Right Anterior versus Right Transaxillary Access for Minimally Invasive Aortic Valve Replacement: A Propensity Matched Competitive Analysis
Abstract
:1. Introduction
2. Materials and Methods
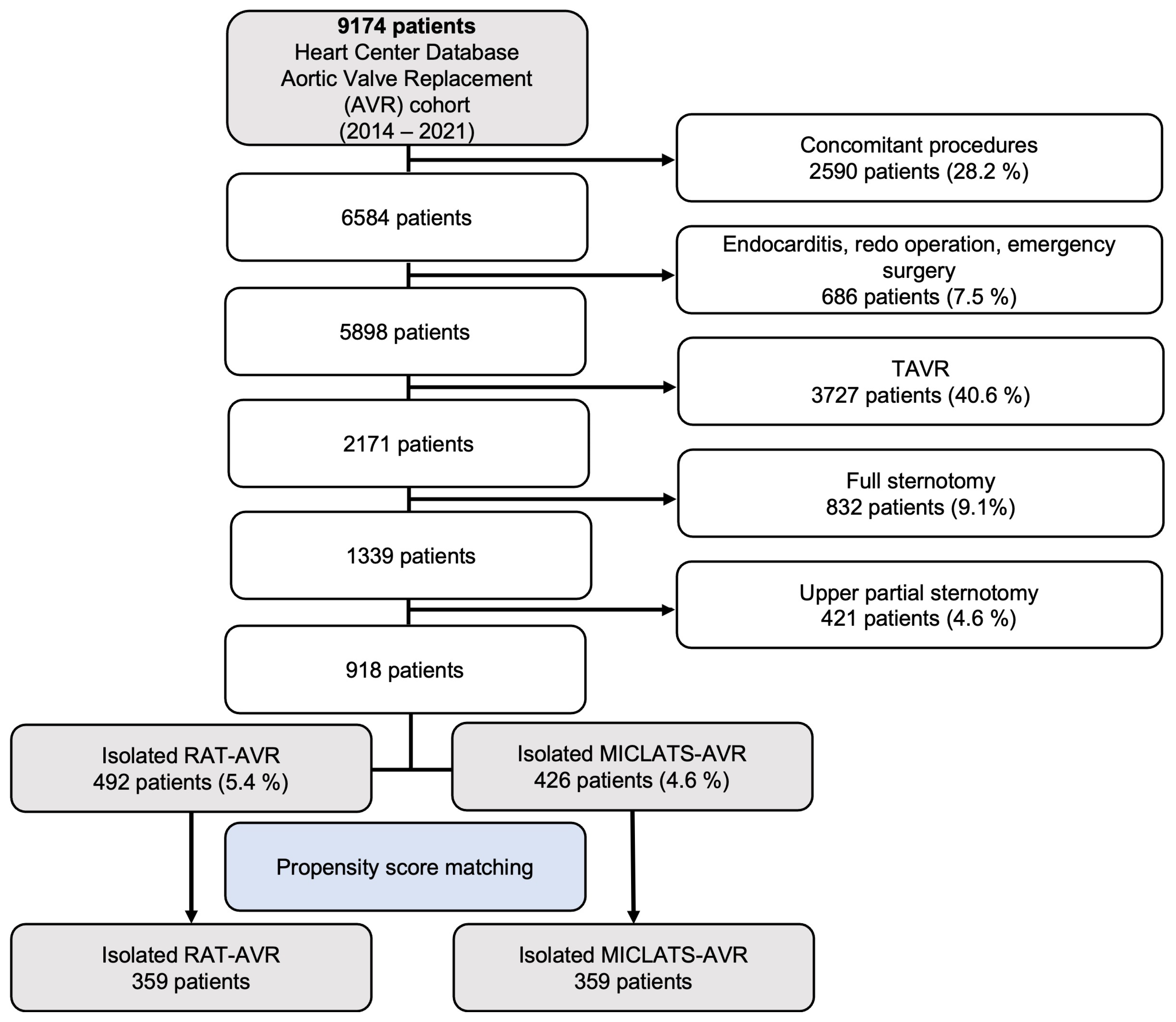
2.1. Inclusion and Exclusion Criteria
2.2. Study Design and Ethical Statement
