Effects of Telerehabilitation Combining Diaphragmatic Breathing Re-Education and Shoulder Stabilization Exercises on Neck Pain, Posture, and Function in Young Adult Men with Upper Crossed Syndrome: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
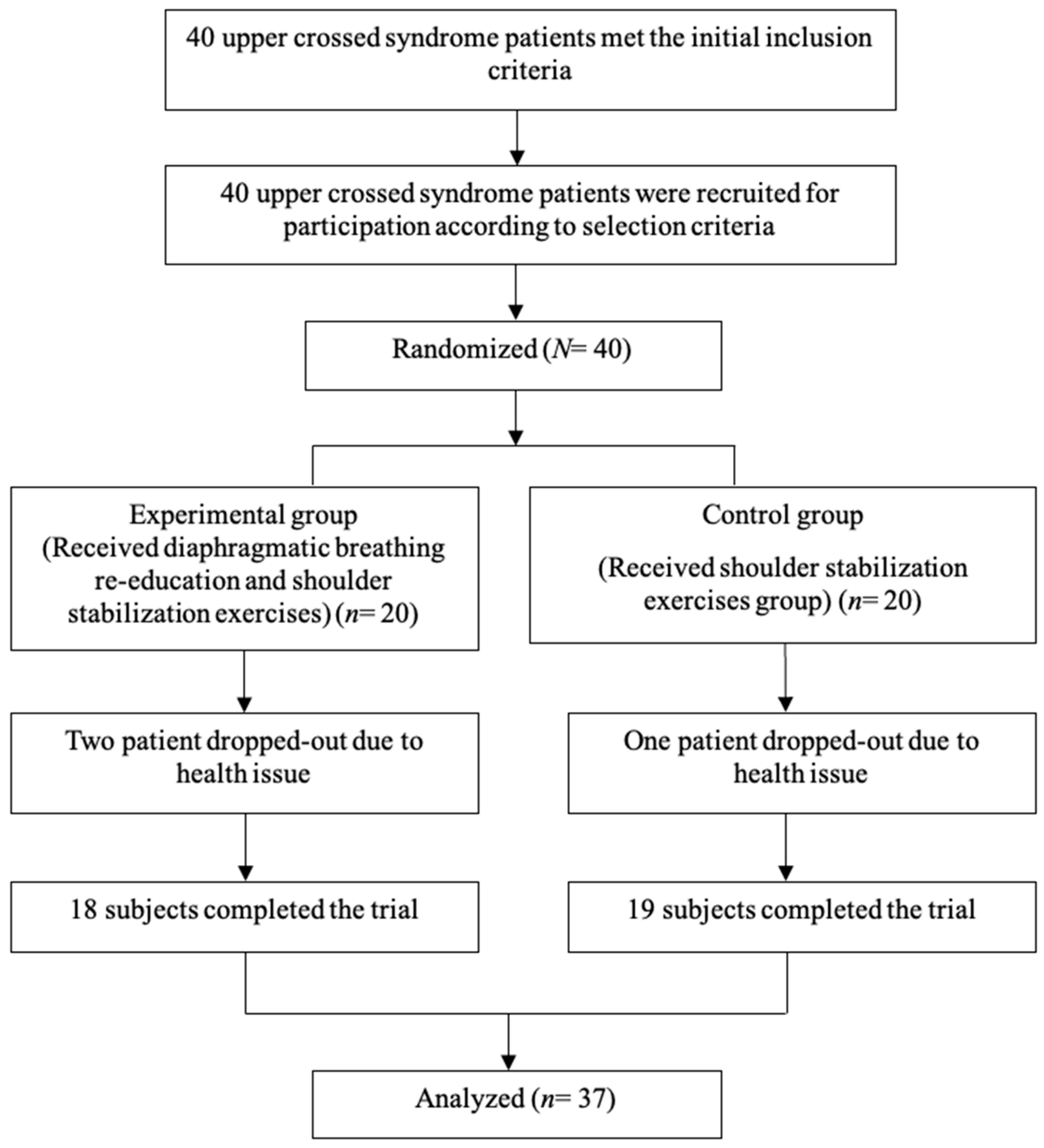
2.1. Subjects
2.2. Experimental Procedure
2.3. Training Program
2.3.1. Diaphragmatic Breathing Re-Education Program
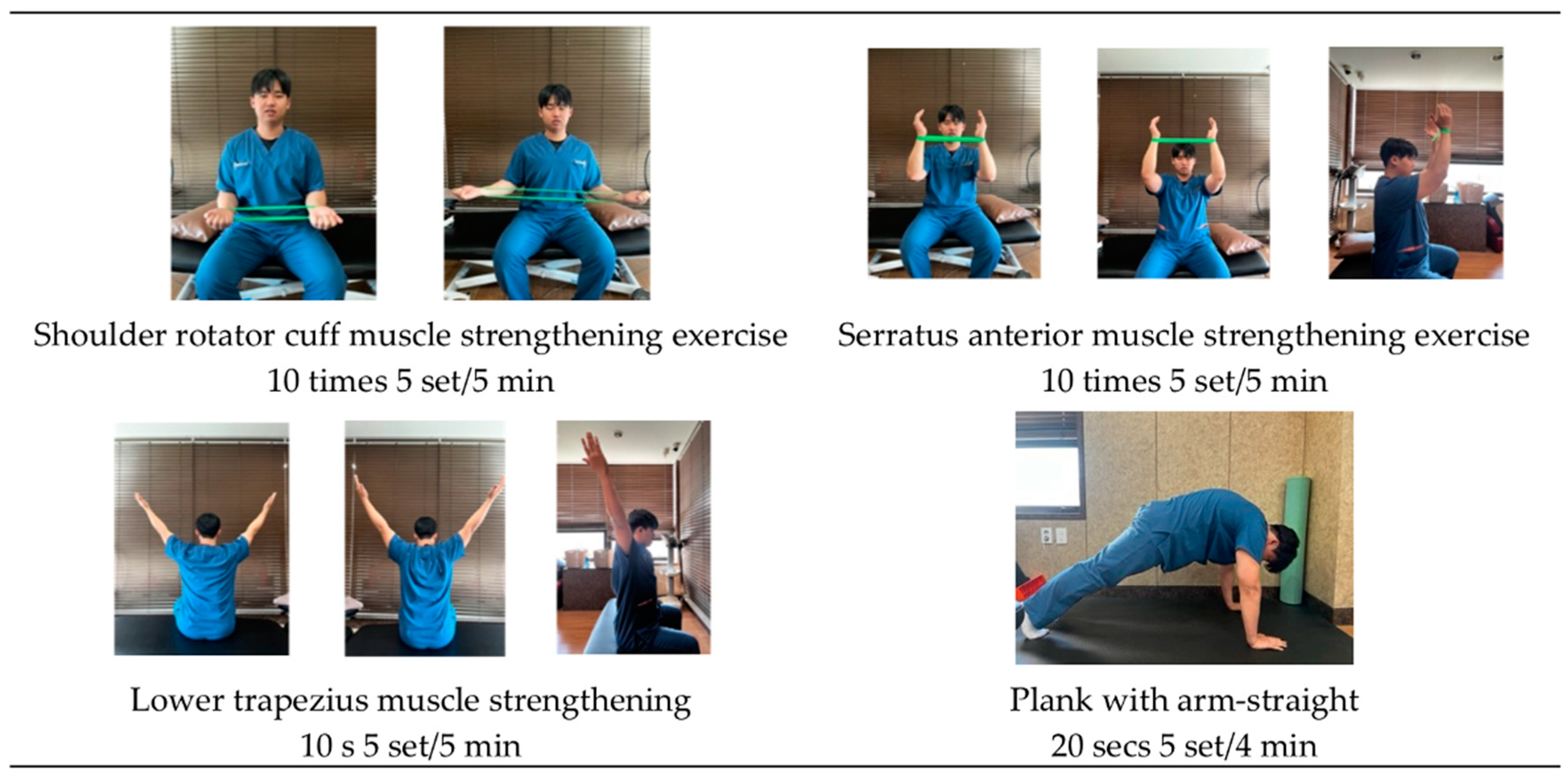
2.3.2. Shoulder Stabilization Exercises Program
2.3.3. Outcome Measures
2.3.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Janda, V. Muscles and Motor Control in Cervicogenic Disorders; Churchill Livingstone: New York, NY, USA, 1994; pp. 195–216. [Google Scholar]
- Yong, M.S.; Lee, H.Y.; Lee, M.Y. Correlation between head posture and proprioceptive function in the cervical region. J. Phys. Ther. Sci. 2016, 28, 857–860. [Google Scholar] [CrossRef]
- Shaghayeghfard, B.; Ahmadi, A.; Maroufi, N.; Sarrafzadeh, J. Evaluation of forward head posture in sitting and standing positions. Eur. Spine J. 2016, 25, 3577–3582. [Google Scholar] [CrossRef]
- Kim, K.H.; Kim, S.G.; Hwangbo, G. The effects of horse-riding simulator exercise and Kendall exercise on the forward head posture. J. Phys. Ther. Sci. 2015, 27, 1125–1127. [Google Scholar] [CrossRef]
- Harman, K.; Hubley-Kozey, C.L.; Butler, H. Effectiveness of an Exercise Program to Improve Forward Head Posture in Normal Adults: A Randomized, Controlled 10-Week Trial. J. Man. Manip. Ther. 2013, 13, 163–176. [Google Scholar] [CrossRef]
- Lee, M.Y.; Lee, H.Y.; Yong, M.S. Characteristics of cervical position sense in subjects with forward head posture. J. Phys. Ther. Sci. 2014, 26, 1741–1743. [Google Scholar] [CrossRef] [PubMed]
- Deodato, M.; Granato, A.; Borgino, C.; Galmonte, A.; Manganotti, P. Instrumental assessment of physiotherapy and onabolulinumtoxin-A on cervical and headache parameters in chronic migraine. Neurol. Sci. 2021, 43, 2021–2029. [Google Scholar] [CrossRef] [PubMed]
- Okuro, R.T.; Morcillo, A.M.; Ribeiro, M.Â.G.O.; Sakano, E.; Conti, P.B.M.; Ribeiro, J.D. Mouth breathing and forward head posture: Effects on respiratory biomechanics and exercise capacity in children. J. Bras. Pneumol. Publicacao Soc. Bras. Pneumol. Tisilogia 2011, 37, 471–479. [Google Scholar] [CrossRef]
- Zafar, H.; Albarrati, A.; Alghadir, A.H.; Iqbal, Z.A. Effect of Different Head-Neck Postures on the Respiratory Function in Healthy Males. BioMed Res. Int. 2018, 2018, 4518269. [Google Scholar] [CrossRef] [PubMed]
