Preeclampsia Management and Maternal Ophthalmic Artery Doppler Measurements between 19 and 23 Weeks of Gestation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
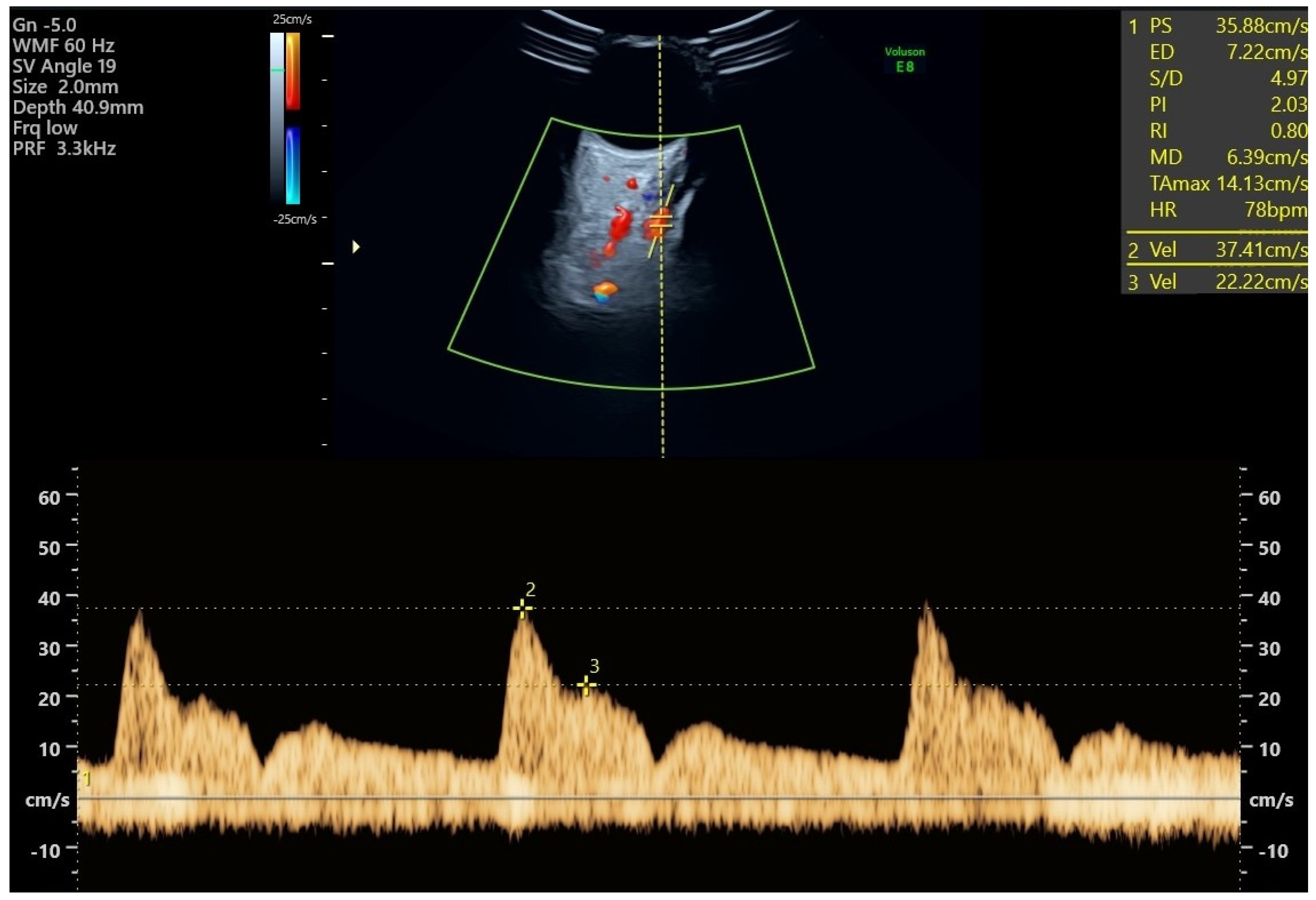
2.2. Doppler Measurements of the Ophthalmic Arteries
2.3. Outcome Measures
2.4. Ethical Considerations
2.5. Data Analysis
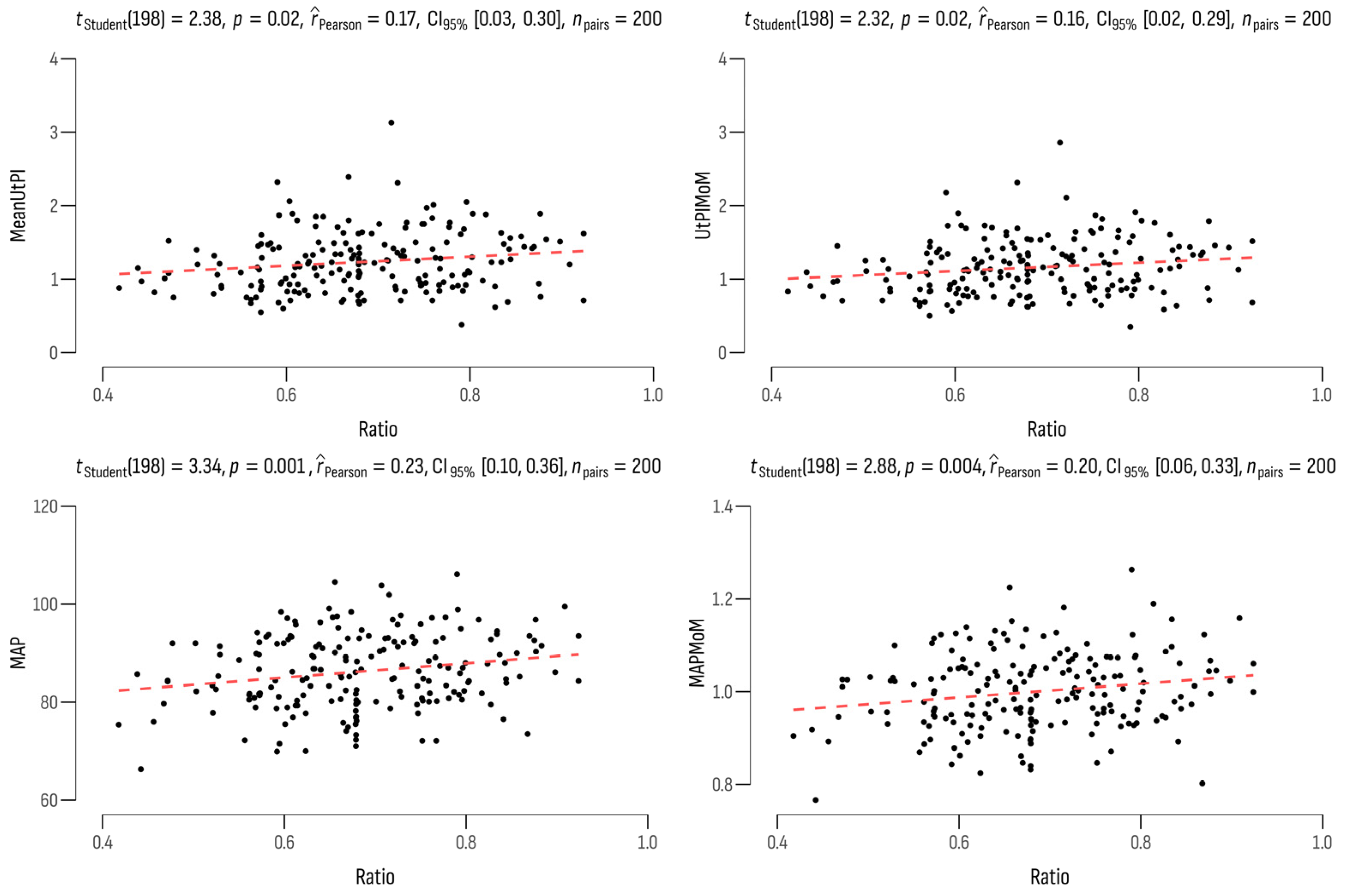
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brown, M.A.; Lindheimer, M.D.; de Swiet, M.; Assche, A.V.; Moutquin, J.-M. The Classification and Diagnosis of the Hypertensive Disorders of Pregnancy: Statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens. Pregnancy 2001, 20, ix–xiv. [Google Scholar] [CrossRef]
- Brown, M.A.; Magee, L.A.; Kenny, L.C.; Karumanchi, S.A.; McCarthy, F.P.; Saito, S.; Hall, D.R.; Warren, C.E.; Adoyi, G.; Ishaku, S. The Hypertensive Disorders of Pregnancy: ISSHP Classification, Diagnosis & Management Recommendations for International Practice. Pregnancy Hypertens. 2018, 13, 291–310. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.-J.; Seow, K.-M.; Chen, K.-H. Preeclampsia: Recent Advances in Predicting, Preventing, and Managing the Maternal and Fetal Life-Threatening Condition. Int. J. Environ. Res. Public Health 2023, 20, 2994. [Google Scholar] [CrossRef] [PubMed]
