Impact of Prosthetic Material and Restoration Type on Peri-Implant Bone Resorption: A Retrospective Analysis in a Romanian Sample
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Sample Selection
2.3. Assessment of Bone Resorption
2.4. Statistical Analysis
3. Results
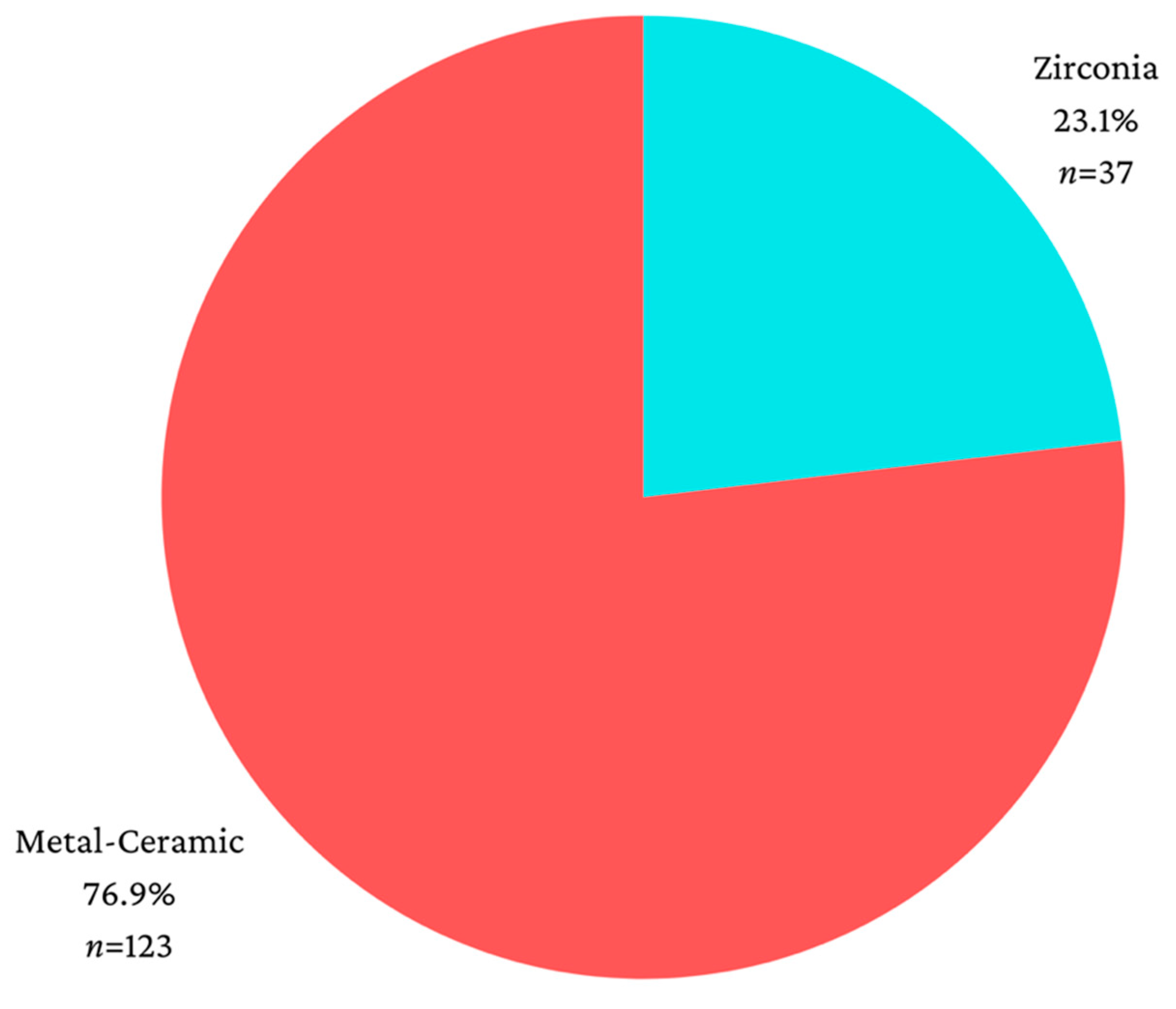
3.1. Sample Characteristics
3.2. Material Used for Prosthetic Restoration and Amount of Resorption
- For zirconia restorations, resorption in the mesial-vertical plane (median = 1.65, IQR = 0.93–2.43) was significantly higher than resorption in the mesial-horizontal plane (median = 0.56, IQR = 0–1.10) (p < 0.001) or compared to the resorption in the distal-horizontal plane (median = 0.51, IQR = 0–1.07) (p = 0.001).
