A Novel Ophthalmic Solution Containing Glicopro® Complex for the Treatment of Patients with Dry Eye Disease: Results from a Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study and Patients
2.2. Ocular Surface Workup
2.3. Tear Analysis
2.4. Outcomes
2.5. Statistical Analysis
3. Results
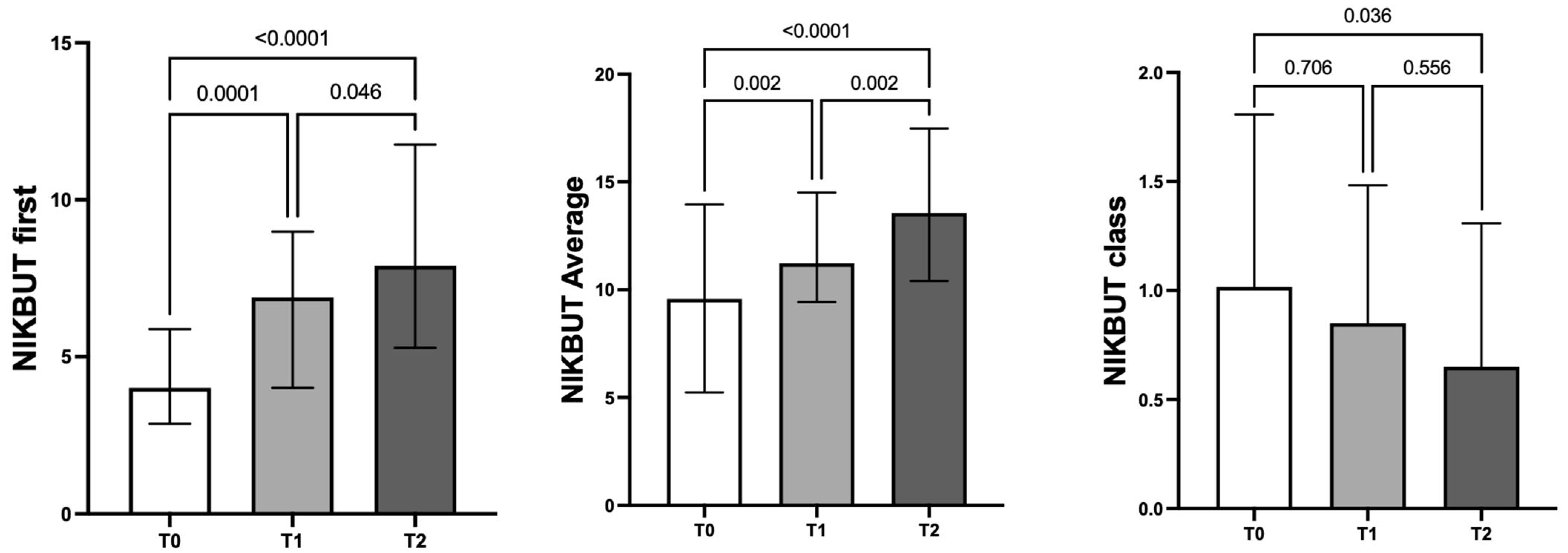
3.1. Ocular Parameters
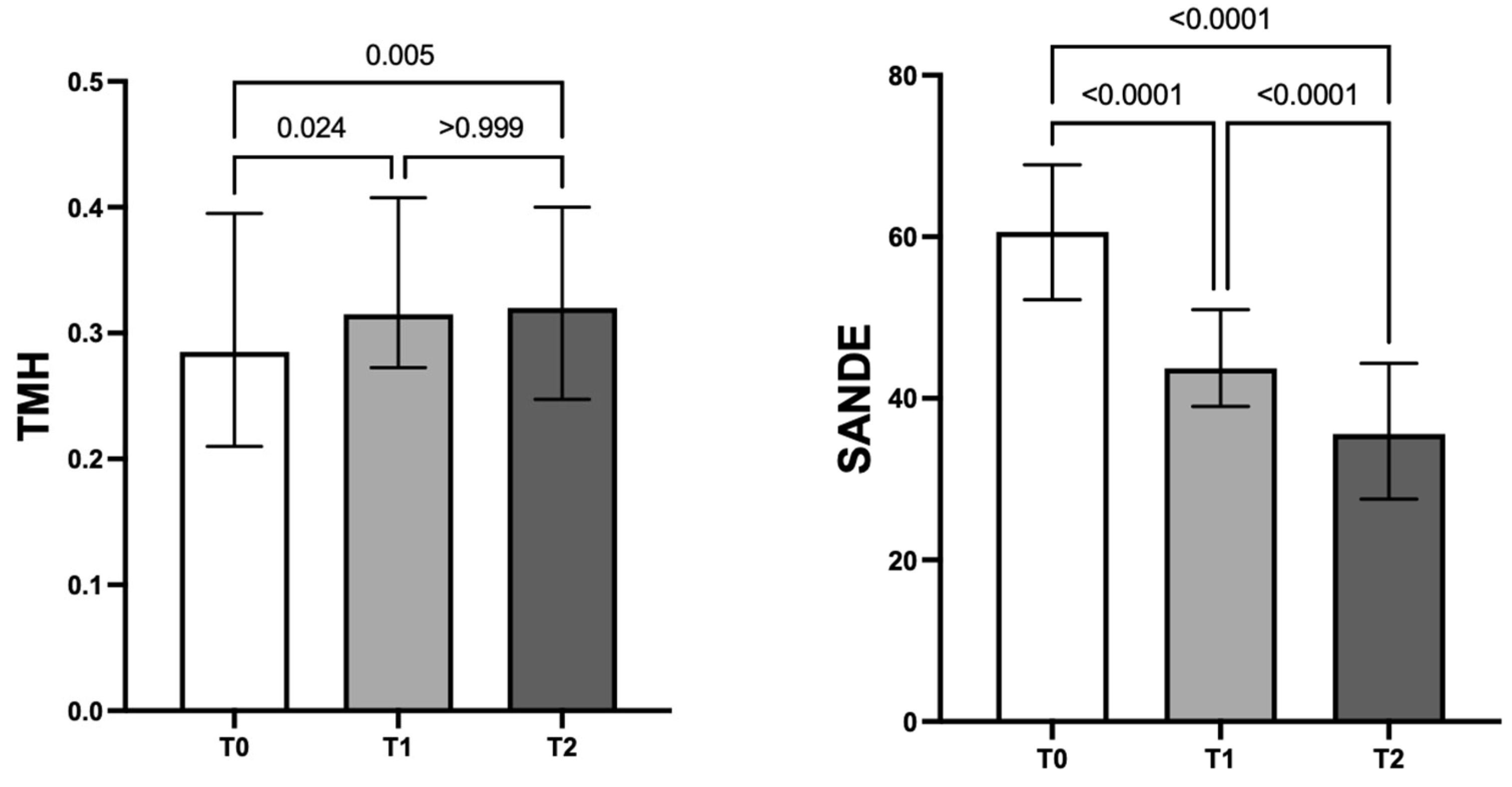
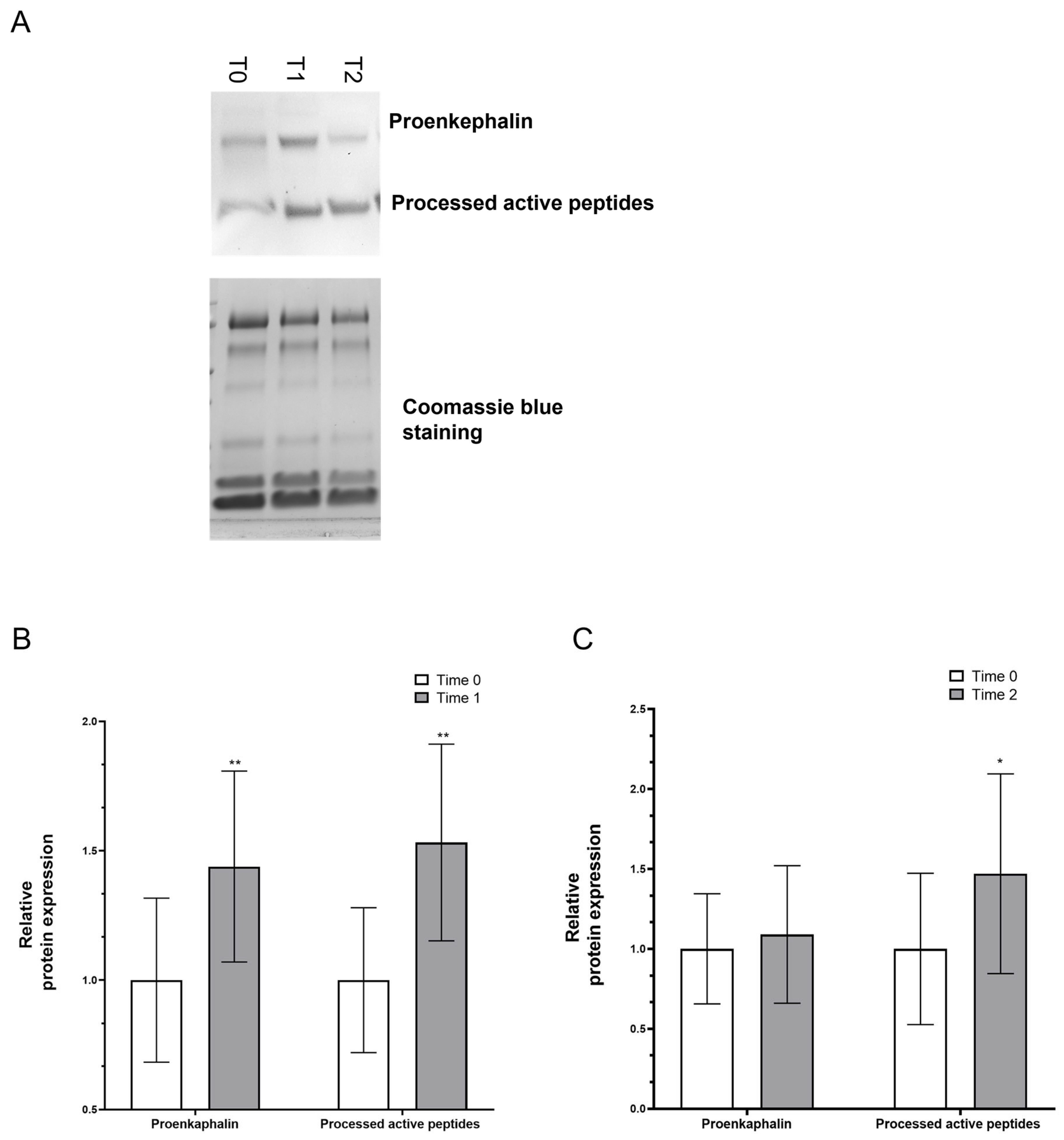
3.2. Tear Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rouen, P.A.; White, M.L. Dry Eye Disease: Prevalence, Assessment, and Management. Home Healthc. Now 2018, 36, 74–83. [Google Scholar] [CrossRef]
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. TFOS DEWS II Definition and Classification Report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Bron, A.J.; de Paiva, C.S.; Chauhan, S.K.; Bonini, S.; Gabison, E.E.; Jain, S.; Knop, E.; Markoulli, M.; Ogawa, Y.; Perez, V.; et al. TFOS DEWS II pathophysiology report. Ocul. Surf. 2017, 15, 438–510, Erratum in Ocul. Surf. 2019, 17, 842. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, F.; Alves, M.; Bunya, V.Y.; Jalbert, I.; Lekhanont, K.; Malet, F.; Na, K.S.; Schaumberg, D.; Uchino, M.; Vehof, J.; et al. TFOS DEWS II Epidemiology Report. Ocul. Surf. 2017, 15, 334–365. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, M.S. Anatomy of cornea and ocular surface. Indian J. Ophthalmol. 2018, 66, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.; Li, D.Q.; Corrales, R.M.; Pflugfelder, S.C. Hyperosmolar saline is a proinflammatory stress on the mouse ocular surface. Eye Contact Lens. 2005, 31, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Li, D.Q.; Chen, Z.; Song, X.J.; Luo, L.; Pflugfelder, S.C. Stimulation of matrix metalloproteinases by hyper-osmolarity via a JNK pathway in human corneal epithelial cells. Investig. Ophthalmol. Vis. Sci. 2004, 45, 4302–4311. [Google Scholar] [CrossRef] [PubMed]
- Rhee, M.K.; Mah, F.S. Inflammation in Dry Eye Disease: How Do We Break the Cycle? Ophthalmology 2017, 124, S14–S19. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.P.; D’Souza, S.; Shetty, R.; Ahuja, P.; Kundu, G.; Khamar, P.; Dadachanji, Z.; Paritekar, P.; Patel, P.; Dickman, M.M.; et al. Altered ocular surface immune cell profile in patients with dry eye disease. Ocul. Surf. 2021, 21, 96–106. [Google Scholar] [CrossRef]
