Clinical, Radiologic, and Functional Outcomes following Bone Grafting for Metacarpal Non-Unions: A Systematic Review
Abstract
1. Introduction
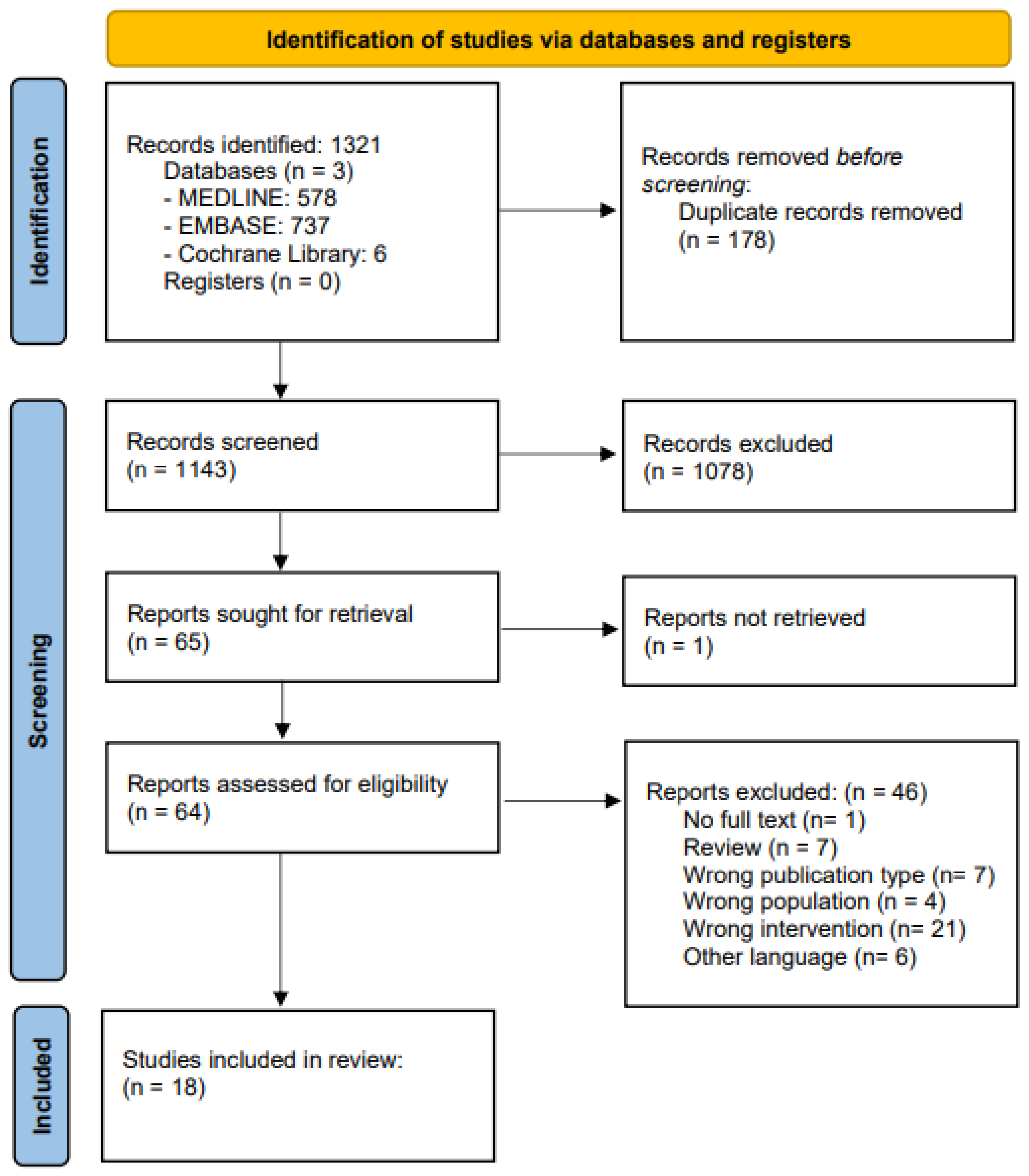
2. Methods
2.1. Search Strategy
2.2. Study Selection and Eligibility
3. Results
3.1. Study Characteristics
3.2. Patient Characteristics
3.3. Non-Union Features and Grafting Techniques
3.4. Post-Operative Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Phieffer, L.S.; Goulet, J.A. Delayed unions of the tibia. J. Bone Jt. Surg. Am. 2006, 88, 206–216. [Google Scholar] [CrossRef] [PubMed]
- LaVelle, D.G. Delayed union and nonunion of fractures. Campbell Oper. Orthop. 2003, 3, 3125–3165. [Google Scholar]
- Yeo, J.H.; Kim, J.Y. Surgical Strategy for Scaphoid Nonunion Treatment. J. Hand Surg. Asian Pac. Vol. 2018, 23, 450–462. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.A.; Moon, M.S. Treatment strategy for nonunions and malunions. Surg. Treat. Orthop. Trauma 2007, 1, 77–100. [Google Scholar]
- Joshua, D.T.; James, L.K. Bone Nonunion; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Rajasekaran, S.; Giannoudis, P.V. Open injuries of the lower extremity: Issues and unknown frontiers. Injury 2012, 43, 1783–1784. [Google Scholar] [CrossRef]
- Copuroglu, C.; Calori, G.M.; Giannoudis, P.V. Fracture non-union: Who is at risk? Injury 2013, 44, 1379–1382. [Google Scholar] [CrossRef]
- Dimitriou, R.; Kanakaris, N.; Soucacos, P.N.; Giannoudis, P.V. Genetic predisposition to non-union: Evidence today. Injury 2013, 44 (Suppl. S1), S50–S53. [Google Scholar] [CrossRef]
- Pountos, I.; Georgouli, T.; Pneumaticos, S.; Giannoudis, P.V. Fracture non-union: Can biomarkers predict outcome? Injury 2013, 44, 1725–1732. [Google Scholar] [CrossRef]
- Bishop, J.A.; Palanca, A.A.; Bellino, M.J.; Lowenberg, D.W. Assessment of compromised fracture healing. J. Am. Acad. Orthop. Surg. 2012, 20, 273–282. [Google Scholar] [CrossRef]
- Hak, D.J.; Fitzpatrick, D.; Bishop, J.A.; Marsh, J.L.; Tilp, S.; Schnettler, R.; Simpson, H.; Alt, V. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury 2014, 45 (Suppl. S2), S3–S7. [Google Scholar] [CrossRef]
- Clancey, G.J.; Hansen, S.T., Jr. Open fractures of the tibia: A review of one hundred and two cases. J. Bone Jt. Surg. Am. 1978, 60, 118–122. [Google Scholar] [CrossRef]
- Velazco, A.; Whitesides, T.E.; Jr Fleming, L.L. Open fractures of the tibia treated with the Lottes nail. J. Bone Jt. Surg. Am. 1983, 65, 879–885. [Google Scholar] [CrossRef]