- Sahrmann, S.; Azevedo, D.C.; Van Dillen, L. Diagnosis and treatment of movement system impairment syndromes. Braz. J. Phys. Ther. 2017, 21, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadis, Z.; Kapreli, E.; Strimpakos, N.; Oldham, J. Respiratory weakness in patients with chronic neck pain. Man. Ther. 2013, 18, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Lynch, S.S.; Thigpen, C.A.; Mihalik, J.P.; Prentice, W.E.; Padua, D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br. J. Sports Med. 2010, 44, 376–381. [Google Scholar] [CrossRef]
- Finley, M.A.; Lee, R.Y. Effect of sitting posture on 3-dimensional scapular kinematics measured by skin-mounted electromagnetic tracking sensors. Arch. Phys. Med. Rehabil. 2003, 84, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Kibler, W.B. Rehabilitation of rotator cuff tendinopathy. Clin. Sports Med. 2003, 22, 837–847. [Google Scholar] [CrossRef]
- Kebaetse, M.; McClure, P.; Pratt, N.A. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch. Phys. Med. Rehabil. 1999, 80, 945–950. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.; Kamboj, R.; Pawalia, A. Effect of Interferential Therapy and Elastic Band Exercises on Subjects with Round Shoulder and Forward Head Posture: A Randomized Trial. J. Dow Univ. Health Sci. 2022, 16, 59–65. Available online: https://www.jduhs.com/index.php/jduhs/article/view/1639 (accessed on 27 February 2024). [CrossRef]
- Bordoni, B.; Marelli, F.; Morabito, B.; Sacconi, B. Manual evaluation of the diaphragm muscle. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 1949–1956. [Google Scholar] [CrossRef] [PubMed]
- Kocjan, J.; Adamek, M.; Gzik-Zroska, B.; Czyżewski, D.; Rydel, M. Network of breathing. Multifunctional role of the diaphragm: A review. Adv. Respir. Med. 2017, 85, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Anwar, S.; Arsalan, S.A.; Zafar, H.; Ahmed, A.; Gillani, S.A.; Hanif, A. Effects of breathing re-education on endurance, strength of deep neck flexors and pulmonary function in patients with chronic neck pain: A randomised controlled trial. S. Afr. J. Physiother. 2022, 78, 1611. [Google Scholar] [CrossRef]
- Özden, F.; Özkeskin, M.; Ak, S.M. Physical exercise intervention via telerehabilitation in patients with neurological disorders: A narrative literature review. Egypt. J. Neurol. Psychiatry Neurosurg. 2022, 58, 26. [Google Scholar] [CrossRef]
