A Three-Dimensional Evaluation of Skeletal and Dentoalveolar Changes in Growing Class II Patients after Functional Appliance Therapy: A Retrospective Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
- Treatment with a removable functional appliance followed by full fixed appliances.
- Overjet of more than 3 mm and a Class II molar relationship (at least half cusp on both sides, or a full Class II molar relationship on one side in case of subdivision).
- Pre- (T0) and post-treatment (T1) CBCT scans and 3D digital models.
- Caucasian origin.
- Class I or mild Class II patients (less than half cusp Class II molar relationship on both sides);
- No use of any kind of functional appliance;
- Limited use of Class II elastics was accepted;
- Pre- (T0) and post-treatment (T1) CBCT scans and 3D digital models.
2.1. Image Processing and Analysis
2.2. 3D Digital Model Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McNamara, J.A., Jr. Components of class II malocclusion in children 8–10 years of age. Angle Orthod. 1981, 51, 177–202. [Google Scholar]
- McLain, J.B.; Proffitt, W.R. Oral health status in the United States: Prevalence of malocclusion. J. Dent. Educ. 1985, 49, 386–397. [Google Scholar] [CrossRef]
- Pancherz, H.; Zieber, K.; Hoyer, B. Cephalometric characteristics of Class II division 1 and Class II division 2 malocclusions: A comparative study in children. Angle Orthod. 1997, 67, 111–120. [Google Scholar]
- Jacob, H.B.; Buschang, P.H. Mandibular growth comparisons of Class I and Class II division 1 skeletofacial patterns. Angle Orthod. 2014, 84, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., 3rd; McNamara, J.A., Jr.; Lawrence, T.M. Components of adult Class II open-bite malocclusion. J. Oral Maxillofac. Surg. 1985, 43, 92–105. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A., Jr.; Bookstein, F.L.; Shaughnessy, T.G. Skeletal and dental changes following functional regulator therapy on class II patients. Am. J. Orthod. 1985, 88, 91–110. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A., Jr.; Bryan, F.A. Long-term mandibular adaptations to protrusive function: An experimental study in Macaca mulatta. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 98–108. [Google Scholar] [CrossRef]
- Woodside, D.G.; Metaxas, A.; Altuna, G. The influence of functional appliance therapy on glenoid fossa remodeling. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 181–198. [Google Scholar] [CrossRef]
- Marsico, E.; Gatto, E.; Burrascano, M.; Matarese, G.; Cordasco, G. Effectiveness of orthodontic treatment with functional appliances on mandibular growth in the short term. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 24–36. [Google Scholar] [CrossRef]
- de Almeida, M.R.; Flores-Mir, C.; Brandao, A.G.; de Almeida, R.R.; de Almeida-Pedrin, R.R. Soft tissue changes produced by a banded-type Herbst appliance in late mixed dentition patients. World J. Orthod. 2008, 9, 121–131. [Google Scholar]
