Surgical and Fertility Outcomes of Reduced-Port Robotic Myomectomy: A Single-Center Experience of 401 Cases
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cramer, S.F.; Patel, A. The frequency of uterine leiomyomas. Am. J. Clin. Pathol. 1990, 94, 435–438. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Magaoay, B.; Rosen, M.P.; Cedars, M.I. Presence of Fibroids on Transvaginal Ultrasonography in a Community-Based, Diverse Cohort of 996 Reproductive-Age Female Participants. JAMA Netw. Open 2023, 6, e2312701. [Google Scholar] [CrossRef]
- Pritts, E.A.; Parker, W.H.; Olive, D.L. Fibroids and infertility: An updated systematic review of the evidence. Fertil. Steril. 2009, 91, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Hu, Y.; Chen, X.C.; Zheng, F.Y.; Lin, F.; Zhou, K.; Chen, F.D.; Gu, H.Z. Laparoscopic versus open myomectomy—A meta-analysis of randomized controlled trials. Eur. J. Obstet. Gynecol. Reprod. Biol. 2009, 145, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Bhave Chittawar, P.; Franik, S.; Pouwer, A.W.; Farquhar, C. Minimally invasive surgical techniques versus open myomectomy for uterine fibroids. Cochrane Database Syst. Rev. 2014, 10, Cd004638. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.H.; Song, E.; Kim, S.K.; Lee, J.R.; Suh, C.S. Operative and Obstetric Outcomes after Single-Port Laparoscopic Myomectomy: A Retrospective Single-Center Analysis of 504 Cases. J. Minim. Invasive Gynecol. 2021, 28, 2080–2088. [Google Scholar] [CrossRef]
- Orlando, M.; Kollikonda, S.; Hackett, L.; Kho, R. Non-hysteroscopic Myomectomy and Fertility Outcomes: A Systematic Review. J. Minim. Invasive Gynecol. 2021, 28, 598–618.e591. [Google Scholar] [CrossRef]
- Iavazzo, C.; Mamais, I.; Gkegkes, I.D. Robotic assisted vs laparoscopic and/or open myomectomy: Systematic review and meta-analysis of the clinical evidence. Arch. Gynecol. Obstet. 2016, 294, 5–17. [Google Scholar] [CrossRef]
- Jeong, H.G.; Lee, M.J.; Lee, J.R.; Jee, B.C.; Kim, S.K. The Largest Uterine Leiomyoma Removed by Robotic-Assisted Laparoscopy in the Late Reproductive Age: A Case Report. J. Menopausal Med. 2021, 27, 37–41. [Google Scholar] [CrossRef]
- Advincula, A.P.; Xu, X.; Goudeau, S.t.; Ransom, S.B. Robot-assisted laparoscopic myomectomy versus abdominal myomectomy: A comparison of short-term surgical outcomes and immediate costs. J. Minim. Invasive Gynecol. 2007, 14, 698–705. [Google Scholar] [CrossRef]