- Na, K.S.; Mok, J.W.; Kim, J.Y.; Rho, C.R.; Joo, C.K. Correlations between tear cytokines, chemokines, and soluble receptors and clinical severity of dry eye disease. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5443–5450. [Google Scholar] [CrossRef]
- Lam, H.; Bleiden, L.; de Paiva, C.S.; Farley, W.; Stern, M.E.; Pflugfelder, S.C. Tear cytokine profiles in dysfunctional tear syndrome. Am. J. Ophthalmol. 2009, 147, 198–205.e1. [Google Scholar] [CrossRef]
- Johnson, M.E. The association between symptoms of discomfort and signs in dry eye. Ocul. Surf. 2009, 7, 199–211. [Google Scholar] [CrossRef]
- Friedman, N.J. Impact of dry eye disease and treatment on quality of life. Curr. Opin. Ophthalmol. 2010, 21, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Aragona, P.; Giannaccare, G.; Mencucci, R.; Rubino, P.; Cantera, E.; Rolando, M. Modern approach to the treatment of dry eye, a complex multifactorial disease: A P.I.C.A.S.S.O. board review. Br. J. Ophthalmol. 2021, 105, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Barabino, S.; Labetoulle, M.; Rolando, M.; Messmer, E.M. Understanding Symptoms and Quality of Life in Patients with Dry Eye Syndrome. Ocul. Surf. 2016, 14, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Reaux-Le Goazigo, A.; Poras, H.; Ben-Dhaou, C.; Ouimet, T.; Baudouin, C.; Wurm, M.; Parsadaniantz, S.M. Dual enkephalinase inhibitor PL265: A novel topical treatment to alleviate corneal pain and inflammation. Pain 2019, 160, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Kanjhan, R. Opioids and pain. Clin. Exp. Pharmacol. Physiol. 1995, 22, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Giannaccare, G.; Ghelardini, C.; Mancini, A.; Scorcia, V.; Di Cesare Mannelli, L. New Perspectives in the Pathophysiology and Treatment of Pain in Patients with Dry Eye Disease. J. Clin. Med. 2021, 11, 108. [Google Scholar] [CrossRef]
