Fracture Severity and Triangular Fibrocartilage Complex Injury in Distal Radius Fractures with or without Osteoporosis
Abstract
1. Introduction
2. Materials and Methods
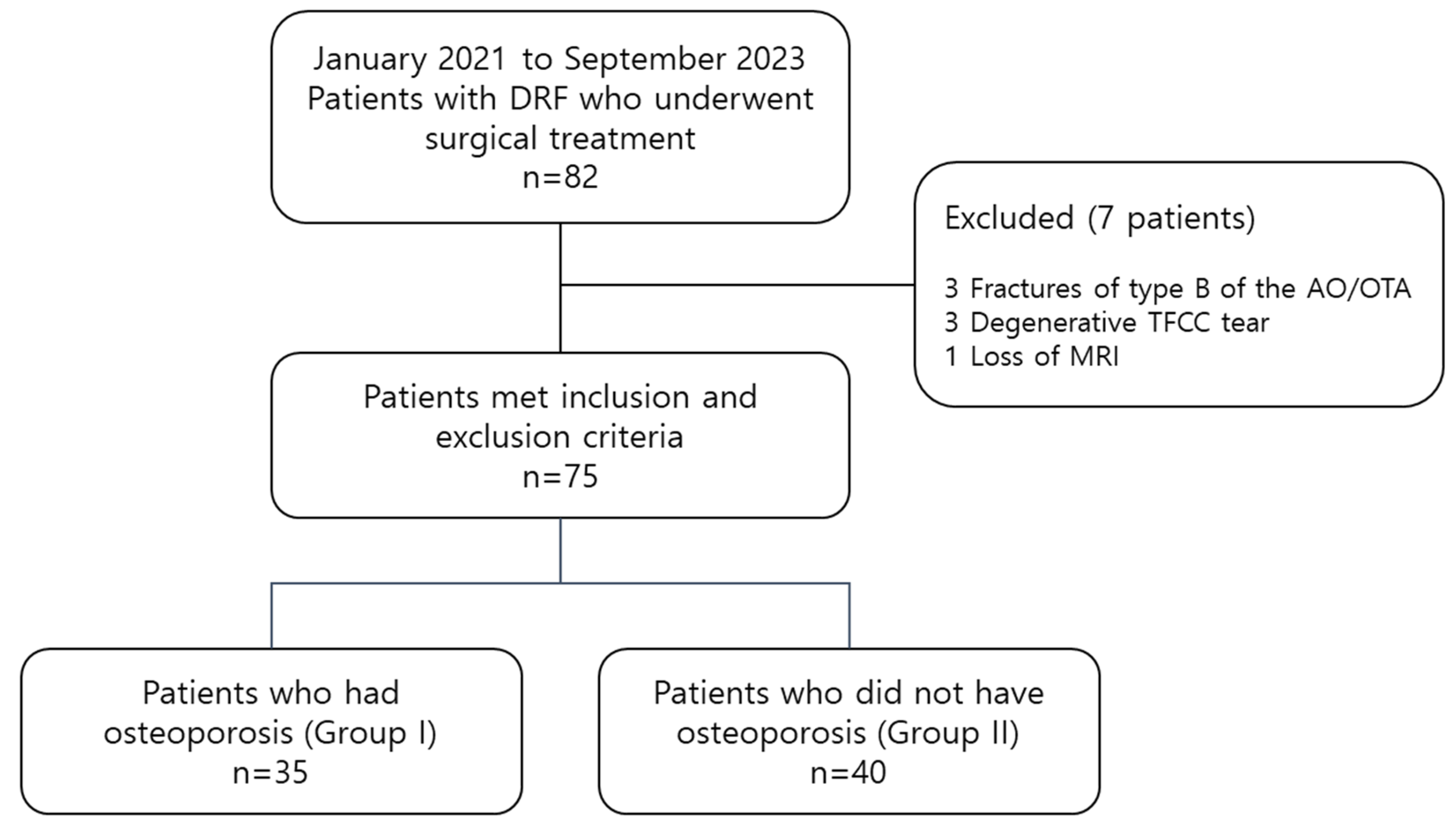
2.1. Patient Selection
2.2. Radiologic Evaluations
2.3. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rundgren, J.; Bojan, A.; Mellstrand Navarro, C.; Enocson, A. Epidemiology, classification, treatment and mortality of distal radius fractures in adults: An observational study of 23,394 fractures from the national Swedish fracture register. BMC Musculoskelet. Disord. 2020, 21, 88. [Google Scholar] [CrossRef]
- Lindau, T.; Adlercreutz, C.; Aspenberg, P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J. Hand Surg. Am. 2000, 25, 464–468. [Google Scholar] [CrossRef]
- Atzei, A.; Luchetti, R. Foveal TFCC tear classification and treatment. Hand Clin. 2011, 27, 263–272. [Google Scholar] [CrossRef]
- Kasapinova, K.; Kamiloski, V. Outcomes of surgically treated distal radius fractures associated with triangular fibrocartilage complex injury. J. Hand Ther. 2020, 33, 339–345. [Google Scholar] [CrossRef]
- Robin, B.N.; Ellington, M.D.; Jupiter, D.C.; Brennan, M.L. Relationship of bone mineral density of spine and femoral neck to distal radius fracture stability in patients over 65. J. Hand Surg. Am. 2014, 39, 861–866.e3. [Google Scholar] [CrossRef]
- Sakai, A.; Oshige, T.; Zenke, Y.; Suzuki, M.; Yamanaka, Y.; Nakamura, T. Association of bone mineral density with deformity of the distal radius in low-energy Colles’ fractures in Japanese women above 50 years of age. J. Hand Surg. Am. 2008, 33, 820–826. [Google Scholar] [CrossRef]
- Abe, Y.; Moriya, A.; Tominaga, Y.; Yoshida, K. Dorsal Tear of Triangular Fibrocartilage Complex: Clinical Features and Treatment. J. Wrist Surg. 2016, 5, 42–46. [Google Scholar] [CrossRef]
- Minami, A. Triangular fibrocartilage complex tears. Hand Surg. 2015, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kastenberger, T.; Kaiser, P.; Schmidle, G.; Schwendinger, P.; Gabl, M.; Arora, R. Arthroscopic assisted treatment of distal radius fractures and concomitant injuries. Arch. Orthop. Trauma Surg. 2020, 140, 623–638. [Google Scholar] [CrossRef] [PubMed]
- Tomori, Y.; Nanno, M.; Takai, S. The Presence and the Location of an Ulnar Styloid Fracture Associated With Distal Radius Fracture Predict the Presence of Triangular Fibrocartilage Complex 1B Injury. Arthroscopy 2020, 36, 2674–2680. [Google Scholar] [CrossRef] [PubMed]
- Nozaki, T.; Rafijah, G.; Yang, L.; Ueno, T.; Horiuchi, S.; Hitt, D.; Yoshioka, H. High-resolution 3 T MRI of traumatic and degenerative triangular fibrocartilage complex (TFCC) abnormalities using Palmer and Outerbridge classifications. Clin. Radiol. 2017, 72, 904.e1–904.e10. [Google Scholar] [CrossRef]