- Nam, S.H.; Paek, J.; Choi, C.; Nam, S.H.; Kim, W.Y. A comparison between reduced-port robotic surgery and multiport robot-assisted laparoscopy for myomectomy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 213, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Lönnerfors, C.; Persson, J. Pregnancy following robot-assisted laparoscopic myomectomy in women with deep intramural myomas. Acta Obstet. Gynecol. Scand. 2011, 90, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Cela, V.; Freschi, L.; Simi, G.; Tana, R.; Russo, N.; Artini, P.G.; Pluchino, N. Fertility and endocrine outcome after robot-assisted laparoscopic myomectomy (RALM). Gynecol. Endocrinol. 2013, 29, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Tusheva, O.A.; Gyang, A.; Patel, S.D. Reproductive outcomes following robotic-assisted laparoscopic myomectomy (RALM). J. Robot. Surg. 2013, 7, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Pitter, M.C.; Srouji, S.S.; Gargiulo, A.R.; Kardos, L.; Seshadri-Kreaden, U.; Hubert, H.B.; Weitzman, G.A. Fertility and Symptom Relief following Robot-Assisted Laparoscopic Myomectomy. Obstet. Gynecol. Int. 2015, 2015, 967568. [Google Scholar] [CrossRef] [PubMed]
- Flyckt, R.; Soto, E.; Nutter, B.; Falcone, T. Comparison of Long-Term Fertility and Bleeding Outcomes after Robotic-Assisted, Laparoscopic, and Abdominal Myomectomy. Obstet. Gynecol. Int. 2016, 2016, 2789201. [Google Scholar] [CrossRef] [PubMed]
- Huberlant, S.; Lenot, J.; Neron, M.; Ranisavljevic, N.; Letouzey, V.; De Tayrac, R.; Masia, F.; Warembourg, S. Fertility and obstetrical outcomes after robot-assisted laparoscopic myomectomy. Int. J. Med. Robot. 2020, 16, e2059. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, H.R.; McCaffrey, C.; Amjad, H.; Kives, S. Fertility and Pregnancy Outcomes after Robotic-assisted Laparoscopic Myomectomy in a Canadian Cohort. J. Minim. Invasive Gynecol. 2022, 29, 72–76. [Google Scholar] [CrossRef]
- Morales, H.S.G.; López, R.R.; López, G.G.P.; Mondragón, P.J.C.; Cortés, D.V.; Hernández, H.S.; Guiot, M.L.; Camacho, F.M.R. Surgical approach to uterine myomatosis in patients with infertility: Open, laparoscopic, and robotic surgery; results according to the quantity of fibroids. JBRA Assist. Reprod. 2022, 26, 44–49. [Google Scholar] [CrossRef]
- Lebovitz, O.; Orvieto, R.; James, K.E.; Styer, A.K.; Brown, D.N. Predictors of reproductive outcomes following myomectomy for intramural fibroids. Reprod. Biomed. Online 2019, 39, 484–491. [Google Scholar] [CrossRef]
- Al-Serehi, A.; Mhoyan, A.; Brown, M.; Benirschke, K.; Hull, A.; Pretorius, D.H. Placenta accreta: An association with fibroids and Asherman syndrome. J. Ultrasound Med. 2008, 27, 1623–1628. [Google Scholar] [CrossRef]