- Say, L.; Chou, D.; Gemmill, A.; Tunçalp, Ö.; Moller, A.-B.; Daniels, J.; Gülmezoglu, A.M.; Temmerman, M.; Alkema, L. Global Causes of Maternal Death: A WHO Systematic Analysis. Lancet Glob. Health 2014, 2, e323–e333. [Google Scholar] [CrossRef] [PubMed]
- Adekanmi, A.; Olatunji, R.; Obajimi, M.; Roberts, O.; Ojo, T. Maternal Ophthalmic Artery Doppler Velocimetry in Pre-Eclampsia in Southwestern Nigeria. Int. J. Women’s Health 2015, 7, 723–734. [Google Scholar] [CrossRef]
- Gonser, M.; Vonzun, L.; Ochsenbein-Kölble, N. Ophthalmic Artery Doppler as a Marker of Pre-eclampsia: Why Does It Work? BJOG Int. J. Obstet. Gynaecol. 2022, 130, 120–121. [Google Scholar] [CrossRef] [PubMed]
- Kane, S.C.; Brennecke, S.P.; da Silva Costa, F. Ophthalmic Artery Doppler Analysis: A Window into the Cerebrovasculature of Women with Pre-eclampsia. Ultrasound Obstet. Gynecol. 2016, 49, 15–21. [Google Scholar] [CrossRef]
- Gonser, M.; Vonzun, L.; Ochsenbein-Kölble, N. Ophthalmic Artery Doppler in Prediction of Pre-eclampsia: Insights from Hemodynamic Considerations. Ultrasound Obstet. Gynecol. 2021, 58, 145–147. [Google Scholar] [CrossRef]
- Mackensen, F.; Paulus, W.E.; Max, R.; Ness, T. Ocular Changes During Pregnancy. Dtsch. Aerzteblatt Online 2014, 111, 567–576. [Google Scholar] [CrossRef]