- Pancherz, H.; Ruf, S.; Kohlhas, P. “Effective condylar growth” and chin position changes in Herbst treatment: A cephalometric roentgenographic long-term study. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 437–446. [Google Scholar] [CrossRef]
- Serbesis-Tsarudis, C.; Pancherz, H. “Effective” TMJ and chin position changes in Class II treatment. Angle Orthod. 2008, 78, 813–818. [Google Scholar] [CrossRef]
- Creekmore, T.D.; Radney, L.J. Frankel appliance therapy: Orthopedic or orthodontic? Am. J. Orthod. 1983, 83, 89–108. [Google Scholar] [CrossRef]
- Gianelly, A.A.; Brosnan, P.; Martignoni, M.; Bernstein, L. Mandibular growth, condyle position and Frankel appliance therapy. Angle Orthod. 1983, 53, 131–142. [Google Scholar]
- Cozza, P.; Baccetti, T.; Franchi, L.; De Toffol, L.; McNamara, J.A., Jr. Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 599.e1–599.e12; discussion e1–e6. [Google Scholar] [CrossRef]
- Perinetti, G.; Primozic, J.; Franchi, L.; Contardo, L. Treatment Effects of Removable Functional Appliances in Pre-Pubertal and Pubertal Class II Patients: A Systematic Review and Meta-Analysis of Controlled Studies. PLoS ONE 2015, 10, e0141198. [Google Scholar] [CrossRef] [PubMed]
- Vargervik, K.; Harvold, E.P. Response to activator treatment in Class II malocclusions. Am. J. Orthod. 1985, 88, 242–251. [Google Scholar] [CrossRef]
- Baccetti, T.; Franchi, L.; Toth, L.R.; McNamara, J.A., Jr. Treatment timing for Twin-block therapy. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, M.S.; Kharbanda, O.P.; Sidhu, S.S. Cephalometric analysis of changes produced by a modified Herbst appliance in the treatment of Class II division 1 malocclusion. Br. J. Orthod. 1995, 22, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Wieslander, L.; Lagerstrom, L. The effect of activator treatment on class II malocclusions. Am. J. Orthod. 1979, 75, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Robertson, N.R. An examination of treatment changes in children treated with the function regulator of Frankel. Am. J. Orthod. 1983, 83, 299–310. [Google Scholar] [CrossRef]
- Pittayapat, P.; Bornstein, M.M.; Imada, T.S.; Coucke, W.; Lambrichts, I.; Jacobs, R. Accuracy of linear measurements using three imaging modalities: Two lateral cephalograms and one 3D model from CBCT data. Eur. J. Orthod. 2015, 37, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Quintero, J.C.; Trosien, A.; Hatcher, D.; Kapila, S. Craniofacial imaging in orthodontics: Historical perspective, current status, and future developments. Angle Orthod. 1999, 69, 491–506. [Google Scholar]
- Baumrind, S.; Frantz, R.C. The reliability of head film measurements. 2. Conventional angular and linear measures. Am. J. Orthod. 1971, 60, 505–517. [Google Scholar] [CrossRef]
- Baumrind, S.; Frantz, R.C. The reliability of head film measurements. 1. Landmark identification. Am. J. Orthod. 1971, 60, 111–127. [Google Scholar] [CrossRef] [PubMed]
- Arai, Y.; Tammisalo, E.; Iwai, K.; Hashimoto, K.; Shinoda, K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac. Radiol. 1999, 28, 245–248. [Google Scholar] [CrossRef]