- Tummers, P.; De Sutter, P.; Dhont, M. Risk of spontaneous abortion in singleton and twin pregnancies after IVF/ICSI. Hum. Reprod. 2003, 18, 1720–1723. [Google Scholar] [CrossRef] [PubMed]
- Pundir, J.; Omanwa, K.; Kovoor, E.; Pundir, V.; Lancaster, G.; Barton-Smith, P. Robotic-Assisted Laparoscopic vs. Abdominal and Laparoscopic Myomectomy: Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2017, 24, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Lonnerfors, C. Robot-assisted myomectomy. Best. Pract. Res. Clin. Obstet. Gynaecol. 2018, 46, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Advincula, A.P.; Wang, K. Evolving role and current state of robotics in minimally invasive gynecologic surgery. J. Minim. Invasive Gynecol. 2009, 16, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo, A.R. Computer-assisted reproductive surgery: Why it matters to reproductive endocrinology and infertility subspecialists. Fertil. Steril. 2014, 102, 911–921. [Google Scholar] [CrossRef] [PubMed]
- Tuschy, B.; Berlit, S.; Brade, J.; Sütterlin, M.; Hornemann, A. Gynaecological laparoscopic surgery for benign conditions: Do women care about incisions? Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 84–87. [Google Scholar] [CrossRef]
- Yeung, P.P., Jr.; Bolden, C.R.; Westreich, D.; Sobolewski, C. Patient preferences of cosmesis for abdominal incisions in gynecologic surgery. J. Minim. Invasive Gynecol. 2013, 20, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J.; Choi, C.; Nam, S.H.; Kim, W.Y. Feasibility of Reduced-Port Robotic Surgery for Myomectomy with the da Vinci Surgical System. J. Minim. Invasive Gynecol. 2017, 24, 926–931. [Google Scholar] [CrossRef]
- Radosa, M.P.; Owsianowski, Z.; Mothes, A.; Weisheit, A.; Vorwergk, J.; Asskaryar, F.A.; Camara, O.; Bernardi, T.S.; Runnebaum, I.B. Long-term risk of fibroid recurrence after laparoscopic myomectomy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 180, 35–39. [Google Scholar] [CrossRef]
- Shiota, M.; Kotani, Y.; Umemoto, M.; Tobiume, T.; Hoshiai, H. Recurrence of uterine myoma after laparoscopic myomectomy: What are the risk factors? Gynecol. Minim. Invasive Ther. 2012, 1, 34–36. [Google Scholar] [CrossRef]
- Kramer, K.J.; Ottum, S.; Gonullu, D.; Bell, C.; Ozbeki, H.; Berman, J.M.; Recanati, M.A. Reoperation rates for recurrence of fibroids after abdominal myomectomy in women with large uterus. PLoS ONE 2021, 16, e0261085. [Google Scholar] [CrossRef] [PubMed]