- For zirconia restorations, resorption in the distal-vertical plane (median = 1.76, IQR = 1.01–2.57) was significantly higher compared to resorption in the mesial-horizontal plane (p < 0.001) or compared to the resorption in the distal-horizontal plane (p < 0.001).
- For metal-ceramic restorations, resorption in the mesial-vertical plane (median = 1.36, IQR = 0.24–2.35) was significantly higher than resorption in the mesial-horizontal plane (median = 0.54, IQR = 0–0.91) (p < 0.001) or compared to the resorption in the distal-horizontal plane (median = 0.49, IQR = 0–1.01) (p < 0.001).
- For metal-ceramic restorations, resorption in the distal-vertical plane (median = 1.65, IQR = 0.54–2.47) was significantly higher compared to the resorption in the mesial-horizontal plane (p < 0.001) or compared to the resorption in the distal-horizontal plane (p < 0.001).
| Resorption | Mean ± SD | Median (IQR) | p * | |
|---|---|---|---|---|
| Zirconia | Mesial-Vertical (p = 0.007 **) | 1.83 ± 1.42 | 1.65 (0.93–2.43) | <0.001 |
| Distal-Vertical (p = 0.466 **) | 1.74 ± 1.03 | 1.76 (1.01–2.57) | ||
| Mesial-Horizontal (p = 0.002 **) | 0.64 ± 0.62 | 0.56 (0–1.10) | ||
| Distal-Horizontal (p < 0.001 **) | 0.61 ± 0.63 | 0.51 (0–1.07) | ||
| Metal-Ceramic | Mesial-Vertical (p < 0.001 **) | 1.62 ± 1.49 | 1.36 (0.24–2.35) | <0.001 |
| Distal-Vertical (p < 0.001 **) | 1.73 ± 1.51 | 1.65 (0.54–2.47) | ||
| Mesial-Horizontal (p < 0.001 **) | 0.65 ± 0.77 | 0.54 (0–0.91) | ||
| Distal-Horizontal (p < 0.001 **) | 0.62 ± 0.69 | 0.49 (0–1.01) |
3.3. Type of Prosthetic Restoration and Amount of Resorption
- For single crowns, the resorption from the mesial-vertical plane (median = 1.58, IQR = 0.24–2.31) was significantly higher than the resorption from the mesial-horizontal plane (median = 0.50, IQR = 0–0.95) (p < 0.001) or compared to the resorption from the distal-horizontal plane (median = 0.56, IQR = 0–1.19) (p = 0.001). Additionally, resorption from the distal-vertical plane (median = 1.74, IQR = 0.99–2.47) was significantly higher compared to the resorption from the mesial-horizontal plane (p < 0.001) or compared to the resorption from the distal-horizontal plane (p < 0.001).
- For connected crowns, the resorption from the mesial-vertical plane (median = 1.22, IQR = 0–2.34) was significantly higher than the resorption from the mesial-horizontal plane (median = 0.53, IQR = 0–0.94) (p < 0.001) or compared to the resorption from the distal-horizontal plane (median = 0.31, IQR = 0–1.02) (p < 0.001). Furthermore, resorption from the distal-vertical plane (median = 1.39, IQR = 0–1.99) was significantly higher compared to the resorption from the mesial-horizontal plane (p < 0.001) or compared to the resorption from the distal-horizontal plane (p < 0.001).
- For dental bridges, the resorption from the mesial-vertical plane (median = 1.86, IQR = 0.74–2.79) was significantly higher than the resorption from the mesial-horizontal plane (median = 0.68, IQR = 0.42–1.10) (p = 0.007) or compared to the resorption from the distal-horizontal plane (median = 0.39, IQR = 0.22–0.87) (p < 0.001). Moreover, resorption from the distal-vertical plane (median = 1.90, IQR = 0.80–3.03) was significantly higher compared to the resorption from the mesial-horizontal plane (p < 0.001) or compared to the resorption from the distal-horizontal plane (p < 0.001) (Table 4).