- Mozzo, P.; Procacci, C.; Tacconi, A.; Martini, P.T.; Andreis, I.A. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur. Radiol. 1998, 8, 1558–1564. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, P.M.; Melsen, B. The use of cone-beam computed tomography in an orthodontic department in between research and daily clinic. World J. Orthod. 2008, 9, 269–282. [Google Scholar]
- de Oliveira, A.E.; Cevidanes, L.H.; Phillips, C.; Motta, A.; Burke, B.; Tyndall, D. Observer reliability of three-dimensional cephalometric landmark identification on cone-beam computerized tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 256–265. [Google Scholar] [CrossRef]
- Cattaneo, P.M.; Yung, A.K.C.; Holm, A.; Mashaly, O.M.; Cornelis, M.A. 3D landmarks of Craniofacial Imaging and subsequent considerations on superimpositions in orthodontics-The Aarhus perspective. Orthod. Craniofac Res. 2019, 22 (Suppl. 1), 21–29. [Google Scholar] [CrossRef]
- Yildirim, E.; Karacay, S.; Erkan, M. Condylar response to functional therapy with Twin-Block as shown by cone-beam computed tomography. Angle Orthod. 2014, 84, 1018–1025. [Google Scholar] [CrossRef]
- Elfeky, H.Y.; Fayed, M.S.; Alhammadi, M.S.; Soliman, S.A.Z.; El Boghdadi, D.M. Three-dimensional skeletal, dentoalveolar and temporomandibular joint changes produced by Twin Block functional appliance. J. Orofac. Orthop. 2018, 79, 245–258. [Google Scholar] [CrossRef]
- Jiang, Y.Y.; Sun, L.; Wang, H.; Zhao, C.Y.; Zhang, W.B. Three-dimensional cone beam computed tomography analysis of temporomandibular joint response to the Twin-block functional appliance. Korean J. Orthod. 2020, 50, 86–97. [Google Scholar] [CrossRef]
- Björk, A. The face in profile: An anthropological X-ray investigation on Swedish children and conscripts. In Svensk Tandläkare-Tidskrift; Berlingska Boktryckeriet: Lund, Sweden, 1947; Volume 40, p. 180. [Google Scholar]
- Ludlow, J.B.; Timothy, R.; Walker, C.; Hunter, R.; Benavides, E.; Samuelson, D.B.; Scheske, M.J. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac. Radiol. 2015, 44, 20140197. [Google Scholar] [CrossRef]
- Kapila, S.D.; Nervina, J.M. CBCT in orthodontics: Assessment of treatment outcomes and indications for its use. Dentomaxillofac. Radiol. 2015, 44, 20140282. [Google Scholar] [CrossRef] [PubMed]
- LeCornu, M.; Cevidanes, L.H.; Zhu, H.; Wu, C.D.; Larson, B.; Nguyen, T. Three-dimensional treatment outcomes in Class II patients treated with the Herbst appliance: A pilot study. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 818–830. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.; Hansen, K.; Hagg, U. Class II correction in patients treated with class II elastics and with fixed functional appliances: A comparative study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 142–149. [Google Scholar] [CrossRef]
- Wei, R.Y.; Atresh, A.; Ruellas, A.; Cevidanes, L.H.S.; Nguyen, T.; Larson, B.E.; Mangum, J.E.; Manton, D.J.; Schneider, P.M. Three-dimensional condylar changes from Herbst appliance and multibracket treatment: A comparison with matched Class II elastics. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 505–517.e6. [Google Scholar] [CrossRef]