2.3. Patient Population
2.4. Involved Surgeons
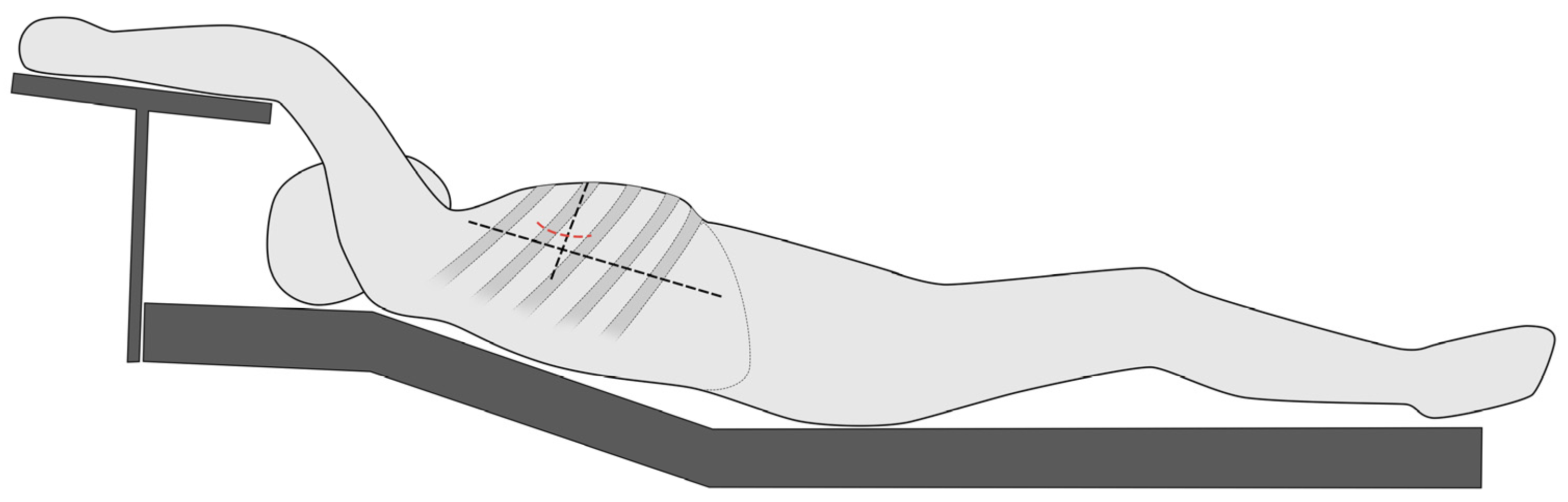
2.5. Sternum-Sparing MICS-AVR Access Routes
2.6. Prosthesis Choice
2.7. Statistical Analysis
3. Results
3.1. Patient Baseline Characteristics
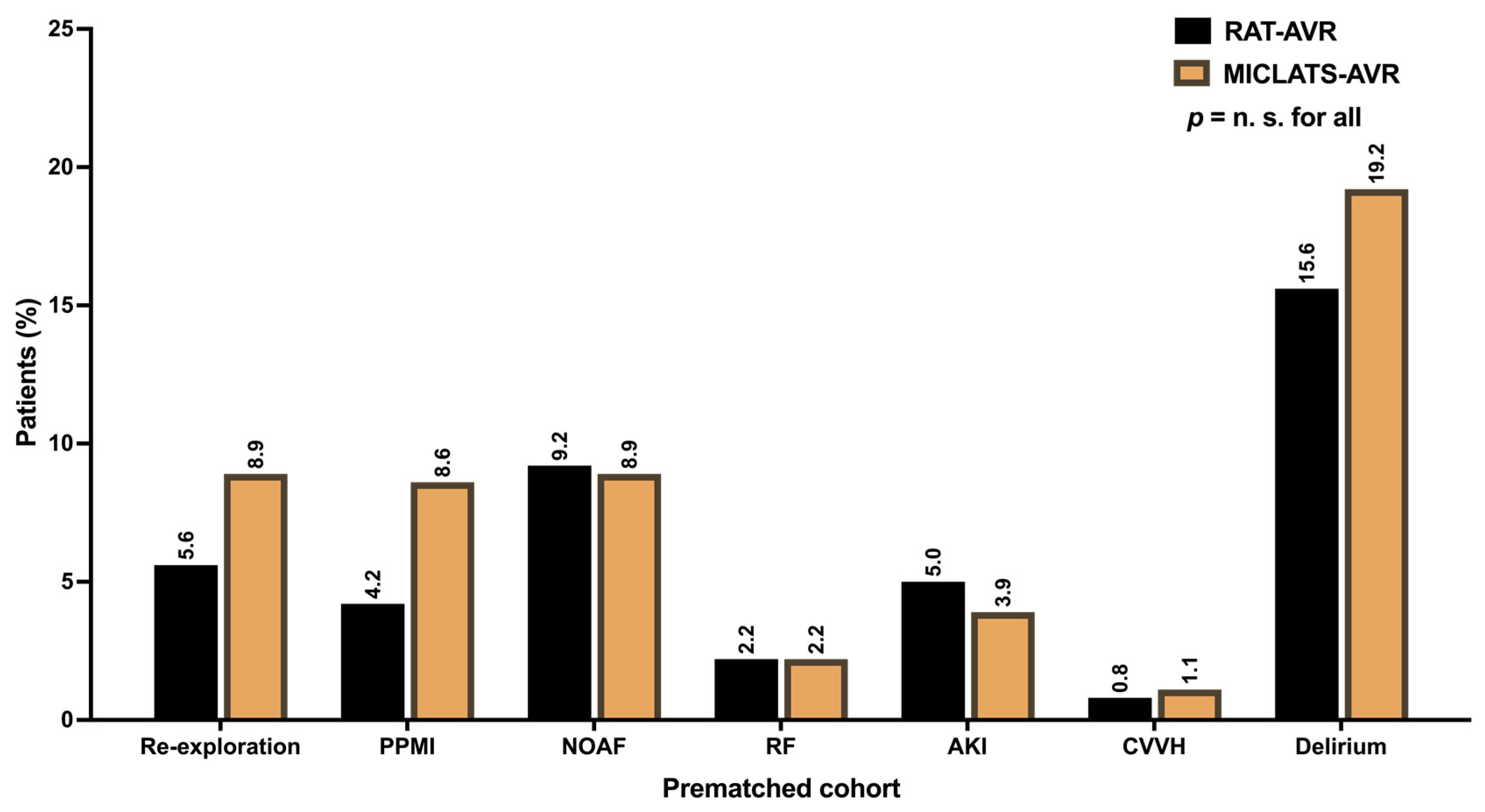
3.2. Unadjusted Outcomes
