Effectiveness of Extracorporeal Shock Wave Therapy in Treatment of Spasticity of Different Aetiologies: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
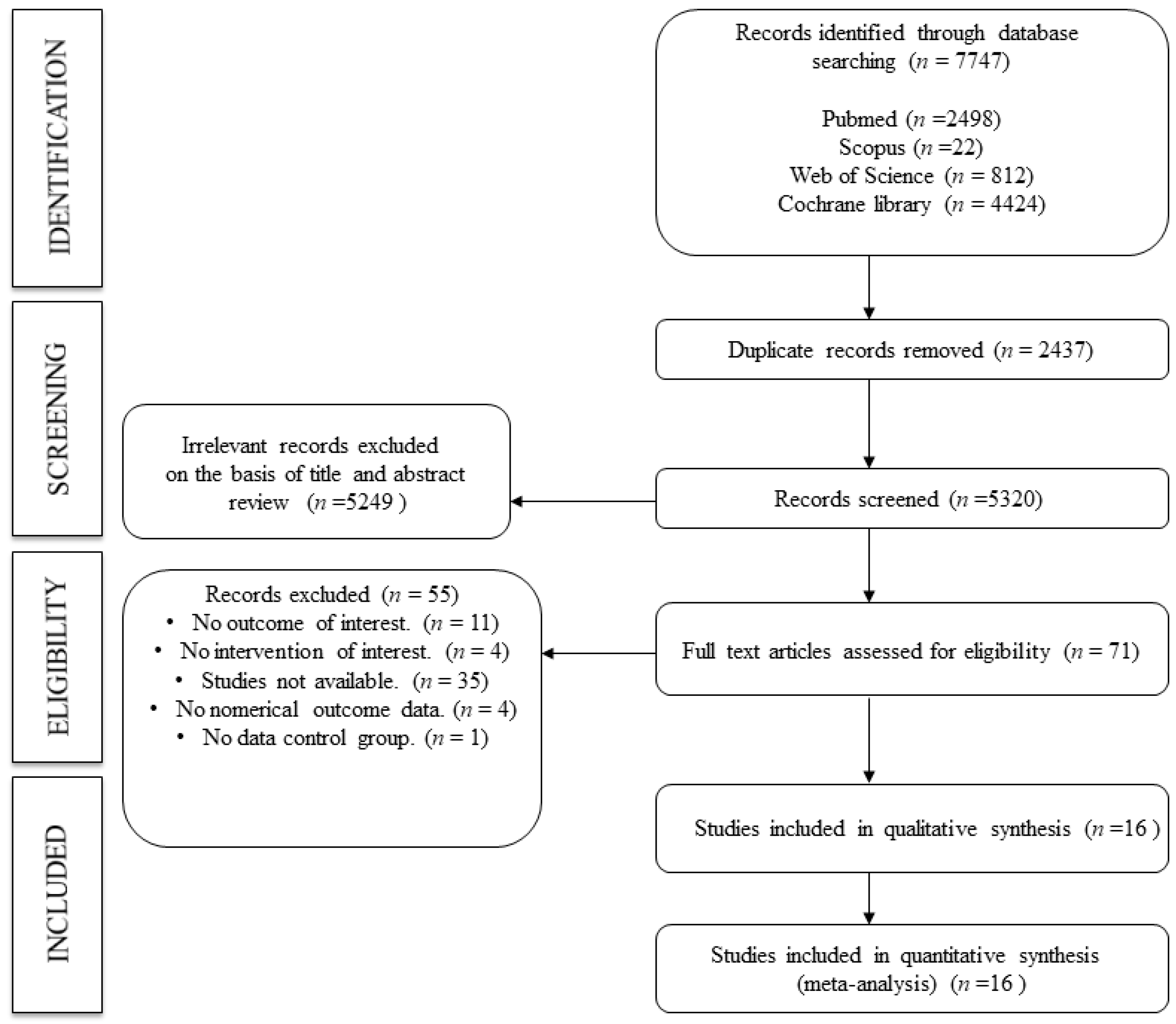
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis and Data Synthesis
3. Results
3.1. Baseline Characteristics
3.2. Quality Assessment
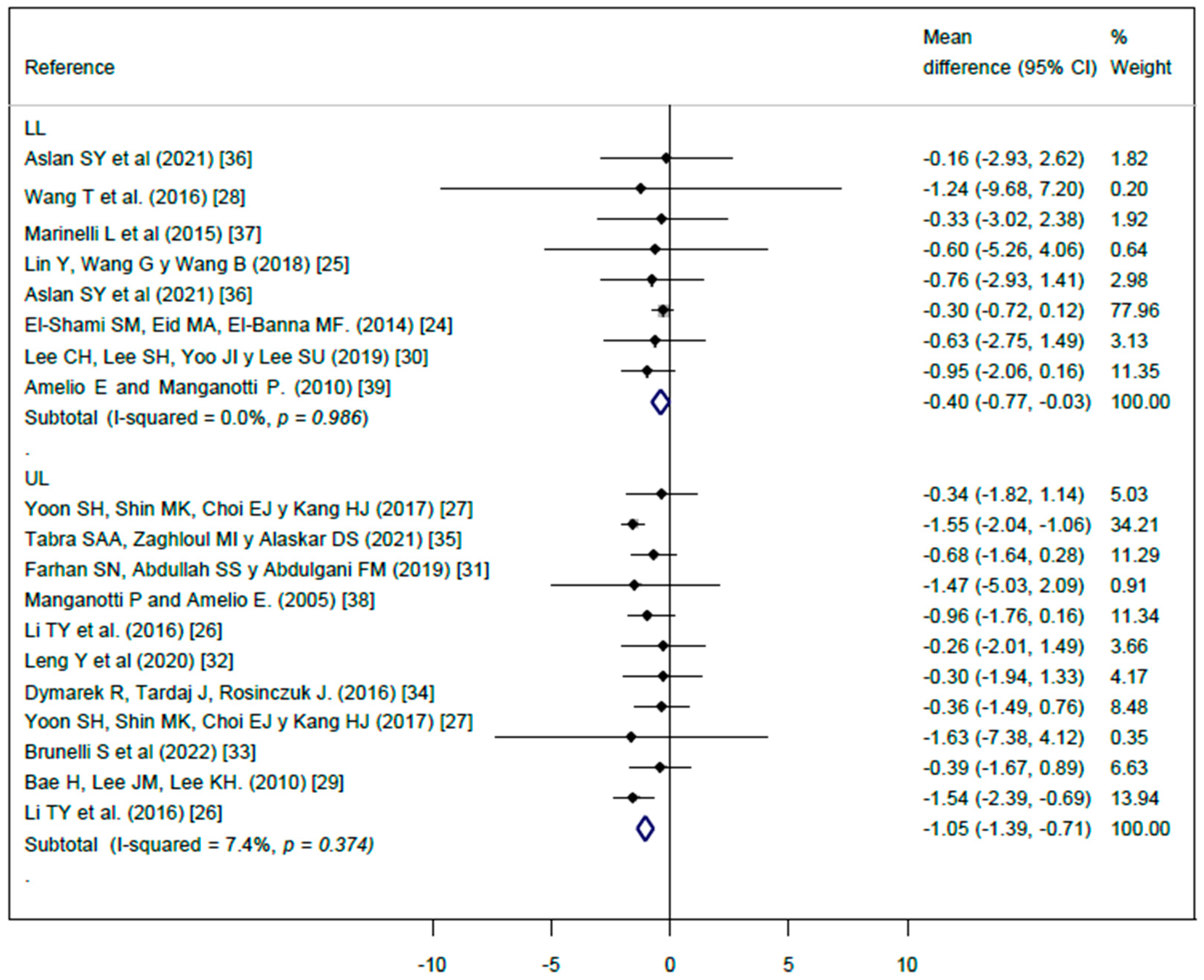
3.3. Effect of Extracorporeal Shock Wave Therapy (ESTW) on Spasticity
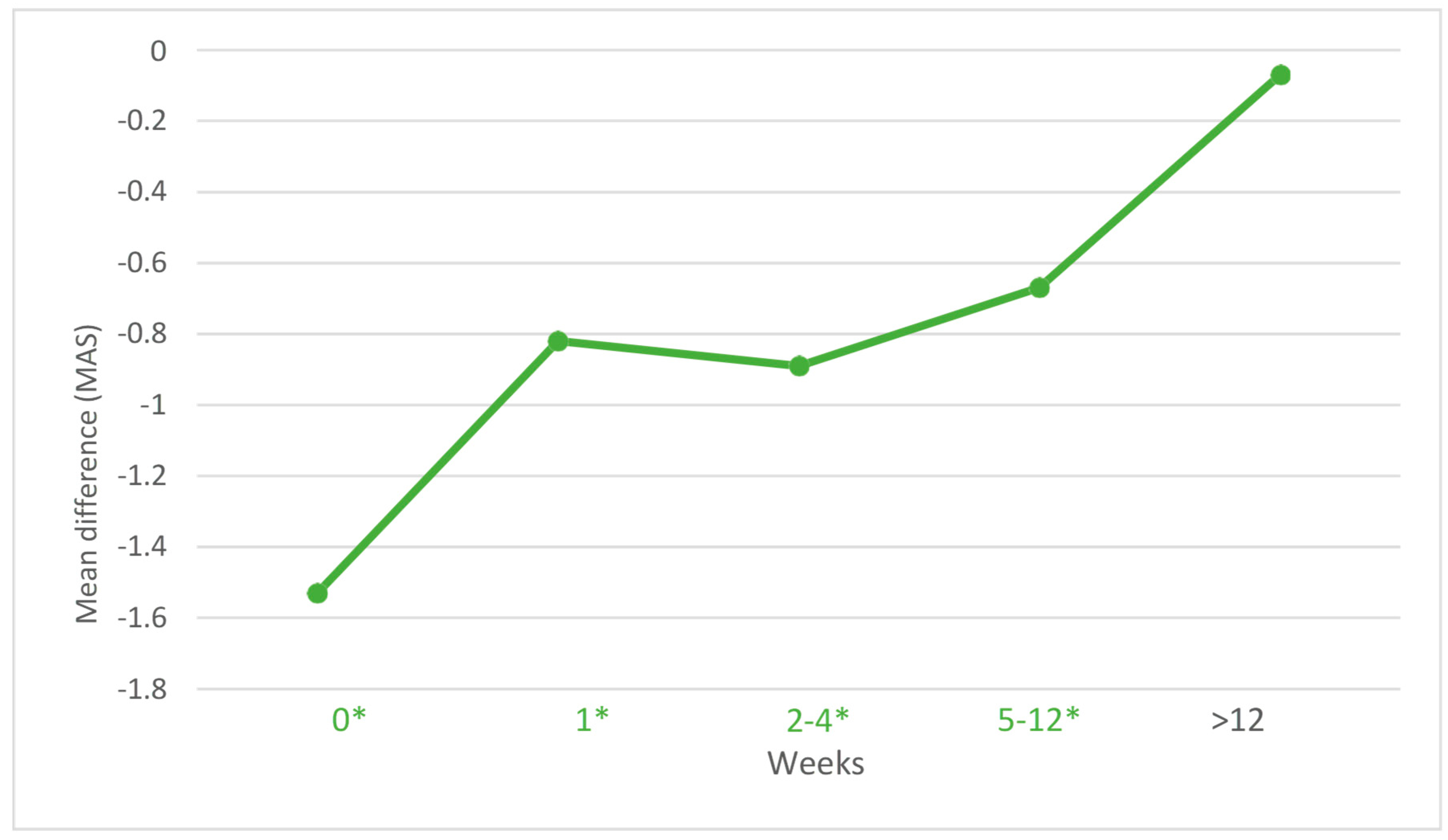
3.4. Effect of Extracoporeal Shock Wave Therapy (ESTW) on Spasticity for Time Periods after Intervention
3.5. Sensitivity Analysis
3.6. Subgroup Analysis and Meta-Regression Models
3.7. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bolaños-Jiménez, R.; Arizmendi-Vargas, J.; Calderón-Álvarez Tostado, J.L.; Carrillo-Ruiz, J.D.; Rivera-Silva, G.; Jiménez-Ponce, F. Espasticidad, conceptos fisiológicos y fisiopatológicos aplicados a la clínica. Rev. Mex. Neurocienc. 2011, 12, 141–148. [Google Scholar]
- Frérebeau, P.; Segnarbieux, F.; Ohanna, F.; Ronzier, J. Clinical features of spasticity. In Neurosurgery for Spasticity; Springer: Vienna, Austria, 1991; pp. 29–32. [Google Scholar] [CrossRef]
- Martínez, I.M.; Sempere-Rubio, N.; Navarro, O.; Faubel, R. Effectiveness of shock wave therapy as a treatment for spasticity: A systematic review. Brain Sci. 2021, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Hugos, C.L.; Cameron, M.H. Assessment and Measurement of Spasticity in MS: State of the Evidence. Curr. Neurol. Neurosci. Rep. 2019, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Guo, P.; Gao, F.; Zhao, T.; Sun, W.; Wang, B.; Li, Z. Positive Effects of Extracorporeal Shock Wave Therapy on Spasticity in Poststroke Patients: A Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2017, 26, 2470–2476. [Google Scholar] [CrossRef]
- Brashear, A.; Lambeth, K. Spasticity. Curr. Treat. Options Neurol. 2009, 11, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Testa, G.; Vescio, A.; Perez, S.; Consoli, A.; Costarella, L.; Sessa, G.; Pavone, V. Extracorporeal Shockwave Therapy Treatment in Upper Limb Diseases: A Systematic Review. J. Clin. Med. 2020, 9, 453. [Google Scholar] [CrossRef] [PubMed]
