Oscillometry Longitudinal Data on COVID-19 Acute Respiratory Distress Syndrome Treated with Non-Invasive Respiratory Support
Abstract
1. Introduction
2. Materials and Methods
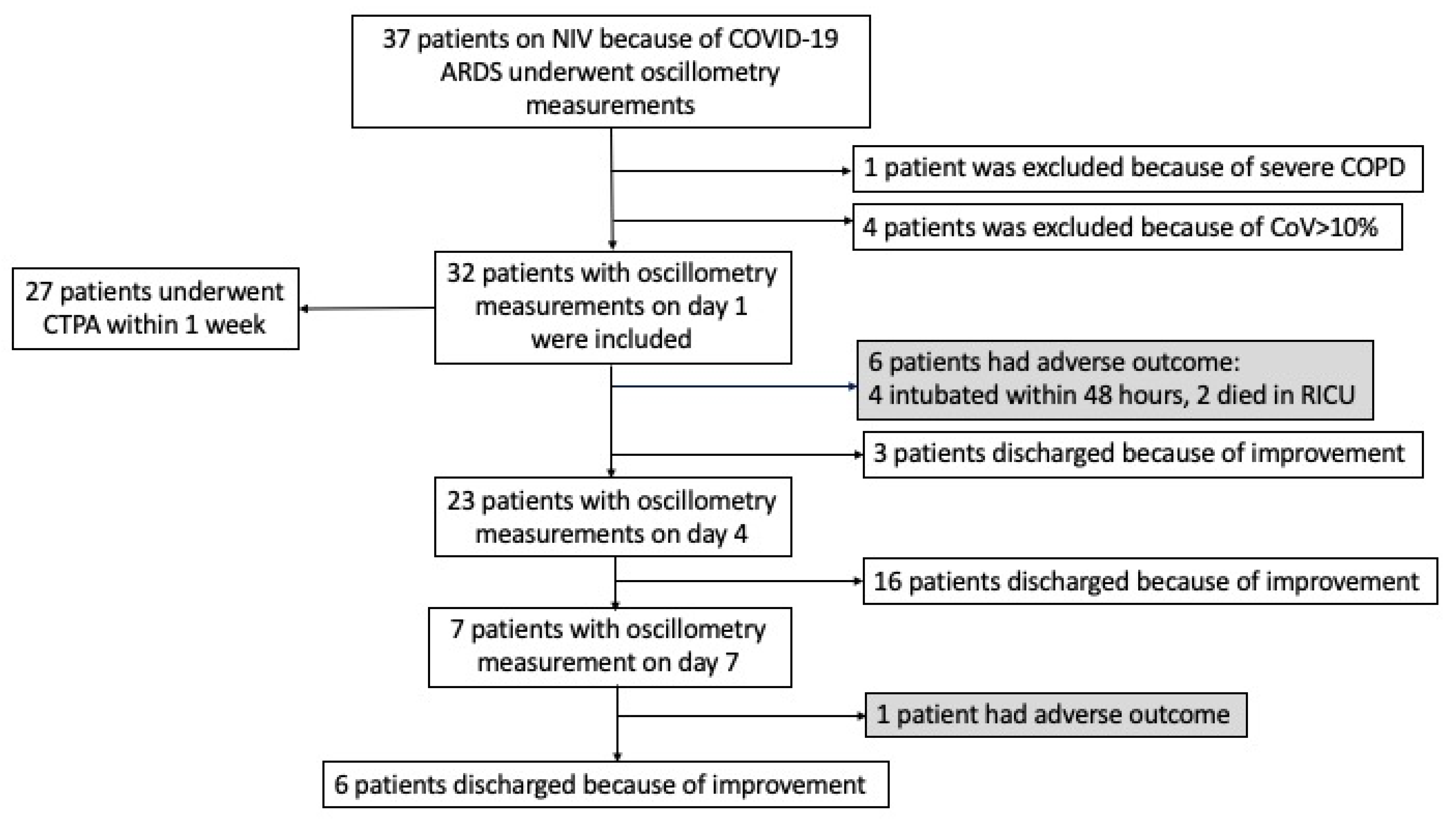
2.1. Study Population
2.2. Data Collection
2.3. Measurements
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
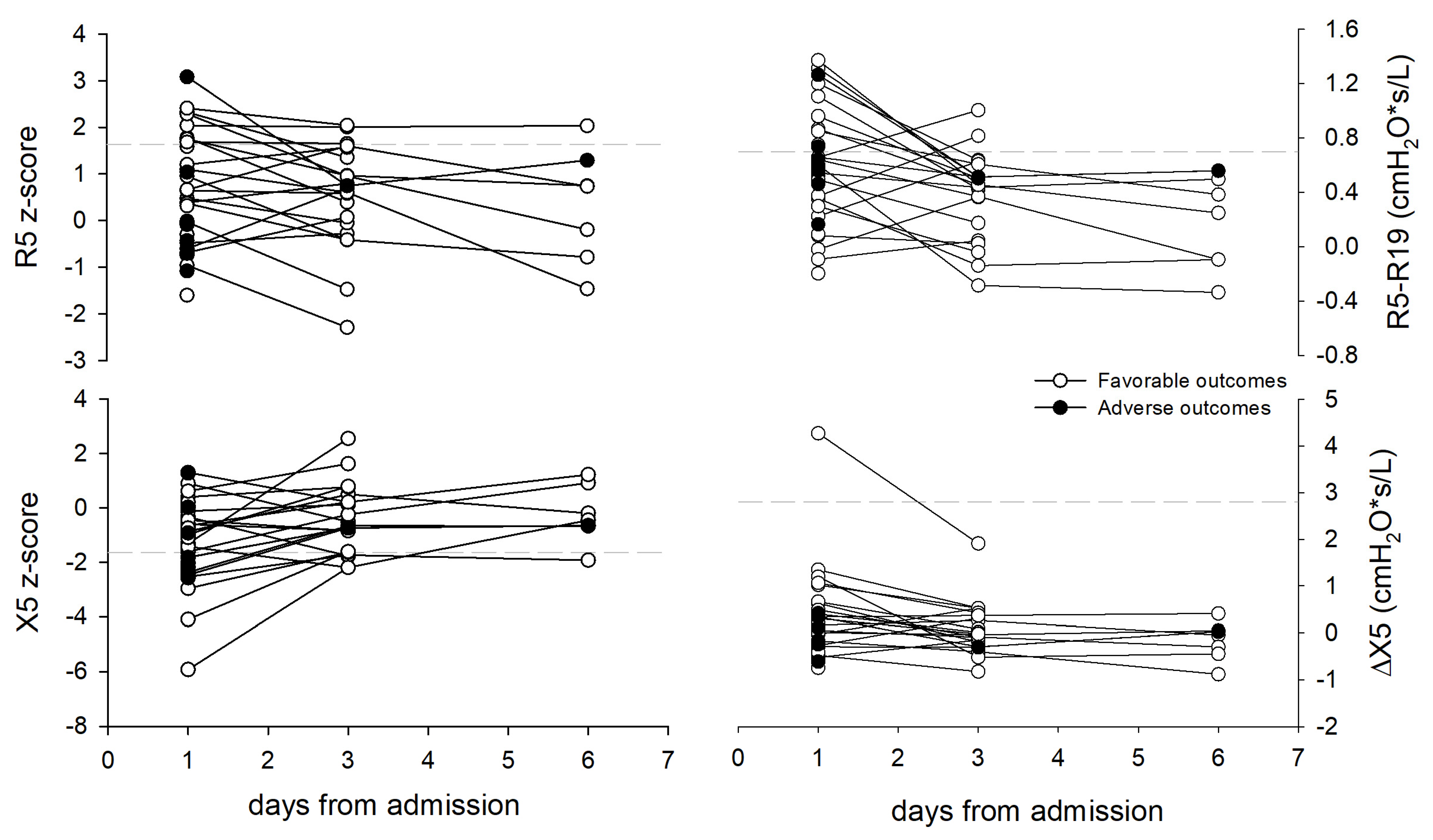
3.1. Lung Mechanics
3.2. Comparison with Imaging and Clinical Data
3.3. Relationship with Clinical Outcomes
4. Discussion
4.1. Lung Mechanics
4.2. Comparison with Imaging and Clinical Data
4.3. Relationship with Clinical Outcomes
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Weerakkody, S.; Arina, P.; Glenister, J.; Cottrell, S.; Boscaini-Gilroy, G.; Singer, M.; Montgomery, H.E. Non-invasive respiratory support in the management of acute COVID-19 pneumonia: Considerations for clinical practice and priorities for research. Lancet Respir. Med. 2022, 10, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Radovanovic, D.; Coppola, S.; Franceschi, E.; Gervasoni, F.; Duscio, E.; Chiumello, D.A.; Santus, P. Mortality and clinical outcomes in patients with COVID-19 pneumonia treated with non-invasive respiratory support: A rapid review. J. Crit. Care 2021, 65, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tobin, M.J.; Jubran, A.; Laghi, F. Noninvasive strategies in COVID-19: Epistemology, randomised trials, guidelines, physiology. Eur. Respir. J. 2021, 57, 2004247. [Google Scholar] [CrossRef] [PubMed]
- Wunsch, H. Mechanical Ventilation in COVID-19: Interpreting the Current Epidemiology. Am. J. Respir. Crit. Care Med. 2020, 202, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, C.; Bouadma, L.; de Montmollin, E.; Goldgran-Toledano, D.; Schwebel, C.; Reignier, J.; Neuville, M.; Ursino, M.; Siami, S.; Ruckly, S.; et al. Association Between Early Invasive Mechanical Ventilation and Day-60 Mortality in Acute Hypoxemic Respiratory Failure Related to Coronavirus Disease-2019 Pneumonia. Crit. Care Explor. 2021, 3, e0329. [Google Scholar] [CrossRef]
- Daniel, P.; Mecklenburg, M.; Massiah, C.; Joseph, M.A.; Wilson, C.; Parmar, P.; Rosengarten, S.; Maini, R.; Kim, J.; Oomen, A.; et al. Non-invasive positive pressure ventilation versus endotracheal intubation in treatment of COVID-19 patients requiring ventilatory support. Am. J. Emerg. Med. 2021, 43, 103–108. [Google Scholar] [CrossRef]
- Menzella, F.; Barbieri, C.; Fontana, M.; Scelfo, C.; Castagnetti, C.; Ghidoni, G.; Ruggiero, P.; Livrieri, F.; Piro, R.; Ghidorsi, L.; et al. Effectiveness of noninvasive ventilation in COVID-19 related-acute respiratory distress syndrome. Clin. Respir. J. 2021, 15, 779–787. [Google Scholar] [CrossRef]