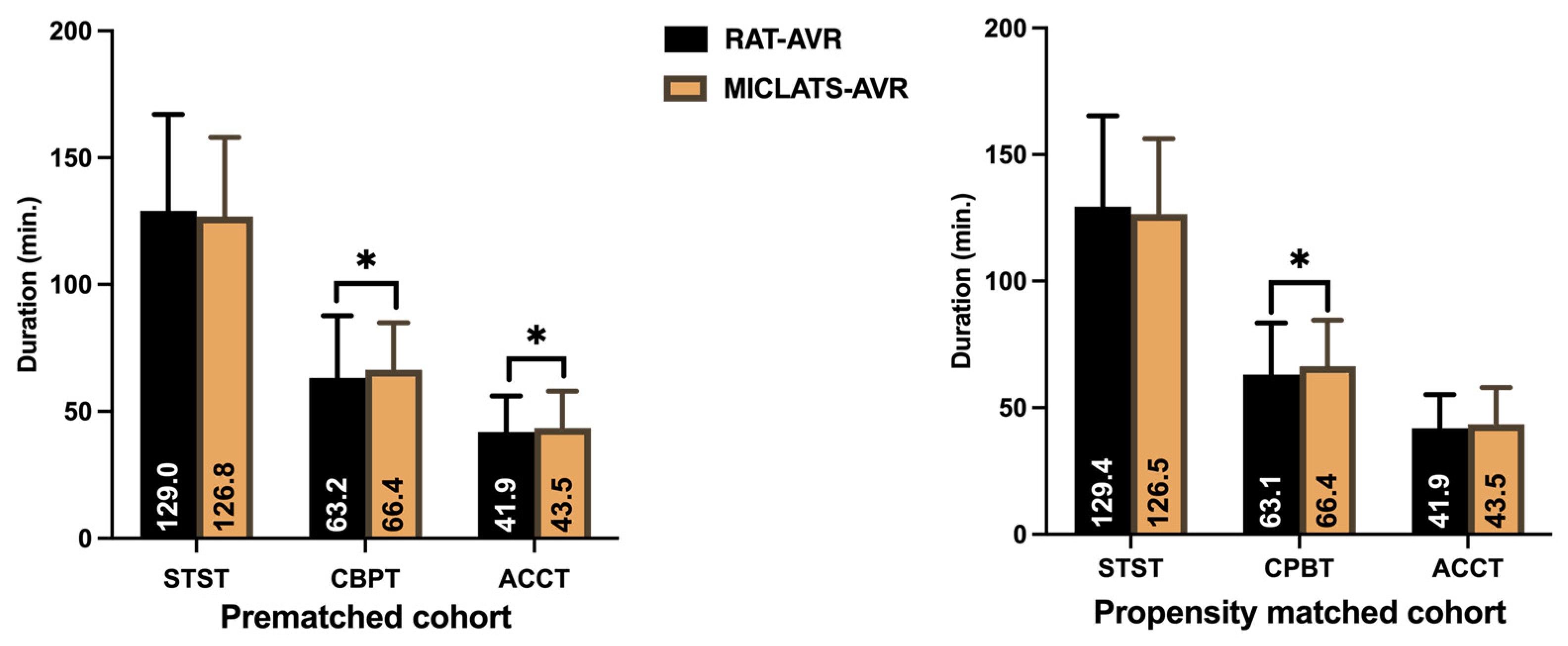
3.2.1. Procedural and Intraoperative Data
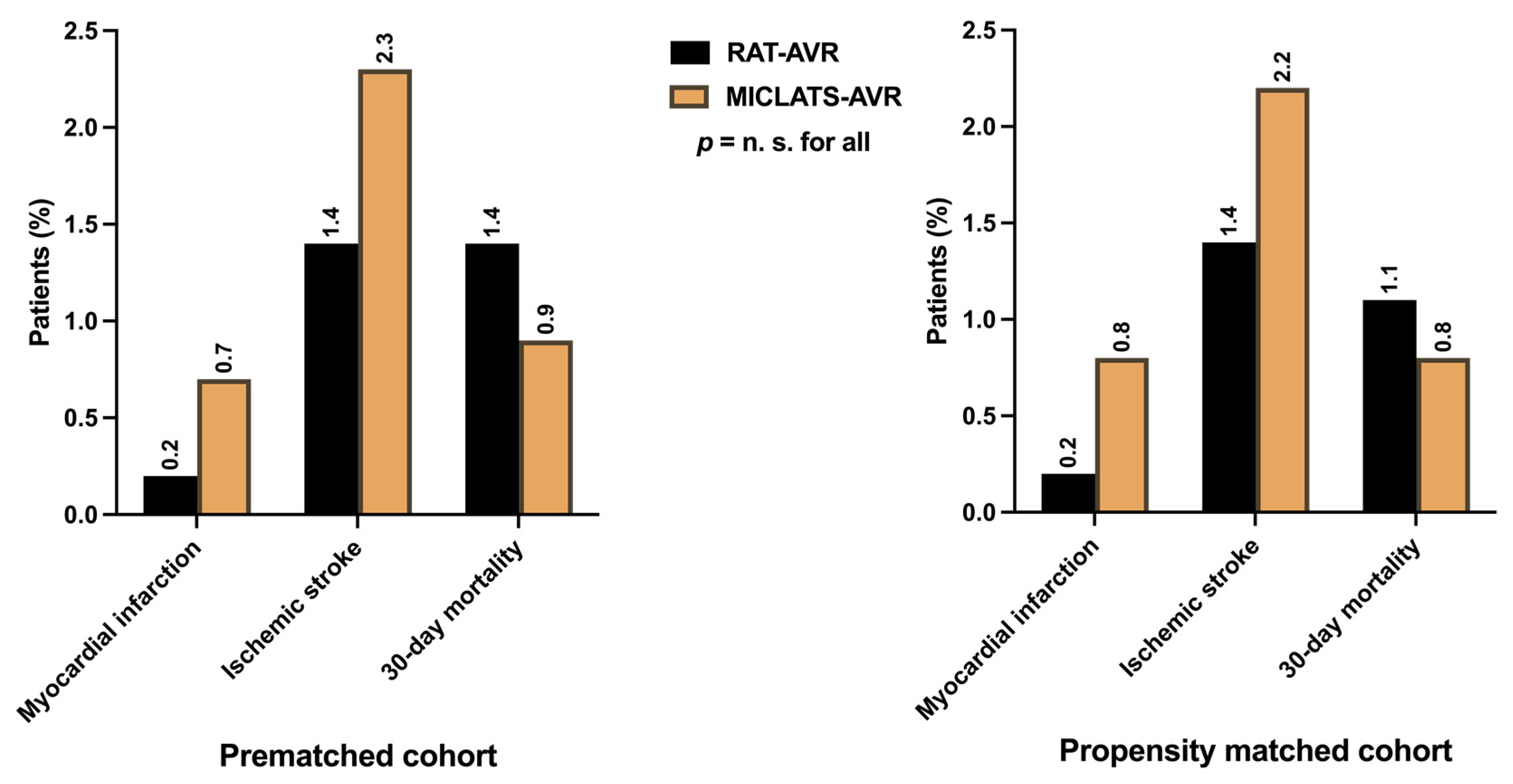
3.2.2. Postoperative Outcomes, Morbidity, and Mortality
3.3. Propensity Score–Matched Cohort
3.3.1. Adjusted Procedural and Intraoperative Data
3.3.2. Adjusted Postoperative Outcomes, Morbidity, and Mortality
4. Discussion
- −
- No significant differences were observed between the two groups in terms of MACCE.
- −
- The MICLATS-AVR group exhibited a shorter overall hospital stay.
- −
- Significantly lower rates of postoperative impaired wound healing were noted in the MICLATS-AVR group.