- Mittermayr, R.; Hartinger, J.; Antonic, V.; Meinl, A.; Pfeifer, S.; Stojadinovic, A.; Schaden, W.; Redl, H. Extracorporeal shock wave therapy (ESWT) minimizes ischemic tissue necrosis irrespective of application time and promotes tissue revascularization by stimulating angiogenesis. Ann. Surg. 2011, 253, 1024–1032. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Park, J.W.; Nam, K. Effect of extracorporeal shockwave therapy on muscle spasticity in patients with cerebral palsy: Meta-analysis and systematic review. Eur. J. Phys. Rehabil. Med. 2019, 55, 761–771. [Google Scholar] [CrossRef]
- Li, G.; Yuan, W.; Liu, G.; Qiao, L.; Zhang, Y.; Wang, Y.; Wang, W.; Zhao, M.; Wang, Y.; Wang, J. Effects of radial extracorporeal shockwave therapy on spasticity of upper-limb agonist/antagonist muscles in patients affected by stroke: A randomized, single-blind clinical trial. Age Ageing 2020, 49, 246–252. [Google Scholar] [CrossRef]
- Xiang, J.; Wang, W.; Jiang, W.; Qian, Q. Effects of extracorporeal shock wave therapy on spasticity in poststroke patients: A systematic review and meta-analysis of randomised controlled trials. J. Rehabil. Med. 2018, 50, 852–859. [Google Scholar] [CrossRef]
- Cabanas-Valdés, R.; Calvo-Sanz, J.; Urrùtia, G.; Serra-Llobet, P.; Pérez-Bellmunt, A.; Germán-Romero, A. The effectiveness of extracorporeal shock wave therapy to reduce lower limb spasticity in stroke patients: A systematic review and meta-analysis. Top. Stroke Rehabil. 2020, 27, 137–157. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Ma, J.; Wang, S.; Wu, D.; Tan, B.; Yin, Y.; Jia, L.; Cheng, L. Long-term Effects of Extracorporeal Shock Wave Therapy on Poststroke Spasticity: A Meta-analysis of Randomised Controlled Trials. J. Stroke Cerebrovasc. Dis. 2020, 29, 104591. [Google Scholar] [CrossRef] [PubMed]