- Cogsil, T.; Boyer, M.I.; Goldfarb, C.A. The Iliac Crest Top Hat Bone Graft for Challenging Metacarpal Nonunion. J. Hand Surg. Am. 2022, 47, 694.e1–694.e4. [Google Scholar] [CrossRef]
- Jupiter, J.B.; Koniuch, M.P.; Smith, R.J. The management of delayed union and nonunion of the metacarpals and phalanges. J. Hand Surg. Am. 1985, 10, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, K.; Chung, K.C. Treatment of scaphoid fractures and nonunions. J. Hand Surg. Am. 2008, 33, 988–997. [Google Scholar] [CrossRef] [PubMed]
- Schottel, P.C.; O’Connor, D.P.; Brinker, M.R. Time Trade-Off as a Measure of Health-Related Quality of Life: Long Bone Nonunions Have a Devastating Impact. J. Bone Jt. Surg. Am. 2015, 97, 1406–1410. [Google Scholar] [CrossRef] [PubMed]
- Brinker, M.R.; Loftis, C.M.; Khoriaty, J.D.; Dunn, W.R. The devastating effects of humeral nonunion on health-related quality of life. J. Shoulder Elbow Surg. 2022, 31, 2578–2585. [Google Scholar] [CrossRef] [PubMed]
- Factor, S.; Druckmann, I.; Atlan, F.; Rosenblatt, Y.; Tordjman, D.; Krespi, R.; Kazum, E.; Pritsch, T.; Eisenberg, G. The Effects of Novel Pulsed Electromagnetic Field Therapy Device on Acute Distal Radius Fractures: A Prospective, Double-Blind, Sham-Controlled, Randomized Pilot Study. J. Clin. Med. 2023, 12, 1866. [Google Scholar] [CrossRef] [PubMed]
- Hayes, D.S.; Cush, C.; El Koussaify, J.; Manzar, S.; Klena, J.C.; Grandizio, L.C. Defining Nonunion for Metacarpal Fractures: A Systematic Review. J. Hand Surg. Glob. Online 2023, 5, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Sen, M.K.; Miclau, T. Autologous iliac crest bone graft: Should it still be the gold standard for treating nonunions? Injury 2007, 38 (Suppl. S1), S75–S80. [Google Scholar] [CrossRef]
- Pinder, R.M.; Brkljac, M.; Rix, L.; Muir, L.; Brewster, M. Treatment of Scaphoid Nonunion: A Systematic Review of the Existing Evidence. J. Hand Surg. Am. 2015, 40, 1797–1805.e3. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Stern, P.J. Management of fractures of the hand over the last 25 years. J. Hand Surg. 2000, 25, 817–823. [Google Scholar] [CrossRef] [PubMed]
- McNemar, T.B.; Howell, J.W.; Chang, E. Management of metacarpal fractures. J. Hand Ther. 2003, 16, 143–151. [Google Scholar] [CrossRef]
- Jones, N.F.; Jupiter, J.B.; Lalonde, D.H. Common fractures and dislocations of the hand. Plast. Reconstr. Surg. 2012, 130, 722e–736e. [Google Scholar] [CrossRef] [PubMed]
- Chin, S.H.; Vedder, N.B. MOC-PS (SM) CME Article: Metacarpal Fractures. Plast. Reconstr. Surg. 2008, 121, 1–13. [Google Scholar] [CrossRef]