- Van Egmond, M.A.; Van Der Schaaf, M.; Vredeveld, T.; Vollenbroek-Hutten, M.M.R.; van Berge Henegouwen, M.I.; Klinkenbijl, J.H.G.; Engelbert, R.H.H. Effectiveness of physiotherapy with telerehabilitation in surgical patients: A systematic review and meta-analysis. Physiotherapy 2018, 104, 277–298. [Google Scholar] [CrossRef]
- Jachak, S.P.; Phansopkar, P.A.; Naqvi, W.M.; Kumar, K. Great awakening-Telerehabilitation in physiotherapy during pandemic and impact of COVID-19. J. Evol. Med. Dent. Sci. 2020, 9, 3387–3393. [Google Scholar] [CrossRef]
- Rodríguez-Huguet, M.; Gil-Salú, J.L.; Rodríguez-Huguet, P.; Cabrera-Afonso, J.R.; Lomas-Vega, R. Effects of Myofascial Release on Pressure Pain Thresholds in Patients with Neck Pain: A Single-Blind Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2018, 97, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.H.; Hwang, U.J.; Kim, J.H.; Gwak, G.T.; Kwon, O.Y. Effect of improved thoracic kyphosis on forward shoulder posture after mobilization in individuals with thoracic hyperkyphosis—Clinical Biomechanics. Clin. Biomech. 2022, 97, 105707. [Google Scholar] [CrossRef] [PubMed]
- Jhung, Y.J.; Park, S.B.; Kim, M.J. Comparison between Computerized Inclinometer and Manual Inclinometer in Measuring Whole Spinal Range of Motion. J. Korean Acad. Rehabil. Med. 2002, 26, 456–460. [Google Scholar]
- Yana, B.; Koch, M.; Kalita, A.; Dutta, A. To Study the Effects of Deep Neck Flexor Strengthening Exercises and Mckenzie Neck Exercises on Smart Phone Users Suffering from Neck Pain: A Comparative Study. Int. J. Pharma Bio Sci. 2021, 11, 261–267. [Google Scholar] [CrossRef]
- Asadpour, E.; Mohammad Rahimi, N.; Aminzadeh, R. Effectiveness of Functional Training on Respiratory Function and Functional Movements among Female Bodybuilders. Phys. Treat.-Specif. Phys. Ther. J. 2023, 13, 267–278. [Google Scholar] [CrossRef]
- Kim, S.H.; Ko, Y.M.; Park, J.W.; Youn, J.I. Quantitative Analysis of Myofascial Pain Syndrome in Trapezius Muscle Using Pressure Algometer and Surface Electromyography. J. Korean Phys. Ther. 2021, 33, 258–263. [Google Scholar] [CrossRef]
- Walton, D.; MacDermid, J.; Nielson, W.; Teasell, R.; Reese, H.; Levesque, L. Pressure Pain Threshold Testing Demonstrates Predictive Ability in People with Acute Whiplash. J. Orthop. Sports Phys. Ther. 2011, 41, 658–665. [Google Scholar] [CrossRef]
- Chesterton, L.S.; Sim, J.; Wright, C.C.; Foster, N.E. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin. J. Pain 2007, 23, 760–766. [Google Scholar] [CrossRef]