- Sharudin, S.N.; Saaid, R.; Samsudin, A.; Mohamad, N.F. Subfoveal Choroidal Thickness in Pre-Eclampsia. Optom. Vis. Sci. 2020, 97, 81–85. [Google Scholar] [CrossRef]
- Abu Samra, K. The Eye and Visual System in the Preeclampsia/Eclampsia Syndrome: What to Expect? Saudi J. Ophthalmol. 2013, 27, 51–53. [Google Scholar] [CrossRef]
- Diniz, A.L.D.; Paes, M.M.B.M. Ophthalmic Artery Doppler in Hypertensive Pregnancies: Small Vessel, Many Possibilities. BJOG Int. J. Obstet. Gynaecol. 2022, 130, 118–119. [Google Scholar] [CrossRef] [PubMed]
- Matias, D.S.; Costa, R.F.; Matias, B.S.; Cláudio Lemos Correia, L. Doppler Velocimetry of the Orbital Vessels in Pregnancies Complicated by Preeclampsia. J. Clin. Ultrasound 2012, 40, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Hata, T.; Hata, K.; Moritake, K. Maternal Ophthalmic Artery Doppler Velocimetry in Normotensive Pregnancies and Pregnancies Complicated by Hypertensive Disorders. Am. J. Obstet. Gynecol. 1997, 177, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Prediction of the Risk for Preeclampsia 11 + 0 to 14 + 1 Weeks. Available online: https://fetalmedicine.org/research/assess/preeclampsia/first-trimester (accessed on 14 December 2023).