- Ochman, S.; Wieskötter, B.; Langer, M.; Vieth, V.; Raschke, M.J.; Stehling, C. High-resolution MRI (3T-MRI) in diagnosis of wrist pain: Is diagnostic arthroscopy still necessary? Arch. Orthop. Trauma Surg. 2017, 137, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Yan, B.; Xu, Z.; Chen, Y.; Yin, W. Prevalence of triangular fibrocartilage complex injuries in patients with distal radius fractures: A 3.0T magnetic resonance imaging study. J. Int. Med. Res. 2019, 47, 3648–3655. [Google Scholar] [CrossRef] [PubMed]
- Graff, S.; Jupiter, J. Fracture of the distal radius: Classification of treatment and indications for external fixation. Injury 1994, 25 (Suppl. 4), SD14–SD25. [Google Scholar] [CrossRef] [PubMed]
- Schousboe, J.T.; Ensrud, K.E. Diagnostic criteria for osteoporosis should not be expanded. Lancet Diabetes Endocrinol. 2015, 3, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Goldfarb, C.A.; Yin, Y.; Gilula, L.A.; Fisher, A.J.; Boyer, M.I. Wrist fractures: What the clinician wants to know. Radiology 2001, 219, 11–28. [Google Scholar] [CrossRef]
- Metz, V.M.; Gilula, L.A. Imaging techniques for distal radius fractures and related injuries. Orthop. Clin. N. Am. 1993, 24, 217–228. [Google Scholar] [CrossRef]
- Yoda, T.; Watanabe, K.; Shirahata, M.; Ogose, A.; Endo, N. Association between bone mineral density and ulnar styloid fracture in older Japanese adults with low-energy distal radius fracture. Arch. Osteoporos. 2020, 15, 51. [Google Scholar] [CrossRef]
- Jayakumar, P.; Teunis, T.; Giménez, B.B.; Verstreken, F.; Di Mascio, L.; Jupiter, J.B. AO Distal Radius Fracture Classification: Global Perspective on Observer Agreement. J. Wrist Surg. 2017, 6, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Lewiecki, E.M.; Binkley, N.; Morgan, S.L.; Shuhart, C.R.; Camargos, B.M.; Carey, J.J.; Gordon, C.M.; Jankowski, L.G.; Lee, J.K.; Leslie, W.D.; et al. Best Practices for Dual-Energy X-ray Absorptiometry Measurement and Reporting: International Society for Clinical Densitometry Guidance. J. Clin. Densitom. 2016, 19, 127–140. [Google Scholar] [CrossRef]
- Kim, K.W.; Lee, C.H.; Choi, J.H.; Ahn, J.M.; Gong, H.S. Distal radius fracture with concomitant ulnar styloid fracture: Does distal radioulnar joint stability depend on the location of the ulnar styloid fracture? Arch. Orthop. Trauma Surg. 2023, 143, 839–845. [Google Scholar] [CrossRef]