- Kinser, A.M.; Sands, W.A.; Stone, M.H. Reliability and validity of a pressure algometer. J. Strength Cond. Res. 2009, 23, 312–314. [Google Scholar] [CrossRef]
- Raine, S.; Twomey, L.T. Head and shoulder posture variations in 160 asymptomatic women and men. Arch. Phys. Med. Rehabil. 1997, 78, 1215–1223. [Google Scholar] [CrossRef]
- Gallego-Izquierdo, T.; Arroba-Díaz, E.; García-Ascoz, G.; Val-Cano, M.d.A.; Pecos-Martin, D.; Cano-de-la-Cuerda, R. Psychometric Proprieties of a Mobile Application to Measure the Craniovertebral Angle a Validation and Reliability Study. Int. J. Environ. Res. Public Health 2020, 17, 6521. [Google Scholar] [CrossRef] [PubMed]
- Kluemper, M.; Uhl, T.; Hazelrigg, H. Effect of Stretching and Strengthening Shoulder Muscles on Forward Shoulder Posture in Competitive Swimmers. J. Sport Rehabil. 2006, 15, 58–70. [Google Scholar] [CrossRef]
- Macdougall, J.; Wenger, H.; Green, H. Physiological Testing of the High-Performance Athlete; Human Kinetics Books: Champaign, IL, USA, 1991. [Google Scholar]
- KJ, S.; BW, C.; BR, C.; GB, S. Cross-cultural adaptation and validation of the Korean version of the neck disability index. Spine 2010, 35, E1045–E1049. [Google Scholar] [CrossRef]
- Davies, G.J.; Zillmer, D.A. Functional Progression of Exercise during Rehabilitation. In Book: Knee Ligament Rehabilitation; Churchill-Livingston: New York, NY, USA, 2000; Chapter 25; pp. 345–360. [Google Scholar]
- Dayson, M. The Relationship between Baseline and Physical Performance Screening Tests, and Game Performance Outcomes in Elite Youth Basketball; University of Kent: Canterbury, UK, 2021. [Google Scholar]
- Lee, D.R.; Kim, L.J. Reliability and validity of the closed kinetic chain upper extremity stability test. J. Phys. Ther. Sci. 2015, 27, 1071–1073. [Google Scholar] [CrossRef] [PubMed]
- Paccione, C.E.; Jacobsen, H.B. Motivational Non-directive Resonance Breathing as a Treatment for Chronic Widespread Pain. Front. Psychol. 2019, 10, 1027. [Google Scholar] [CrossRef]
- Lee, Y.; Shin, M.M.S.; Lee, W. Effects of shoulder stabilization exercise on pain and function in patients with neck pain. J. Phys. Ther. Sci. 2015, 27, 3619–3622. [Google Scholar] [CrossRef]
- Dareh-Deh, H.R.; Hadadnezhad, M.; Letafatkar, A.; Peolsson, A. Therapeutic routine with respiratory exercises improves posture, muscle activity, and respiratory pattern of patients with neck pain: A randomized controlled trial. Sci. Rep. 2022, 12, 4149. [Google Scholar] [CrossRef]