- Vlachopoulos, C.; O’Rourke, M.; Nichols, W.W. McDonald’s Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles, 6th ed.; CRC Press: Boca Raton, FL, USA, 2011. [Google Scholar]
- Sapantzoglou, I.; Wright, A.; Arozena, M.G.; Campos, R.V.; Charakida, M.; Nicolaides, K.H. Ophthalmic Artery Doppler in Combination with Other Biomarkers in Prediction of Pre-eclampsia at 19–23 Weeks’ Gestation. Ultrasound Obstet. Gynecol. 2020, 57, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Sarno, M.; Wright, A.; Vieira, N.; Sapantzoglou, I.; Charakida, M.; Nicolaides, K.H. Ophthalmic Artery Doppler in Prediction of Pre-eclampsia at 35–37 Weeks’ Gestation. Ultrasound Obstet. Gynecol. 2020, 56, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Selima, E.R.; Abar, A.M.; Dessouky, B.A.E. Role of Ophthalmic Artery Doppler in Prediction of Preeclampsia. Egypt. J. Hosp. Med. 2022, 87, 1944–1952. [Google Scholar] [CrossRef]
- Dimitrova, V.; Stratieva, V. Recommendations of the Bulgarian Society of Obstetrics and Gynecology for Preeclampsia; Cochrane Library: Hoboken, NJ, USA, 2011. [Google Scholar]
- Litwinska, M.; Syngelaki, A.; Wright, A.; Wright, D.; Nicolaides, K.H. Management of Pregnancies after Combined Screening for Pre-eclampsia at 19–24 Weeks’ Gestation. Ultrasound Obstet. Gynecol. 2018, 52, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Mynard, J.P.; Kowalski, R.; Cheung, M.M.H.; Smolich, J.J. Beyond the Aorta: Partial Transmission of Reflected Waves from Aortic Coarctation into Supra-Aortic Branches Modulates Cerebral Hemodynamics and Left Ventricular Load. Biomechan. Model. Mechanobiol. 2016, 16, 635–650. [Google Scholar] [CrossRef]
- Mills, C.J.; Gabe, I.T.; Gault, J.H.; Mason, D.T.; Ross, J.; Braunwald, E.; Shillingford, J.P. Pressure-Flow Relationships and Vascular Impedance in Man. Cardiovasc. Res. 1970, 4, 405–417. [Google Scholar] [CrossRef]
- Erickson, S.J.; Hendrix, L.E.; Massaro, B.M.; Harris, G.J.; Lewandowski, M.F.; Foley, W.D.; Lawson, T.L. Color Doppler Flow Imaging of the Normal and Abnormal Orbit. Radiology 1989, 173, 511–516. [Google Scholar] [CrossRef]
- Nicolaides, K.H.; Sarno, M.; Wright, A. Ophthalmic Artery Doppler in the Prediction of Preeclampsia. Am. J. Obstet. Gynecol. 2021, 226, S1098–S1101. [Google Scholar] [CrossRef]
- Wright, D.; Syngelaki, A.; Akolekar, R.; Poon, L.C.; Nicolaides, K.H. Competing Risks Model in Screening for Preeclampsia by Maternal Characteristics and Medical History. Am. J. Obstet. Gynecol. 2015, 213, 62.e1–62.e10. [Google Scholar] [CrossRef] [PubMed]
- Aracil Moreno, I.; Rodríguez-Benitez, P.; Ruiz-Minaya, M.; Bernal Claverol, M.; Ortega Abad, V.; Hernández Martin, C.; Pintado Recarte, P.; Yllana, F.; Oliver-Barrecheguren, C.; Álvarez-Mon, M.; et al. Maternal Perinatal Characteristics in Patients with Severe Preeclampsia: A Case-Control Nested Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 11783. [Google Scholar] [CrossRef] [PubMed]