- Antonarakis, G.S.; Kiliaridis, S. Short-term anteroposterior treatment effects of functional appliances and extraoral traction on class II malocclusion. A meta-analysis. Angle Orthod. 2007, 77, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, J.F.; Phillips, C.; Koch, G.; Proffit, W.R. The effect of early intervention on skeletal pattern in Class II malocclusion: A randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Baysal, A.; Uysal, T. Dentoskeletal effects of Twin Block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur. J. Orthod. 2014, 36, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Siara-Olds, N.J.; Pangrazio-Kulbersh, V.; Berger, J.; Bayirli, B. Long-term dentoskeletal changes with the Bionator, Herbst, Twin Block, and MARA functional appliances. Angle Orthod. 2010, 80, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Mills, C.M.; McCulloch, K.J. Posttreatment changes after successful correction of Class II malocclusions with the twin block appliance. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 24–33. [Google Scholar] [CrossRef]
- Faltin, K.J.; Faltin, R.M.; Baccetti, T.; Franchi, L.; Ghiozzi, B.; McNamara, J.A., Jr. Long-term effectiveness and treatment timing for Bionator therapy. Angle Orthod. 2003, 73, 221–230. [Google Scholar]
- O’Brien, K.; Wright, J.; Conboy, F.; Sanjie, Y.; Mandall, N.; Chadwick, S.; Connolly, I.; Cook, P.; Birnie, D.; Hammond, M.; et al. Effectiveness of early orthodontic treatment with the Twin-block appliance: A multicenter, randomized, controlled trial. Part 1: Dental and skeletal effects. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 234–243; quiz 339. [Google Scholar] [CrossRef]
- Perillo, L.; Femiano, A.; Palumbo, S.; Contardo, L.; Perinetti, G. Skeletal and dental effects produced by functional regulator-2 in pre-pubertal class II patients: A controlled study. Progress. Orthod. 2013, 14, 18. [Google Scholar] [CrossRef] [PubMed]
- Ehsani, S.; Nebbe, B.; Normando, D.; Lagravere, M.O.; Flores-Mir, C. Short-term treatment effects produced by the Twin-block appliance: A systematic review and meta-analysis. Eur. J. Orthod. 2015, 37, 170–176. [Google Scholar] [CrossRef] [PubMed]
| Abbreviation | Landmark | Definition |
|---|---|---|
| A-Point | A-Point | Deepest point on the concave outline of the upper labial alveolar process |
| ANS | Anterior nasal spine | Most anterior midpoint of the anterior nasal spine |
| Apex L1 L | Apex central lower incisor—left | Apex central lower incisor—left |
| Apex L1 R | Apex central lower incisor—right | Apex central lower incisor—right |
| Apex U1 L | Apex central upper incisor—left | Apex central upper incisor—left |
| Apex U1 R | Apex central upper incisor—right | Apex central upper incisor—right |
| B-point | B-Point | Deepest point on the concave outline of the lower labial alveolar process |