3.4. Influence of Age, Gender, Implant Location, and Time Elapsed since Prosthetic Loading on Resorption
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jokstad, A.; Orstavik, J.; Ramstad, T. A Definition of Prosthetic Dentistry. Int. J. Prosthodont. 1998, 11, 295–301. [Google Scholar] [PubMed]
- Sorensen, J.A. The Evolution and Revolution in Prosthodontics Continues. Compend. Contin. Educ. Dent. 2016, 37, 402–404. [Google Scholar] [PubMed]
- Molinero-Mourelle, P.; Bischof, F.; Yilmaz, B.; Schimmel, M.; Abou-Ayash, S. Clinical Performance of Tooth Implant-Supported Removable Partial Dentures: A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2022, 26, 6003–6014. [Google Scholar] [CrossRef]
- Guillaume, B. Dental Implants: A Review. Morphologie 2016, 100, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Kim, N.H.; Shim, J.S. Fabrication of a complete, removable dental prosthesis from a digital intraoral impression for a patient with an excessively tight reconstructed lip after oral cancer treatment: A clinical report. J. Prosthet. Dent. 2017, 117, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Shrestha, B.; Chaudhari, B.K.; Suwal, P.; Singh, R.K. Knowledge, Awareness, and Attitude Regarding Dental Implants among Dental Interns. JNMA J. Nepal Med. Assoc. 2018, 56, 607–615. [Google Scholar] [CrossRef]
- Kashbour, W.A.; Rousseau, N.S.; Ellis, J.S.; Thomason, J.M. Patients’ experiences of dental implant treatment: A literature review of key qualitative studies. J. Dent. 2015, 43, 789–797. [Google Scholar] [CrossRef]
- Elsyad, M.A.; Agha, N.N.; Habib, A.A. Retention and Stability of Implant-Retained Mandibular Overdentures Using Different Types of Resilient Attachments: An In Vitro Study. Int. J. Oral Maxillofac. Implant. 2016, 31, 1040–1048. [Google Scholar] [CrossRef]
- Duong, H.Y.; Roccuzzo, A.; Stähli, A.; Salvi, G.E.; Lang, N.P.; Sculean, A. Oral health-related quality of life of patients rehabilitated with fixed and removable implant-supported dental prostheses. Periodontol. 2000 2022, 88, 201–237. [Google Scholar] [CrossRef]
- Vogel, R.; Smith-Palmer, J.; Valentine, W. Evaluating the health economic implications and cost-effectiveness of dental implants: A literature review. Int. J. Oral Maxillofac. Implant. 2013, 28, 343–356. [Google Scholar] [CrossRef]
- Sartoretto, S.C.; Shibli, J.A.; Javid, K.; Cotrim, K.; Canabarro, A.; Louro, R.S.; Lowenstein, A.; Mourão, C.F.; Moraschini, V. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J. Funct. Biomater. 2023, 14, 142. [Google Scholar] [CrossRef] [PubMed]
- Cristea, I.; Agop-Forna, D.; Martu, M.A.; Dascălu, C.; Topoliceanu, C.; Török, R.; Török, B.; Bardis, D.; Bardi, P.M.; Forna, N. Oral and Periodontal Risk Factors of Prosthetic Success for 3-Unit Natural Tooth-Supported Bridges versus Implant-Supported Fixed Dental Prostheses. Diagnostics 2023, 13, 852. [Google Scholar] [CrossRef] [PubMed]
- Lang-Hua, B.H.; Lang, N.P.; Lo, E.C.; McGrath, C.P. Attitudes of general dental practitioners towards implant dentistry in an environment with widespread provision of implant therapy. Clin. Oral Implant. Res. 2013, 24, 278–284. [Google Scholar] [CrossRef]
- Al-Haj Husain, A.; De Cicco, O.; Stadlinger, B.; Bosshard, F.A.; Schmidt, V.; Özcan, M.; Valdec, S. A Survey on Attitude, Awareness, and Knowledge of Patients Regarding the Use of Dental Implants at a Swiss University Clinic. Dent. J. 2023, 11, 165. [Google Scholar] [CrossRef]
