Hearing Recovery Prediction for Patients with Chronic Otitis Media Who Underwent Canal-Wall-Down Mastoidectomy
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Definition of Recovery
2.3. Machine Learning Models
- (1)
- Logistic Regression
- (2)
- Decision Tree
- (3)
- Random Forest
- (4)
- Support Vector Machine (SVM)
- (5)
- Extreme Gradient Boosting (XGBoost)
- (6)
- Light Gradient Boosting Machine (Light GBM)
2.4. Evaluation Metrics
2.5. Feature Selection
3. Results
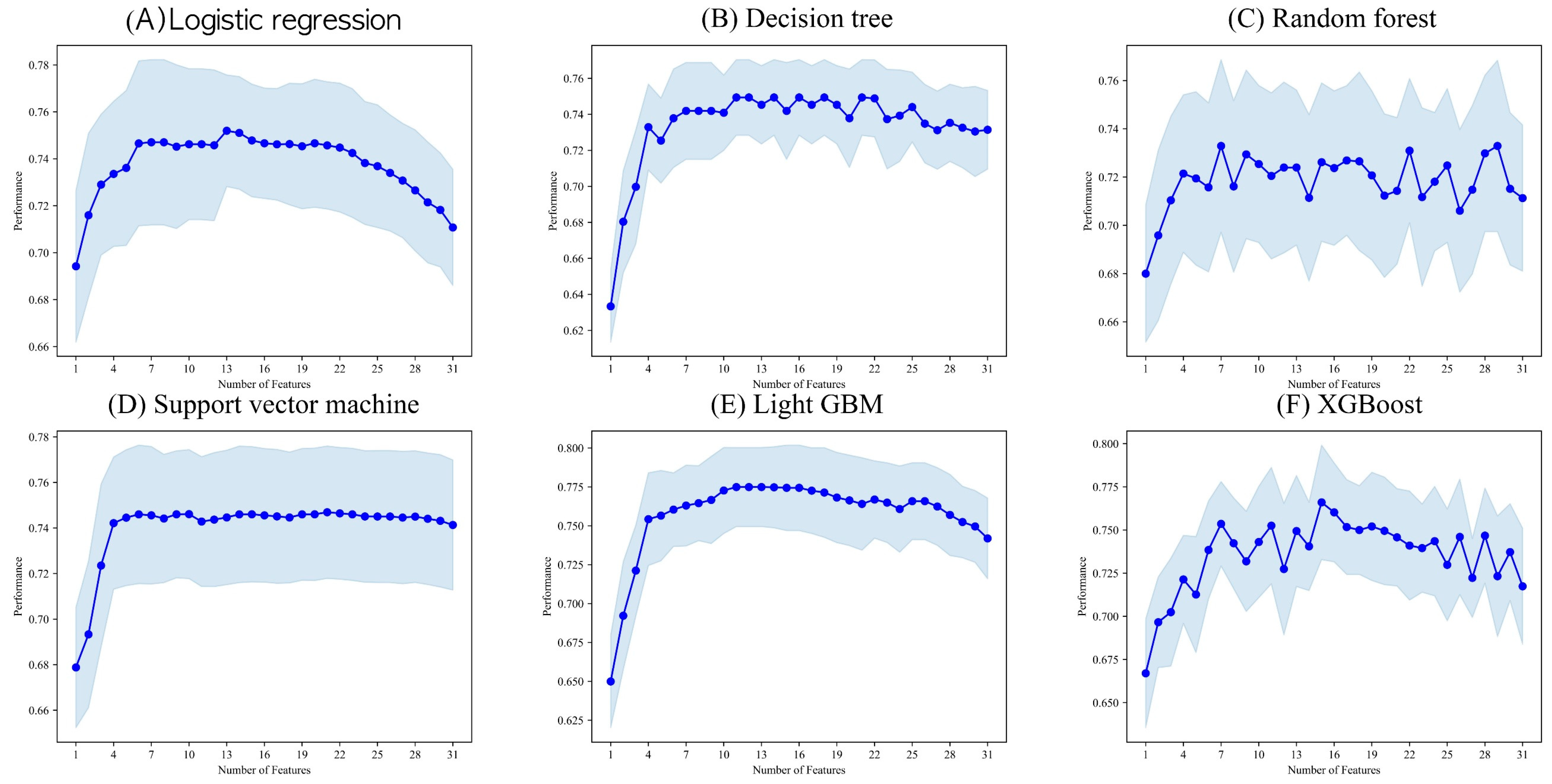
3.1. Feature Screening Results
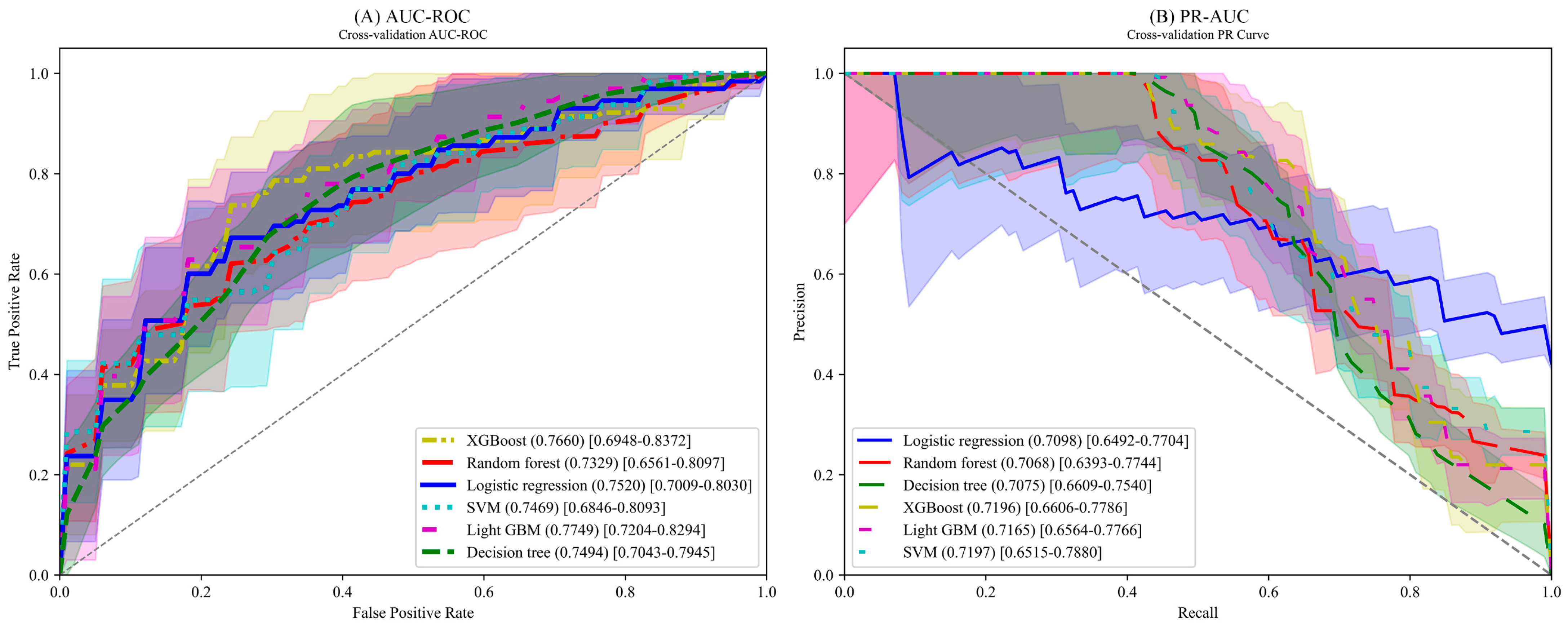
3.2. Performance Results
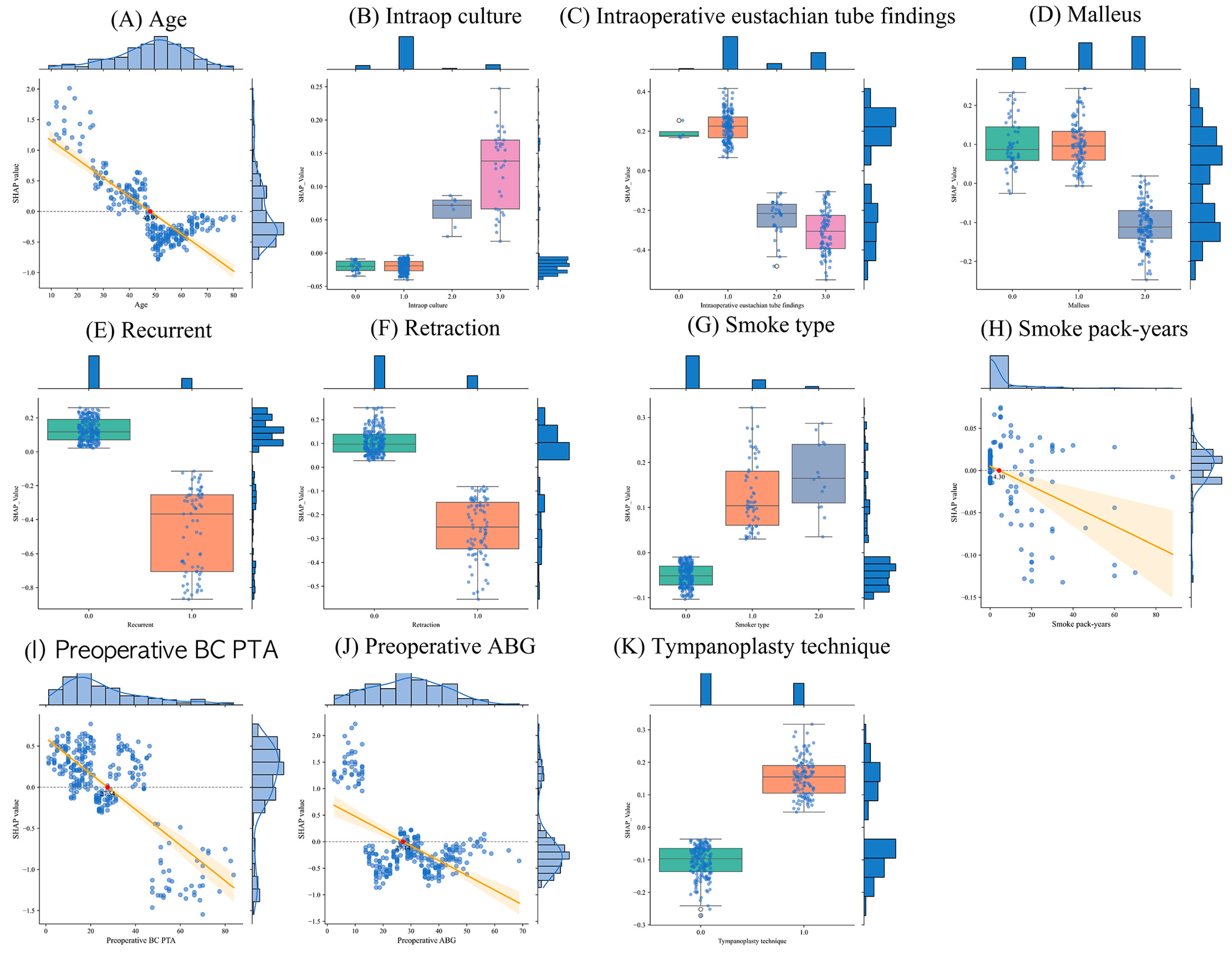
3.3. Analysis Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wallis, S.; Atkinson, H.; Coatesworth, A.P. Chronic otitis media. Postgrad. Med. 2015, 127, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Alakärppä, A.; Alho, O.P. Patient-recorded outcomes and quality of life in evidence-based medicine databases on most common ear, throat and nose procedures: A systematic review. Clin. Otolaryngol. 2012, 37, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Cejas, I.; Barker, D.H.; Petruzzello, E.; Sarangoulis, C.M.; Quittner, A.L. Cochlear Implantation and Educational and Quality-of-Life Outcomes in Adolescence. JAMA Otolaryngol. Head Neck Surg. 2023, 149, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Nadol, J.B., Jr.; Staecker, H.; Gliklich, R.E. Outcomes assessment for chronic otitis media: The Chronic Ear Survey. Laryngoscope 2000, 110, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Kurien, G.; Greeff, K.; Gomaa, N.; Ho, A. Mastoidectomy and mastoid obliteration with autologous bone graft: A quality of life study. J. Otolaryngol. Head Neck Surg. 2013, 42, 49. [Google Scholar] [CrossRef] [PubMed]