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mack, M.J.; Leon, M.B.; Smith, C.R.; Miller, D.C.; Moses, J.W.; Tuzcu, E.M.; Webb, J.G.; Douglas, P.S.; Anderson, W.N.; Blackstone, E.H.; et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (partner 1): A randomised controlled trial. Lancet 2015, 385, 2477–2484. [Google Scholar] [CrossRef] [PubMed]
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef] [PubMed]
- Reardon, M.J.; Van Mieghem, N.M.; Popma, J.J.; Kleiman, N.S.; Sondergaard, L.; Mumtaz, M.; Adams, D.H.; Deeb, G.M.; Maini, B.; Gada, H.; et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N. Engl. J. Med. 2017, 376, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- Forrest, J.K.; Deeb, G.M.; Yakubov, S.J.; Gada, H.; Mumtaz, M.A.; Ramlawi, B.; Bajwa, T.; Teirstein, P.S.; DeFrain, M.; Muppala, M.; et al. 3-Year outcomes after transcatheter or surgical aortic valve replacement in low-risk patients with aortic stenosis. J. Am. Coll. Cardiol. 2023, 81, 1663–1674. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Pibarot, P.; Hahn, R.T.; Genereux, P.; Kodali, S.K.; Kapadia, S.R.; Cohen, D.J.; Pocock, S.J.; et al. Transcatheter aortic-valve replacement in low-risk patients at five years. N. Engl. J. Med. 2023, 389, 1949–1960. [Google Scholar] [CrossRef]
- Rao, P.N.; Kumar, A.S. Aortic valve replacement through right thoracotomy. Tex. Heart Inst. J. 1993, 20, 307–308. [Google Scholar]
- Cosgrove, D.M., 3rd; Sabik, J.F. Minimally invasive approach for aortic valve operations. Ann. Thorac. Surg. 1996, 62, 596–597. [Google Scholar] [CrossRef]
- Beckmann, A.; Meyer, R.; Lewandowski, J.; Markewitz, A.; Blassfeld, D.; Boning, A. German heart surgery report 2021: The annual updated registry of the German society for thoracic and cardiovascular surgery. Thorac. Cardiovasc. Surg. 2022, 70, 362–376. [Google Scholar] [CrossRef]
- Wilbring, M.; Matschke, K.E.; Alexiou, K.; Di Eusanio, M.; Kappert, U. Surgery without scars: Right lateral access for minimally invasive aortic valve replacement. Thorac. Cardiovasc. Surg. 2021, 69, 461–465. [Google Scholar] [CrossRef]
- Wilbring, M.; Alexiou, K.; Schmidt, T.; Petrov, A.; Taghizadeh-Waghefi, A.; Charitos, E.; Matschke, K.; Arzt, S.; Kappert, U. Safety and efficacy of the transaxillary access for minimally invasive aortic valve surgery. Medicina 2023, 59, 160. [Google Scholar] [CrossRef] [PubMed]
- Wilbring, M.; Arzt, S.; Alexiou, K.; Matschke, K.; Kappert, U. Surgery without visible scars-double valve surgery using the right lateral access. Ann. Cardiothorac. Surg. 2020, 9, 424–426. [Google Scholar] [CrossRef]
- Coti, I.; Haberl, T.; Scherzer, S.; Werner, P.; Shabanian, S.; Kocher, A.; Laufer, G.; Andreas, M. Outcome of rapid deployment aortic valves: Long-term experience after 700 implants. Ann. Cardiothorac. Surg. 2020, 9, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.L.; Flynn, C.D.; Mamo, A.A.; Tian, D.H.; Kappert, U.; Wilbring, M.; Folliguet, T.; Fiore, A.; Miceli, A.; D’Onofrio, A.; et al. Long-term outcomes of sutureless and rapid-deployment aortic valve replacement: A systematic review and meta-analysis. Ann. Cardiothorac. Surg. 2020, 9, 265–279. [Google Scholar] [CrossRef] [PubMed]
- Pollari, F.; Mamdooh, H.; Hitzl, W.; Grossmann, I.; Vogt, F.; Fischlein, T. Ten years’ experience with the sutureless aortic valve replacement: Incidence and predictors for survival and valve durability at follow-up. Eur. J. Cardiothorac. Surg. 2023, 63, ezac572. [Google Scholar] [CrossRef] [PubMed]
- Glauber, M.; Miceli, A.; Gilmanov, D.; Ferrarini, M.; Bevilacqua, S.; Farneti, P.A.; Solinas, M. Right anterior minithoracotomy versus conventional aortic valve replacement: A propensity score matched study. J. Thorac. Cardiovasc. Surg. 2013, 145, 1222–1226. [Google Scholar] [CrossRef] [PubMed]