| Ba | Basion | The median point of the anterior margin of the foramen magnum |
| CoL | Condylion—left | Most superior—posterior point of the mandibular condyle—left |
| CoR | Condylion—right | Most superior—posterior point of the mandibular condyle—right |
| Crib plate L | Cribriform plate—left | Deepest point of the cribriform plate—left |
| Crib plate R | Cribriform plate—right | Deepest point of the cribriform plate—right |
| Crib plate mid | Cribriform plate—mid | Deepest point of the cribriform plate—mid |
| FML | Foramen mentale—left | Foramen for n. mentalis sin. |
| FMR | Foramen mentale—right | Foramen for n. mentalis dext. |
| FPM-L | Foramen palatinum major—left | Foramen for n. palatinus major sin. and a. palatina descendes sin. |
| FPM-R | Foramen palatinum major—right | Foramen for n. palatinus major dext. and a. palatina descendes dext. |
| Gn | Gnathion | Most anterior—inferior point on the mandibular symphysis |
| GoL | Gonion—left | The midpoint at the angle of the mandible—left |
| GoR | Gonion—right | The midpoint at the angle of the mandible—right |
| L1L | Incisal edge central lower incisor—left | Incisal edge central lower incisor—left |
| L1R | Incisal edge central lower incisor—right | Incisal edge central lower incisor—right |
| L6L | Mesiolingual cusp lower first molar—left | Mesiolingual cusp lower first molar—left |
| L6R | Mesiolingual cusp lower first molar—right | Mesiolingual cusp lower first molar—right |
| Me | Menton | The lowest point on the lower border of the mandibular symphysis |
| N | Nasion | Anterior point of the frontonasal suture |
| PNS | Posterior nasal spine | Most posterior midpoint of the posterior nasal spine |
| Pog | Pogonion | Most anterior midpoint of the chin |
| S | Sella Turcica | Center of sella turcica |
| U1L | Incisal edge central upper incisor—left | Incisal edge central upper incisor—left |
| U1R | Incisal edge central upper incisor—right | Incisal edge central upper incisor—right |
| U6L | Mesiopalatal cusp upper first molar—left | Mesiopalatal cusp upper first molar—left |
| U6R | Mesiopalatal cusp upper first molar—right | Mesiopalatal cusp upper first molar—right |
| Abbreviation | Plane | Definition |
|---|---|---|
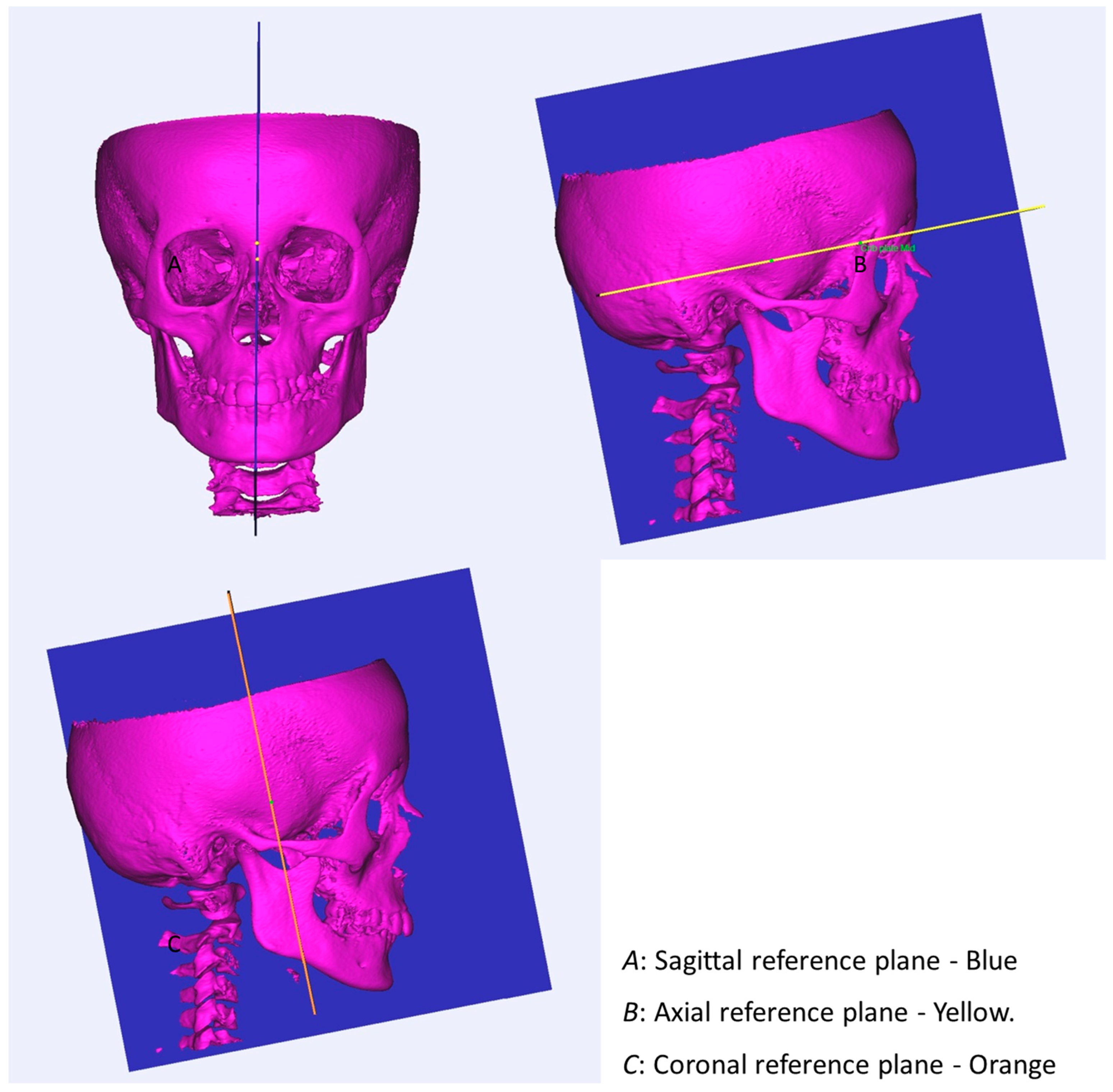
| N-S-Ba | Sagittal plane | The longitudinal plane that divides the head into right and left sections |
| S-crib plate mid-perp to sagittal plane | Axial plane | Plane perpendicular to the sagittal plane going through the stable structures of the cranial base |
| S-perp to axial plane and sagittal plane | Coronal plane | Plane perpendicular to the sagittal plane and axial plane passing through sella |
| GoL-Me-GoR | Mandibular plane | Tangent to the lower border of the body of the mandible |
| U1R-U6R-U6L | Occlusal plane | A plane passing through the occlusal surfaces of the teeth in maximum interdigitation |
| ANS-PNS and perp to sagittal plane | Palatal plane | Plane perpendicular to the sagittal plane going through the most anterior and posterior point of the hard palate |