- Neumeister, M.W.; Webb, K.; McKenna, K. Non-surgical management of metacarpal fractures. Clin. Plast. Surg. 2014, 41, 451–461. [Google Scholar] [CrossRef]
- Stern, P. Fracture of the metacarpals and phalanges. Oper. Hand Surg. 1993, 9, e3871. [Google Scholar]
- de Putter, C.; Selles, R.; Polinder, S.; Panneman, M.; Hovius, S.; van Beeck, E. Economic impact of hand and wrist injuries: Health-care costs and productivity costs in a population-based study. J. Bone Jt. Surg. Am. 2012, 94, e56. [Google Scholar] [CrossRef]
- O'Neill, T.W.; Cooper, C.; Finn, J.D.; Lunt, M.; Purdie, D.; Reid, D.M.; Rowe, R.; Woolf, A.D.; Wallace, W.A. Incidence of distal forearm fracture in British men and women. Osteoporos. Int. 2001, 12, 555–558. [Google Scholar] [CrossRef]
- Zura, R.; Xiong, Z.; Einhorn, T.; Watson, J.T.; Ostrum, R.F.; Prayson, M.J.; Della Rocca, G.J.; Mehta, S.; McKinley, T.; Wang, Z.; et al. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg. 2016, 151, e162775. [Google Scholar] [CrossRef]
- Czerniecki, S.; Mishu, M.; Schmucker, R. Metacarpal and Phalangeal Nonunions. Hand Clin. 2024, 40, 129–139. [Google Scholar] [CrossRef]
- Bhandari, M.; Fong, K.; Sprague, S.; Williams, D.; Petrisor, B. Variability in the definition and perceived causes of delayed unions and nonunions: A cross-sectional, multinational survey of orthopaedic surgeons. JBJS 2012, 94, e109. [Google Scholar] [CrossRef]
- Ali, H.; Rafique, A.; Bhatti, M.; Ghani, S.; Sadiq, M.; Beg, S.A. Management of fractures of metacarpals and phalanges and associated risk factors for delayed healing. J. Pak. Med. Assoc. 2007, 57, 64. [Google Scholar]
- Hastings, H. Open fractures and those with soft-tissue damage: Treatment by external fixation. Fract. Hand Wrist Edinb. Churchill Livingstone 1988, 10, 145–172. [Google Scholar]
- Hammert, W.C. Treatment of nonunion and malunion following hand fractures. Clin. Plast. Surg. 2011, 38, 683–695. [Google Scholar] [CrossRef]
- Milhoan, M.; Hoelscher, V.; Pientka, W.F., 2nd. Iliac Crest Bone Graft with Intramedullary Headless Implant for Metacarpal Bone Loss. Tech. Hand. Up Extrem. Surg. 2023, 27, 120–124. [Google Scholar] [CrossRef]
- Jorquera Aguilera, R.; Melibosky, F.; Brunelli, J.P.F.; Delgado, P.J.; Kaempf de Oliveira, R. Headless Compression Screw for Metacarpal Nonunion: Description of a New Technique and Report of 4 Cases. Tech. Hand Up Extrem. Surg. 2022, 26, 232–239. [Google Scholar] [CrossRef]
- Takami, H.; Takahashi, S.; Ando, M. Scaphoid nonunion treated by open reduction, anterior inlay bone grafting, and Kirschner-wire fixation. Arch. Orthop. Trauma. Surg. 2000, 120, 134–138. [Google Scholar] [CrossRef]
