Review of Classification Systems for Adult Acquired Flatfoot Deformity/Progressive Collapsing Foot Deformity and the Novel Development of the Triple Classification Delinking Instability/Deformity/Reactivity and Foot Type
Abstract
1. Introduction
Aims
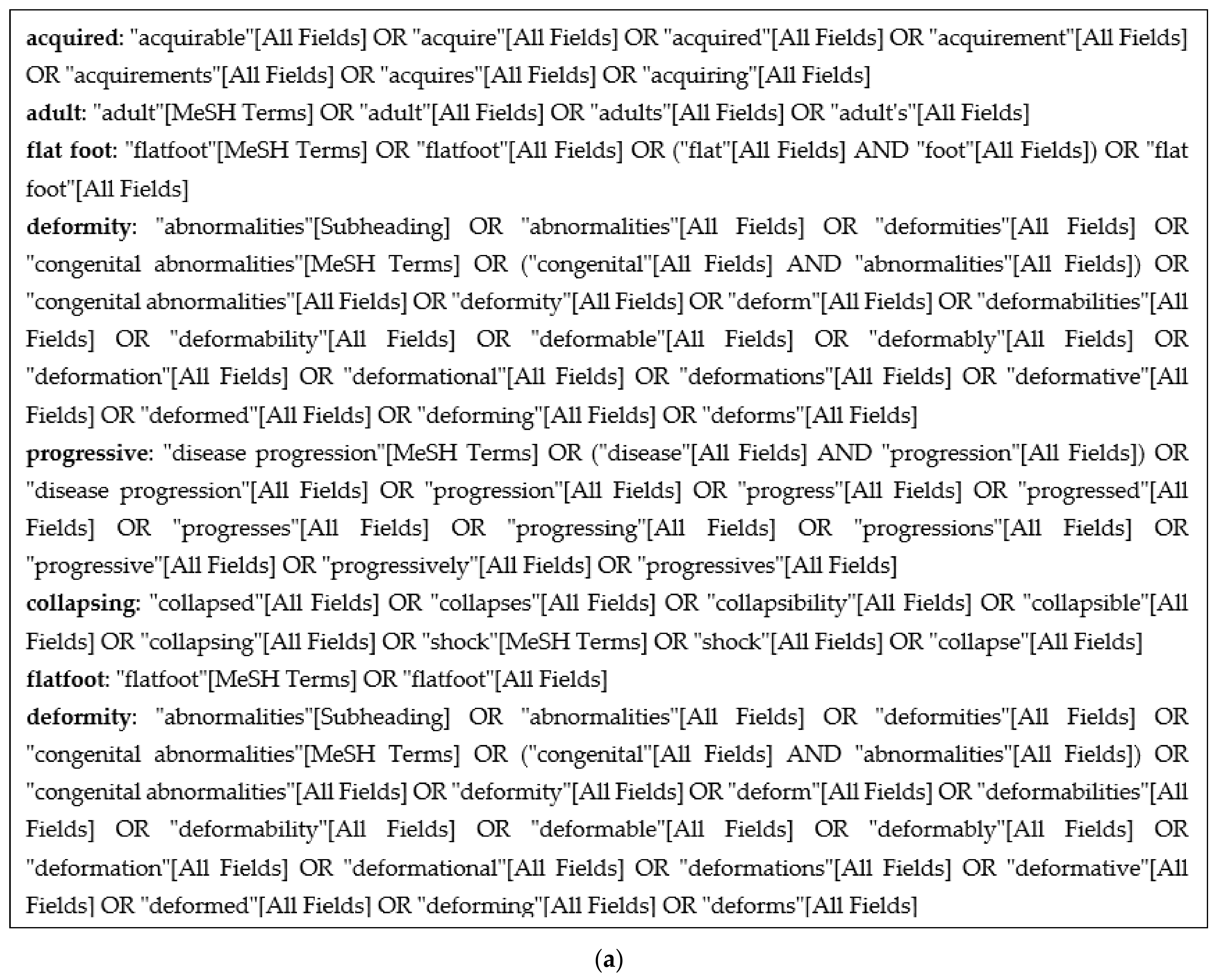
2. Methods
3. Results
A Critical Review of Classifications
4. Discussion
4.1. Understanding the Origin and Identifying Problems of AAFD/PCFD Classifications
- Deformity in AAFD/PCFD is a variable expression of pre-existing foot posture and progressive instability arising from progressive ligament incompetence.
- Anteromedial deltoid instability, lateral column instability, and significant subtalar instability/subluxation from interosseous ligament failure need representation.