- Cabanas-Valdés, R.; Serra-Llobet, P.; Rodriguez-Rubio, P.R.; López-de–Celis, C.; Llauró-Fores, M.; Calvo-Sanz, J. The effectiveness of extracorporeal shock wave therapy for improving upper limb spasticity and functionality in stroke patients: A systematic review and meta-analysis. Clin. Rehabil. 2020, 34, 1141–1156. [Google Scholar] [CrossRef] [PubMed]
- Corrado, B.; Di Luise, C.; Servodio Iammarrone, C. Management of Muscle Spasticity in Children with Cerebral Palsy by Means of Extracorporeal Shockwave Therapy: A Systematic Review of the Literature. Dev. Neurorehabilit. 2021, 24, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kudva, A.; Abraham, M.E.; Gold, J.; Patel, N.A.; Gendreau, J.L.; Herschman, Y.; Mammis, A. Intrathecal baclofen, selective dorsal rhizotomy, and extracorporeal shockwave therapy for the treatment of spasticity in cerebral palsy. A systematic review. Neurosurg. Rev. 2021, 44, 3209–3228. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 2020–2021. [Google Scholar]
- Higgins, J.P.T.; Green, S. Selecting studies and collecting data. In Cochrane Handbook of Systematic Reviews of Interventions; Version 5.1.0; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- DerSimonian, R.; Kacker, R. Random-effects model for meta-analysis of clinical trials: An update. Contemp. Clin. Trials 2007, 28, 105–114. [Google Scholar] [CrossRef]
- Jackson, D.; Turner, R. Power analysis for random-effects meta-analysis. Res. Synth. Methods 2017, 8, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Egger, M.; Smith, G.D. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001, 323, 101–105. [Google Scholar] [CrossRef]
- El-Shamy, S.M.; Eid, M.A.; El-Banna, M.F. Effect of extracorporeal shock wave therapy on gait pattern in hemiplegic cerebral palsy: A randomised controlled tiral. Am. J. Phys. Med. Rehabil. 2014, 93, 1065–1072. [Google Scholar] [CrossRef]
- Lin, Y.; Wang, G.; Wang, B. Rehabilitation treatment of spastic cerebral palsy with radial extracorporeal shock wave therapy and rehabilitation therapy. Medicine 2018, 97, e13828. [Google Scholar] [CrossRef]