- Clayton, R.A.; Gaston, M.S.; Ralston, S.H.; Court-Brown, C.M.; McQueen, M.M. Association between decreased bone mineral density and severity of distal radial fractures. J. Bone Jt. Surg. Am. 2009, 91, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Lill, C.A.; Goldhahn, J.; Albrecht, A.; Eckstein, F.; Gatzka, C.; Schneider, E. Impact of bone density on distal radius fracture patterns and comparison between five different fracture classifications. J. Orthop. Trauma 2003, 17, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Dhainaut, A.; Daibes, K.; Odinsson, A.; Hoff, M.; Syversen, U.; Haugeberg, G. Exploring the relationship between bone density and severity of distal radius fragility fracture in women. J. Orthop. Surg. Res. 2014, 9, 57. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hollevoet, N.; Verdonk, R. Outcome of distal radius fractures in relation to bone mineral density. Acta Orthop. Belg. 2003, 69, 510–514. [Google Scholar] [PubMed]
- Xie, X.; Bärenholdt, O. Bone density and geometric properties of the distal radius in displaced and undisplaced Colles’ fractures: Quantitative CT in 70 women. Acta Orthop. Scand. 2001, 72, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Stuart, P.R.; Berger, R.A.; Linscheid, R.L.; An, K.N. The dorsopalmar stability of the distal radioulnar joint. J. Hand Surg. Am. 2000, 25, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Moritomo, H.; Masatomi, T.; Murase, T.; Miyake, J.; Okada, K.; Yoshikawa, H. Open repair of foveal avulsion of the triangular fibrocartilage complex and comparison by types of injury mechanism. J. Hand Surg. Am. 2010, 35, 1955–1963. [Google Scholar] [CrossRef] [PubMed]
- Skalski, M.R.; White, E.A.; Patel, D.B.; Schein, A.J.; RiveraMelo, H.; Matcuk, G.R., Jr. The Traumatized TFCC: An Illustrated Review of the Anatomy and Injury Patterns of the Triangular Fibrocartilage Complex. Curr. Probl. Diagn. Radiol. 2016, 45, 39–50. [Google Scholar] [CrossRef]
- Potter, H.G.; Asnis-Ernberg, L.; Weiland, A.J.; Hotchkiss, R.N.; Peterson, M.G.; McCormack, R.R., Jr. The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J. Bone Jt. Surg. Am. 1997, 79, 1675–1684. [Google Scholar] [CrossRef]
- Blazar, P.E.; Chan, P.S.; Kneeland, J.B.; Leatherwood, D.; Bozentka, D.J.; Kowalchick, R. The effect of observer experience on magnetic resonance imaging interpretation and localization of triangular fibrocartilage complex lesions. J. Hand Surg. Am. 2001, 26, 742–748. [Google Scholar] [CrossRef]
- Spence, L.D.; Savenor, A.; Nwachuku, I.; Tilsley, J.; Eustace, S. MRI of fractures of the distal radius: Comparison with conventional radiographs. Skelet. Radiol. 1998, 27, 244–249. [Google Scholar] [CrossRef]
- Ryoo, H.J.; Kim, Y.B.; Kwak, D.; Choi, I.C.; Park, J.W. Ulnar positive variance associated with TFCC foveal tear. Skelet. Radiol. 2023, 52, 1485–1491. [Google Scholar] [CrossRef]
- Schierenbeck, M.; Grozinger, M.; Reichardt, B.; Jansen, O.; Kauczor, H.U.; Campbell, G.M.; Sedaghat, S. Detecting Bone Marrow Edema of the Extremities on Spectral Computed Tomography Using a Three-Material Decomposition. Diagnostics 2023, 13, 2745. [Google Scholar] [CrossRef]