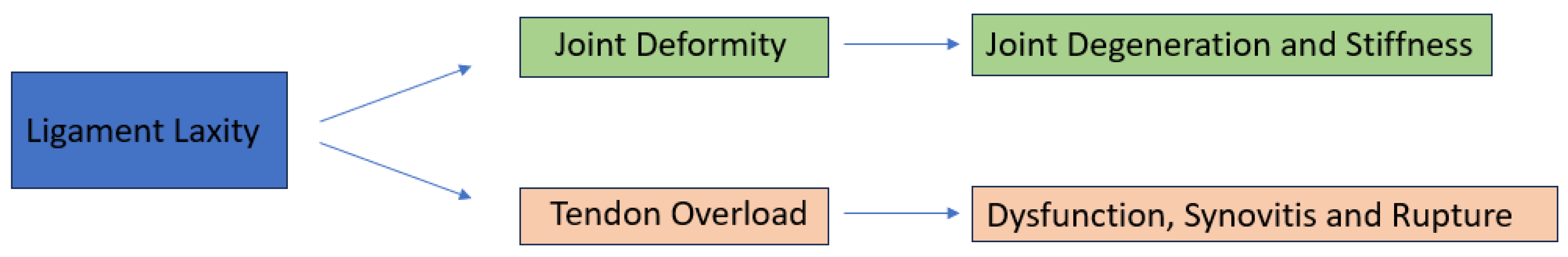
- Overload reactivity of the plantar fascia [11] and the musculotendinous units [23] arise as a result of instability and changes to the subtalar axis (see below). Tendon overload and reactivity vary as the deformity progresses (PL and Tendoachilles), as they become offloaded and may not manifest in all AAFD/PCFD stages.
- Cavus foot types with SL laxity and FRI may have no visible deformity yet have significant instability from ligament laxity and tendon [TP and PL] overload pain [23].
- WB [axial gravitational force] stress joints in the axial plane. Many joints act perpendicular to the axial plane and, therefore, may not be expressive of the respective joint instability on weight-bearing radiographs. Joints whose motion acts perpendicular to the axial weight-bearing axis accentuate instability when forces are applied in the direction of their action. (TN joint: lateral plane/ankle: anteroposterior motion instability and rotational ankle instability at the deltoid).
- Foot abduction stress radiographs exacerbate TN uncoverage, and ankle valgus stress views may accentuate deltoid instability. Both may be significantly underrepresented on weight-bearing radiographs.
4.2. Key Aspects to Take into Consideration in Any New Classification
4.2.1. Importance of Plantar Fascia (PF) in Protecting the SL and Effects of Tight TA
4.2.2. The Role of Musculotendinous Units and Their Overload
4.2.3. Ligament Laxity
What Is New about Instability/Ligament Laxity?
- Progressive ligament laxity is key to symptoms.
- Progressively collapse manifests as soft tissue reactivity and deformity, varying between individuals.
- Feet may not progress through all instability stages. Instability starts medially at the spring ligament and its associated superficial deltoid attachment (deltospring ligament complex) and commonly associated secondary first ray instability to progress to more widespread laxity involving the subtalar joint, ankle, and the lateral column and the ankle. Progression rates may vary.
- Some feet start with pre-existing laxity that has been physiologically normal for that foot, thus not painful. Increased instability progresses the foot to become symptomatic. Normal laxity for any foot may be gauged by contralateral foot comparison if unaffected, from serial foot assessment, or may never be ascertained if no pre-existing reference point exists.
- Lateral column instability, subtalar instability, and anteromedial deltoid instability reflect a greater extent of foot ligament failure than the isolated failure of the medial column. Addressing the medial column alone (superficial deltoid/spring and first ray) may not restore all the foot instabilities that have developed completely.