| U6R—perp to sagittal plane and occlusal plane | Wits plane | A vertical plane going through the first upper molar enabling the measurements for the Wits appraisal |
| L1L-Apex L1L | Mand. incisor inclination L | Plane going through the incisal edge and apex of the left central lower incisor perpendicular to the sagittal plane |
| L1R-Apex L1R | Mand. incisor inclination R | Plane going through the incisal edge and apex of the right central lower incisor perpendicular to the sagittal plane |
| U1L-Apex U1L | Max. incisor inclination L | Plane going through the incisal edge and apex of the left upper central incisor perpendicular to the sagittal plane |
| U1R-Apex U1R | Max. incisor inclination R | Plane going through the incisal edge and apex of the right upper central incisor perpendicular to the sagittal plane |
| Measurement | Definition |
|---|---|
| Corpus mand. length Left | Linear measurement between GoL and Gn |
| Corpus mand. length Right | Linear measurement between GoR and Gn |
| Effective mand. length Left | Linear measurement between CoL and Gn |
| Effective mand. length Right | Linear measurement between CoR and Gn |
| LAFH | Linear measurement between ANS and Me describing the lower anterior face height |
| UAFH | Linear measurement between N and ANS describing the upper anterior face height |
| AFH | Linear measurement between N and Me describing the total anterior face height |
| Palatal length | Linear measurement between PNS and ANS |
| Palatal width | Linear measurement between foramen palatinum major left and right |
| Ramus length (left) | Linear measurement between CoL and GoL |
| Ramus length (right) | Linear measurement between CoR and GoR |
| N-S-Ba angle | Angle formed by the intersection of lines SN and SBa, which measures the cranial base angle |
| ANB angle | Angle formed by the intersection of lines NA and NB, which measures the anterior– posterior relation of the maxilla and the mandible |
| SNA angle | Angle formed by the intersection of lines SN and NA, which measures the horizontal position of the maxilla in relation to the cranial base |
| SNB angle | Angle formed by the intersection of lines SN and NB, which measures the horizontal position of the mandible in relation to the cranial base |
| Wits appraisal | Distance from Wits plane to A-point subtracted the distance from wits plane to B-point |
| Upper right central incisor inclination | Angle between the palatal plane and the plane for max. incisor inclination—right |
| Upper left central incisor inclination | Angle between the palatal plane and the plane for max. incisor inclination—left |
| Lower right central incisor inclination | Angle between the mandibular plane and the plane for mand. incisor inclination—right |
| Lower left central incisor inclination | Angle between the mandibular plane and the plane for mand. incisor inclination—left |
| Measurement | FAG | CG |
|---|---|---|
| ANB (°) | 0.37 | 0.28 |
| SNA (°) | 0.47 | 0.57 |
| SNB (°) | 0.37 | 0.46 |