- Grieco, D.L.; Maggiore, S.M.; Roca, O.; Spinelli, E.; Patel, B.K.; Thille, A.W.; Barbas, C.S.V.; De Acilu, M.G.; Cutuli, S.L.; Bongiovanni, F.; et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Med. 2021, 47, 851–866. [Google Scholar] [CrossRef]
- Grasselli, G.; Tonetti, T.; Protti, A.; Langer, T.; Girardis, M.; Bellani, G.; Laffey, J.; Carrafiello, G.; Carsana, L.; Rizzuto, C.; et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 2020, 8, 1201–1208. [Google Scholar] [CrossRef]
- Bos, L.D.J.; Sinha, P.; Dickson, R.P. Response to COVID-19 phenotyping correspondence. Eur. Respir. J. 2020, 56, 2002756. [Google Scholar] [CrossRef]
- Ferrando, C.; Suarez-Sipmann, F.; Mellado-Artigas, R.; Hernández, M.; Gea, A.; Arruti, E.; Aldecoa, C.; Martínez-Pallí, G.; Martínez-González, M.A.; Slutsky, A.S.; et al. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med. 2020, 46, 2200–2211. [Google Scholar] [CrossRef] [PubMed]
- Vandenbunder, B.; Ehrmann, S.; Piagnerelli, M.; Sauneuf, B.; Serck, N.; Soumagne, T.; Textoris, J.; Vinsonneau, C.; Aissaoui, N.; for the COVADIS study group; et al. Static compliance of the respiratory system in COVID-19 related ARDS: An international multicenter study. Crit. Care 2021, 25, 52. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Chiumello, D.; Caironi, P.; Busana, M.; Romitti, F.; Brazzi, L.; Camporota, L. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020, 46, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Chiumello, D.; Busana, M.; Coppola, S.; Romitti, F.; Formenti, P.; Bonifazi, M.; Pozzi, T.; Palumbo, M.M.; Cressoni, M.; Herrmann, P.; et al. Physiological and quantitative CT-scan characterization of COVID-19 and typical ARDS: A matched cohort study. Intensive Care Med. 2020, 46, 2187–2196. [Google Scholar] [CrossRef] [PubMed]
- Marini, J.J.; Gattinoni, L. Management of COVID-19 Respiratory Distress. JAMA 2020, 323, 2329. [Google Scholar] [CrossRef] [PubMed]
- Puah, S.H.; Cove, M.E.; Phua, J.; Kansal, A.; Venkatachalam, J.; Ho, V.K.; Sewa, D.W.; Gokhale, R.S.; Liew, M.F.; Ho, B.C.H.; et al. Association between lung compliance phenotypes and mortality in COVID-19 patients with acute respiratory distress syndrome. Ann. Acad. Med. Singap. 2021, 50, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Tomazini, B.M.; Costa, E.L.V.; Besen, B.A.M.P.; Zampieri, F.G.; de Carvalho, C.R.R.; Caser, E.B.; de Souza-Dantas, V.C.; Boschi, E.; Fumis, R.R.L.; de Alencar Filho, M.S.; et al. Clinical outcomes and lung mechanics characteristics between COVID-19 and non-COVID-19-associated acute respiratory distress syndrome: A propensity score analysis of two major randomized trials. Rev. Bras. Ter. Intensiv. 2022, 34, 335–341. [Google Scholar] [CrossRef]