Evidence for Sequential/Progressive Instabilities in AAFD
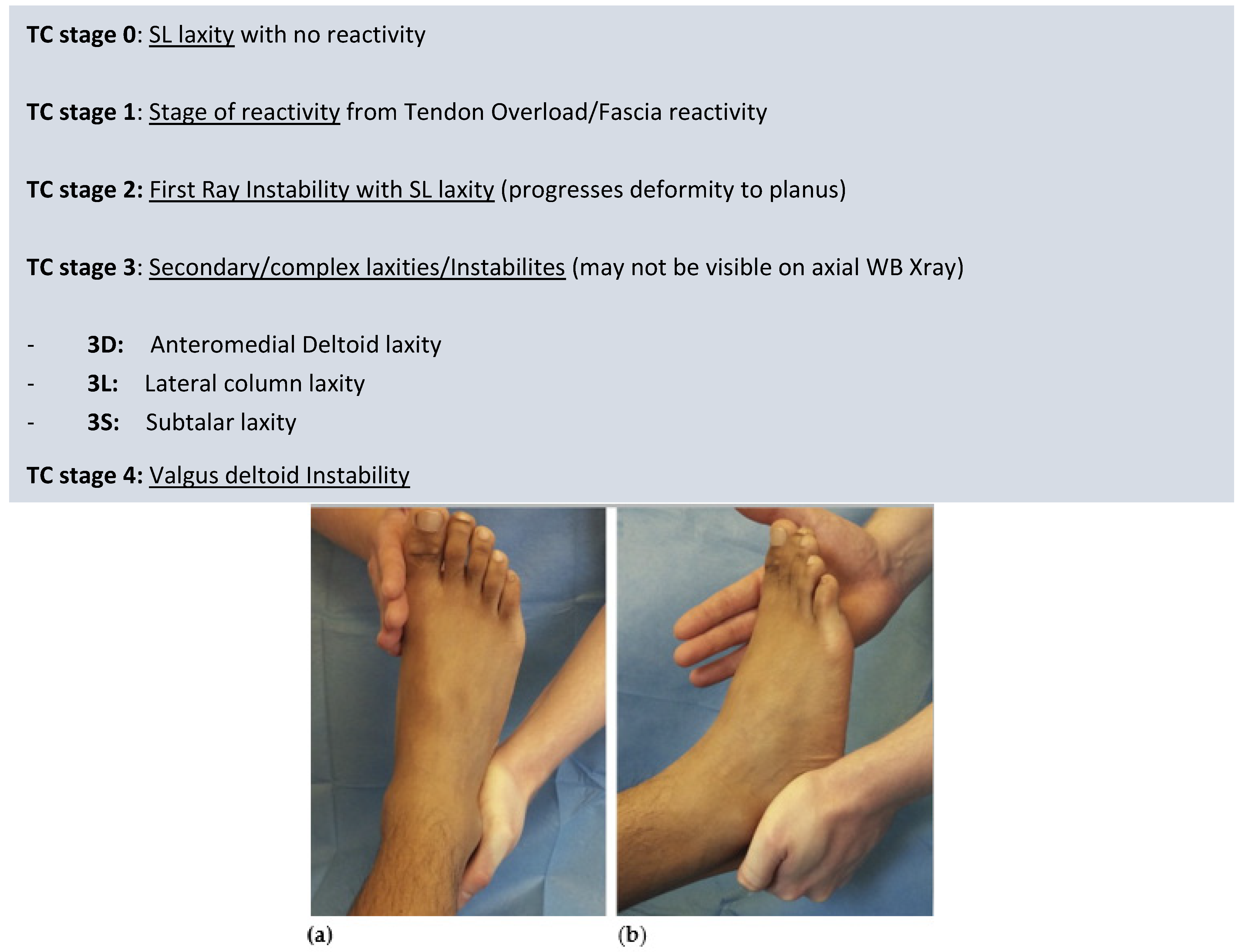
First Ray Instability and Its Classification
Lateral Column Instability/Laxity
Deltoid Ligament Laxity
Subtalar Ligament Laxity
4.3. Foot Type and Potential Differential Behaviour of Cavus Feet
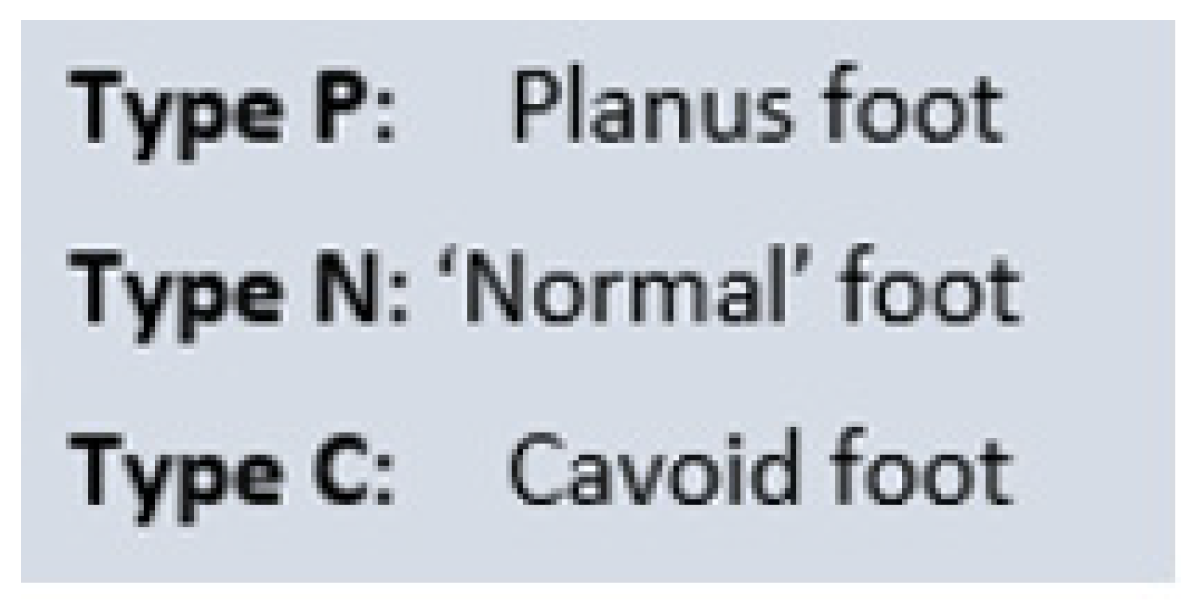
4.4. Triple Classification: Foot Type/Stage of Ligament Laxity/Zone of Deformity
4.4.1. TC Foot Type
4.4.2. TC Stage Based on Ligament Laxity/Instability
Triple Classification Stages
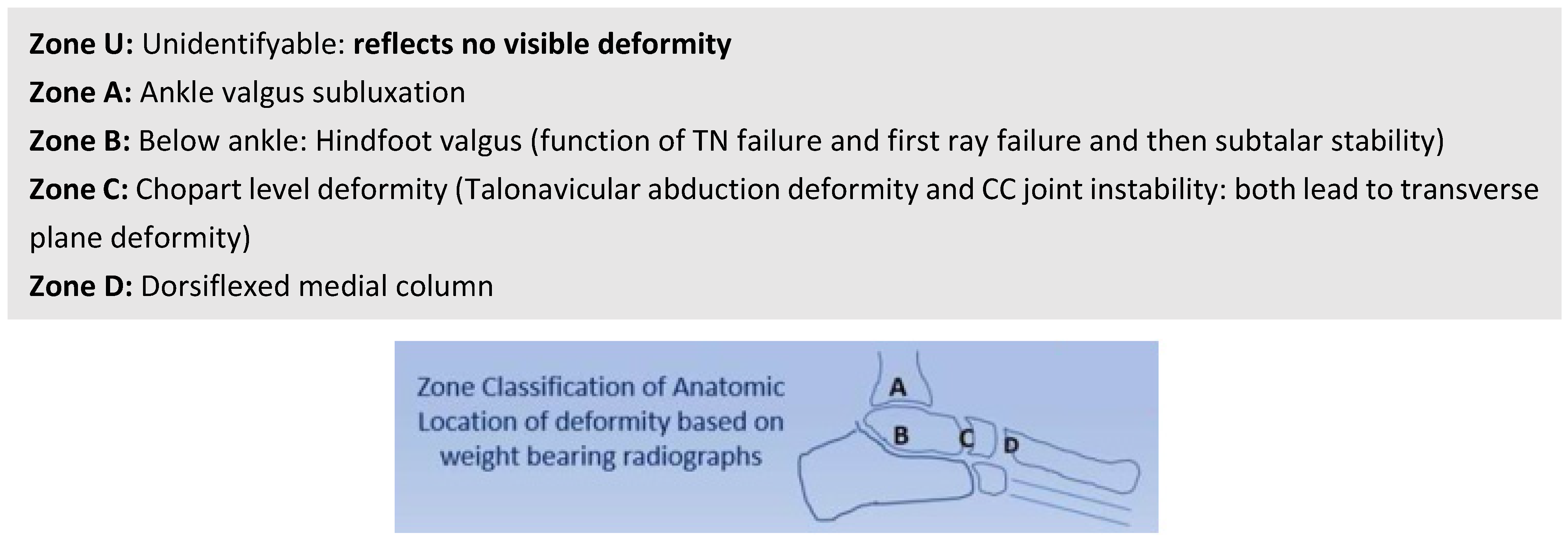
4.5. Overview Diagram of the Triple Classification System
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnson, K.; Strom, D. Tibialis posterior tendon dysfunction. Clin. Orthop. Relat. Res. 1989, 239, 196–206. [Google Scholar] [CrossRef]
- Myerson, M. Adult acquired flatfoot deformity: Treatment of dysfunction of the posterior tibial tendon. Instr. Course Lect. 1997, 46, 393–405. [Google Scholar] [PubMed]
- Weinraub, G.; Heilala, M.A. Adult flatfoot/posterior tibial tendon dysfunction: Outcomes analysis of surgical treatment utilizing an algorithmic approach. J Foot and Ankle Surg. 2000, 6, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Bluman, E.; Title, C.; Myerson, M. Posterior tibial tendon rupture: A refined classification system. Foota Ankle Clin. 2007, 12, 233–249. [Google Scholar] [CrossRef] [PubMed]
- Deland, J.T. Adult-acquired flatfoot deformity. J. Am. Acad. Orthop. Surg. 2008, 16, 399–406. [Google Scholar] [CrossRef]
- Parsons, S.; Naim, S.; Richards, P.; McBride, D. Correction and prevention of deformity in type II tibialis posterior dysfunction. Clin. Orthop. Relat. Res. 2010, 468, 1025–1032. [Google Scholar] [CrossRef]
- Raikin, S.; Winters, B.; Daniel, J. The RAM classification: A novel, systematic approach to the adult-acquired flatfoot. Foot Ankle Clin. 2012, 17, 169–181. [Google Scholar] [CrossRef]
- Lintz, F.; Bernasconi, A.; Li, S.; Lalevée, M.; Fernando, C.; Barg, A.; Dibbern, K.; de Cesar Netto, C. Diagnostic accuracy of measurements in progressive collapsing foot deformity using weight bearing computed tomography: A matched case-control study. Foot Ankle Surg. 2022, 28, 912–918. [Google Scholar] [CrossRef]
- Mansur, N.; Lalevee, M.; Maly, C.; Dibbern, K.; Lee, H.; Godoy-Santos, A.; Lintz, F.; de Cesar Netto, C. Association between Middle Facet Subluxation and Foot and Ankle Offset in Progressive Collapsing Foot Deformity. Foot Ankle Int. 2022, 43, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Myerson, M.; Thordarson, D.; Johnson, J.; Hintermann, B.; Sangeorzan, B.; Deland, J.; Schon, L.; Ellis, S.; de Cesar Netto, C. Classification and Nomenclature: Progressive Collapsing Foot Deformity. Foot Ankle Int. 2020, 41, 1271–1276. [Google Scholar] [CrossRef] [PubMed]
- Pasapula, C.; Cutts, S. Modern Theory of the Development of Adult Acquired Flat Foot and an Updated Spring Ligament Classification System. Clin. Res. Foot Ankle 2017, 5, 247. [Google Scholar] [CrossRef]