- Choudry, U.H.; Bakri, K.; Moran, S.L.; Karacor, Z.; Shin, A.Y. The vascularized medial femoral condyle periosteal bone flap for the treatment of recalcitrant bony nonunions. Ann. Plast. Surg. 2008, 60, 174–180. [Google Scholar] [CrossRef]
- Ferguson, D.O.; Shanbhag, V.; Hedley, H.; Reichert, I.; Lipscombe, S.; Davis, T.R. Scaphoid fracture non-union: A systematic review of surgical treatment using bone graft. J. Hand Surg. Eur. Vol. 2016, 41, 492–500. [Google Scholar] [CrossRef]
- Hirche, C.; Xiong, L.; Heffinger, C.; Münzberg, M.; Fischer, S.; Kneser, U.; Kremer, T. Vascularized versus non-vascularized bone grafts in the treatment of scaphoid non-union: A clinical outcome study with therapeutic algorithm. J. Orthop. Surg. 2017, 25, 2309499016684291. [Google Scholar] [CrossRef]
- Taylor, G.I.; Miller, G.D.; Ham, F.J. The free vascularized bone graft: A clinical extension of microvascular techniques. Plast. Reconstr. Surg. 1975, 55, 533–544. [Google Scholar] [CrossRef]
- Allsopp, B.J.; Hunter-Smith, D.J.; Rozen, W.M. Vascularized versus nonvascularized bone grafts: What is the evidence? Clin. Orthop. Relat. Res. 2016, 474, 1319–1327. [Google Scholar] [CrossRef]
- Testa, G.; Lucenti, L.; D’amato, S.; Sorrentino, M.; Cosentino, P.; Vescio, A.; Pavone, V. Comparison between vascular and non-vascular bone grafting in scaphoid nonunion: A systematic review. J. Clin. Med. 2022, 11, 3402. [Google Scholar] [CrossRef]
- Kim, J.; Yoon, J.; Baek, H. Corticocancellous bone graft vs cancellous bone graft for the management of unstable scaphoid nonunion. Orthop. Traumatol. Surg. Res. 2018, 104, 115–120. [Google Scholar] [CrossRef]
- Robbins, R.R.; Carter, P.R. Iliac crest bone grafting and Herbert screw fixation of nonunions of the scaphoid with avascular proximal poles. J. Hand Surg. 1995, 20, 818–831. [Google Scholar] [CrossRef]
- Harpf, C.; Gabl, M.; Reinhart, C.; Schoeller, T.; Bodner, G.; Pechlaner, S.; Piza-Katzer, H.; Hussl, H. Small free vascularized iliac crest bone grafts in reconstruction of the scaphoid bone: A retrospective study in 60 cases. Plast. Reconstr. Surg. 2001, 108, 664–674. [Google Scholar] [CrossRef]
- Han, C.S.; Wood, M.B.; Bishop, A.T.; Cooney, W.P., 3rd. Vascularized bone transfer. J. Bone Jt. Surg. Am. 1992, 74, 1441–1449. [Google Scholar] [CrossRef]
- Weiland, A.J. Current concepts review: Vascularized free bone transplants. J. Bone Jt. Surg. Am. 1981, 63, 166–169. [Google Scholar] [CrossRef]