- Neely, R.C.; Boskovski, M.T.; Gosev, I.; Kaneko, T.; McGurk, S.; Leacche, M.; Cohn, L.H. Minimally invasive aortic valve replacement versus aortic valve replacement through full sternotomy: The Brigham and Women’s Hospital experience. Ann. Cardiothorac. Surg. 2015, 4, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Bowdish, M.E.; Hui, D.S.; Cleveland, J.D.; Mack, W.J.; Sinha, R.; Ranjan, R.; Cohen, R.G.; Baker, C.J.; Cunningham, M.J.; Barr, M.L.; et al. A comparison of aortic valve replacement via an anterior right minithoracotomy with standard sternotomy: A propensity score analysis of 492 patients. Eur. J. Cardiothorac. Surg. 2016, 49, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Gummert, J.F.; Funkat, A.; Beckmann, A.; Schiller, W.; Hekmat, K.; Ernst, M.; Haverich, A. Cardiac surgery in Germany during 2007: A report on behalf of the German society for thoracic and cardiovascular surgery. Thorac. Cardiovasc. Surg. 2008, 56, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Lamelas, J. Minimally invasive aortic valve replacement: The “Miami Method”. Ann. Cardiothorac. Surg. 2015, 4, 71–77. [Google Scholar] [CrossRef]
- Salenger, R.; Gammie, J.S.; Collins, J.A. Minimally Invasive Aortic Valve Replacement. J. Card. Surg. 2016, 31, 38–50. [Google Scholar] [CrossRef]
- Modi, P.; Chitwood, W.R., Jr. Retrograde femoral arterial perfusion and stroke risk during minimally invasive mitral valve surgery: Is there cause for concern? Ann. Cardiothorac. Surg. 2013, 2, E1. [Google Scholar] [CrossRef]
- Murzi, M.; Cerillo, A.G.; Miceli, A.; Bevilacqua, S.; Kallushi, E.; Farneti, P.; Solinas, M.; Glauber, M. Antegrade and retrograde arterial perfusion strategy in minimally invasive mitral-valve surgery: A propensity score analysis on 1280 patients. Eur. J. Cardiothorac. Surg. 2013, 43, e167–e172. [Google Scholar] [CrossRef]
- Bedeir, K.; Reardon, M.; Ramchandani, M.; Singh, K.; Ramlawi, B. Elevated Stroke Risk Associated With Femoral Artery Cannulation during mitral valve surgery. Semin. Thorac. Cardiovasc. Surg. 2015, 27, 97–103. [Google Scholar] [CrossRef]
- Murzi, M.; Cerillo, A.G.; Gasbarri, T.; Margaryan, R.; Kallushi, E.; Farneti, P.; Solinas, M. Antegrade and retrograde perfusion in minimally invasive mitral valve surgery with transthoracic aortic clamping: A single-institution experience with 1632 patients over 12 years. Interdiscip. Cardiovasc. Thorac. Surg. 2017, 24, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Kruse, J.; Silaschi, M.; Velten, M.; Wittmann, M.; Alaj, E.; Ahmad, A.E.; Zimmer, S.; Borger, M.A.; Bakhtiary, F. Femoral or axillary cannulation for extracorporeal circulation during minimally invasive heart valve surgery (FAMI): Protocol for a multi-center prospective randomized trial. J. Clin. Med. 2023, 12, 5344. [Google Scholar] [CrossRef] [PubMed]
- Tabata, M.; Umakanthan, R.; Cohn, L.H.; Bolman, R.M., 3rd; Shekar, P.S.; Chen, F.Y.; Couper, G.S.; Aranki, S.F. Early and late outcomes of 1000 minimally invasive aortic valve operations. Eur. J. Cardiothorac. Surg. 2008, 33, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Glower, D.D.; Desai, B.S.; Hughes, G.C.; Milano, C.A.; Gaca, J.G. Aortic valve replacement via right minithoracotomy versus median sternotomy: A propensity score analysis. Innovations 2014, 9, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Doll, N.; Borger, M.A.; Hain, J.; Bucerius, J.; Walther, T.; Gummert, J.F.; Mohr, F.W. Minimal access aortic valve replacement: Effects on morbidity and resource utilization. Ann. Thorac. Surg. 2002, 74, S1318–S1322. [Google Scholar] [CrossRef] [PubMed]