- Johnson, M.K.; Birch, M.; Carter, R.; Kinsella, J.; Stevenson, R.D. Use of reactance to estimate transpulmonary resistance. Eur. Respir. J. 2005, 25, 1061–1069. [Google Scholar] [CrossRef]
- Dellaca, R.L.; Andersson Olerud, M.; Zannin, E.; Kostic, P.; Pompilio, P.P.; Hedenstierna, G.; Pedotti, A.; Frykholm, P. Lung recruitment assessed by total respiratory system input reactance. Intensive Care Med. 2009, 35, 2164–2172. [Google Scholar] [CrossRef]
- King, G.G.; Bates, J.; Berger, K.I.; Calverley, P.; de Melo, P.L.; Dellacà, R.L.; Farré, R.; Hall, G.L.; Ioan, I.; Irvin, C.G.; et al. Technical standards for respiratory oscillometry. Eur. Respir. J. 2020, 55, 1900753. [Google Scholar] [CrossRef]
- Dellacà, R.L.; Veneroni, C.; Vendettuoli, V.; Zannin, E.; Matassa, P.G.; Pedotti, A.; Colnaghi, M.; Mosca, F. Relationship between respiratory impedance and positive end-expiratory pressure in mechanically ventilated neonates. Intensive Care Med. 2013, 39, 511–519. [Google Scholar] [CrossRef]
- Raffaeli, G.; Veneroni, C.; Ghirardello, S.; Lavizzari, A.; Passera, S.; Mosca, F.; Cavallaro, G.; Dellacà, R.L. Role of Lung Function Monitoring by the Forced Oscillation Technique for Tailoring Ventilation and Weaning in Neonatal ECMO: New Insights From a Case Report. Front. Pediatr. 2018, 6, 332. [Google Scholar] [CrossRef] [PubMed]
- Torregiani, C.; Veneroni, C.; Confalonieri, P.; Citton, G.M.; Salton, F.; Jaber, M.; Confalonieri, M.; Dellaca’, R.L. Monitoring respiratory mechanics by oscillometry in COVID-19 patients receiving non-invasive respiratory support. PLoS ONE 2022, 17, e0265202. [Google Scholar] [CrossRef] [PubMed]
- Luan, Y.; Yin, C.; Yao, Y. Update Advances on C-Reactive Protein in COVID-19 and Other Viral Infections. Front. Immunol. 2021, 12, 720363. [Google Scholar] [CrossRef]
- Plebani, M. Why C-reactive protein is one of the most requested tests in clinical laboratories? Clin. Chem. Lab. Med. 2023, 61, 1540–1545. [Google Scholar] [CrossRef]
- Mantovani, A.; Garlanda, C. Humoral Innate Immunity and Acute-Phase Proteins. N. Engl. J. Med. 2023, 388, 439–452. [Google Scholar] [CrossRef]
- Oostveen, E.; Boda, K.; van der Grinten, C.P.M.; James, A.L.; Young, S.; Nieland, H.; Hantos, Z. Respiratory impedance in healthy subjects: Baseline values and bronchodilator response. Eur. Respir. J. 2013, 42, 1513–1523. [Google Scholar] [CrossRef]