- Ozdogan, S.; Sonmez, C.; Yolcu, D.; Gungormus, M. Tear Opiorphin Levels in Ocular Pain Caused by Corneal Foreign Body. Cornea 2020, 39, 1377–1380. [Google Scholar] [CrossRef]
- Mencucci, R.; Strazzabosco, G.; Cristofori, V.; Alogna, A.; Bortolotti, D.; Gafà, R.; Cennamo, M.; Favuzza, E.; Trapella, C.; Gentili, V.; et al. GlicoPro, Novel Standardized and Sterile Snail Mucus Extract for Multi-Modulative Ocular Formulations: New Per-spective in Dry Eye Disease Management. Pharmaceutics 2021, 13, 2139. [Google Scholar] [CrossRef]
- Trapella, C.; Rizzo, R.; Gallo, S.; Alogna, A.; Bortolotti, D.; Casciano, F.; Zauli, G.; Secchiero, P.; Voltan, R. HelixComplex snail mucus exhibits pro-survival, proliferative and pro-migration effects on mammalian fibroblasts. Sci. Rep. 2018, 8, 17665. [Google Scholar] [CrossRef]
- Tsoutsos, D.; Kakagia, D.; Tamparopoulos, K. The efficacy of Helix aspersa Müller extract in the healing of partial thickness burns: A novel treatment for open burn management protocols. J. Dermatolog. Treat. 2009, 20, 219–222. [Google Scholar] [CrossRef]
- Gentili, V.; Bortolotti, D.; Benedusi, M.; Alogna, A.; Fantinati, A.; Guiotto, A.; Turrin, G.; Cervellati, C.; Trapella, C.; Rizzo, R.; et al. HelixComplex snail mucus as a potential technology against O3 induced skin damage. PLoS ONE 2020, 15, e0229613. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H.; et al. TFOS DEWS II diagnostic methodology report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef] [PubMed]
- García-Montero, M.; Rico-Del-Viejo, L.; Lorente-Velázquez, A.; Martínez-Alberquilla, I.; Hernández-Verdejo, J.L.; Madrid-Costa, D. Repeatability of Noninvasive Keratograph 5M Measurements Associated with Contact Lens Wear. Eye Contact Lens. 2019, 45, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Qu, J.H.; Zhang, X.Y.; Sun, X.G. Repeatability and Reproducibility of Noninvasive Keratograph 5M Measurements in Patients with Dry Eye Disease. J. Ophthalmol. 2016, 2016, 8013621. [Google Scholar] [CrossRef]
- Rico-Del-Viejo, L.; Benítez-Del-Castillo, J.M.; Gómez-Sanz, F.J.; García-Montero, M.; Llorens-Quintana, C.; Madrid-Costa, D. The influence of meibomian gland loss on ocular surface clinical parameters. Cont. Lens Anterior Eye 2019, 42, 562–568. [Google Scholar] [CrossRef]