- Watrowski, R.; Jäger, C.; Forster, J. Predictors of postoperative hemoglobin drop after laparoscopic myomectomy. Wideochir Inne Tech. Maloinwazyjne 2017, 12, 81–87. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Mean ± SD (Range) or n (%) |
|---|---|
| Age (years) | 39.7 ± 6.0 (24–56) |
| BMI (kg/m2) | 23.0 ± 3.6 (16.1–40.5) |
| Previous abdominal surgery | |
| Yes | 159 (39.7%) |
| No | 242 (60.3%) |
| Indication | |
| Menorrhagia | 128 (31.9%) |
| Size increase | 124 (30.9%) |
| Dysmenorrhea | 9 (2.2%) |
| Chronic pelvic pain | 41 (10.2%) |
| Infertility | 57 (14.2%) |
| Urinary symptoms | 23 (5.7%) |
| Others | 19 (4.7%) |
| Total no. of myomas removed | 4.7 ± 4.1 (1–22) |
| Largest diameter of myoma (cm) | 7.8 ± 2.5 (2.5–16.0) |
| Largest myoma size (cm) | |
| ≤5 | 58 (14.5%) |
| >5 to ≤10 | 284 (70.8%) |
| >10 | 59 (14.7%) |
| Type of largest myoma | |
| Submucosal | 21 (5.2%) |
| Intramural | 253 (63.1%) |
| Subserosal | 104 (25.9%) |
| Intraligamentary | 10 (2.5%) |
| Pedunculated | 10 (2.5%) |
| Cervical | 2 (0.5%) |
| Ectopic | 1 (0.2%) |
| Operative Outcomes | Mean ± SD or n (%) |
|---|---|
| Operative time (min) | 103.7 ± 45.6 |
| Estimated blood loss (mL) | 149.6 ± 180.2 |
| Hb decrease after surgery (g/dL) | 2.0 ± 1.0 |
| Post-operative hospital stay (days) | 2.1 ± 0.6 |
| Numeric rating scale pain score | |
| At 1 h | 6.2 ± 1.2 |
| At 6 h | 3.1 ± 0.7 |
| At 24 h | 3.0 ± 0.7 |
| Suture methods | |
| Continuous | 197 (49.1%) |
| Continuous + interrupted | 204 (50.9%) |
| Conversion to Laparotomy | 0 (0%) |
| Insertion of additional Port | 0 (0%) |
| Intra-operative complications | |
| Yes | 8 (2.0%) |
| No | 393 (98.0%) |
| Post-operative complications | |
| Yes | 39 (9.7%) |
| No | 362 (90.3%) |
| Weight of specimen (g) | 235.3 ± 194.4 |
| Pathologic condition | |
| Leiomyoma | 386 (96.3%) |
| Combined adenomyosis | 15 (3.7%) |
| Recurrence Rate ** | 14/95 (14.7%) |
| Re-operation rate | 7/95 (7.4%) |
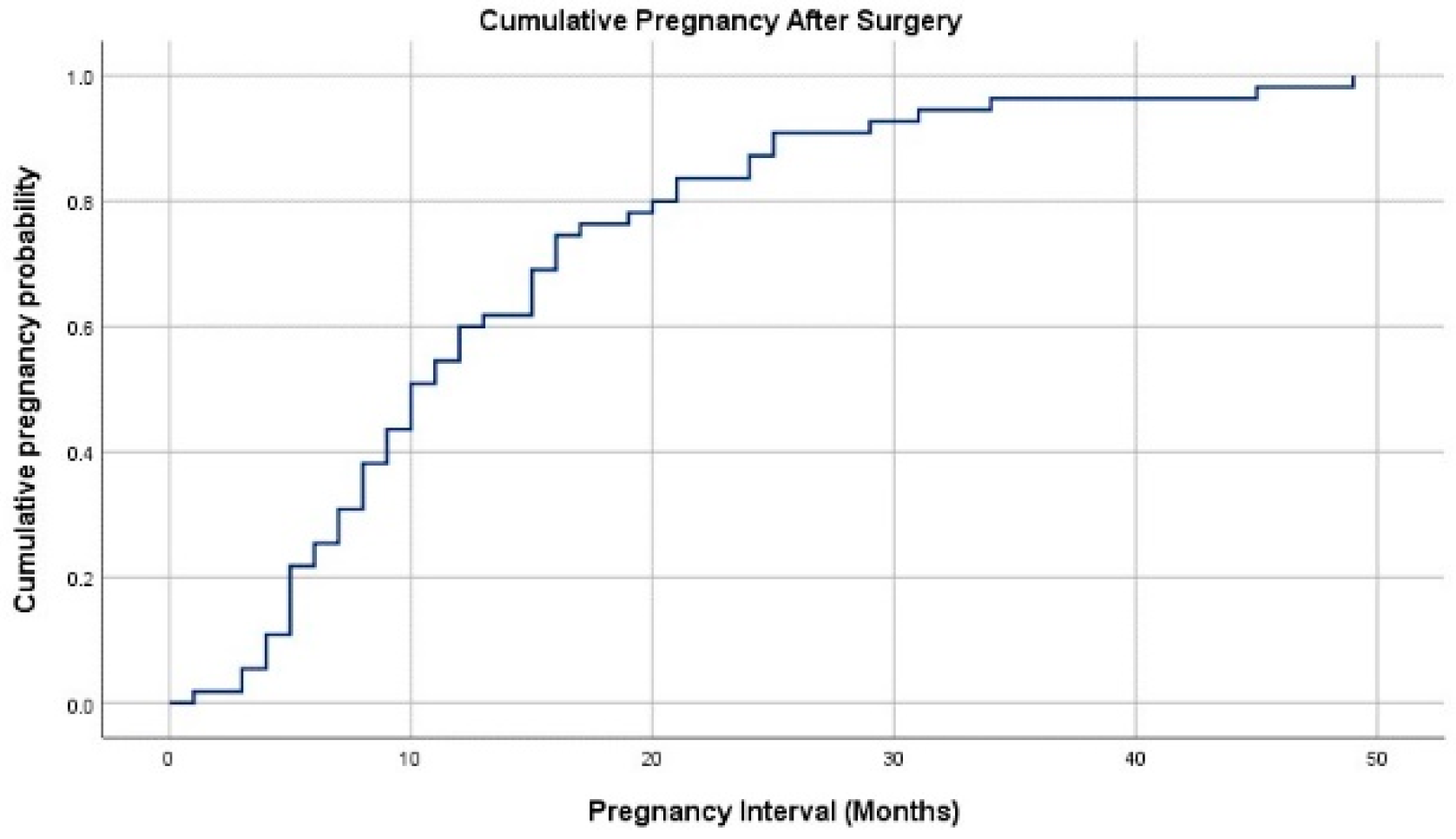
| Fertility Outcomes | Mean ± SD or n (%) |
|---|---|
| No. of women of reproductive age (20–45) | 327 (81.5%) |
| Pregnancy attempts after surgery | 70 |
| Clinical Pregnancy rate | 56/70 (80.0%) |
| Miscarriage rate | 7/70 (10.0%) |
| Live birth rate | 44/70 (62.9%) |
| Ongoing pregnancy rate | 5/70 (7.1%) |
| Interval between surgery and pregnancy (months) | 13.5 ± 10.1 |
| Method of conception | |
| Natural | 21 (37.5%) |
| IUI | 2 (3.6%) |
| IVF-ET | 33 (58.9%) |
| Multiple gestations | |
| Singleton | 40 (81.6%) |
| Twin pregnancy | 9 (18.4%) |
| Delivery term | |
| Term | 38 (86.4%) |
| Preterm | 6 (13.6%) |