- Jeng, C.; Myerson, M. The uses of tendon transfers to correct paralytic deformity of the foot and ankle. Foot Ankle Clin. 2004, 9, 319–337. [Google Scholar] [CrossRef] [PubMed]
- Cifuentes-De la Portilla, C.; Larrainzar-Garijo, R.; Bayod, J. Analysis of the main passive soft tissues associated with adult acquired flatfoot deformity development: A computational modeling approach. J. Biomech. 2019, 84, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Crary, J.; Marcus Hollis, J.; Manoli, A., 2nd. The effect of plantar fascia release on strain in the spring and long plantar ligaments. Foot Ankle Int. 2003, 24, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Mizel, M.; Temple, H.; Scranton, P.J.; Gellman, R.; Hecht, P.; Horton, G.; McCluskey, L.; KA, M. Role of the peroneal tendons in the production of the deformed foot with posterior tibial tendon deficiency. Foot Ankle Int. 1999, 20, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Yeap, J.; Birch, R.; Singh, D. Long-term results of tibialis posterior tendon transfer for drop-foot. Int. Orthop. 2001, 25, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Pecheva, M.; Devany, A.; Nourallah, B.; Cutts, S.; Pasapula, C. Long-term follow-up of patients undergoing tibialis posterior transfer: Is acquired pes planus a complication? Foot 2017, 34, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Dyal, C.; Feder, J.; Deland, J.; Thompson, F. Pes planus in patients with posterior tibial tendon insufficiency: Asymptomatic versus symptomatic foot. Foot Ankle Int. 1997, 18, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Lalevée, M.; Barbachan Mansur, N.; Lee, H.; Ehret, A.; Tazegul, T.; de Carvalho, K.; Bluman, E.; de Cesar Netto, C. A comparison between the Bluman et al. and the progressive collapsing foot deformity classifications for flatfeet assessment. Arch. Orthop. Trauma Surg. 2023, 143, 1331–1339. [Google Scholar] [CrossRef]
- Lee, H.; Barbachan Mansur, N.; Lalevée, M.; Dibbern, K.; Myerson, M.; Ellis, S.; Femino, J.; de Cesar Netto, C. Intra- and Interobserver Reliability of the New Classification System of Progressive Collapsing Foot Deformity. Foot Ankle Int. 2022, 43, 582–589. [Google Scholar] [CrossRef]
- Li, S.; Zhu, M.; Gu, W.; Hamati, M.; Hunt, K.; de Cesar Netto, C.; Simonson, T.; Myerson, M. Diagnostic Accuracy of the Progressive Collapsing Foot Deformity (PCFD) Classification. Foot Ankle Int. 2022, 43, 800–809. [Google Scholar] [CrossRef]
- Boakye, L.; Uzosike, A.; Bluman, E. Progressive Collapsing Foot Deformity: Should We Be Staging It Differently? Foot Ankle Clin. 2021, 26, 417–425. [Google Scholar] [CrossRef]
- Cifuentes-De la Portilla, C.; Pasapula, C.; Gutiérrez-Narvarte, B.; Larrainzar-Garijo, R.; Bayod, J. Peroneus Longus overload caused by soft tissue deficiencies associated with early adult acquired flatfoot: A finite element analysis. Clin. Biomech. 2021, 86, 105383. [Google Scholar] [CrossRef]