- Jung, N.Y.; Lee, C.B.; Jeong, S.-W.; Heo, K.W.; Kang, M.K. The Efficacy of Mastoid Obliteration in Patients Who Recieved Canal Wall Up Tympanomastoidectomy for Chronic Otitis Media. J. Clin. Otolaryngol. Head Neck Surg. 2019, 30, 182–188. [Google Scholar] [CrossRef]
- Lucidi, D.; De Corso, E.; Paludetti, G.; Sergi, B. Quality of life and functional results in canal wall down vs canal wall up mastoidectomy. Acta Otorhinolaryngol. Ital. 2019, 39, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Han, C.S.; Kim, H.B.; Park, J.R.; Jeong, E.H.; Oh, J.G.; Lee, W.Y.; Kim, C.A.; Ahn, J.K.; Gu, T.W.; Kang, M.K. Reconstruction of the Posterior Canal Wall with Mastoid Obliteration after Canal Wall Down Mastoidectomy. Korean J. Otorhinolaryngol. Head Neck Surg. 2008, 51, 33–40. [Google Scholar]
- Kim, Y.; Chae, M.; Cho, N.; Gil, H.; Lee, H. Machine Learning-Based Prediction Models of Acute Respiratory Failure in Patients with Acute Pesticide Poisoning. Mathematics 2022, 10, 4633. [Google Scholar] [CrossRef]
- Quinlan, J.R. Induction of decision trees. Mach. Learn. 1986, 1, 81–106. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Chauhan, V.K.; Dahiya, K.; Sharma, A. Problem formulations and solvers in linear SVM: A review. Artif. Intell. Rev. 2019, 52, 803–855. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.-Y. Lightgbm: A highly efficient gradient boosting decision tree. In Proceedings of the Dvances in Neural Information Processing Systems 30: Annual Conference on Neural Information Processing Systems, Long Beach, CA, USA, 4–9 December 2017. [Google Scholar]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–16 August 2016; pp. 785–794. [Google Scholar]
- Raschka, S. MLxtend: Providing machine learning and data science utilities and extensions to Python’s scientific computing stack. J. Open Source Softw. 2018, 3, 638. [Google Scholar] [CrossRef]