- Kim, M.S.; Cha, Y.J.; Choi, J.D. Correlation between forward head posture, respiratory functions, and respiratory accessory muscles in young adults. J. Back Musculoskelet. Rehabil. 2017, 30, 711–715. [Google Scholar] [CrossRef]
- Kang, J.I.; Jeong, D.K.; Choi, H. The effect of feedback respiratory exercise on muscle activity, craniovertebral angle, and neck disability index of the neck flexors of patients with forward head posture. J. Phys. Ther. Sci. 2016, 28, 2477–2481. [Google Scholar] [CrossRef]
- Ricoy, J.; Rodríguez-Núñez, N.; Álvarez-Dobaño, J.M.; Toubes, M.E.; Riveiro, V.; Valdés, L. Diaphragmatic dysfunction. Pulmonology 2019, 25, 223–235. [Google Scholar] [CrossRef]
- Fogarty, M.J.; Mantilla, C.B.; Sieck, G.C. Breathing: Motor Control of Diaphragm Muscle. Physiology 2018, 33, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Wallden, M. The diaphragm—More than an inspired design. J. Bodyw. Mov. Ther. 2017, 21, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Shaw, I.; Shaw, B.S.; Brown, G.A. Role of diaphragmatic breathing and aerobic exercise in improving pulmonary function and maximal oxygen consumption in asthmatics. Sci. Sports 2010, 25, 139–145. [Google Scholar] [CrossRef]
- Hamasaki, H. Effects of Diaphragmatic Breathing on Health: A Narrative Review. Medicines 2020, 7, 65. [Google Scholar] [CrossRef] [PubMed]
- Yaghoubitajani, Z.; Gheitasi, M.; Bayattork, M.; Andersen, L.L. Corrective exercises administered online vs. at the workplace for pain and function in the office workers with upper crossed syndrome: Randomized controlled trial. Int. Arch. Occup. Environ. Health 2022, 95, 1703–1718. [Google Scholar] [CrossRef]
- Shah, N.; Shetty, G.M.; Kanna, R.; Thakur, H. Efficacy of telerehabilitation for spine pain during the Coronavirus pandemic lockdown: A retrospective propensity score-matched analysis. Disabil. Rehabil. Assist. Technol. 2022, 1–8. [Google Scholar] [CrossRef]
- Mustian, K.M.; Peppone, L.; Darling, T.V.; Palesh, O.; Heckler, C.E.; Morrow, G.R. A 4-week home-based aerobic and resistance exercise program during radiation therapy: A pilot randomized clinical trial. J. Support. Oncol. 2009, 7, 158. [Google Scholar]
- Kanyılmaz, T.; Topuz, O.; Ardıç, F.N.; Alkan, H.; Öztekin, S.N.S.; Topuz, B.; Ardıç, F. Effectiveness of conventional versus virtual reality-based vestibular rehabilitation exercises in elderly patients with dizziness: A randomized controlled study with 6-month follow-up. Braz. J. Otorhinolaryngol. 2022, 88 (Suppl. S3), S41–S49. [Google Scholar] [CrossRef]