- Hsu, C.C.; Tseng, J.; Lin, Y.T. Chimeric Medial Femoral Condyle Osteocutaneous Flap for Reconstruction of Multiple Metacarpal Defects. J. Hand Surg. Am. 2018, 43, 781.e1–781.e9. [Google Scholar] [CrossRef]
- Soucacos, P.N.; Kokkalis, Z.T.; Piagkou, M.; Johnson, E.O. Vascularized bone grafts for the management of skeletal defects in orthopaedic trauma and reconstructive surgery. Injury 2013, 44, S70–S75. [Google Scholar] [CrossRef]
- Foster, R.D.; Anthony, J.P.; Sharma, A.; Pogrel, M.A. Vascularized bone flaps versus nonvascularized bone grafts for mandibular reconstruction: An outcome analysis of primary bony union and endosseous implant success. Head Neck J. Sci. Spec. Head Neck 1999, 21, 66–71. [Google Scholar] [CrossRef]
- Bumbasirevic, M.; Stevanovic, M.; Bumbasirevic, V.; Lesic, A.; Atkinson, H.D. Free vascularised fibular grafts in orthopaedics. Int. Orthop. 2014, 38, 1277–1282. [Google Scholar] [CrossRef]
- Pogrel, M.; Podlesh, S.; Anthony, J.P.; Alexander, J. A comparison of vascularized and nonvascularized bone grafts for reconstruction of mandibular continuity defects. J. Oral. Maxillofac. Surg. 1997, 55, 1200–1206. [Google Scholar] [CrossRef]
- Garnavos, C. Treatment of aseptic non-union after intramedullary nailing without removal of the nail. Injury 2017, 48, S76–S81. [Google Scholar] [CrossRef]
- Phillips, M.R.; Harrison, A.; Mehta, S.; Nolte, P.A.; Bhandari, M.; Zura, R. A Scoping Review of Operative and Non-Invasive Management in the Treatment of Nonunions. Injury 2022, 53, 3872–3878. [Google Scholar] [CrossRef]
- Nolte, P.A.; van der Krans, A.; Patka, P.; Janssen, I.M.; Ryaby, J.P.; Albers, G.R. Low-intensity pulsed ultrasound in the treatment of nonunions. J. Trauma Acute Care Surg. 2001, 51, 693–703. [Google Scholar] [CrossRef]
- Lerner, A.; Stein, H.; Soudry, M. Compound high-energy limb fractures with delayed union: Our experience with adjuvant ultrasound stimulation (exogen). Ultrasonics 2004, 42, 915–917. [Google Scholar] [CrossRef]
- Leighton, R.; Watson, J.T.; Giannoudis, P.; Papakostidis, C.; Harrison, A.; Steen, R.G. Healing of fracture nonunions treated with low-intensity pulsed ultrasound (LIPUS): A systematic review and meta-analysis. Injury 2017, 48, 1339–1347. [Google Scholar] [CrossRef]
- Haller, P.; Nunag, P.; Papadopoulos, A. Low-Intensity Pulsed Ultrasound Treatment for Non-unions of Long Bone Fractures in a Scottish District General Hospital. Cureus 2023, 15, e34159. [Google Scholar] [CrossRef] [PubMed]
- Bioventus. Exogen: Ultrasound Bone Healing System. Available online: https://www.exogen.com/cd/ (accessed on 1 September 2023).