- Ferri, F.J.; Pudil, P.; Hatef, M.; Kittler, J. Comparative study of techniques for large-scale feature selection. In Machine Intelligence and Pattern Recognition; Elsevier: Amsterdam, The Netherlands, 1994; Volume 16, pp. 403–413. [Google Scholar]
- Lundberg, S.M.; Lee, S.-I. A unified approach to interpreting model predictions. In Advances in Neural Information Processing Systems; Nips Foundation: La Jolla, CA, USA, 2017; Volume 30. [Google Scholar]
- Uhm, T.; Lee, J.E.; Yi, S.; Choi, S.W.; Oh, S.J.; Kong, S.K.; Lee, I.W.; Lee, H.M. Predicting hearing recovery following treatment of idiopathic sudden sensorineural hearing loss with machine learning models. Am. J. Otolaryngol. 2021, 42, 102858. [Google Scholar] [CrossRef] [PubMed]
- Shew, M.; New, J.; Wichova, H.; Koestler, D.C.; Staecker, H. Using machine learning to predict sensorineural hearing loss based on perilymph micro RNA expression profile. Sci. Rep. 2019, 9, 3393. [Google Scholar] [CrossRef] [PubMed]
- Park, K.V.; Oh, K.H.; Jeong, Y.J.; Rhee, J.; Han, M.S.; Han, S.W.; Choi, J. Machine learning models for predicting hearing prognosis in unilateral idiopathic sudden sensorineural hearing loss. Clin. Exp. Otorhinolaryngol. 2020, 13, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Bing, D.; Ying, J.; Miao, J.; Lan, L.; Wang, D.; Zhao, L.; Yin, Z.; Yu, L.; Guan, J.; Wang, Q. Predicting the hearing outcome in sudden sensorineural hearing loss via machine learning models. Clin. Otolaryngol. 2018, 43, 868–874. [Google Scholar] [CrossRef]
- Koyama, H.; Mori, A.; Nagatomi, D.; Fujita, T.; Saito, K.; Osaki, Y.; Yamasoba, T.; Doi, K. Machine learning technique reveals prognostic factors of vibrant soundbridge for conductive or mixed hearing loss patients. Otol. Neurotol. 2021, 42, e1286–e1292. [Google Scholar] [CrossRef] [PubMed]



| General Characteristics | Total Patient | Recovery Group | Non-Recovery Group | p-Value |