- Matthay, M.A.; Arabi, Y.; Arroliga, A.C.; Bernard, G.; Bersten, A.D.; Brochard, L.J.; Calfee, C.S.; Combes, A.; Daniel, B.M.; Ferguson, N.D.; et al. A New Global Definition of Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2024, 209, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Cottini, M.; Bondi, B.; Bagnasco, D.; Braido, F.; Passalacqua, G.; Licini, A.; Lombardi, C.; Berti, A.; Comberiati, P.; Landi, M.; et al. Impulse oscillometry defined small airway dysfunction in asthmatic patients with normal spirometry: Prevalence, clinical associations, and impact on asthma control. Respir. Med. 2023, 218, 107391. [Google Scholar] [CrossRef]
- Dellacà, R.L.; Santus, P.; Aliverti, A.; Stevenson, N.; Centanni, S.; Macklem, P.T.; Pedotti, A.; Calverley, P.M.A. Detection of expiratory flow limitation in COPD using the forced oscillation technique. Eur. Respir. J. 2004, 23, 232–240. [Google Scholar] [CrossRef]
- Kaminsky, D.A.; Simpson, S.J.; Berger, K.I.; Calverley, P.; De Melo, P.L.; Dandurand, R.; Dellacà, R.L.; Farah, C.S.; Farré, R.; Hall, G.L.; et al. Clinical significance and applications of oscillometry. Eur. Respir. Rev. 2022, 31, 210208. [Google Scholar] [CrossRef] [PubMed]
- Terraneo, S.; Rinaldo, R.F.; Sferrazza Papa, G.F.; Ribolla, F.; Gulotta, C.; Maugeri, L.; Gatti, E.; Centanni, S.; Di Marco, F. Distinct Mechanical Properties of the Respiratory System Evaluated by Forced Oscillation Technique in Acute Exacerbation of COPD and Acute Decompensated Heart Failure. Diagnostics 2021, 11, 554. [Google Scholar] [CrossRef]
- Dhont, S.; Derom, E.; Van Braeckel, E.; Depuydt, P.; Lambrecht, B.N. The pathophysiology of ‘happy’ hypoxemia in COVID-19. Respir. Res. 2020, 21, 198. [Google Scholar] [CrossRef] [PubMed]
- Pelosi, P.; Tonelli, R.; Torregiani, C.; Baratella, E.; Confalonieri, M.; Battaglini, D.; Marchioni, A.; Confalonieri, P.; Clini, E.; Salton, F.; et al. Different Methods to Improve the Monitoring of Noninvasive Respiratory Support of Patients with Severe Pneumonia/ARDS Due to COVID-19: An Update. J. Clin. Med. 2022, 11, 1704. [Google Scholar] [CrossRef] [PubMed]
- Kleinhendler, E.; Rosman, M.; Fireman, E.; Freund, O.; Gershman, I.; Pumin, I.; Perluk, T.; Tiran, B.; Unterman, A.; Bar-Shai, A. Impulse Oscillometry as an Alternative Lung Function Test for Hospitalized Adults. Respir. Care 2024, respcare.10963. [Google Scholar] [CrossRef]
- Tonelli, R.; Fantini, R.; Tabbì, L.; Castaniere, I.; Pisani, L.; Pellegrino, M.R.; Della Casa, G.; D’Amico, R.; Girardis, M.; Nava, S.; et al. Early Inspiratory Effort Assessment by Esophageal Manometry Predicts Noninvasive Ventilation Outcome in De Novo Respiratory Failure. A Pilot Study. Am. J. Respir. Crit. Care Med. 2020, 202, 558–567. [Google Scholar] [CrossRef]