- Garcia-Queiruga, J.; Pena-Verdeal, H.; Sabucedo-Villamarin, B.; Garcia-Resua, C.; Giraldez, M.J.; Yebra-Pimentel, E. Analysis of the Differences in Ocular Surface Damage and Inflammatory Signs between Healthy and Evaporative Dry Eye Participants. Ocul. Immunol. Inflamm. 2023, 31, 970–977. [Google Scholar] [CrossRef]
- Pult, H.; Riede-Pult, B.H. Non-contact meibography: Keep it simple but effective. Cont. Lens Anterior Eye 2012, 35, 77–80. [Google Scholar] [CrossRef]
- Schulze, M.M.; Ng, A.; Yang, M.; Panjwani, F.; Srinivasan, S.; Jones, L.W.; Senchyna, M. Bulbar Redness and Dry Eye Disease: Comparison of a Validated Subjective Grading Scale and an Objective Automated Method. Optom. Vis. Sci. 2021, 98, 113–120. [Google Scholar] [CrossRef]
- Gulati, A.; Sullivan, R.; Buring, J.E.; Sullivan, D.A.; Dana, R.; Schaumberg, D.A. Validation and repeatability of a short questionnaire for dry eye syndrome. Am. J. Ophthalmol. 2006, 142, 125–131. [Google Scholar] [CrossRef]
- Schaumberg, D.A.; Gulati, A.; Mathers, W.D.; Clinch, T.; Lemp, M.A.; Nelson, J.D.; Foulks, G.N.; Dana, R. Development and validation of a short global dry eye symptom index. Ocul. Surf. 2007, 5, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Kielkopf, C.L.; Bauer, W.; Urbatsch, I.L. Bradford Assay for Determining Protein Concentration. Cold Spring Harb. Protoc. 2020, 2020, 102269. [Google Scholar] [CrossRef] [PubMed]
- Mazzone, P.; Congestrì, M.; Scudiero, I.; Polvere, I.; Voccola, S.; Zerillo, L.; Telesio, G.; Vito, P.; Stilo, R.; Zotti, T. UBAC1/KPC2 regulates TLR3 signaling in human keratinocytes through functional interaction with the CARD14/CARMA2sh-TANK complex. Int. J. Mol. Sci. 2020, 21, 9365. [Google Scholar] [CrossRef] [PubMed]
- Brunelle, J.L.; Green, R. Coomassie blue staining. Methods Enzymol. 2014, 541, 161–167. [Google Scholar] [PubMed]
- Lambiase, A.; Sullivan, B.D.; Schmidt, T.A.; Sullivan, D.A.; Jay, G.D.; Truitt, E.R., III; Bruscolini, A.; Sacchetti, M.; Mantelli, F. A Two-Week, Randomized, Double-masked Study to Evaluate Safety and Efficacy of Lubricin (150 μg/mL) Eye Drops Versus Sodium Hyaluronate (HA) 0.18% Eye Drops (Vismed®) in Patients with Moderate Dry Eye Disease. Ocul. Surf. 2017, 15, 77–87. [Google Scholar] [CrossRef]