|---|---|---|---|---|
| Age | 48.20 ± 14.03 | 43.81 ± 16.56 | 51.42 ± 10.81 | 0.1559 |
| Gender, male | 148 (49.67%) | 64 (50.79%) | 84 (48.88%) | 0.8287 |
| Recurrent | 71 (23.83%) | 23 (18.25%) | 48 (27.91%) | 0.0727 |
| Diabetes mellitus | 34 (11.41%) | 12 (9.52%) | 22 (12.79%) | 0.4890 |
| Hypertension | 65 (21.81%) | 17 (13.49%) | 48 (27.91%) | 0.0046 |
| Smoke type | 0.3746 | |||
| Non-smoker | 224 (75.17%) | 91 (72.22%) | 133 (77.33%) | |
| Smoker | 60 (20.13%) | 30 (23.81%) | 30 (17.44%) | |
| Ex-smoker | 14 (4.70%) | 5 (3.97%) | 9 (5.23%) | |
| Smoke pack-years | 4.58 ± 12.03 | 5.24 ± 14.25 | 4.09 ± 10.13 | 0.5370 |
| Tympanic membrane condition | 0.6181 | |||
| Less than 25% | 175 (58.72%) | 76 (60.32%) | 99 (57.56%) | |
| 25% to 50% | 47 (15.77%) | 21 (16.67%) | 23 (13.37%) | |
| 50% to 75% | 38 (12.75%) | 15 (11.90%) | 23 (13.37%) | |
| 75% over or tube inserted | 38 (12.75) | 14 (11.11%) | 24 (13.95%) | |
| Perforation margin TSP | 66 (22.15%) | 28 (22.22%) | 38 (22.09%) | 1.0 |
| Retraction | 84 (28.19%) | 28 (22.22%) | 56 (32.56%) | 0.0674 |
| Attic destruction | 159 (53.36%) | 73 (57.94%) | 86 (50%) | 0.2153 |
| Preop otorrhea | 96 (32.21%) | 46 (36.51%) | 50 (29.07%) | 0.2180 |
| Preop culture | 0.6427 | |||
| None | 164 (55.03%) | 65 (51.59%) | 99 (57.56%) | |
| No bacteria/normal flora | 62 (20.81%) | 30 (23.81%) | 32 (18.6%) | |
| MRSA, CRPA | 11 (3.69%) | 4 (3.17%) | 7 (4.07%) | |
| Others | 61 (20.47%) | 27 (21.43%) | 34 (19.77%) | |
| Intraoperative culture | 0.4801 | |||
| None | 27 (9.06%) | 15 (11.90%) | 12 (6.98%) | |
| No bacteria/normal flora | 231 (77.52%) | 93 (73.81%) | 138 (80.23%) | |
| MRSA, CRPA | 7 (2.35%) | 2 (1.59%) | 4 (2.33%) | |
| Others | 33 (11.07%) | 15 (11.90%) | 18 (10.47%) | |
| Intraoperative eustachian tube findings | 0.0000 | |||
| None | 4 (9.06%) | 3 (2.38%) | 1 (0.58%) | |