- Li, T.Y.; Chang, C.Y.; Chou, Y.C.; Chen, L.C.; Chu, H.Y.; Chiang, S.L.; Chang, S.T.; Wu, Y.T. Effect of radial shock wave therapy on spasticity of the upper limb in patients with chronic stroke a prospective, randomised, single blind, controlled trial. Medicine 2016, 95, 3544. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.H.; Shin, M.K.; Choi, E.J.; Kang, H.J. Effective site for the application of extracorporeal shock-wave therapy on spasticity in chronic stroke: Muscle belly or myotendinous junction. Ann. Rehabil. Med. 2017, 41, 547–555. [Google Scholar] [CrossRef]
- Wang, T.; Du, L.; Shan, L.; Dong, H.; Feng, J.; Kiessling, M.C.; Angstman, N.B.; Schmitz, C.; Jia, F. A prospective case-control study of radial extracorporeal shock wave therapy for spastic plantar flexor muscles in very young children with cerebral palsy. Medicine 2016, 95, e3649. [Google Scholar] [CrossRef] [PubMed]
- Bae, H.; Lee, J.M.; Lee, K.H. The effects of extracorporeal shock wave therapy on spasticity in chronic stroke patients. J. Korean Acad. Rehabil. Med. 2010, 34, 663–669. [Google Scholar]
- Lee, C.H.; Lee, S.H.; Yoo, J.I.; Lee, S.U. Ultrasonographic Evaluation for the Effect of Extracorporeal Shock Wave Therapy on Gastrocnemius Muscle Spasticity in Patients With Chronic Stroke. PMR 2019, 11, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Farhan, S.N.; Abdullah, S.S.; Abdulgani, F.M. Impact of extracorporeal shock wave therapy on spastic handfunction with assistive devices in children with cerebral palsy. Ann. Trop. Med. Public Health 2019, 22, 60–69. [Google Scholar] [CrossRef]
- Leng, Y.; Lo, W.L.A.; Hu, C.; Bian, R.; Xu, Z.; Shan, X.; Huang, D.; Li, L. The Effects of Extracorporeal Shock Wave Therapy on Spastic Muscle of the Wrist Joint in Stroke Survivors: Evidence From Neuromechanical Analysis. Front. Neurosci. 2021, 14, 580762. [Google Scholar] [CrossRef] [PubMed]
- Brunelli, S.; Gentileschi, N.; Spanò, B.; Pratesi, L.; Calvani, A.; Mucci, R.; Foti, C. Effect of Early Radial Shock Wave Treatment on Spasticity in Subacute Stroke Patients: A Pilot Study. Biomed Res. Int. 2022, 2022, 8064548. [Google Scholar] [CrossRef] [PubMed]