- Kim, B.S.; Cho, C.H.; Lee, K.J.; Lee, S.W.; Byun, S.H. Pathomechanism of Triangular Fibrocartilage Complex Injuries in Patients with Distal-Radius Fractures: A Magnetic-Resonance Imaging Study. J. Clin. Med. 2022, 11, 6168. [Google Scholar] [CrossRef] [PubMed]
- von Borstel, D.; Wang, M.; Small, K.; Nozaki, T.; Yoshioka, H. High-Resolution 3T MR Imaging of the Triangular Fibrocartilage Complex. Magn. Reson. Med. Sci. 2017, 16, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Im, J.; Kang, S.J.; Lee, S.J. A Comparative Study between Conservative and Surgical Treatments of Triangular Fibrocartilage Complex Injury of the Wrist with Distal Radius Fractures. Clin. Orthop. Surg. 2021, 13, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Nishiwaki, M.; Welsh, M.F.; Gammon, B.; Ferreira, L.M.; Johnson, J.A.; King, G.J. Effect of Volarly Angulated Distal Radius Fractures on Forearm Rotation and Distal Radioulnar Joint Kinematics. J. Hand Surg. Am. 2015, 40, 2236–2242. [Google Scholar] [CrossRef] [PubMed]
- Nishiwaki, M.; Welsh, M.; Gammon, B.; Ferreira, L.M.; Johnson, J.A.; King, G.J. Distal radioulnar joint kinematics in simulated dorsally angulated distal radius fractures. J. Hand Surg. Am. 2014, 39, 656–663. [Google Scholar] [CrossRef] [PubMed]
- Scheer, J.H.; Adolfsson, L.E. Patterns of triangular fibrocartilage complex (TFCC) injury associated with severely dorsally displaced extra-articular distal radius fractures. Injury 2012, 43, 926–932. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.K.; Park, J.K.; Choi, S.M. Reattachment using the suture bridge augmentation for Achilles tendon avulsion fracture with osteoporotic bony fragment. Foot 2017, 31, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Rauer, T.; Twerenbold, R.; Flückiger, R.; Neuhaus, V. Avulsion Fracture of the Calcaneal Tuberosity: Case Report and Literature Review. J. Foot Ankle Surg. 2018, 57, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Abe, S.; Kashii, M.; Shimada, T.; Suzuki, K.; Nishimoto, S.; Nakagawa, R.; Horiki, M.; Yasui, Y.; Namba, J.; Kuriyama, K. Relationship between distal radius fracture severity and 25-hydroxyvitamin-D level among perimenopausal and postmenopausal women. Bone Jt. Open 2022, 3, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Bendre, H.H.; Oflazoglu, K.; van Leeuwen, W.F.; Rakhorst, H.; Ring, D.; Chen, N.C. The Prevalence of Triangular Fibrocartilage Complex Signal Abnormalities on Magnetic Resonance Imaging Relative to Clinical Suspicion of Pathology. J. Hand Surg. Am. 2018, 43, 819–826.e1. [Google Scholar] [CrossRef]

| Group I (n = 35) | Group II (n = 40) | p Value | |
|---|---|---|---|