- Huang, C.; Kitaoka, H.; An, K.; Chao, E. Biomechanical evaluation of longitudinal arch stability. Foot Ankle 1993, 14, 353–357. [Google Scholar] [CrossRef]
- Hirakawa, K.; Tsutsumi, M.; Kudo, S. Investigation of the relationship between the thickness of the plantar calcaneonavicular ligament and plantar fascia in patients with plantar fasciitis. Foot 2022, 50, 101890. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.; Kolodziej, L.; Kimmel, H. The Frequency of Association between Pathologic Subtalar Joint Alignment in Patients with Recalcitrant Plantar Fasciopathy—A Retrospective Radiographic Evaluation. Clin. Res. Foot Ankle 2019, 7, 2. [Google Scholar]
- McMillan, A.; Landorf, K.; Gilheany, M.; Bird, A.; Morrow, A.; Menz, H. Ultrasound guided corticosteroid injection for plantar fasciitis: Randomised controlled trial. BMJ 2012, 344, e3260. [Google Scholar] [CrossRef] [PubMed]
- Robberecht, J.; Shah, D.; Taylan, O.; Natsakis, T.; Vandeputte, G.; Vander Sloten, J.; Jonkers, I. The role of medial ligaments and tibialis posterior in stabilising the medial longitudinal foot arch: A cadaveric gait simulator study. Foot Ankle Surg. 2022, 28, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Ringleb, S.; Kavros, S.; Kotajarvi, B.; Hansen, D.; Kitaoka, H.; Kaufman, K. Changes in gait associated with acute stage II posterior tibial tendon dysfunction. Gait Posture 2007, 25, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.; Lin, K.; Yang, W.; Chang, Y.; Chou, L. Changes in lower extremity biomechanics and muscle activity after six-minute fast-walk in individuals with flatfoot. Ann. Phys. Rehabil. Med. 2018, 61, 446. [Google Scholar] [CrossRef]
- Jennings, M.; Christensen, J. The effects of sectioning the spring ligament on rearfoot stability and posterior tibial tendon efficiency. J. Foot Ankle Surg. 2008, 47, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Pate, M.; Hall, J.; Albright, P.; Bohay, D.; Anderson, J.; Roberts, J. Increasing Values of the Lateral Talar-First Metatarsal Angle Preoperatively Predict Spring Ligament Attenuation in Adult Acquired Flat Foot Deformity. Foot Ankle Orthop. 2019, 4, 2473011419S00338. [Google Scholar] [CrossRef]
- Pasapula, C.; Devany, A.; Magan, A.; Memarzadeh, A.; Pasters, V.; Shariff, S. Neutral heel lateral push test: The first clinical examination of spring ligament integrity. Foot 2015, 25, 69–74. [Google Scholar] [CrossRef]
- Baxter, J.; LaMothe, J.; Walls, R.; Prado, M.; Gilbert, S.; Deland, J. Reconstruction of the medial talonavicular joint in simulated flatfoot deformity. Foot Ankle Int. 2015, 36, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Amaha, K.; Nimura, A.; Yamaguchi, R.; Kampan, N.; Tasaki, A.; Yamaguchi, K.; Kato, R.; Akita, K. Anatomic study of the medial side of the ankle base on the joint capsule: An alternative description of the deltoid and spring ligament. J. Exp. Orhopaedics 2019, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Chu, I.; Myerson, M.; Nyska, M.; Parks, B. Experimental flatfoot model: The contribution of dynamic loading. Foot Ankle Int. 2001, 22, 220–225. [Google Scholar] [CrossRef]