- Dymarek, R.; Taradaj, J.; Rosińczuk, J. The Effect of Radial Extracorporeal Shock Wave Stimulation on Upper Limb Spasticity in Chronic Stroke Patients: A Single-Blind, Randomised, Placebo-Controlled Study. Ultrasound Med. Biol. 2016, 42, 1862–1875. [Google Scholar] [CrossRef] [PubMed]
- Tabra, S.A.A.; Zaghloul, M.I.; Alashkar, D.S. Extracorporeal shock wave as adjuvant therapy for wrist and hand spasticity in poststroke patients: A randomised controlled trial. Egypt. Rheumatol. Rehabil. 2021, 48, 21. [Google Scholar] [CrossRef]
- Yoldaş Aslan, Ş.; Kutlay, S.; Düsünceli Atman, E.; Elhan, A.H.; Gök, H.K.A. Does Extracorporeal shock wave therapy decrease spasticity of anke plantar flexor muscles in patients with stroke: A randomized controlled trial. Clin. Rehabil. 2021, 35, 1442–1453. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, L.; Mori, L.; Solaro, C.; Uccelli, A.; Pelosin, E.; Currà, A.; Molfetta, L.; Abbruzzese, G.; Trompetto, C. Effect of radial shock wave therapy on pain and muscle hypertonia: A double-blind study in patients with multiple sclerosis. Mult. Scler. 2015, 21, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Manganotti, P.; Amelio, E. Long-term effect of shock wave therapy on upper limb hypertonia in patients affected by stroke. Stroke 2005, 36, 1967–1971. [Google Scholar] [CrossRef]
- Amelio, E.; Manganotti, P. Effect of shock wave stimulation on hypertonic plantar flexor muscles in patients with cerebral palsy: A placebo-controlled study. J. Rehabil. Med. 2010, 42, 339–343. [Google Scholar] [CrossRef]
- Li, F.; Wu, Y.; Li, X. Test-retest reliability and inter-rater of the Modified Tardieu Scale and the Modified Ashworth Scale in the hemiplegic patients with stroke. Eur. J. Phys. Rehabil. Med. 2014, 50, 9–15. [Google Scholar]