| Patent | 174 (77.52%) | 90 (71.43%) | 84 (48.84%) | |
| Partially obstructive | 31 (2.35%) | 10 (7.94%) | 21 (12.21%) | |
| Completely obstructive | 89 (11.07%) | 23 (18.25%) | 66 (38.37%) | |
| Stapes fixation | 0.7280 | |||
| Unknown | 20 (6.23%) | 6 (5.26%) | 11 (5.85%) | |
| No | 283 (88.18%) | 120 (90.23%) | 163 (86.70%) | |
| Yes | 18 (6.23%) | 7 (5.26%) | 11 (7.45%) | |
| Malleus | 0.0195 | |||
| Intact | 50 (16.78%) | 22 (19.84%) | 25 (14.53%) | |
| Partial removal/defected | 111 (37.25%) | 55 (43.65%) | 56 (2.91%) | |
| Total removal/defected | 137 (45.97%) | 46 (36.51%) | 91 (52.91%) | |
| Tympanoplasty technique | 0.3378 | |||
| None | 92 (30.87%) | 37 (29.37%) | 55 (31.98%) | |
| Underlay | 49 (16.44%) | 18 (14.29%) | 31 (18.02%) | |
| Overunderlay | 30 (10.07%) | 14 (11.11%) | 16 (9.30%) | |
| Overlay | 119 (39.93%) | 51 (40.48%) | 68 (39.53%) | |
| Umbo-anchoring | 8 (2.68%) | 6 (4.76%) | 2 (1.16%) | |
| Preoperative AC PTA, dB | 55 ± 23.99 | 45.43 ± 20.47 | 62.01 ± 24.01 | 0.2139 |
| Preoperative BC PTA, dB | 26.08 ± 17.80 | 24.96 ± 14.29 | 31.82 ± 11.44 | 0.0195 |
| Preoperative ABG, dB | 28.92 ± 13.14 | 31.82 ± 11.44 | 22.96 ± 14.29 | 0.0002 |
| Parameter | Description |
|---|---|
| Air-conduction PTA (AC PTA) | The mean of the frequencies at 500 Hz, 1 kHz, 2 kHz, and 4 kHz. |
| Bone-conduction PTA (BC PTA) | The mean of the frequencies at 500 Hz, 1 kHz, 2 kHz, and 4 kHz. |
| Air–bone gap (ABG) | The difference between AC PTA and BC PTA. |
| Algorithm | PPV | Sensitivity | F1 Score |
|---|---|---|---|
| Logistic regression | 0.6322 [0.5795–0.6849] | 0.6917 [0.5786–0.8047] | 0.6528 [0.5841–0.7215] |
| Decision tree | 0.6218 [0.5761–0.6674] | 0.7574 [0.6385–0.8743] | 0.6751 [0.6130–0.7373] |
| Random forest | 0.5925 [0.5149–0.6702] | 0.5686 [0.4255–0.7116] | 0.5535 [0.4699–0.6372] |