- Lopes, A.J.; Litrento, P.F.; Provenzano, B.C.; Carneiro, A.S.; Monnerat, L.B.; da Cal, M.S.; Ghetti, A.T.A.; Mafort, T.T. Small airway dysfunction on impulse oscillometry and pathological signs on lung ultrasound are frequent in post-COVID-19 patients with persistent respiratory symptoms. PLoS ONE 2021, 16, e0260679. [Google Scholar] [CrossRef]
- Veneroni, C.; Perissin, R.; Di Marco, F.; Dellaca’, R.L. Home monitoring of lung mechanics by oscillometry before, during and after severe COVID-19 disease: A case study. ERJ Open Res. 2023, 9, 00480–02022. [Google Scholar] [CrossRef]
- Wagner, C.; Griesel, M.; Mikolajewska, A.; Mueller, A.; Nothacker, M.; Kley, K.; Metzendorf, M.-I.; Fischer, A.-L.; Kopp, M.; Stegemann, M.; et al. Systemic corticosteroids for the treatment of COVID-19. Cochrane Database Syst. Rev. 2021, 2021, CD014963. [Google Scholar] [CrossRef]
- Salton, F.; Confalonieri, P.; Meduri, G.U.; Mondini, L.; Trotta, L.; Barbieri, M.; Bozzi, C.; Torregiani, C.; Lerda, S.; Bellan, M.; et al. Theory and Practice of Glucocorticoids in COVID-19: Getting to the Heart of the Matter—A Critical Review and Viewpoints. Pharmaceuticals 2023, 16, 924. [Google Scholar] [CrossRef] [PubMed]
- Tonelli, R.; Busani, S.; Tabbì, L.; Fantini, R.; Castaniere, I.; Biagioni, E.; Mussini, C.; Girardis, M.; Clini, E.; Marchioni, A. Inspiratory Effort and Lung Mechanics in Spontaneously Breathing Patients with Acute Respiratory Failure due to COVID-19: A Matched Control Study. Am. J. Respir. Crit. Care Med. 2021, 204, 725–728. [Google Scholar] [CrossRef]
- Busana, M.; Giosa, L.; Cressoni, M.; Gasperetti, A.; Di Girolamo, L.; Martinelli, A.; Sonzogni, A.; Lorini, L.; Palumbo, M.M.; Romitti, F.; et al. The impact of ventilation-perfusion inequality in COVID-19: A computational model. J. Appl. Physiol. 2021, 130, 865–876. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Kang, J.; Seo, W.J.; Park, S.H.; Kang, H.K.; Park, H.K.; Hyun, J.; Song, J.E.; Kwak, Y.G.; Kim, K.H.; et al. Prediction models for respiratory outcomes in patients with COVID-19: Integration of quantitative computed tomography parameters, demographics, and laboratory features. J. Thorac. Dis. 2023, 15, 1506–1516. [Google Scholar] [CrossRef] [PubMed]
- Lanza, E.; Muglia, R.; Bolengo, I.; Santonocito, O.G.; Lisi, C.; Angelotti, G.; Morandini, P.; Savevski, V.; Politi, L.S.; Balzarini, L. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Eur. Radiol. 2020, 30, 6770–6778. [Google Scholar] [CrossRef] [PubMed]