| N-S-Ba (°) | 0.62 | 0.74 |
| Corpus mandibular length left (mm) | 0.80 | 1.08 |
| Corpus mandibular length right (mm) | 0.87 | 1.04 |
| Ramus length left (mm) | 1.02 | 1.15 |
| Ramus length right (mm) | 1.09 | 1.07 |
| Effective mandibular length left (mm) | 0.55 | 0.57 |
| Effective mandibular length right (mm) | 0.47 | 0.58 |
| Palatal length (mm) | 1.05 | 1.40 |
| Palatal width (mm) | 0.61 | 0.52 |
| Total anterior face height (mm) | 0.44 | 0.61 |
| Upper anterior face height (mm) | 0.46 | 0.59 |
| Lower anterior face height (mm) | 0.48 | 0.45 |
| Wits appraisal (mm) | 0.46 | 0.35 |
| Upper right central incisor inclination (°) | 1.22 | 1.29 |
| Upper left central incisor inclination (°) | 1.02 | 1.15 |
| Lower right central incisor inclination (°) | 1.27 | 1.22 |
| Lower left central incisor inclination (°) | 0.92 | 1.09 |
| Measurement | FAG | CG | Comparison | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p-Value | Significance | |
| Overjet (mm) | 8.9 | 2.8 | 4.0 | 1.7 | <0.01 | * |
| Overbite (mm) | 4.0 | 1.7 | 3.8 | 1.5 | 0.45 | NS |
| ANB (°) | 5.7 | 2.0 | 3.2 | 1.4 | <0.01 | * |
| SNA (°) | 80.1 | 3.7 | 79.6 | 4.8 | 0.95 | NS |
| SNB (°) | 74.4 | 3.4 | 76.6 | 4.7 | 0.04 | * |
| S-N-Ba (°) | 132.1 | 4.4 | 132 | 7.0 | 0.97 | NS |
| Corpus mandibular length (left) (mm) | 80.4 | 4.0 | 82.7 | 5.1 | 0.13 | NS |
| Corpus mandibular length (right) (mm) | 80.1 | 3.4 | 81.4 | 4.9 | 0.31 | NS |
| Ramus length (left) (mm) | 49.9 | 3.0 | 53.7 | 4.5 | <0.01 | * |
| Ramus length (right) (mm) | 50.6 | 3.2 | 54.0 | 4.1 | <0.01 | * |
| Effective mandibular length (left) (mm) | 112.5 | 4.0 | 116.9 | 5.9 | 0.01 | * |
| Effective mandibular length (right) (mm) | 113.0 | 4.1 | 116.6 | 5.9 | 0.02 | * |
| Palatal length (mm) | 53.2 | 2.5 | 51.9 | 3.5 | 0.17 | NS |
| Palatal width (mm) | 27.5 | 1.5 | 27.6 | 2.3 | 0.89 | NS |
| Total anterior face height (mm) | 107.8 | 6.6 | 109.6 | 6.2 | 0.36 | NS |
| Upper anterior face height (mm) | 49.1 | 2.6 | 49.6 | 2.8 | 0.52 | NS |
| Lower anterior face height (mm) | 61.0 | 5.7 | 61.5 | 4.7 | 0.77 | NS |
| Wits appraisal (mm) | 5.6 | 2.7 | 0.5 | 1.5 | <0.01 | * |
| Upper right central incisor inclination (°) | 67.3 | 6.5 | 72.5 | 6.6 | 0.02 | * |
| Upper left central incisor inclination (°) | 66.7 | 5.9 | 72.0 | 7.0 | 0.01 | * |
| Lower right central incisor inclination (°) | 85.2 | 3.4 | 83.5 | 6.5 | 0.27 | NS |
| Lower left central incisor inclination (°) | 84.5 | 3.9 | 82.3 | 6.6 | 0.29 | NS |
| Measurement | FAG (T1-T0) | CG (T1-T0) | Comparison of Treatment Effect | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | p-Value | Significance | Mean | SD | p-Value | Significance | p-Value | Significance | |
| Overjet (mm) | −6.8 | 2.8 | <0.01 | * | −1.8 | 1.8 | <0.01 | * | <0.01 | * |
| Overbite (mm) | −2.2 | 1.8 | <0.01 | * | −2.2 | 1.6 | <0.01 | * | 0.97 | NS |
| ANB (°) | −1.2 | 1.5 | <0.01 | * | −0.1 | 0.6 | 0.37 | NS | 0.01 | * |
| SNA (°) | −0.8 | 0.8 | <0.01 | * | −0.3 | 0.7 | 0.06 | NS | 0.06 | * |