- Sansone, F.; Punta, G.; Parisi, F.; Dato, G.M.; Zingarelli, E.; Flocco, R.; Forsennati, P.G.; Bardi, G.L.; del Ponte, S.; Casabona, R. Right minithoracotomy versus full sternotomy for the aortic valve replacement: Preliminary results. Heart Lung Circ. 2012, 21, 169–173. [Google Scholar] [CrossRef]
- Taghizadeh-Waghefi, A.; Wilbring, M.; Arzt, S.; Petrov, A.; Alexiou, K.; Matschke, K.; Kappert, U. Die rechts-lateral transaxilläre thorakotomie für mehrfachklappeneingriffe. Z. Herz- Thorax- Gefäßchirurgie 2023, 37, 285–294. [Google Scholar] [CrossRef]

| Pre-Matched Cohort | Propensity Score-Matched Cohort | |||||
|---|---|---|---|---|---|---|
| RAT-AVR (n = 492) | MICLATS-AVR (n = 426) | p | RAT-AVR (n = 359) | MICLATS-AVR (n = 359) | p | |
| Age (years), mean ± SD | 68.0 ± 10.0 | 68.0 ± 8.5 | 0.191 | 67.5 ± 9.7 | 67.6 ± 8.8 | 0.715 |
| Sex (male), n (%) | 312 (63.4) | 264 (62.0) | 0.681 | 234 (65.2) | 228 (63.5) | 0.697 |
| Height (cm), mean ± SD | 170.7 ± 9.4 | 170.7 ± 9.3 | 0.872 | 171.4 ± 9.5 | 170.7 ± 9.3 | 0.300 |
| Weight (kg), mean ± SD | 78.4 ± 13.6 | 81.7 ± 15.3 | ≤0.001 ** | 80.5 ± 13.7 | 80.6 ± 14.5 | 0.721 |
| BMI (kg/m2), mean ± SD | 26.8 ± 3.9 | 28.0 ± 4.6 | ≤0.001 ** | 27.4 ± 4.0 | 27.6 ± 4.3 | 0.456 |
| Arterial hypertension, n (%) | 453 (92.1) | 380 (89.2) | 0.139 | 333 (92.8) | 320 (89.1) | 0.118 |
| Diabetes mellitus, n (%) | 132 (26.8) | 119 (27.9) | 0.711 | 86 (24.0) | 92 (25.6) | 0.666 |
| Dyslipidemia, n (%) | 260 (52.8) | 247 (58.0) | 0.126 | 201 (56.0) | 207 (57.7) | 0.706 |
| Coronary artery disease, n (%) | 131 (26.6) | 115 (27.0) | 0.940 | 100 (27.9) | 89 (24.8) | 0.383 |
| LVEF (%), mean ± SD | 57.8 ± 10.5 | 56.9 ± 11.0 | 0.314 | 55.6 ± 8.5 | 56.0 ± 9.3 | 0.989 |
| COPD, n (%) | 38 (7.7) | 30 (7.0) | 0.707 | 20 (5.6) | 26 (7.2) | 0.446 |
| Pulmonary arterial hypertension, n (%) | 69 (14.0) | 54 (12.7) | 0.562 | 69 (14.0) | 54 (12.7) | ≥0.999 |
| Renal insufficiency, n (%) | 75 (15.2) | 75 (17.6) | 0.371 | 49 (13.6) | 64 (17.8) | 0.151 |
| Hemodialysis, n (%) | 2 (0.4) | 3 (0.7) | 0.668 | 0 (0.0) | 3 (0.8) | 0.249 |
| CRCL (mL/min.), mean ± SD | 80.8 ± 25.8 | 84.1 ± 25.9 | 0.029 * | 84.0 ± 25.6 | 83.5 ± 25.6 | 0.917 |
| PAOD, n (%) | 15 (3.0) | 21 (4.9) | 0.173 | 14 (3.9) | 13 (3.6) | ≥0.999 |
| Carotid artery stenosis > 50%, n (%) | 19 (3.9) | 17 (4.0) | ≥0.999 | 15 (4,2) | 11 (3.1) | 0.55 |
| TIA, n (%) | 14 (2.8) | 5 (1.2) | ≥0.999 | 12 (3.3) | 5 (1.4) | 0.139 |
| Ischemic stroke, n (%) | 20 (4.0) | 21 (5.9) | 0.543 | 13 (3.6) | 15 (4.1) | 0.714 |
| Pacemaker, n (%) | 13 (2.6) | 17 (4.0) | 0.269 | 6 (1.7) | 10 (2.8) | 0.449 |
| Smoker status, n (%) | 51 (10.4) | 50 (11.7) | 0.527 | 36 (10.0) | 47 (13.1) | 0.243 |
| NYHA class III or IV, n (%) | 259 (52.6) | 280 (65.7) | ≤0.001 ** | 220 (61.3) | 223 (62.1) | 0.803 |
| EuroSCORE II (%), mean ± SD | 1.6 ± 1.0 | 1.6 ± 1.1 | 0.764 | 1.6 ± 1.0 | 1.6 ± 1.1 | 0.632 |
| STS-PROM Score, mean ± SD | 1.4 ± 0.8 | 1.2 ± 0.7 | ≤0.001 ** | 1.2 ± 0.6 | 1.2 ± 0.7 | 0.125 |
| Pre-Matched Cohort | Propensity-Score-Matched Cohort | |||||
|---|---|---|---|---|---|---|
| RAT-AVR (n = 492) | MICLATS-AVR (n = 426) | p | RAT-AVR (n = 359) | MICLATS-AVR (n = 359) | p | |
| Prosthesis size (mm), mean ± SD | 24.0 ± 1.9 | 24.2 ± 2.1 | 0.044 * | 24.1 ± 1.9 | 24.2 ± 2.1 | 0.200 |
| STST (min.), mean ± SD | 129.0 ± 38.1 | 126.8 ± 31.2 | 0.845 | 129.4 ± 35.9 | 126.5 ± 29.8 | 0.790 |
| CPBT (min.), mean ± SD | 63.2 ± 24.5 | 66.4 ± 18.5 | ≤0.001 ** | 63.1 ± 20.4 | 66.4 ± 18.2 | ≤0.001 ** |
| ACCT (min.), mean ± SD | 41.9 ± 14.2 | 43.5 ± 14.4 | 0.044 * | 41.9 ± 13.3 | 43.5 ± 14.4 | 0.182 |