- Cappabianca, S.; Fusco, R.; De Lisio, A.; Paura, C.; Clemente, A.; Gagliardi, G.; Lombardi, G.; Giacobbe, G.; Russo, G.M.; Belfiore, M.P.; et al. Correction to: Clinical and laboratory data, radiological structured report findings and quantitative evaluation of lung involvement on baseline chest CT in COVID-19 patients to predict prognosis. Radiol. Med. 2021, 126, 643. [Google Scholar] [CrossRef] [PubMed]
- Ball, L.; Robba, C.; Herrmann, J.; Gerard, S.E.; Xin, Y.; Mandelli, M.; Battaglini, D.; Brunetti, I.; Minetti, G.; Seitun, S.; et al. Lung distribution of gas and blood volume in critically ill COVID-19 patients: A quantitative dual-energy computed tomography study. Crit. Care 2021, 25, 214. [Google Scholar] [CrossRef] [PubMed]
- Chiumello, D.; Mongodi, S.; Algieri, I.; Vergani, G.L.; Orlando, A.; Via, G.; Crimella, F.; Cressoni, M.; Mojoli, F. Assessment of Lung Aeration and Recruitment by CT Scan and Ultrasound in Acute Respiratory Distress Syndrome Patients*. Crit. Care Med. 2018, 46, 1761–1768. [Google Scholar] [CrossRef] [PubMed]
- Chiumello, D.; Chiodaroli, E.; Coppola, S.; Cappio Borlino, S.; Granata, C.; Pitimada, M.; Wendel Garcia, P.D. Awake prone position reduces work of breathing in patients with COVID-19 ARDS supported by CPAP. Ann. Intensive Care 2021, 11, 179. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.F.; Pershad, Y.; Kang, P.; Ridenour, L.; Lavon, B.; Lanclus, M.; Godon, R.; De Backer, J.; Glassberg, M.K. Altered pulmonary blood volume distribution as a biomarker for predicting outcomes in COVID-19 disease. Eur. Respir. J. 2021, 58, 2004133. [Google Scholar] [CrossRef]
- Revel, M.-P.; Boussouar, S.; de Margerie-Mellon, C.; Saab, I.; Lapotre, T.; Mompoint, D.; Chassagnon, G.; Milon, A.; Lederlin, M.; Bennani, S.; et al. Study of Thoracic CT in COVID-19: The STOIC Project. Radiology 2021, 301, E361–E370. [Google Scholar] [CrossRef]
- Araiza, A.; Duran, M.; Patiño, C.; Marik, P.E.; Varon, J. The Ichikado CT score as a prognostic tool for coronavirus disease 2019 pneumonia: A retrospective cohort study. J. Intensive Care 2021, 9, 51. [Google Scholar] [CrossRef]
- Le Berre, A.; Boeken, T.; Caramella, C.; Afonso, D.; Nhy, C.; Saccenti, L.; Tardivel, A.-M.; Gerber, S.; Frison Roche, A.; Emmerich, J.; et al. Dual-energy CT angiography reveals high prevalence of perfusion defects unrelated to pulmonary embolism in COVID-19 lesions. Insights Imaging 2021, 12, 24. [Google Scholar] [CrossRef]
- Swenson, K.E.; Hardin, C.C. Pathophysiology of Hypoxemia in COVID-19 Lung Disease. Clin. Chest Med. 2023, 44, 239–248. [Google Scholar] [CrossRef]