- Sabău, D.T.; Juncar, R.I.; Moca, A.E.; Juncar, M. The influence of the prosthetic abutments color in the aesthetics of the frontal teeth. A case report. Acta Stomatol. Marisiensis J. 2023, 6, 22–28. [Google Scholar] [CrossRef]
- Marconcini, S.; Giammarinaro, E.; Covani, U.; Mascolo, A.; Caso, G.; Del Corso, M. Immediate restoration of fixed full-arch prostheses placed on implants in both fresh and healed sockets using the flat one-bridge technique: A 7-year retrospective study. BMC Oral Health 2021, 21, 617. [Google Scholar] [CrossRef] [PubMed]
- Ionescu, R.N.; Totan, A.R.; Imre, M.M.; Țâncu, A.M.C.; Pantea, M.; Butucescu, M.; Farcașiu, A.T. Prosthetic Materials Used for Implant-Supported Restorations and Their Biochemical Oral Interactions: A Narrative Review. Materials 2022, 15, 1016. [Google Scholar] [CrossRef]
- Sanz-Martín, I.; Sanz-Sánchez, I.; Carrillo de Albornoz, A.; Figuero, E.; Sanz, M. Effects of modified abutment characteristics on peri-implant soft tissue health: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 118–129. [Google Scholar] [CrossRef]
- Hosseini, M.; Worsaae, N.; Gotfredsen, K. A 5-year randomized controlled trial comparing zirconia-based versus metal-based implant-supported single-tooth restorations in the premolar region. Clin. Oral Implant. Res. 2022, 33, 792–803. [Google Scholar] [CrossRef]
- van Brakel, R.; Meijer, G.J.; Verhoeven, J.W.; Jansen, J.; de Putter, C.; Cune, M.S. Soft tissue response to zirconia and titanium implant abutments: An in vivo within-subject comparison. J. Clin. Periodontol. 2012, 39, 995–1001. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Serra-Pastor, B.; Roig-Vanaclocha, A.; Fons-Font, A.; Solá-Ruiz, M.F. Fracture resistance and the mode of failure produced in metal-free crowns cemented onto zirconia abutments in dental implants. PLoS ONE 2019, 14, e0220551. [Google Scholar] [CrossRef]
- Carames, J.; Tovar Suinaga, L.; Yu, Y.C.; Pérez, A.; Kang, M. Clinical Advantages and Limitations of Monolithic Zirconia Restorations Full Arch Implant Supported Reconstruction: Case Series. Int. J. Dent. 2015, 2015, 392496. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Valente, N.A.; Strasding, M.; Zwahlen, M.; Liu, S.; Sailer, I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 199–214. [Google Scholar] [CrossRef]
- Limmer, B.; Sanders, A.E.; Reside, G.; Cooper, L.F. Complications and Patient-Centered Outcomes with an Implant-Supported Monolithic Zirconia Fixed Dental Prosthesis: 1 Year Results. J. Prosthodont. 2014, 23, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Rokaya, D.; Srimaneepong, V.; Wisitrasameewon, W.; Humagain, M.; Thunyakitpisal, P. Peri-implantitis Update: Risk Indicators, Diagnosis, and Treatment. Eur. J. Dent. 2020, 14, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Prasad, K.D.; Shetty, M.; Bansal, N.; Hegde, C. Platform switching: An answer to crestal bone loss. J. Dent. Implant. 2011, 1, 13–17. [Google Scholar]
- Berglundh, T.; Lindhe, J.; Ericsson, I.; Marinello, C.P.; Liljenberg, B.; Thornsen, P. The soft tissue barrier at implants and teeth. Clin. Oral Implant. Res. 1991, 2, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Mattheos, N.; Vergoullis, I.; Janda, M.; Miseli, A. The Implant Supracrestal Complex and Its Significance for Long-Term Successful Clinical Outcomes. Int. J. Prosthodont. 2021, 34, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Marrone, A.; Lasserre, J.; Bercy, P.; Brecx, M.C. Prevalence and risk factors for peri-implant disease in Belgian adults. Clin. Oral Implant. Res. 2013, 24, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Elemek, E.; Agrali, O.B.; Kuru, B.; Kuru, L. Peri-implantitis and Severity Level. Eur. J. Dent. 2020, 14, 24–30. [Google Scholar] [CrossRef][Green Version]