| SNB (°) | 0.5 | 1.9 | 0.18 | NS | −0.3 | 0.9 | 0.19 | NS | 0.10 | NS |
| N-S-Ba (°) | −0.1 | 1 | 0.52 | NS | 0.2 | 1.1 | 0.38 | NS | 0.27 | NS |
| Corpus mandibular length (left) (mm) | 3.6 | 1.8 | <0.01 | * | 2.3 | 1.8 | <0.01 | * | 0.02 | * |
| Corpus mandibular length (right) (mm) | 3.8 | 1.8 | <0.01 | * | 2.8 | 1.9 | <0.01 | * | 0.09 | NS |
| Ramus length (left) (mm) | 4.5 | 2.2 | <0.01 | * | 3 | 1.9 | <0.01 | * | 0.04 | * |
| Ramus length (right) (mm) | 4 | 1.9 | <0.01 | * | 2.5 | 1.8 | <0.01 | * | 0.02 | * |
| Effective mandibular length (left) (mm) | 6.3 | 2.6 | <0.01 | * | 3.9 | 2.6 | <0.01 | * | <0.01 | * |
| Effective mandibular length (right) (mm) | 6.1 | 2.6 | <0.01 | * | 3.8 | 2.2 | <0.01 | * | 0.01 | * |
| Palatal length (mm) | 1.8 | 1.4 | <0.01 | * | 1.3 | 1.1 | <0.01 | * | 0.24 | NS |
| Palatal width (mm) | 1.4 | 0.7 | <0.01 | * | 0.8 | 0.5 | <0.01 | * | <0.01 | * |
| Total anterior face height (mm) | 7.1 | 2.6 | <0.01 | * | 4.6 | 2.3 | <0.01 | * | <0.01 | * |
| Upper anterior face height (mm) | 2.2 | 1.3 | <0.01 | * | 1.2 | 1.1 | <0.01 | * | 0.01 | * |
| Lower anterior face height (mm) | 4.8 | 2.1 | <0.01 | * | 3.5 | 2 | <0.01 | * | 0.01 | * |
| Wits appraisal | 4 | 2.3 | <0.01 | * | −0.4 | 0.9 | 0.06 | NS | <0.01 | * |
| Upper right central incisor inclination (°) | 6.4 | 7.5 | <0.01 | * | −2 | 4.9 | 0.1 | NS | <0.01 | * |
| Upper left central incisor inclination (°) | 6.9 | 6.8 | <0.01 | * | −1.8 | 6.9 | 0.3 | NS | <0.01 | * |
| Lower right central incisor inclination (°) | −8.9 | 4.9 | <0.01 | * | −4.5 | 6.0 | 0.01 | * | 0.01 | * |
| Lower left central incisor inclination (°) | −8.8 | 5.8 | <0.01 | * | −5.5 | 8.0 | 0.01 | * | 0.13 | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cattaneo, P.M.; Holm, A.; Yung, A.K.C.; Isidor, S.; Cornelis, M.A. A Three-Dimensional Evaluation of Skeletal and Dentoalveolar Changes in Growing Class II Patients after Functional Appliance Therapy: A Retrospective Case-Control Study. J. Clin. Med. 2024, 13, 1315. https://doi.org/10.3390/jcm13051315
Cattaneo PM, Holm A, Yung AKC, Isidor S, Cornelis MA. A Three-Dimensional Evaluation of Skeletal and Dentoalveolar Changes in Growing Class II Patients after Functional Appliance Therapy: A Retrospective Case-Control Study. Journal of Clinical Medicine. 2024; 13(5):1315. https://doi.org/10.3390/jcm13051315
Chicago/Turabian StyleCattaneo, Paolo M., Annemarie Holm, Augustine K. C. Yung, Stig Isidor, and Marie A. Cornelis. 2024. "A Three-Dimensional Evaluation of Skeletal and Dentoalveolar Changes in Growing Class II Patients after Functional Appliance Therapy: A Retrospective Case-Control Study" Journal of Clinical Medicine 13, no. 5: 1315. https://doi.org/10.3390/jcm13051315
APA StyleCattaneo, P. M., Holm, A., Yung, A. K. C., Isidor, S., & Cornelis, M. A. (2024). A Three-Dimensional Evaluation of Skeletal and Dentoalveolar Changes in Growing Class II Patients after Functional Appliance Therapy: A Retrospective Case-Control Study. Journal of Clinical Medicine, 13(5), 1315. https://doi.org/10.3390/jcm13051315