- Shi, R.; Lai, C.; Teboul, J.-L.; Dres, M.; Moretto, F.; De Vita, N.; Pham, T.; Bonny, V.; Mayaux, J.; Vaschetto, R.; et al. COVID-19 ARDS is characterized by higher extravascular lung water than non-COVID-19 ARDS: The PiCCOVID study. Crit. Care Lond. Engl. 2021, 25, 186. [Google Scholar] [CrossRef]
- Duan, J.; Han, X.; Bai, L.; Zhou, L.; Huang, S. Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients. Intensive Care Med. 2017, 43, 192–199. [Google Scholar] [CrossRef]
- Santus, P.; Pini, S.; Amati, F.; Saad, M.; Gatti, M.; Mondoni, M.; Tursi, F.; Rizzi, M.; Chiumello, D.A.; Monzani, V.; et al. Predictors of Helmet CPAP Failure in COVID-19 Pneumonia: A Prospective, Multicenter, and Observational Cohort Study. Can. Respir. J. 2022, 2022, 1499690. [Google Scholar] [CrossRef]
- Henry, B.M.; de Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef]
| ALL (n = 32) | FAVORABLE Outcome (n = 25) | ADVERSE Outcome (n = 7) | |
|---|---|---|---|
| Patient data | |||
| Age (years) | 60 (53; 69) | 58 (52; 65) | 69 (61; 78) |
| Females | 7 (22%) | 7 (28%) | 0 |
| BMI (kg/m2) | 28.5 (26.0; 32.8) | 28.7 (26.2; 31.3) | 26.5 (24.6; 37.8) |
| Smokers (no; ex; yes) | 18; 11; 3 | 13; 9; 3 | 5; 2; 0 |
| Charlson Comorbidity Index | 2 (1; 3) | 2 (1; 3) | 3 (2.5; 3.5) |
| Clinical parameters | |||
| PaO2/FiO2—HFNC | 91 (74; 115) | 92 (77; 115) | 73 (61; 116) |
| PaO2/FiO2—NIV | 151 (146; 191) | 162 (150; 197) | 144 (84; 149) * |
| TVE/PBW mL/kg | 9.1 (7.9; 10.2) | 9.0 (8.1; 10.2) | 8.2 (7.7; 10.5) |
| APACHE | 8.5 (6.5; 10.0) | 8.0 (6.0; 10.0) | 9.0 (7.2; 12.7) |
| LDH units/L | 378 (318; 477) | 343 (304; 447) | 484 (435; 505) * |
| D-dimer mcg/L | 873 (566; 1143) | 865 (488; 1087) | 1154 (638; 1691) |
| CRP mg/L | 75.0 (28.5; 99.2) | 73.8 (32.2; 97.1) | 76.3 (23.6; 105.1) |
| HACOR | 3 (2; 4) | 3 (2; 4) | 4 (4; 6) * |
| CT parameters a | |||
| Inflated (%) | 59.0 (53.0; 63.5) | 61.0 (56.5; 65.0) | 54.0 (50.2; 54.7) * |
| Overaerated (%) | 13.8 (12.2; 19.6) | 14.0 (12.7; 19.2) | 13.6 (8.0; 20.4) |
| Poorly aerated (%) | 18.1 (16.1; 25.8) | 17.8 (15.3; 24.1) | 23.6 (19.1; 28.4) |
| Collapsed (%) | 4.2 (3.4; 5.9) | 4.0 (3.4; 5.6) | 5.5 (3.9; 6.4) |
| Oscillometry parameters | |||
| R5 z-score | 0.43 (−0.46; 1.64) | 0.64 (−0.35; 1.70) | −0.08 (−0.64; 0.77) |
| X5 z-score | −1.04 (−2.27; −0.06) | −0.98 (−2.12; −0.08) | −1.83 (−2.32; −0.22) |
| dX | 0.13 (−0.25; 0.45) | 0.21 (−0.27; 0.64) | −0.17 (−0.23; 0.28) |
| R5–R19 | 0.59 (0.33; 0.86) | 0.60 (0.28; 0.89) | 0.58 (0.49; 0.71) |
| Hospital stay | |||
| Hospital stay before RICU admission (days) | 1 (0; 3) | 1 (0; 3) | 2 (0.5; 8) * |
| RICU stay (days) | 6 (4; 7) | 6 (4; 7) | 2 (2; 8.5) |