- Klotz, A.L.; Grill, S.K.; Hassel, A.J.; Rammelsberg, P.; Ze Nthofer, A. Differences Between the Oral Health of People Aged 50 and 70 Years—An Exploratory Cohort Study. Oral Health Prev. Dent. 2020, 18, 239–243. [Google Scholar] [CrossRef]
- Barbe, A.G.; Javadian, S.; Rott, T.; Scharfenberg, I.; Deutscher, H.C.D.; Noack, M.J.; Derman, S.H.M. Objective masticatory efficiency and subjective quality of masticatory function among patients with periodontal disease. J. Clin. Periodontol. 2020, 47, 1344–1353. [Google Scholar] [CrossRef] [PubMed]
- Takeda, M.; Matsuda, Y.; Ikebuchi, K.; Takeda, M.; Abe, T.; Tominaga, K.; Isomura, M.; Nabika, T.; Kanno, T. Relationship between Oral Health Status and Bone Mineral Density in Community-Dwelling Elderly Individuals: A Cross-Sectional Study. Healthcare 2021, 9, 432. [Google Scholar] [CrossRef] [PubMed]
- Negri, M.; Galli, C.; Smerieri, A.; Macaluso, G.M.; Manfredi, E.; Ghiacci, G.; Toffoli, A.; Bonanini, M.; Lumetti, S. The effect of age, gender, and insertion site on marginal bone loss around endosseous implants: Results from a 3-year trial with premium implant system. Biomed. Res. Int. 2014, 2014, 369051. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, M.S.; Su, S.; Crespo, C.J.; Hung, M. Men and Oral Health: A Review of Sex and Gender Differences. Am. J. Mens Health 2021, 15, 15579883211016361. [Google Scholar] [CrossRef] [PubMed]
- Ajanović, M.; Hamzić, A.; Redžepagić, S.; Kamber-Ćesir, A.; Kazazić, L.; Tosum, S. Radiographic Evaluation of Crestal Bone Loss Around Dental Implants in Maxilla and Mandible: One Year Prospective Clinical Study. Acta Stomatol. Croat. 2015, 49, 128–136. [Google Scholar] [CrossRef]
- Anitua, E.; Alkhraisat, M.H. 15-year follow-up of short dental implants placed in the partially edentulous patient: Mandible Vs maxilla. Ann. Anat. 2019, 222, 88–93. [Google Scholar] [CrossRef]
- Vidal, R.; Greenwell, H.; Hill, M.; Papageorgakopoulos, G.; Scheetz, J.P. Success rate of immediate implants placed and restored by novice operators. Implant. Dent. 2010, 19, 81–90. [Google Scholar] [CrossRef]
- Dorj, O.; Lin, C.K.; Salamanca, E.; Pan, Y.H.; Wu, Y.F.; Hsu, Y.S.; Lin, J.C.; Lin, H.K.; Chang, W.J. Marginal Bone Loss around Implant-Retaining Overdentures versus Implant-Supported Fixed Prostheses 12-Month Follow-Up: A Retrospective Study. Int. J. Environ. Res. Public Health 2022, 19, 1750. [Google Scholar] [CrossRef]
- Cinquini, C.; Alfonsi, F.; Marchio, V.; Gallo, F.; Zingari, F.; Bolzoni, A.R.; Romeggio, S.; Barone, A. The Use of Zirconia for Implant-Supported Fixed Complete Dental Prostheses: A Narrative Review. Dent. J. 2023, 11, 144. [Google Scholar] [CrossRef]
| Material | Mean ± SD | Median (IQR) | Medium Rank | p * |
|---|---|---|---|---|
| Mesial-Vertical | ||||
| Zirconia (p = 0.007 **) | 1.83 ± 1.42 | 1.65 (0.93–2.43) | 86.65 | 0.355 |
| Metal-ceramic (p < 0.001 **) | 1.62 ± 1.49 | 1.36 (0.24–2.35) | 78.65 | |
| Distal-Vertical | ||||
| Zirconia (p = 0.466 **) | 1.74 ± 1.03 | 1.76 (1.01–2.57) | 85.46 | 0.456 |
| Metal-ceramic (p < 0.001 **) | 1.73 ± 1.51 | 1.65 (0.54–2.47) | 79.01 | |
| Mesial-Horizontal | ||||
| Zirconia (p = 0.002 **) | 0.64 ± 0.62 | 0.56 (0–1.10) | 82.22 | 0.794 |
| Metal-ceramic (p < 0.001 **) | 0.65 ± 0.77 | 0.54 (0–0.91) | 79.98 | |