| Mode of delivery | |
| Vaginal delivery | 1 (2.3%) |
| Cesarean section | 43 (97.7%) |
| Gestational age at delivery (weeks) | 37.3 ± 1.9 |
| Birthweight (kg) | 2.87 ± 0.53 |
| Gender | |
| Male | 29 (55.8%) |
| Female | 23 (44.2%) |
| Obstetric complications * | 8 (16.3%) |
| Postpartum complications † | 3 (6.8%) |
| Uterine rupture rate | 0 (0%) |
| Characteristics | Pregnant (n = 56) | Not Pregnant (n = 14) | p-Value |
|---|---|---|---|
| Age (years) | 35 [32.25–39] | 38.5 [33–41.25] | 0.097 * |
| BMI (kg/m2) | 22.80 [20.70–25.30] | 23.43 [20.49–27.48] | 0.618 * |
| Previous Abdominal Surgery | 0.699 † | ||
| Yes | 39 (69.6%) | 9 (64.3%) | |
| No | 17 (30.4%) | 5 (35.7%) | |
| Total no. of myomas removed | 4 [1–5.75] | 3.5 [1–7.25] | 0.89 * |
| Largest Diameter of myoma (cm) | 6.7 [4.8–8.0] | 8 [5.35–10.25] | 0.311 * |
| Type of largest myoma | 0.286 ‡ | ||
| Submucosal | 2 (14.3%) | 2 (14.3%) | |
| Intramural | 38 (64.3%) | 9 (64.3%) | |
| Subserosal | 16 (21.4%) | 3 (21.4%) | |
| Operative Time (min) | 127.5 [96.25–175] | 135 [118.75–157.50] | 0.67 |
| Estimated blood loss (mL) | 150 [100–300] | 150 [100–200] | 0.457 |
| Hb decrease after surgery (g/dL) | 1.9 [1.35–2.40] | 2.0 [1.2–2.8] | 0.994 |
| Postop Hospital stay (days) | 2 [2–2] | 2 [2–2] | 1 |
| Suture methods | 0.129 † | ||
| Continuous | 27 (48.2%) | 6 (42.9%) | |
| Continuous + Interrupted | 29 (51.8%) | 8 (57.1%) | |
| Complications | 4 (7.1%) | 0 (0%) | N/A |
| Weight of specimen (g) | 103 [54.75–240.25] | 202 [99.25–376.75] | 0.13 |
| Author, Year | Study Design | Comparison Arms | Port Number | Largest Diameter | Myoma No | Myoma Weight | Hospital Stay (Day) | Operation Time (min) | Blood Loss (mL) | Follow up Duration | Clinical Pregnancy Rate | Live Birth Rate/Ongoing Pregnancy Rate | Complication Operation/Ut Rupture in Pregnancy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lonnerfors 2011 [12] | Prospective observational study | RALM (n = 31) Deep intramural myomas | 4 | 7 (4–11) | 1 (1–5) | N/A | 2 (1–3) | 132 (82–213) | 50 (25–200) | 42 m | 68% | 45.5%/9.7% | 22.6% (including minor ones)/0% |
| Cela 2013 [13] | Retrospective study | RALM (n = 48) | 4 | 7 (1.5–9) | 1 (1–7) | N/A | 2 (1–3) | 121 ± 46 | N/A | 6 m | 77.8% | 77.8% | N/A/0% |
| Tusheva 2013 [14] | Retrospective study | RALM (n = 30) | 4 | 6.5 ± 1.7 | 2.0 ± 1.0 | N/A | 0 days (discharged 2–4 h after surg) | 210.0 ± 53 | 100 (50–350) | N/A | 75% | 68.8%/0% | 0%/0% |
| Pitter 2015 [15] | Retrospective survey | RALM (n = 426) | 4 | N/A | N/A | N/A | N/A | N/A | N/A | 36 m | 50.8% | N/A | N/A/0.9% |