- Thomopoulos, C.; Salamalekis, G.; Kintis, K.; Andrianopoulou, I.; Michalopoulou, H.; Skalis, G.; Archontakis, S.; Argyri, O.; Tsioufis, C.; Makris, T.K.; et al. Risk of Hypertensive Disorders in Pregnancy Following Assisted Reproductive Technology: Overview and Meta-analysis. J. Clin. Hypertens. 2016, 19, 173–183. [Google Scholar] [CrossRef]
- Wright, A.; Wright, D.; Ispas, C.A.; Poon, L.C.; Nicolaides, K.H. Mean Arterial Pressure in the Three Trimesters of Pregnancy: Effects of Maternal Characteristics and Medical History. Ultrasound Obstet. Gynecol. 2015, 45, 698–706. [Google Scholar] [CrossRef]
- Tayyar, A.; Krithinakis, K.; Wright, A.; Wright, D.; Nicolaides, K.H. Mean Arterial Pressure at 12, 22, 32 and 36 Weeks’ Gestation in Screening for Pre-Eclampsia. Ultrasound Obstet. Gynecol. 2016, 47, 573–579. [Google Scholar] [CrossRef]
- Antwi, E.; Amoakoh-Coleman, M.; Vieira, D.L.; Madhavaram, S.; Koram, K.A.; Grobbee, D.E.; Agyepong, I.A.; Klipstein-Grobusch, K. Systematic Review of Prediction Models for Gestational Hypertension and Preeclampsia. PLOS ONE 2020, 15, e0230955. [Google Scholar] [CrossRef] [PubMed]
- Papageorghiou, A.T.; Yu, C.K.H.; Bindra, R.; Pandis, G.; Nicolaides, K.H. Multicenter Screening for Pre-eclampsia and Fetal Growth Restriction by Transvaginal Uterine Artery Doppler at 23 Weeks of Gestation. Ultrasound Obstet. Gynecol. 2001, 18, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Lees, C.; Parra, M.; Missfelder-Lobos, H.; Morgans, A.; Fletcher, O.; Nicolaides, K.H. Individualized Risk Assessment for Adverse Pregnancy Outcome by Uterine Artery Doppler at 23 Weeks. Obstet. Gynecol. 2001, 98, 369–373. [Google Scholar] [CrossRef]
- Stoilov, B.; Zaharieva-Dinkova, P.; Stoilova, L.; Uchikova, E.; Karaslavova, E. Independent Predictors of Preeclampsia and Their Impact on the Complication in Bulgarian Study Group of Pregnant Women. Folia Medica 2023, 65, 384–392. [Google Scholar] [CrossRef]
- Matias, D.S.; Costa, R.F.; Matias, B.S.; Gordiano, L.; Correia, L.C.L. Predictive Value of Ophthalmic Artery Doppler Velocimetry in Relation to Development of Pre-eclampsia. Ultrasound Obstet. Gynecol. 2014, 44, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Kumari, N.; Ranjan, R.K.; Rai, N.; Xalxo, A.R.; Toppo, S.K.; Ram, P.N. A Correlational Study of Ophthalmic Artery Doppler Parameters and Maternal Blood Pressure in Normotensive and Pre-Eclamptic Pregnancies at a Tertiary Care Hospital. Cureus 2023, 15, e40713. [Google Scholar] [CrossRef]
- Gao, J.; Shen, J.; Jiang, Y.; Zhou, X.; Qi, H.; Liu, X.; Liu, J.; Yang, J.; Bian, X. Value of second trimester maternal serum sFlt-1, PlGF and their ratio in the prediction of preeclampsia. Zhonghua Fu Chan Ke Za Zhi 2014, 49, 22–25. (In Chinese) [Google Scholar]
- UK National Screening Committee. Screening for Prediction and Prevention of Pre-Eclampsia; UK National Screening Committee: London, UK, 2022.