| Total hospital stay (days) | 15 (11; 20) | 15 (11; 20) | 31 (25; 39) |
| Inflated | Poorly Aerated | Collapsed | ||||
|---|---|---|---|---|---|---|
| mL | % | mL | % | mL | % | |
| R5 z-score | 0.38 (0.045) | 0.30 (0.12) | −0.10 (0.59) | −0.29 (0.13) | 0.14 (0.46) | 0.02 (0.90) |
| X5 z-score | 0.06 (0.76) | 0.09 (0.65) | −0.12 (0.53) | −0.18 (0.35) | −0.38 (0.046) | −0.37 (0.051) |
| PaO2/FiO2 NIV | 0.17 (0.41) | 0.38 (0.06) | −0.52 (0.01) | −0.56 (0.004) | −0.21 (0.32) | −0.23 (0.27) |
| APACHE | −0.24 (0.20) | −0.44 (0.02) | 0.28 (0.14) | 0.30 (0.10) | 0.36 (0.050) | 0.39 (0.033) |
| LDH | 0.05 (0.79) | −0.60 (0.0005) | 0.58 (0.0008) | 0.47 (0.009) | 0.48 (0.008) | 0.33 (0.08) |
| HACOR | −0.17 (0.41) | −0.34 (0.10) | 0.50 (0.01) | 0.56 (0.004) | 0.208 (0.33) | 0.27 (0.21) |
| Days in RICU | Total Hospital Days | |
|---|---|---|
| PaO2/FiO2 HFNC (mmHg) | −0.45 (0.02) | −0.37 (0.06) |
| APACHE | 0.48 (0.01) | 0.26 (0.20) |
| LDH units/L | 0.45 (0.02) | 0.42 (0.03) |
| CT–Inflated % a | −0.39 (0.08) | −0.53 (0.01) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torregiani, C.; Baratella, E.; Segalotti, A.; Ruaro, B.; Salton, F.; Confalonieri, P.; Tavano, S.; Lapadula, G.; Bozzi, C.; Confalonieri, M.; et al. Oscillometry Longitudinal Data on COVID-19 Acute Respiratory Distress Syndrome Treated with Non-Invasive Respiratory Support. J. Clin. Med. 2024, 13, 1868. https://doi.org/10.3390/jcm13071868
Torregiani C, Baratella E, Segalotti A, Ruaro B, Salton F, Confalonieri P, Tavano S, Lapadula G, Bozzi C, Confalonieri M, et al. Oscillometry Longitudinal Data on COVID-19 Acute Respiratory Distress Syndrome Treated with Non-Invasive Respiratory Support. Journal of Clinical Medicine. 2024; 13(7):1868. https://doi.org/10.3390/jcm13071868
Chicago/Turabian StyleTorregiani, Chiara, Elisa Baratella, Antonio Segalotti, Barbara Ruaro, Francesco Salton, Paola Confalonieri, Stefano Tavano, Giulia Lapadula, Chiara Bozzi, Marco Confalonieri, and et al. 2024. "Oscillometry Longitudinal Data on COVID-19 Acute Respiratory Distress Syndrome Treated with Non-Invasive Respiratory Support" Journal of Clinical Medicine 13, no. 7: 1868. https://doi.org/10.3390/jcm13071868
APA StyleTorregiani, C., Baratella, E., Segalotti, A., Ruaro, B., Salton, F., Confalonieri, P., Tavano, S., Lapadula, G., Bozzi, C., Confalonieri, M., Dellaca’, R. L., & Veneroni, C. (2024). Oscillometry Longitudinal Data on COVID-19 Acute Respiratory Distress Syndrome Treated with Non-Invasive Respiratory Support. Journal of Clinical Medicine, 13(7), 1868. https://doi.org/10.3390/jcm13071868