| Age (years) * | 69.1 ± 9.0 | 59.0 ± 5.3 | <0.001 |
| Sex * | |||
| Male (%) | 4 (11.4) | 16 (40.0) | 0.005 |
| Female (%) | 31 (88.6) | 24 (60.0) | |
| BMI (kg/m2) | 24.4 ± 3.6 | 25.6 ± 4.2 | 0.185 |
| Involvement of dominant side (%) | 13 (37.1) | 18 (45.0) | 0.423 |
| Low energy trauma (%) * | 22 (55.0) | 27 (77.1) | 0.044 |
| Radial inclination (°) * | 13.7 ± 5.4 | 17.9 ± 4.2 | <0.001 |
| Dorsal angulation (°) * | 22.2 ± 12.1 | 16.5 ± 9.4 | 0.024 |
| Ulnar variance (mm) * | 4.15 ± 2.1 | 2.2 ± 1.9 | <0.001 |
| TFCC foveal tear (%) * | 17 (48.6) | 13 (32.5) | 0.156 |
| Group I (n = 35) | Group II (n = 40) | |
|---|---|---|
| AO/OTA classification | ||
| A2 | 1 (2.9) | 1 (2.5) |
| A3 | 8 (22.9) | 13 (32.5) |
| C1 | 2 (5.7) | 2 (5.0) |
| C2 | 20 (57.1) | 18 (45.0) |
| C3 | 4 (11.4) | 6 (15.0) |
| Ulnar styloid fracture location | ||
| None | 13 (37.1) | 16 (40.0) |
| Tip | 7 (20.0) | 7 (17.5) |
| Base | 15 (42.9) | 17 (42.5) |
| Factors | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Sex | 1.34 | 0.02–7.35 | 0.887 | |||
| Age | 1.10 | 0.82–1.48 | 0.524 | |||
| Involvement of the dominant side | 2.89 | 0.08–10.32 | 0.175 | |||
| BMI | 0.55 | 0.24–1.23 | 0.145 | |||
| Osteoporosis | 0.01 | 0.00–2.31 | 0.133 | |||
| Low energy trauma | 0.02 | 0.00–6.53 | 0.182 | |||
| Intra-articular involvement of fracture | 0.18 | 0.00–58.52 | 0.565 | |||
| Ulnar styloid base fracture | 1.68 | 0.04–74.31 | 0.790 | |||
| Radial inclination | 1.09 | 0.69–1.73 | 0.705 | |||
| Dorsal angulation | 1.63 | 0.97–2.75 | 0.067 | 1.26 | 1.05–1.50 | 0.011 |
| Ulnar variance | 9.81 | 1.48–64.92 | 0.038 | 39.91 | 3.88–410.60 | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-W.; Kim, K.-T.; Lee, S.; Yoon, J.-H.; Kim, J.-Y. Fracture Severity and Triangular Fibrocartilage Complex Injury in Distal Radius Fractures with or without Osteoporosis. J. Clin. Med. 2024, 13, 992. https://doi.org/10.3390/jcm13040992
Lee H-W, Kim K-T, Lee S, Yoon J-H, Kim J-Y. Fracture Severity and Triangular Fibrocartilage Complex Injury in Distal Radius Fractures with or without Osteoporosis. Journal of Clinical Medicine. 2024; 13(4):992. https://doi.org/10.3390/jcm13040992
Chicago/Turabian StyleLee, Ho-Won, Ki-Tae Kim, Sanghyeon Lee, Joon-Hyeok Yoon, and Jung-Youn Kim. 2024. "Fracture Severity and Triangular Fibrocartilage Complex Injury in Distal Radius Fractures with or without Osteoporosis" Journal of Clinical Medicine 13, no. 4: 992. https://doi.org/10.3390/jcm13040992
APA StyleLee, H.-W., Kim, K.-T., Lee, S., Yoon, J.-H., & Kim, J.-Y. (2024). Fracture Severity and Triangular Fibrocartilage Complex Injury in Distal Radius Fractures with or without Osteoporosis. Journal of Clinical Medicine, 13(4), 992. https://doi.org/10.3390/jcm13040992