| Distal-Horizontal | ||||
| Zirconia (p < 0.001 **) | 0.61 ± 0.63 | 0.51 (0–1.07) | 81.05 | 0.932 |
| Metal-ceramic (p < 0.001 **) | 0.62 ± 0.69 | 0.49 (0–1.01) | 80.33 | |
| Restoration | Mean ± SD | Median (IQR) | Medium Rank | p * |
|---|---|---|---|---|
| Mesial-Vertical | ||||
| Single crown (p < 0.001 **) | 1.59 ± 1.48 | 1.58 (0.24–2.31) | 77.87 | 0.217 |
| Connected crowns (p < 0.001 **) | 1.53 ± 1.43 | 1.22 (0–2.34) | 75.88 | |
| Bridge (p = 0.025 **) | 1.98 ± 1.53 | 1.86 (0.74–2.79) | 91.24 | |
| Distal-Vertical | ||||
| Single crown (p < 0.001 **) | 1.81 ± 1.44 | 1.74 (0.99–2.47) | 83.44 | 0.026 |
| Connected crowns (p < 0.001 **) | 1.43 ± 1.28 | 1.39 (0–1.99) | 69.45 | |
| Bridge (p = 0.029 **) | 2.10 ± 1.51 | 1.90 (0.80–3.03) | 93.82 | |
| Mesial-Horizontal | ||||
| Single crown (p < 0.001 **) | 0.56 ± 0.56 | 0.5 (0.5–0.95) | 76.90 | 0.055 |
| Connected crowns (p < 0.001 **) | 0.55 ± 0.64 | 0.53 (0–0.94) | 74.20 | |
| Bridge (p < 0.001 **) | 0.93 ± 1.00 | 0.68 (0.42–1.10) | 95.16 | |
| Distal-Horizontal | ||||
| Single crown (p < 0.001 **) | 0.68 ± 0.68 | 0.56 (0–1.19) | 85.33 | 0.283 |
| Connected crowns (p < 0.001 **) | 0.54 ± 0.69 | 0.31 (0–1.02) | 73.55 | |
| Bridge (p < 0.001 **) | 0.65 ± 0.66 | 0.39 (0.22–0.87) | 84.88 | |
| Resorbtion | Mean ± SD | Median (IQR) | p * | |
|---|---|---|---|---|
| Single | Mesial-Vertical (p < 0.001 **) | 1.59 ± 1.48 | 1.58 (0.24–2.31) | <0.001 |
| Distal-Vertical (p < 0.001 **) | 1.81 ± 1.44 | 1.74 (0.99–2.47) | ||
| Mesial-Horizontal (p < 0.001 **) | 0.56 ± 0.56 | 0.50 (0–0.95) | ||
| Distal-Horizontal (p < 0.001 **) | 0.68 ± 0.68 | 0.56 (0–1.19) | ||
| Connected | Mesial-Vertical (p < 0.001 **) | 1.53 ± 1.43 | 1.22 (0–2.34) | <0.001 |
| Distal-Vertical (p < 0.001 **) | 1.43 ± 1.28 | 1.39 (0–1.99) | ||
| Mesial-Horizontal (p < 0.001 **) | 0.55 ± 0.64 | 0.53 (0–0.94) | ||
| Distal-Horizontal (p < 0.001 **) | 0.54 ± 0.69 | 0.31 (0–1.02) | ||
| Bridge | Mezial-Vertical (p = 0.025 **) | 1.98 ± 1.53 | 1.86 (0.74–2.79) | <0.001 |
| Distal-Vertical (p = 0.029 **) | 2.10 ± 1.51 | 1.90 (0.80–3.03) | ||
| Mezial-Orizontal (p < 0.001 **) | 0.93 ± 1.00 | 0.68 (0.42–1.10) | ||
| Distal-Orizontal (p < 0.001 **) | 0.65 ± 0.66 | 0.39 (0.22–0.87) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sabău, D.T.; Juncar, R.I.; Moca, A.E.; Bota, T.; Moca, R.T.; Juncar, M. Impact of Prosthetic Material and Restoration Type on Peri-Implant Bone Resorption: A Retrospective Analysis in a Romanian Sample. J. Clin. Med. 2024, 13, 1794. https://doi.org/10.3390/jcm13061794
Sabău DT, Juncar RI, Moca AE, Bota T, Moca RT, Juncar M. Impact of Prosthetic Material and Restoration Type on Peri-Implant Bone Resorption: A Retrospective Analysis in a Romanian Sample. Journal of Clinical Medicine. 2024; 13(6):1794. https://doi.org/10.3390/jcm13061794
Chicago/Turabian StyleSabău, Denisa Tabita, Raluca Iulia Juncar, Abel Emanuel Moca, Teofana Bota, Rahela Tabita Moca, and Mihai Juncar. 2024. "Impact of Prosthetic Material and Restoration Type on Peri-Implant Bone Resorption: A Retrospective Analysis in a Romanian Sample" Journal of Clinical Medicine 13, no. 6: 1794. https://doi.org/10.3390/jcm13061794
APA StyleSabău, D. T., Juncar, R. I., Moca, A. E., Bota, T., Moca, R. T., & Juncar, M. (2024). Impact of Prosthetic Material and Restoration Type on Peri-Implant Bone Resorption: A Retrospective Analysis in a Romanian Sample. Journal of Clinical Medicine, 13(6), 1794. https://doi.org/10.3390/jcm13061794