| Support vector machine | 0.6238 [0.5565–0.6912] | 0.5788 [0.4842–0.6734] | 0.5917 [0.5321–0.6512] |
| Light GBM | 0.6945 [0.6018–0.7872] | 0.5788 [0.4852–0.6725] | 0.6204 [0.5512–0.6895] |
| XGBoost | 0.6375 [0.5880–0.6870] | 0.5397 [0.4394–0.6401] | 0.5777 [0.5028–0.6526] |
| Algorithm | PPV | Sensitivity | F1 Score |
|---|---|---|---|
| With a threshold of 10% FPR | |||
| Logistic regression | 0.6518 [0.5629–0.7408] | 0.3494 [0.2351–0.4636] | 0.4464 [0.3316–0.5612] |
| Decision tree | 0.6939 [0.6244–0.7635] | 0.3355 [0.2387–0.4322] | 0.4421 [0.3456–0.5385] |
| Random forest | 0.7100 [0.6053–0.8147] | 0.3571 [0.2572–0.4569] | 0.4678 [0.3582–0.5774] |
| Support vector machine | 0.6689 [0.5487–0.7892] | 0.3276 [0.2294–0.4257] | 0.4314 [0.3162–0.5466] |
| Light GBM | 0.6179 [0.4549–0.7808] | 0.2763 [0.1467–0.4059] | 0.3693 [0.2265–0.5121] |
| XGBoost | 0.6161 [0.5409–0.6913] | 0.2519 [0.1346–0.3692] | 0.3378 [0.2140–0.4617] |
| With a threshold of 20% FPR | |||
| Logistic regression | 0.6577 [0.6052–0.7103] | 0.4667 [0.3698–0.5636] | 0.5390 [0.4645–0.6134] |
| Decision tree | 0.6512 [0.5947–0.7077] | 0.4596 [0.3365–0.5828] | 0.5183 [0.4252–0.6115] |
| Random forest | 0.6264 [0.5428–0.7100] | 0.4859 [0.3486–0.6232] | 0.5375 [0.4199–0.6552] |
| Support vector machine | 0.6343 [0.5254–0.7432] | 0.4308 [0.2783–0.5833] | 0.4933 [0.3497–0.6368] |
| Light GBM | 0.6646 [0.5920–0.7372] | 0.4699 [0.3596–0.5802] | 0.5436 [0.4447–0.6424] |
| XGBoost | 0.6117 [0.5725–0.6509] | 0.4519 [0.3606–0.5433] | 0.5132 [0.4422–0.5842] |
| With a threshold of 30% FPR | |||
| Logistic regression | 0.6195 [0.5525–0.6865] | 0.6404 [0.5465–0.7343] | 0.6252 [0.5551–0.6953] |
| Decision tree | 0.6214 [0.5777–0.6651] | 0.7083 [0.6053–0.8113] | 0.6574 [0.5979–0.7168] |
| Random forest | 0.5774 [0.5223–0.6325] | 0.6276 [0.5281–0.7270] | 0.5995 [0.5238–0.6752] |