| Reference | Country | Study Design | Population Characteristics | Intervention Characteristics | Outcome Variable: Spasticity | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size (n Women) | Age (Years) | Population Type | Baseline MAS | Area of Application | Measurement Weeks | Frecuency (Hz) | Energy (mJ/mm2) | Impact (Shots per Muscle) | Measurement Method | MAS Scale Reduction (MD ± SD) | |||
| Manganotti, P. and Amelio, E. (2005) [38] | Italy | CCT | 20 (9) | 38–76 | Chronic stroke | EG: 3.28 ± 2.04 CG: 3.28 ± 2.04 | Wrist flexor Finguer flexor | Inmediatly after therapy, weeks 1, 4, and 12 | NR | 0.030 | 800–1500 | MAS | EG: −1.59 ± 7.397 CG: −0.72 ± 2.661 |
| Amelio, E. and Manganotti, P. (2010) [39] | Italy | CCT | 12 (6) | 8 ± 2.31 | CP | EG: 3.3 ± 0.49 CG: 3.3 ± 0.49 | Plantar flexors | Inmediatly after therapy, weeks 1, 4, and 12 | NR | 0.030 | 1500 | MAS | EG: −1.15 ± 1.750 CG: −0.2 ± 0.620 |
| Bae, H., Lee, J.M., Lee, K.H. (2010) [29] | Republic of Korea | RCT | 32 (12) | EG: 56.7 ± 12.4 CG: 53.4 ± 16.8 | Chronic stroke | EG: 2.9 ± 0.3 CG: 2.6 ± 0.5 | Elbow flexors | Inmediatly after therapy, weeks 1 and 4 | 4 | 0.12 | 1200 | MAS | EG: −0.42 ± 1.713 CG: −0.03 ± 1.224 |
| El-Shami, S.M., Eid, M.A., El-Banna, M.F. (2014) [24] | Egypt | RCT | 30 (12) | EG: 6.93 ± 0.8 CG: 6.8 ± 0.7 | CP | EG: 2.34 ± 0.48 CG: 2.27 ± 0.92 | Ankle plantar flexor | Week 12 | 5 | 0.030 | 1500 | MAS | EG: −0.71 ± 0.531 CG: −0.41 ± 0.600 |
| Marinelli, L. et al. (2016) [37] | Italy | RCT | 68 (38) | EG: 51.74 ± 11.29 CG: 51 ± 13.17 | Multiple sclerosis | EG: 2.68 ± 0.77 CG: 2.56 ± 0.92 | Ankle extensor muscles and Achiles tendon | Inmediatly after therapy, weeks 1 and 4 | 4 | NR | 2000 | MAS | EG: −0.44 ± 5.147 CG: −0.11 ± 6.024 |
| Dymarek, R., Tardaj, J., Rosinczuk, J. (2016) [34] | Poland | RCT | 60 (26) | EG: 61.46 ± 12.74 CG: 60.87 ± 9.51 | Chronic stroke | EG: 1.66 ± 1.65 CG: 1.68 ± 1.93 | Elbow joint Finger joints Radio-carpal joints | Inmediatly after therapy | 5 | 0.030 | 1500 | MAS | EG: −0.317 ± 2.321 CG: −0.015 ± 2.768 |