- Wiegerinck, J.; Stufkens, S. Deltoid Rupture in Ankle Fractures: To Repair or Not to Repair? Foot Ankle Clin. 2021, 26, 361–371. [Google Scholar] [CrossRef]
- Chrastek, D.; Elmousili, M.; Al-Sukaini, A.; Austin, I.; Pasapula, C. Quantitative Assessment of Dorsal Sagittal Lateral Column Instability in Unilateral Adult Acquired Flatfoot Deformity (AAFD); British Orthopaedic Association Annual Congress: Aberdeen, UK, 2021. [Google Scholar]
- Michelson, J.; Varner, K.; Checcone, M. Diagnosing deltoid injury in ankle fractures: The gravity stress view. Clin. Orthop. Relat. Res. 2001, 387, 178–182. [Google Scholar] [CrossRef]
- Femino, J.; Vaseenon, T.; Phisitkul, P.; Tochigi, Y.; Anderson, D.; Amendola, A. Varus external rotation stress test for radiographic detection of deep deltoid ligament disruption with and without syndesmotic disruption: A cadaveric study. Foot Ankle Int. 2013, 34, 251–260. [Google Scholar] [CrossRef]
- de Cesar Netto, C.; Saito, G.; Roney, A.; Roberts, L.; Fansa, A.; Greditzer, H.; Sofka, C.; Deland, J.; Ellis, S. Weightbearing CT and MRI findings of Stage II Flatfoot Deformity: Can We Predict Patients at High-Risk for Foot Collapse? Foot Ankle Orthop. 2019, 4, 2473011419S00161. [Google Scholar] [CrossRef]
- Kato, T. The diagnosis and treatment of instability of the subtalar joint. J. Bone Jt. Surg. Br. 1995, 77, 400–406. [Google Scholar] [CrossRef]


| Classification and Year | Article | Categories | |
|---|---|---|---|
| 1 | Johnson and Strom [1] | 1989 | Original stage 1–3 classification |
| 2 | Myerson et al. [2] | 1997 | Myerson modification of stages 1–4 |
| 3 | Weinraub and Heilala [3] | 2002 | Stage 1–3 and grades (A, B, C) |
| 4 | Bluman et al. [4] | 2007 | Stage 1–4 (A, B, C subtypes) |
| 5 | Deland [5] | 2008 | Stages 1–4 (7 subtypes) |
| 6 | Parsons et al. [6] | 2010 | Stage 1–4 Stage 2 subtypes (A, B, C) |
| 7 | Raikin et al. [7] | 2012 | RAM classification Three categories and six subtypes |
| 8 | Pasapula et al. [11] | 2017 | Stage 0–4 |
| 9 | Myerson et al. [10] | 2020 | Stages 1–2 (5 stages and 2 deformities) |
| Stage of Deformity | ||
|---|---|---|
| Stage I (Flexible) or Stage II (Rigid) | ||
| Type of Deformity | ||
| Deformity Type/Location | Clinical/Radiographic Findings | |
| Class A | Hindfoot valgus deformity | Hindfoot valgus alignment Increased hindfoot moment arm, hindfoot alignment ankle, foot and ankle offset |
| Class B | Midfoot/forefoot abduction deformity | Decreased talar head coverage Increased talonavicular coverage angle Presence of sinus tarsi impingement |