| Characteristics | Experimental Group (n = 18) | Control Group (n = 19) | t (p) |
|---|---|---|---|
| Age (years) | 29.78 ± 1.89 | 29.95 ± 2.63 | −0.224 (0.824) |
| Height (cm) | 176.38 ± 4.59 | 176.84 ± 6.98 | −0.232 (0.818) |
| Weight (kg) | 81.22 ± 9.53 | 81.89 ± 8.41 | −0.228 (0.821) |
| Variable | Experimental Group (n = 18) | Control Group (n = 19) | t (p) | Time F (p) | Group F (p) | Time × Group F (p) | |
|---|---|---|---|---|---|---|---|
| Lt. PPT (kg/cm2) | Pretest | 2.27 ± 0.39 | 2.20 ± 0.40 | 0.586 (0.561) | |||
| Post-test | 2.75 ± 0.51 | 2.47 ± 0.30 | |||||
| Mean difference | 0.47 ± 0.31 | 0.27 ± 0.18 | 81.214 (0.001) | 1.839 (0.157) | 5.377 (0.026) | ||
| 95% CI for difference | (0.31 to 0.62) | (0.19 to 0.36) | |||||
| t (p) | −6.419 (0.001) | −6.707 (0.001) | |||||
| Rt. PPT (kg/cm2) | Pretest | 2.30 ± 0.43 | 2.24 ± 0.31 | 0.510 (0.614) | |||
| Post-test | 2.68 ± 0.44 | 2.34 ± 0.25 | |||||
| Mean difference | 0.37 ± 0.28 | 0.10 ± 0.21 | 34.617 (0.001) | 3.088 (0.088) | 11.018 (0.002) | ||
| 95% CI for difference | (0.23 to 0.51) | (0.001 to 0.20) | |||||
| t (p) | −5.685 (0.001) | −2.137 (0.047) | |||||
| Variable | Experimental Group (n = 18) | Control Group (n = 19) | t (p) | Time F (p) | Group F (p) | Time × Group F (p) | |
|---|---|---|---|---|---|---|---|
| CVA (degrees, °) | Pretest | 48.11 ± 3.32 | 46.68 ± 4.20 | 1.141 (0.262) | |||
| Post-test | 52.11 ± 3.67 | 48.36 ± 3.98 | |||||
| Mean difference | 4.00 ± 2.91 | 1.68 ± 1.60 | 54.984 (0.001) | 4.663 (0.038) | 9.126 (0.005) | ||
| 95% CI for difference | (−5.44 to −2.55) | (−2.45 to −0.91) | |||||
| t (p) | −5.831 (0.001) | −4.587 (0.001) | |||||
| STD (degrees, °) | Pretest | 4.22 ± 1.66 | 4.00 ± 1.73 | 0.397 (0.693) | |||
| Post-test | 1.38 ± 0.50 | 3.00 ± 1.47 | |||||
| Mean difference | 2.83 ± 1.72 | 1.00 ± 1.85 | 42.256 (0.001) | 3.501 (0.070) | 9.665 (0.004) | ||
| 95% CI for difference | (1.97 to 3.69) | (0.10 to 1.89) | |||||
| t (p) | 6.974 (0.001) | 2.349 (0.030) | |||||
| Lt. RSP (mm) | Pretest | 86.72 ± 11.29 | 85.15 ± 6.54 | 0.519 (0.607) | |||
| Post-test | 74.66 ± 11.44 | 79.00 ± 6.48 | |||||
| Mean difference | 12.05 ± 12.66 | 6.15 ± 4.53 | 34.625 (0.001) | 0.284 (0.598) | 3.630 (0.065) | ||
| 95% CI for difference | (5.75 to 18.35) | (3.97 to 8.34) | |||||
| t (p) | 4.037 (0.001) | 5.916 (0.001) | |||||
| Rt. RSP (mm) | Pretest | 90.66 ± 10.24 | 88.68 ± 7.28 | 0.681 (0.500) | |||
| Post-test | 78.00 ± 9.13 | 81.52 ± 7.52 | |||||