- Salarić, I.; Sabalić, M.; Alajbeg, I. Opiorphin in burning mouth syndrome patients: A case-control study. Clin. Oral Investig. 2017, 21, 2363–2370. [Google Scholar] [CrossRef] [PubMed]
- Ozdogan, M.S.; Gungormus, M.; Ince Yusufoglu, S.; Ertem, S.Y.; Sonmez, C.; Orhan, M. Salivary opiorphin in dental pain: A potential biomarker for dental disease. Arch. Oral Biol. 2019, 99, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Dufour, E.; Villard-Saussine, S.; Mellon, V.; Leandri, R.; Jouannet, P.; Ungeheuer, M.N.; Rougeot, C. Opiorphin se-cretion pattern in healthy volunteers: Gender difference and organ specificity. Biochem. Anal. Biochem. 2013, 2, 2–11. [Google Scholar]
- Wisner, A.; Dufour, E.; Messaoudi, M.; Nejdi, A.; Marcel, A.; Ungeheuer, M.N.; Rougeot, C. Human Opiorphin, a natural antinociceptive modulator of opioid-dependent pathways. Proc. Natl. Acad. Sci. USA 2006, 103, 17979–17984. [Google Scholar] [CrossRef]
- Mennini, N.; Mura, P.; Nativi, C.; Richichi, B.; Di Cesare Mannelli, L.; Ghelardini, C. Injectable liposomal formulations of opiorphin as a new therapeutic strategy in pain management. Future Sci. OA 2015, 1, FSO2. [Google Scholar] [CrossRef] [PubMed]
- Rougeot, C.; Messaoudi, M. Identification of human opiorphin, a natural antinociceptive modulator of opioid dependent pathways. Med. Sci. 2007, 23, 33–35. [Google Scholar] [CrossRef]
- Power, I. An update on analgesics. Br. J. Anaesth. 2011, 107, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Popik, P.; Kamysz, E.; Kreczko, J.; Wrobel, M. Human opiorphin: The lack of physiological dependence, tolerance to antinociceptive effects and abuse liability in laboratory mice. Behavioural Brain Res. 2010, 213, 88–93. [Google Scholar] [CrossRef]
- Rougeot, C.; Robert, F.; Menz, L.; Bisson, J.F.; Messaoudi, M. Systemically active human opiorphin is a potent yet non-addictive analgesic without drug tolerance effects. J. Physiol. Pharmacol. 2010, 61, 483–490. [Google Scholar]