| Class C | Forefoot varus deformity/medial column instability | Increased talus-first metatarsal angle Plantar gapping first tarsometatarsal (TMT) joint/naviculocuneiform (NC) joints Clinical forefoot varus |
| Class D | Peritalar subluxation/dislocation | Significant subtalar joint subluxation/sub-fibular impingement |
| Class E | Ankle instability | Valgus tilting of the ankle joint |
| Name of Classification | Year | Positive Aspects of Classification | Negative Aspects of Classification |
|---|---|---|---|
| Johnson and Strom [1] | 1989 | 1. Original classification that classification systems are based upon 2. Establishedd a basic understanding/method of cummincation patholgy. More severe deformities/stiffness correspond to a greater stage 3. Recognition of tendon reactivity in early stages of AAFD/PCFD where no deformity can present with a reactive TP | 1. No proven linearity of progression between stages 2. Fails to consider foot may not start in neutral 3. Focuses on the tibialis posterior as the prime driving force/causal 4. Stage 2 is very under simplified 5. Very little on the validation of the classification system |
| Myerson [2] | 1997 | 1. Modified Johnson and Strom classification to establish deep deltoid failure in stage 4 | 1. Still focused on tibialis posterior as the prime cause 2. Failure to acknowledge that anteromedial ankle instability occurs prior to deep deltoid ligament failure 3. Assumed linearity of progression |
| Weinraub and Heilala [3] | 2002 | 1. Understood that multiple factors determined the failure of the flatfoot 2. Recognized that the midtarsal joint played an important role in the stabilisation of flatfoot 3. Delinked deformity and tendon pathology | 1. Still primarily focused upon the tibialis posterior tendon as the cause. 2. Based classification upon progressive inflammation/degenerative changes of the tendon |
| Bluman [4] | 2007 | 1. Began to subclassify stage 2 and expand the different types 2. Graded level of deformity 3. Bluman classified a myriad of treatment options for all the subtypes | 1. Classification based upon the tibialis posterior in early stages 2. Implies progression of deformity through set stages 3. No discussion of the spring ligament and other ligaments that fail |
| Deland [5] | 2008 | 1. Recognition of the SL as a cause of potential instability | 2. Still focused on the TP |
| Parsons [6] | 2010 | 1. Began to subtype stage 2 into subtypes of A, B, C | 1. Still focused on stage tibialis posterior as the cause of the flatfoot 2. Broadly based upon Johnson and Strom classification |
| Raikin [7] | 2012 | 1. Previous classifications did not take into consideration the involvement of the mid-foot 2. Classification was based on anatomic location, including the ankle, hindfoot, and mid-foot 3. Subgroups based on characteristic clinical and radiographic findings 4. Treatment algorithms then suggested based on these findings | 1. Several categories make communication more difficult 2. Still focused on tibialis posterior in early stages of the hindfoot |