| Mean difference | 12.66 ± 10.12 | 7.15 ± 6.70 | 49.811 (0.001) | 0.099 (0.755) | 3.846 (0.058) | ||
| 95% CI for difference | (7.62 to 17.70) | (3.92 to 10.38) | |||||
| t (p) | 5.306 (0.001) | 4.655 (0.001) | |||||
| Variable | Experimental Group (n = 18) | Control Group (n = 19) | t (p) | Time F (p) | Group F (p) | Time × Group F (p) | |
|---|---|---|---|---|---|---|---|
| NDI (scores) | Pretest | 8.66 ± 5.72 | 8.47 ± 5.59 | 0.104 (0.262) | |||
| Post-test | 2.50 ± 2.66 | 3.15 ± 2.63 | |||||
| Mean difference | 6.16 ± 4.74 | 5.31 ± 3.30 | 73.719 (0.001) | 0.032 (0.858) | 0.405 (0.529) | ||
| 95% CI for difference | (3.80 to 8.52) | (3.72 to 6.90) | |||||
| t (p) | 5.516 (0.001) | 7.020 (0.001) | |||||
| CKCUEST (times) | Pretest | 18.00 ± 2.76 | 18.00 ± 3.38 | 0.000 (1.000) | |||
| Post-test | 28.00 ± 3.94 | 27.00 ± 3.62 | |||||
| Mean difference | 10.00 ± 3.86 | 9.00 ± 2.96 | 283.467 (0.001) | 0.257 (0.616) | 0.785 (0.382) | ||
| 95% CI for difference | (−11.92 to −8.07) | (−10.42 to −7.57) | |||||
| t (p) | −10.976 (0.001) | −13.241 (0.001) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, G.-H.; Lee, B.-H. Effects of Telerehabilitation Combining Diaphragmatic Breathing Re-Education and Shoulder Stabilization Exercises on Neck Pain, Posture, and Function in Young Adult Men with Upper Crossed Syndrome: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 1612. https://doi.org/10.3390/jcm13061612
Jeong G-H, Lee B-H. Effects of Telerehabilitation Combining Diaphragmatic Breathing Re-Education and Shoulder Stabilization Exercises on Neck Pain, Posture, and Function in Young Adult Men with Upper Crossed Syndrome: A Randomized Controlled Trial. Journal of Clinical Medicine. 2024; 13(6):1612. https://doi.org/10.3390/jcm13061612
Chicago/Turabian StyleJeong, Gyeong-Hyeon, and Byoung-Hee Lee. 2024. "Effects of Telerehabilitation Combining Diaphragmatic Breathing Re-Education and Shoulder Stabilization Exercises on Neck Pain, Posture, and Function in Young Adult Men with Upper Crossed Syndrome: A Randomized Controlled Trial" Journal of Clinical Medicine 13, no. 6: 1612. https://doi.org/10.3390/jcm13061612
APA StyleJeong, G.-H., & Lee, B.-H. (2024). Effects of Telerehabilitation Combining Diaphragmatic Breathing Re-Education and Shoulder Stabilization Exercises on Neck Pain, Posture, and Function in Young Adult Men with Upper Crossed Syndrome: A Randomized Controlled Trial. Journal of Clinical Medicine, 13(6), 1612. https://doi.org/10.3390/jcm13061612