| Li, T.Y. et al. (2016) [26] | China | RCT | 60 (19) | EG1: 55.35 ± 3.05 EG2: 56.80 ± 3.00 CG: 55.95 ± 2.64 | Chronic stroke | EG1: 3.07 ± 0.89 EG2: 3.10 ± 0.68 CG: 2.65 ± 0.03 | Wrist Hand | Inmediatly after therapy, weeks 1, 4, 8, 12, and 16 | 5 | NR | 1500–4000 | MAS | EG1: −1.51 ± 1.825 EG2: −0.93 ± 1.688 CG: 0.03 ± 0.491 |
| Wang, T. et al. (2016) [28] | China | RCT | 86 (22) | EG: 26.9 ± 13.1 month CG: 27.0 ± 14.2 month | CP | EG: 2.09 ± 2.99 CG: 2.1 ± 2.99 | Plantar flexor muscles | Weeks 4 and 12 | 8 | 0.03 | 1500 | MAS | EG: −1.35 ± 18.415 CG: −0.11 ± 15.686 |
| Yoon, S.H., Shin, M.K., Choi, E.J. and Kang, H.J. (2017) [27] | Republic of Korea | RCT | 124 (5) | EG1: 58.7 ± 15.7 EG2: 63.1 ± 11.8 CG: 63.4 ± 13.8 | Chronic stroke | EG1: 2.84 ± 3.59 EG2: 2.86 ± 2.43 CG: 2.52 ± 3.13 | Elbow flexor | Week 1 | 5 | 0.068–0.093 | 1500 | MAS | EG1: −0.34 ± 4.896 EG2: −0.36 ± 3.688 CG: 0 ± 0.667 |
| Lin, Y., Wang, G. and Wang, B. (2018) [25] | China | RCT | 82 | EG: 7.5 ± 1.3 CG: 7.9 ± 1.7 | CP | EG: 4.50 ± 2.45 CG: 4.70 ± 2.45 | Triceps and hamstring muscles | Weeks 2 and 4 | 10 | NR | 2000 | MAS | EG: −2.050 ± 9.324 CG: −1.45 ± 11.853 |
| Farhan, S.N., Abdullah, S.S. and Abdulgani, F.M. (2019) [31] | Irak | RCT | 32 (15) | EG: 6.37 ± 1.44 CG: 6.68 ± 2.63 | CP | NR | Wrist and elbow flexors | Week 8 | 10 | 0.03 | 800 | MAS | EG: −1.06 ± 2.179 CG: −0.380 ± 1.631 |
| Lee, C.H., Lee, S.H., Yoo, J.I. and Lee, S.U. (2019) [30] | Republic of Korea | RCT | 18 (2) | EG: 50.89 ± 8.81 CG: 44.11 ± 4.07 | Chronic stroke | EG: 2.22 ± 1.09 CG: 1.78 ± 0.67 | Gastrocnemius muscle | Inmediatly after therapy, weeks 1 and 4 | 4 | 0.1 | 2000 | MAS | EG: −0.52 ± 2.258 CG: 0.11 ± 1.967 |
| Leng, Y. et al. (2020) [32] | China | RCT | 27 (5) | EG: 51.14 ± 13.68 CG: 8.921 ± 10.08 | Chronic stroke | EG: 2 ± 0.78 CG: 1.85 ± 0.80 | Wrist Joint | Inmediatly after therapy and week 1 | 4 | 0.038 | 1500 | MAS | EG: −0.96 ± 2.873 CG: −0.7 ± 1.082 |
| Tabra, S.A.A., Zaghloul, M.I. and Alaskar, D.S. (2021) [35] | Egypt | RCT | 40 (5) | EG: 55.70 ± 9.30 CG: 53.85 ± 10.20 | Chronic stroke | EG: 3.17 ± 0.66 CG: 3.12 ± 0.66 | Wrist and hand muscles | Weeks 2 and 12 | 15 | 0.25–0.84 | 2000–3000 | MAS | EG: −1.55 ± 0.742 CG: 0 ± 0.787 |