| Prosthesis type | ||||||
| − Mechanical, n (%) | 41 (8.4) | 20 (4.7) | 31 (8.7) | 19 (5.3) | ||
| − Bioprosthetic, n (%) | 190 (38.7) | 57 (13.4) | ≤0.001 ** | 135 (37.7) | 48 (13.4) | ≤0.001 ** |
| − RDV, n (%) | 260 (53.0) | 349 (81.9) | 192 (53.6) | 292 (81.3) | ||
| Pre-Matched Cohort | Propensity-Score-Matched Cohort | |||||
|---|---|---|---|---|---|---|
| RAT-AVR (n = 492) | MICLATS-AVR (n = 426) | p | RAT-AVR (n = 359) | MICLATS-AVR (n = 359) | p | |
Ventilation time (hours)
| 447 (91.2) 31 (6.3) 12 (2.4) | 382 (89.7) 32 (7.5) 12 (2.8) | 0.426 | 326 (91.1) 21 (5.9) 11 (3.1) | 321 (89.4) 29 (8.1) 9 (2.5) | 0.487 |
| Respiratory failure †, n (%) | 9 (1.8) | 11 (2.6) | 0.501 | 8 (2.2) | 8 (2.2) | ≥0.999 |
| ICU stay (days), mean ± SD | 1.9 ± 2.3 | 2.0 ± 3.2 | 0.833 | 1.9 ± 2.5 | 2.0 ± 2.7 | 0.465 |
| Hospital stay (days), mean ± SD | 9.7 ± 5.0 | 9.3 ± 5.0 | 0.003 ** | 9.7 ± 5.2 | 9.2 ± 4.5 | 0.01 * |
| Transfusion of PRBC, mean ± SD | 0.6 ± 2.6 | 0.6 ± 1.6 | 0.358 | 0.6 ± 2.9 | 0.5 ± 1.4 | 0.067 |
| AKI, n (%) | 31 (6.3) | 17 (4.0) | 0.137 | 18 (5.0) | 14 (3.9) | 0.476 |
| AKI grade II or III, n (%) | 26 (5.3) | 17 (4.0) | 0.434 | 17 (4.7) | 14 (3.9) | 0.588 |
| CVVH, n (%) | 5 (1.0) | 6 (1.4) | 0.763 | 3 (0.8) | 4 (1.1) | ≥0.999 |
| Conversion to sternotomy, n (%) | 18 (3.7) | 7 (1.6) | 0.069 | 14 (3.9) | 6 (1.7) | 0.110 |
| Re-exploration, n (%) | 27 (5.5) | 39 (9.2) | 0.040 * | 20 (5.6) | 32 (8.9) | 0.112 |
| Impaired wound healing, n (%) | 54 (11.0) | 22 (5.2) | 0.002 ** | 42 (11.7) | 14 (3.9) | <0.001 ** |
| Postoperative delirium, n (%) | 76 (15.5) | 77 (18.1) | 0.329 | 56 (15.6) | 69 (19.2) | 0.238 |
| Ischemic stroke, n (%) any Rankin > 2 | 7 (1.4) 3 (0.6) | 10 (2.3) 4 (0.9) | 0.335 0.824 | 5 (1.4) 3 (0.8) | 8 (2.2) 3 (0.8) | 0.578 ≥0.999 |
| TIA, n (%) | 4 (0.8) | 1 (0.2) | 0.38 | 3 (0.8) | 1 (0.3) | 0.373 |
| PPM implantation, n (%) | 23 (4.7) | 34 (8.0) | 0.126 | 15 (4.2) | 31 (8.6) | 0.058 |
| NOAF, n (%) | 49 (10.0) | 41 (9.6) | 0.921 | 33 (9.2) | 32 (8.9) | 0.897 |
| Myocardial infarction, n (%) | 1 (0.2) | 3 (0.7) | 0.343 | 1 (0.3) | 3 (0.8) | 0.624 |
| 30-day mortality, n (%) | 7 (1.4) | 4 (0.9) | 0.558 | 4 (1.1) | 3 (0.8) | ≥0.999 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taghizadeh-Waghefi, A.; Arzt, S.; Wenzel, L.; Petrov, A.; Wilbring, M.; Matschke, K.; Kappert, U.; Alexiou, K. Right Anterior versus Right Transaxillary Access for Minimally Invasive Aortic Valve Replacement: A Propensity Matched Competitive Analysis. J. Clin. Med. 2024, 13, 985. https://doi.org/10.3390/jcm13040985
Taghizadeh-Waghefi A, Arzt S, Wenzel L, Petrov A, Wilbring M, Matschke K, Kappert U, Alexiou K. Right Anterior versus Right Transaxillary Access for Minimally Invasive Aortic Valve Replacement: A Propensity Matched Competitive Analysis. Journal of Clinical Medicine. 2024; 13(4):985. https://doi.org/10.3390/jcm13040985
Chicago/Turabian StyleTaghizadeh-Waghefi, Ali, Sebastian Arzt, Lisa Wenzel, Asen Petrov, Manuel Wilbring, Klaus Matschke, Utz Kappert, and Konstantin Alexiou. 2024. "Right Anterior versus Right Transaxillary Access for Minimally Invasive Aortic Valve Replacement: A Propensity Matched Competitive Analysis" Journal of Clinical Medicine 13, no. 4: 985. https://doi.org/10.3390/jcm13040985
APA StyleTaghizadeh-Waghefi, A., Arzt, S., Wenzel, L., Petrov, A., Wilbring, M., Matschke, K., Kappert, U., & Alexiou, K. (2024). Right Anterior versus Right Transaxillary Access for Minimally Invasive Aortic Valve Replacement: A Propensity Matched Competitive Analysis. Journal of Clinical Medicine, 13(4), 985. https://doi.org/10.3390/jcm13040985