| Pasapula [11] | 2017 | 1. Introduced the concept of stage 0 2. Recognised that the tibialis posterior may or may not react despite the foot SL weakening and failing | Still used the Johnson and Strom classification Focused on the tibialis posterior in stage 1 Continued to simplify stage 2 |
| Myerson [10] | 2020 | 1. Readdresses the pathology away from the tibialis posterior tendon 2. Several categories allow a more accurate representation of deformity in the foot | 1. Static weight-bearing imaging may miss or underestimate the associated dynamic instabilities 2. Multiple tendon reactivity may be a significant presentation and can present without deformity, which needs representation 3. Focusing on deformity detracts from representing feet with ligament instability and no deformity 4. 242 subtypes identified makes comparative analysis and communication of different grades and stages difficult |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pasapula, C.S.; Choudkhuri, M.R.; Monzó, E.R.G.; Dhukaram, V.; Shariff, S.; Pasterse, V.; Richie, D.; Kobezda, T.; Solomou, G.; Cutts, S. Review of Classification Systems for Adult Acquired Flatfoot Deformity/Progressive Collapsing Foot Deformity and the Novel Development of the Triple Classification Delinking Instability/Deformity/Reactivity and Foot Type. J. Clin. Med. 2024, 13, 942. https://doi.org/10.3390/jcm13040942
Pasapula CS, Choudkhuri MR, Monzó ERG, Dhukaram V, Shariff S, Pasterse V, Richie D, Kobezda T, Solomou G, Cutts S. Review of Classification Systems for Adult Acquired Flatfoot Deformity/Progressive Collapsing Foot Deformity and the Novel Development of the Triple Classification Delinking Instability/Deformity/Reactivity and Foot Type. Journal of Clinical Medicine. 2024; 13(4):942. https://doi.org/10.3390/jcm13040942
Chicago/Turabian StylePasapula, Chandra Seker, Makhib Rashid Choudkhuri, Eva R. Gil Monzó, Vivek Dhukaram, Sajid Shariff, Vitālijs Pasterse, Douglas Richie, Tamas Kobezda, Georgios Solomou, and Steven Cutts. 2024. "Review of Classification Systems for Adult Acquired Flatfoot Deformity/Progressive Collapsing Foot Deformity and the Novel Development of the Triple Classification Delinking Instability/Deformity/Reactivity and Foot Type" Journal of Clinical Medicine 13, no. 4: 942. https://doi.org/10.3390/jcm13040942
APA StylePasapula, C. S., Choudkhuri, M. R., Monzó, E. R. G., Dhukaram, V., Shariff, S., Pasterse, V., Richie, D., Kobezda, T., Solomou, G., & Cutts, S. (2024). Review of Classification Systems for Adult Acquired Flatfoot Deformity/Progressive Collapsing Foot Deformity and the Novel Development of the Triple Classification Delinking Instability/Deformity/Reactivity and Foot Type. Journal of Clinical Medicine, 13(4), 942. https://doi.org/10.3390/jcm13040942