| Flyckt 2016 [16] | Retrospective Cohort study | RALM (n = 25) LM (n = 28) Open (n = 81) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 8 y | 50%/50%/66.7% (NS) | 50%/50%/56% (NS) | 14.8% */0% vs. 0% vs. 0% |
| Huberlant 2019 [17] | Retrospective cohort study | RALM (n = 53) | 4 | 6.9 ± 1.8 | 2 ± 1.57 | 173 ± 129.4 | 4.5 ± 0.8 | N/A | 260 ± 295 | 32 m | 52.8% | 41.5% | 15.1%/0% |
| Goldberg 2022 [18] | Retrospective case series | RALM (n = 123) | 4 | 8.9 ± 2.2 | 1 (1–3) | N/A | N/A | N/A | N/A | 1–6 y | 70.0% | 63.3%, 15.5% | N/A/0% (uterine rupture) |
| Morales 2022 [19] | Retrospective observational study | Robotic (n = 24), Laparoscopic (n = 24), Open (n = 21) myomectomy | N/A | 5.61 ± 4.63 vs. 4.22 ± 2.99 vs. 9.69 ± 7.91 (p = 0.004) | 3.85 ± 3.06 vs. 2.56 ± 1.7 vs. 9.24 ± 8.7 (p = 0.000) | 33.84 ± 76.70 vs. 21.6 ± 67.5 vs. 482.86 ± 1307 (p = 0.005) | 2.0 ± 0.85 vs. 1.88 ± 0.6 vs. 2.1 ± 0.3 (p = 0.525) | 189.85 ± 94.07 vs. 47.08 ± 98.3 vs. 42.86 ± 115.24 (p = 0.000) | 206.54 ± 360.17 vs. 224 ± 392.14 vs. 502.86 ± 733.05 (p = 0.097) | N/A (Time to pregnancy: 3.87 y) | 29.1% vs. 29.1% vs. 14.3% | 16.7% vs. 12/5% vs. 9.5% (NS) 8.3% vs. 12.5% vs. 0% | 0% vs. 0% vs. 4%/N/A |
| Present Study | Retrospective cohort study | RPRM (n = 401) | 3 | 7.8 ± 2.5 | 4.7 ± 4.1 | 235.3 ± 194.4 | 2.1 ± 0.6 | 103.7 ± 45.6 | 149.6 ± 180.2 | 24 m | 80.0% | 62.9%/7.1% | 11.2% (including minor ones)/0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paik, H.; Hong, Y.H.; Choi, Y.J.; Kim, S.K.; Lee, J.R.; Suh, C.S. Surgical and Fertility Outcomes of Reduced-Port Robotic Myomectomy: A Single-Center Experience of 401 Cases. J. Clin. Med. 2024, 13, 1807. https://doi.org/10.3390/jcm13061807
Paik H, Hong YH, Choi YJ, Kim SK, Lee JR, Suh CS. Surgical and Fertility Outcomes of Reduced-Port Robotic Myomectomy: A Single-Center Experience of 401 Cases. Journal of Clinical Medicine. 2024; 13(6):1807. https://doi.org/10.3390/jcm13061807
Chicago/Turabian StylePaik, Haerin, Yeon Hee Hong, Yae Ji Choi, Seul Ki Kim, Jung Ryeol Lee, and Chang Suk Suh. 2024. "Surgical and Fertility Outcomes of Reduced-Port Robotic Myomectomy: A Single-Center Experience of 401 Cases" Journal of Clinical Medicine 13, no. 6: 1807. https://doi.org/10.3390/jcm13061807
APA StylePaik, H., Hong, Y. H., Choi, Y. J., Kim, S. K., Lee, J. R., & Suh, C. S. (2024). Surgical and Fertility Outcomes of Reduced-Port Robotic Myomectomy: A Single-Center Experience of 401 Cases. Journal of Clinical Medicine, 13(6), 1807. https://doi.org/10.3390/jcm13061807