| Support vector machine | 0.5255 [0.4491–0.6019] | 0.5571 [0.4239–0.6902] | 0.5355 [0.4313–0.6397] |
| Light GBM | 0.6158 [0.5390–0.6926] | 0.6212 [0.5221–0.7202] | 0.6127 [0.5370–0.6884] |
| XGBoost | 0.6291 [0.5971–0.6611] | 0.5788 [0.4811–0.6766] | 0.5975 [0.5321–0.6630] |
| With a threshold of 40% FPR | |||
| Logistic regression | 0.5452 [0.4893–0.6012] | 0.6968 [0.6025–0.7911] | 0.6089 [0.5411–0.6767] |
| Decision tree | 0.6194 [0.5746–0.6641] | 0.7641 [0.6498–0.8784] | 0.6778 [0.6162–0.7394] |
| Random forest | 0.5612 [0.5083–0.6140] | 0.6994 [0.5701–0.8286] | 0.6188 [0.5331–0.7046] |
| Support vector machine | 0.5450 [0.5053–0.5848] | 0.6737 [0.5677–0.7798] | 0.5999 [0.5331–0.6668] |
| Light GBM | 0.5480 [0.5057–0.5903] | 0.7160 [0.6144–0.8177] | 0.6168 [0.5571–0.6766] |
| XGBoost | 0.5944 [0.5550–0.6338] | 0.7019 [0.5762–0.8276] | 0.6318 [0.5665–0.6971] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chae, M.; Yoon, H.; Lee, H.; Choi, J. Hearing Recovery Prediction for Patients with Chronic Otitis Media Who Underwent Canal-Wall-Down Mastoidectomy. J. Clin. Med. 2024, 13, 1557. https://doi.org/10.3390/jcm13061557
Chae M, Yoon H, Lee H, Choi J. Hearing Recovery Prediction for Patients with Chronic Otitis Media Who Underwent Canal-Wall-Down Mastoidectomy. Journal of Clinical Medicine. 2024; 13(6):1557. https://doi.org/10.3390/jcm13061557
Chicago/Turabian StyleChae, Minsu, Heesoo Yoon, Hwamin Lee, and June Choi. 2024. "Hearing Recovery Prediction for Patients with Chronic Otitis Media Who Underwent Canal-Wall-Down Mastoidectomy" Journal of Clinical Medicine 13, no. 6: 1557. https://doi.org/10.3390/jcm13061557
APA StyleChae, M., Yoon, H., Lee, H., & Choi, J. (2024). Hearing Recovery Prediction for Patients with Chronic Otitis Media Who Underwent Canal-Wall-Down Mastoidectomy. Journal of Clinical Medicine, 13(6), 1557. https://doi.org/10.3390/jcm13061557








