. BMC Musculoskelet. Disord. 2021, 22, 185. [Google Scholar] [CrossRef]
- Zou, L.; Liu, J.; Lu, H. Characteristics and risk factors for proximal junctional kyphosis in adult spinal deformity after correction surgery: A systematic review and meta-analysis. Neurosurg. Rev. 2019, 42, 671–682. [Google Scholar] [CrossRef]
- Luhmann, S.J.; Roth, J.; DeFreitas, D.; McCormick, S. The impact of segmental spinal alignment on the development of proximal junctional kyphosis after instrumented posterior spinal fusions for idiopathic scoliosis. Spine Deform. 2022, 10, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Cao, K.; Wang, B.; Li, H.; Zhou, X.; Xu, X.; Lin, N.; Liu, Q.; Lu, H. Incidence and Risk Factors for Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis After Correction Surgery: A Meta-Analysis. World Neurosurg. 2019, 125, e326–e335. [Google Scholar] [CrossRef] [PubMed]
- Ilharreborde, B. Sagittal balance and idiopathic scoliosis: Does final sagittal alignment influence outcomes, degeneration rate or failure rate? Eur. Spine J. 2018, 27, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.L.; Dolan, L.A.; Cheng, J.C.; Danielsson, A.; Morcuende, J.A. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- Erkilinc, M.; Baldwin, K.D.; Pasha, S.; Mistovich, R.J. Proximal junctional kyphosis in pediatric spinal deformity surgery: A systematic review and critical analysis. Spine Deform. 2022, 10, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Maruo, K.; Ha, Y.; Inoue, S.; Samuel, S.; Okada, E.; Hu, S.S.; Deviren, V.; Burch, S.; William, S.; Ames, C.P.; et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine 2013, 38, E1469–E1476. [Google Scholar] [CrossRef] [PubMed]
- Solla, F.; Ilharreborde, B.; Blondel, B.; Prost, S.; Bauduin, E.; Laouissat, F.; Riouallon, G.; Wolff, S.; Challier, V.; Obeid, I.; et al. Can Lumbopelvic Parameters Be Used to Predict Thoracic Kyphosis at All Ages? A National Cross-Sectional Study. Glob. Spine J. 2022, 21925682221134040. [Google Scholar] [CrossRef]
- Rothenfluh, D.A.; Stratton, A.; Nnadi, C.; Beresford-Cleary, N. A Critical Thoracic Kyphosis Is Required to Prevent Sagittal Plane Deterioration in Selective Thoracic Fusions in Lenke I and II AIS. Eur. Spine J. 2019, 28, 3066–3075. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Qiu, G.; Zhao, Y.; Guo, S.; Wang, Y.; Zhang, J.; Shen, J. Risk factors of proximal junctional angle increase after selective posterior thoracolumbar/lumbar fusion in patients with adolescent idiopathic scoliosis. Eur. Spine J. 2015, 24, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Ohrt-Nissen, S.; Bari, T.; Dahl, B.; Gehrchen, M. Sagittal Alignment After Surgical Treatment of Adolescent Idiopathic Scoliosis-Application of the Roussouly Classification. Spine Deform. 2018, 6, 537–544. [Google Scholar] [CrossRef]
- Angelliaume, A.; Ferrero, E.; Mazda, K.; Le Hanneur, M.; Accabled, F.; de Gauzy, J.S.; Ilharreborde, B. Titanium vs cobalt chromium: What is the best rod material to enhance adolescent idiopathic scoliosis correction with sublaminar bands? Eur. Spine J. 2017, 26, 1732–1738. [Google Scholar] [CrossRef]
- Cammarata, M.; Aubin, C.E.; Wang, X.; Mac-Thiong, J.M. Biomechanical risk factors for proximal junctional kyphosis: A detailed numerical analysis of surgical instrumentation variables. Spine 2014, 39, E500–E507. [Google Scholar] [CrossRef]
- Thawrani, D.P.; Glos, D.L.; Coombs, M.T.; Bylski-Austrow, D.I.; Sturm, P.F. Transverse process hooks at upper instrumented vertebra provide more gradual motion transition than pedicle screws. Spine 2014, 39, E826–E832. [Google Scholar] [CrossRef]