- Stratieva, V. Placental Dysfunction-Screening Model for Risk Assessment. Ph.D. Thesis, Medical University of Varna, Varna, Bulgaria, 2016. [Google Scholar]
- Poon, L.C.; Sahota, D. Screening and Prevention of Preeclampsia. Matern. Med. 2019, 1, 25–30. [Google Scholar] [CrossRef]
- August, P.; Jeyabalan, A. Preeclampsia: Prevention. Available online: https://www.uptodate.com/contents/preeclampsia-prevention?sectionName=LOW-DOSE%20ASPIRIN (accessed on 18 December 2023).
| Variables | Overall (n = 200) | High-Risk Women (n = 60) | Low-Risk Women (n = 140) | p |
|---|---|---|---|---|
| Age, years (mean ± SD) | 34.1 ± 5.0 | 35.4 ± 4.9 | 33.6 ± 4.9 | 0.020 |
| Age ≤ 35, % (n) | 66.0% (132) | 56.7% (34) | 70.0% (98) | 0.068 |
| Age > 35, % (n) | 34.0% (68) | 43.3% (26) | 30.0% (42) | |
| BMI, kg/m3 (mean ± SD) | 26.7 ± 5.3 | 27.5 ± 5.4 | 26.4 ± 5.3 | 0.184 |
| BMI ≤ 30 kg/m3 (n) | 78.5% (157) | 70% (42) | 82.1% (115) | 0.055 |
| BMI > 30 kg/m3 (n) | 21.5% (43) | 30% (18) | 17.9% (25) | |
| Conception method | ||||
| Spontaneous, % (n) | 90.5% (181) | 83.3% (50) | 93.6% (131) | 0.024 |
| IVF, % (n) | 9.5% (19) | 16.7% (10) | 6.4% (9) | |
| Smoking | ||||
| No, % (n) | 88.0% (176) | 95.0% (57) | 85.0% (119) | 0.046 |
| Yes, % (n) | 12.0% (24) | 5.0% (3) | 15.0% (21) | |
| GDM | ||||
| No, % (n) | 93.5% (187) | 98.3% (59) | 91.4% (128) | 0.070 |
| Yes, % (n) | 6.5% (13) | 1.7% (1) | 8.6% (12) | |
| Previous PE | ||||
| No, % (n) | 90.0% (180) | 93.3% (56) | 88.6% (124) | 0.304 |
| Yes, % (n) | 10.0% (20) | 6.7% (4) | 11.4% (16) | |
| Previous FGR | ||||
| No, % (n) | 96.0% (192) | 100% (60) | 94.3% (132) | 0.059 |
| Yes, % (n) | 4.0% (8) | 0% (0) | 5.7% (8) | |
| Women | ||||
| Multigravida, % (n) | 11.5% (23) | 6.7% (4) | 13.6% (19) | 0.161 |
| Nulligravida, % (n) | 88.5% (177) | 93.3% (56) | 86.4% (121) | |
| Acetylsalicylic acid | ||||
| No, % (n) | 91.0% (182) | 81.7% (49) | 95.0% (133) | 0.003 |
| Yes, % (n) | 9.0% (18) | 18.3% (11) | 5.0% (7) | |
| Interval last delivery ≥ 24 months (mean ± SD) | 3.7 ± 3.5 (23) | 3.2 ± 2.1 (4) | 3.8 ± 3.8 (19) | 0.743 |
| GA at time of delivery (mean ± SD) | 39.1 ± 2.0 | 38.6 ± 2.5 | 39.4 ± 1.6 | 0.010 |
| GA, at which PE was diagnosed (mean ± SD) | 36.2 ± 2.8 | 35.6 ± 3.0 | 37.1 ± 2.5 | 0.244 |
| Did not develop PE | 90.0% (180) | 81.7% (49) | 93.6% (131) | 0.010 |
| Developed PE | 10.0% (20) | 18.3% (11) | 6.4% (9) | |
| Clinical variables | ||||
| PSV2/PSV1 ratio (mean ± SD) | 0.68 ± 0.12 | 0.72 ± 0.09 | 0.65 ± 0.11 | 0.000 |