| Age, mean value (SD), years | 67.00 (8.00) |
| Sex (M/F) | 23/37 |
| Caucasian race, n (%) | 60 (100) |
| TMH, median value (IQR), mm | 0.28 (0.21–0.39) |
| NIKBUT first, median value (IQR), s | 4.01 (2.87–5.88) |
| NIKBUT average, mean value (SD), s | 9.63 (5.03) |
| SANDE score, median value (IQR) | 60.60 (52.21–68.90) |
| Bulbar redness score, median value (IQR) | 1.35 (1.02–1.60) |
| MGL scale, median value (IQR) | 1.50 (1.00–2.00) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giannaccare, G.; Vaccaro, S.; Borselli, M.; Rossi, C.; Carnovale Scalzo, G.; Scalia, G.; Di Cesare Mannelli, L.; Ghelardini, C.; Zerillo, L.; Polvere, I.; et al. A Novel Ophthalmic Solution Containing Glicopro® Complex for the Treatment of Patients with Dry Eye Disease: Results from a Pilot Study. J. Clin. Med. 2024, 13, 1447. https://doi.org/10.3390/jcm13051447
Giannaccare G, Vaccaro S, Borselli M, Rossi C, Carnovale Scalzo G, Scalia G, Di Cesare Mannelli L, Ghelardini C, Zerillo L, Polvere I, et al. A Novel Ophthalmic Solution Containing Glicopro® Complex for the Treatment of Patients with Dry Eye Disease: Results from a Pilot Study. Journal of Clinical Medicine. 2024; 13(5):1447. https://doi.org/10.3390/jcm13051447
Chicago/Turabian StyleGiannaccare, Giuseppe, Sabrina Vaccaro, Massimiliano Borselli, Costanza Rossi, Giovanna Carnovale Scalzo, Giovanni Scalia, Lorenzo Di Cesare Mannelli, Carla Ghelardini, Lucrezia Zerillo, Immacolata Polvere, and et al. 2024. "A Novel Ophthalmic Solution Containing Glicopro® Complex for the Treatment of Patients with Dry Eye Disease: Results from a Pilot Study" Journal of Clinical Medicine 13, no. 5: 1447. https://doi.org/10.3390/jcm13051447
APA StyleGiannaccare, G., Vaccaro, S., Borselli, M., Rossi, C., Carnovale Scalzo, G., Scalia, G., Di Cesare Mannelli, L., Ghelardini, C., Zerillo, L., Polvere, I., Vito, P., Zotti, T., Stilo, R., & Scorcia, V. (2024). A Novel Ophthalmic Solution Containing Glicopro® Complex for the Treatment of Patients with Dry Eye Disease: Results from a Pilot Study. Journal of Clinical Medicine, 13(5), 1447. https://doi.org/10.3390/jcm13051447