- Pahys, J.M.; Vivas, A.C.; Samdani, A.F.; Cunn, G.; Betz, R.R.; Newton, P.O.; Cahill, P.J. Assessment of proximal junctional kyphosis and shoulder balance with proximal screws versus hooks in posterior spinal fusion for adolescent idiopathic scoliosis. Spine 2018, 43, E1322–E1328. [Google Scholar] [CrossRef] [PubMed]




| Study | Country | Patients | Male | Female | Age | Surgical_Intervention | PJK | Non_PJK | FU |
|---|---|---|---|---|---|---|---|---|---|
| Albay 2022 [8] | Turkey | 115 | 17 | 98 | 14.6 | Posterior Instrumented Fusion | 41 | 74 | 24 m |
| Alzakri 2019 [9] | France | 85 | 10 | 75 | 15.6 | Posterior Instrumented Fusion | 8 | 77 | Min 24 m |
| Boeckenfoerde 2022 [10] | Germany | 169 | 21 | 148 | 14.7 | Posterior Instrumented Fusion with Screws | 30 | 139 | 27 m |
| Burton 2020 [11] | USA | 84 | 26 | 58 | 15 | Posterior Instrumented Fusion with Screws | 7 | 77 | Min 34 m |
| Chen 2021 [12] | China | 35 | 5 | 30 | 15.7 | Posterior Instrumented Fusion with Screws | 15 | 20 | Min 24 m |
| Clement 2021 [13] | France | 570 | 88 | 482 | 15 | Various | 102 | 468 | 49 m |
| Ferrero 2018 [14] | France | 365 | 53 | 312 | 15 | Posterior Instrumented Fusion with Screws | 57 | 308 | Min 24 m |
| Hu 2022 [15] | China | 98 | 21 | 77 | 15.6 | Posterior Instrumented Fusion | 23 | 75 | 24 m |
| Kim 2007 [4] | USA | 410 | 73 | 337 | 14.7 | Posterior Instrumented Fusion | 111 | 299 | 24 m |
| Kim 2021 [16] | Korea | 69 | 7 | 62 | 14.2 | Posterior Instrumented Fusion | 7 | 62 | Min 60 m |
| Lee 1999 [1] | USA | 69 | 8 | 61 | 14.5 | Posterior Instrumented Fusion | 32 | 37 | Min 24 m |
| Li 2018 [17] | China | 77 | 9 | 68 | 14.75 | 40 Anterior/37 Posterior | 6 | 71 | Min 65.2 m |
| Lim 2020 [18] | Singapore | 36 | 0 | 36 | 14.2 | 25 Anterior/11 Posterior | 9 | 27 | 120 m |
| Lonner 2017 [19] | USA | 851 | 183 | 668 | 14.4 | Posterior Instrumented Fusion | 60 | 791 | 24 m |
| Ogura 2021 [20] | USA | 345 | 68 | 277 | 14.5 | Posterior Instrumented Fusion | 15 | 330 | Min 12 m |
| Peng 2020 [21] | China | 44 | 10 | 34 | 18 | Posterior Instrumented Fusion | 10 | 34 | Min 12 m |
| Wang 2020 [23] | China | 84 | 25 | 59 | 14.63 | Posterior Instrumented Fusion | 20 | 64 | 24 m |
| Wang 2021 [22] | China | 52 | 11 | 41 | 14 | Posterior Instrumented Fusion | 12 | 40 | Min 24 m |
| Yang 2003 [24] | Taiwan | 14 | 1 | 13 | 15.8 | Posterior Instrumented Fusion | 6 | 8 | Min 24 m |
| Zhao 2018 [25] | China | 87 | 21 | 66 | 13.51 | Posterior Instrumented Fusion | 35 | 52 | Average 56 m |
| Zhou 2021 [26] | China | 70 | 16 | 54 | 15.3 | Posterior Instrumented Fusion | 13 | 57 | Min 24 m |
| Kim 2005 [5] | USA | 193 | 27 | 166 | 14.3 | Posterior Instrumented Fusion | 50 | 143 | Min 60 m |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katzouraki, G.; Vasiliadis, E.S.; Kaspiris, A.; Evangelopoulos, D.-S.; Grivas, T.B.; Pneumatikos, S.G. Sagittal Balance Parameters and Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis. J. Clin. Med. 2024, 13, 1895. https://doi.org/10.3390/jcm13071895
Katzouraki G, Vasiliadis ES, Kaspiris A, Evangelopoulos D-S, Grivas TB, Pneumatikos SG. Sagittal Balance Parameters and Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis. Journal of Clinical Medicine. 2024; 13(7):1895. https://doi.org/10.3390/jcm13071895
Chicago/Turabian StyleKatzouraki, Galateia, Elias S. Vasiliadis, Angelos Kaspiris, Dimitrios-Stergios Evangelopoulos, Theodoros B. Grivas, and Spiros G. Pneumatikos. 2024. "Sagittal Balance Parameters and Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis" Journal of Clinical Medicine 13, no. 7: 1895. https://doi.org/10.3390/jcm13071895
APA StyleKatzouraki, G., Vasiliadis, E. S., Kaspiris, A., Evangelopoulos, D.-S., Grivas, T. B., & Pneumatikos, S. G. (2024). Sagittal Balance Parameters and Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis. Journal of Clinical Medicine, 13(7), 1895. https://doi.org/10.3390/jcm13071895