| Aslan, S.Y. et al. (2021) [36] | Turkey | RCT | 49 (22) | EG1: 57.5 ± 14.3 EG2: 58.8 ± 10.8 CG: 60.6 ± 9.6 | Chronic stroke | EG1: 2.5 ± 0.7 EG2: 2.2 ± 1 CG: 2.1 ± 0.9 | Ankle plantar flexor | Weeks 2 and 6 | 10 | NR | 1500 | MAS | EG1: −0.91 ± 2.787 EG2: −0.31 ± 4.306 CG: −0.15 ± 3.316 |
| Brunelli, S. et al. (2022) [33] | Italy | RCT | 32 (13) | EG: 54.80 ± 17.29 CG: 62.18 ± 16.17 | Chronic stroke | EG: 1.09 ± 1.69 CG: 0.91 ± 1.94 | Anterior area of forearm or arm or shoulder | Weeks 1 and 4 | 10 | NR | 2000 | MAS | EG: −0.5 ± 6.471 CG: 1.13 ± 9.046 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otero-Luis, I.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Martinez-Rodrigo, A.; Pascual-Morena, C.; Moreno-Herráiz, N.; Saz-Lara, A. Effectiveness of Extracorporeal Shock Wave Therapy in Treatment of Spasticity of Different Aetiologies: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 1323. https://doi.org/10.3390/jcm13051323
Otero-Luis I, Cavero-Redondo I, Álvarez-Bueno C, Martinez-Rodrigo A, Pascual-Morena C, Moreno-Herráiz N, Saz-Lara A. Effectiveness of Extracorporeal Shock Wave Therapy in Treatment of Spasticity of Different Aetiologies: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(5):1323. https://doi.org/10.3390/jcm13051323
Chicago/Turabian StyleOtero-Luis, Iris, Iván Cavero-Redondo, Celia Álvarez-Bueno, Arturo Martinez-Rodrigo, Carlos Pascual-Morena, Nerea Moreno-Herráiz, and Alicia Saz-Lara. 2024. "Effectiveness of Extracorporeal Shock Wave Therapy in Treatment of Spasticity of Different Aetiologies: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 5: 1323. https://doi.org/10.3390/jcm13051323
APA StyleOtero-Luis, I., Cavero-Redondo, I., Álvarez-Bueno, C., Martinez-Rodrigo, A., Pascual-Morena, C., Moreno-Herráiz, N., & Saz-Lara, A. (2024). Effectiveness of Extracorporeal Shock Wave Therapy in Treatment of Spasticity of Different Aetiologies: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 13(5), 1323. https://doi.org/10.3390/jcm13051323