| Mean Ut PI (mean ± SD) | 1.23 ± 0.40 | 1.65 ± 0.34 | 1.05 ± 0.27 | 0.000 |
| Ut PI MoM (mean ± SD) | 1.15 ± 0.37 | 1.54 ± 0.32 | 0.99 ± 0.26 | 0.000 |
| MAP (mean ± SD) | 86.08 ± 7.55 | 91.56 ± 6.06 | 83.74 ± 6.90 | 0.000 |
| MAP MoM (mean ± SD) | 1.00 ± 0.08 | 1.05 ± 0.71 | 0.98 ± 0.08 | 0.000 |
| sFLT-1 MoM (mean ± SD) | 1.13 ± 0.81 | 1.05 ± 0.72 | 1.16 ± 0.85 | 0.382 |
| PlGF MoM (mean ± SD) | 1.12 ± 0.50 | 1.04 ± 0.59 | 1.16 ± 0.45 | 0.108 |
| sFLT-1/PlGF ratio (mean ± SD) | 1.38 ± 2.70 | 1.96 ± 4.73 | 1.13 ± 0.85 | 0.044 |
| Variables (% (n)) | Did Not Develop PE (n = 180) | Developed PE (n = 20) | χ2 | p |
|---|---|---|---|---|
| Previous PE | ||||
| No | 92.7% (162) | 75.5% (18) | - | - |
| Yes | 7.2% (18) | 25.0% (2) | ||
| Acetylsalicylic acid | ||||
| No | 92.7% (167) | 75.5% (15) | 6.95 | 0.008 |
| Yes | 7.2% (13) | 25.0% (5) | ||
| Variables (mean ± SD) | Did not develop PE | Developed PE | F | p |
| PSV2/PSV1 ratio | 0.67 ± 0.1 | 0.76 ± 0.1 | 12.07 | 0.001 |
| Mean Ut PI | 1.22 ± 0.4 | 1.29 ± 0.4 | 0.52 | 0.474 |
| Ut PI MoM | 1.15 ± 0.4 | 1.21 ± 0.4 | 0.48 | 0.492 |
| MAP | 85.26 ± 7.2 | 93.48 ± 6.3 | 23.74 | 0.000 |
| MAP MoM | 0.99 ± 0.1 | 1.07 ± 0.1 | 16.71 | 0.000 |
| sFLT-1 MoM | 1.16 ± 0.8 | 0.91 ± 0.6 | 1.71 | 0.193 |
| PlGFMoM | 1.14 ± 0.5 | 0.94 ± 0.4 | 2.94 | 0.088 |
| sFLT-1/PlGF ratio | 1.26 ± 1.6 | 2.46 ± 7.0 | 3.65 | 0.058 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gyokova, E.; Hristova-Atanasova, E.; Iskrov, G. Preeclampsia Management and Maternal Ophthalmic Artery Doppler Measurements between 19 and 23 Weeks of Gestation. J. Clin. Med. 2024, 13, 950. https://doi.org/10.3390/jcm13040950
Gyokova E, Hristova-Atanasova E, Iskrov G. Preeclampsia Management and Maternal Ophthalmic Artery Doppler Measurements between 19 and 23 Weeks of Gestation. Journal of Clinical Medicine. 2024; 13(4):950. https://doi.org/10.3390/jcm13040950
Chicago/Turabian StyleGyokova, Elitsa, Eleonora Hristova-Atanasova, and Georgi Iskrov. 2024. "Preeclampsia Management and Maternal Ophthalmic Artery Doppler Measurements between 19 and 23 Weeks of Gestation" Journal of Clinical Medicine 13, no. 4: 950. https://doi.org/10.3390/jcm13040950
APA StyleGyokova, E., Hristova-Atanasova, E., & Iskrov, G. (2024). Preeclampsia Management and Maternal Ophthalmic Artery Doppler Measurements between 19 and 23 Weeks of Gestation. Journal of Clinical Medicine, 13(4), 950. https://doi.org/10.3390/jcm13040950