| Study | Management | Time to Follow up (Mean) | Time to Bone Fusion (Mean) | Rates of Non-Union (%) | Radiological Outcomes | VAS Score | Pain | ROM | Grip Strength |
|---|---|---|---|---|---|---|---|---|---|
| Aguilera et al. (2022) | M1: Immobilized for 2 w M2: Immobilized with wrist plaster for 7 d, and finger buddy taping for 3 w M3: NR F1: NR | M1: 5 w M2: 45 d M3: 10 w F1: 2 m (1.8 m) | M1: 5 w M2: 45 d M3: 10 w F1: NR (1.8 m) | 0/3 (0%) | M1: Bone healing at 5 w postoperatively M2: Fracture healing present at 45 d of evolution M3: Complete bone healing after 10 w F1: NR | NR | M1: NR M2: NR M3: NR F1: Completely painless | M1: Same as contralateral side M2: Full ROM at 45 d of evolution M3: Comparable to contralateral side. F1: Full ROM without any fracture mobility | M1: NR M2: NR M3: NR F1: 14 kg vs. 16 kg in the uninjured side |
| Akmaz et al. (2004) | Wound irrigation and debridement | M1: 12 m M2: 13 m M3: 15 m M4: 20 m M5: 8 m M6: 30 m M7: 9 m M8: 11 m (14.8 m) | M1: 16 w M2: 10 w M3: 12 w M4: 12 w M5: 8 w M6: 16 w M7: 10 w M8: 12 w (12 m) | 0/8 (0%) | Radiological union established in all cases | NR | All fingers were painless | Pre: Post (MP joint) M1: 2nd metacarpal 40°:75° 3rd metacarpal: 30°: 60° M2: 55°:75° M3: 40°:85° M4: 60°:60° M5: 50°:80° M6: 50°:80° M7: 60°:80° M8: 55°:85° | Pre (injured side/uninjured side): Post (kg) M1: 16/35:20 M2: 20/35:26 M3: 15/42:19 M4: 22/35:27 M5: 20/38:25 M6: 20/35:24 M7: 20/38:23 M8: 20/40:26 |
| Anderson et al. (2022) | Maximal hand therapy | Short-term: 2 y post-injury Long-term: 5 y post-injury | NR | NR | NR | NR | 2y post-injury: Discomfort at the dorsal metacarpal plate 5y post-injury: Overall doing well | MPJ: - 10° to 80° PIPJ: +15° to 100° DIPJ: 0° to 65° TAM: 270° | 41 lbs vs. 110 lbs in uninjured hand |
| Christen et al. (2022) | 100 mg Aspirin DIE × 1 m | NR | P1: 7 m P2: 5 m P3: 7 m P4: 8 m (6.75 m) | 0/4 (0%) | NR | NR | NR | P1: Severe 5th ray stiffness P2: Full active ROM, slight 15° PIPJ extension lag P3: Limited 60° PIPJ flexion P4: Limited 25° MPJ flexion, MPJ extension stiffness | NR |
| Cogsil et al. (2022) | Hand therapy and removable brace started at 1 w, worn ×6–8 w based on radiographic bony union evidence | M: 3 m F: 4 m (3.5 m) | M: 3 m F: 4 m (3.5 m) | 0/2 (0%) | M: Solid healing at 3 m postoperatively F: Full consolidation and healing 4 m postoperatively | NR | M: NR F: Pain free | M: Full finger motion F: NR | Pre/Post (lb) M: 125/50 F: NR |
| Deng et Al. (2020) | NR | 24 m | 24 m | 0/1 (0%) | United graft with no signs of instability | NR | Pain free | 70° MPJ flexion, no extension lag | NR |
| Doi and Sakai (1994) | NR | NR | 2m | 0/1 (0%) | NR | NR | NR | NR | NR |
| Ebraheim et al. (1997) | NR | 1st FU: 3 m 2nd FU:12 m | 3 m | 0/1 (0%) | NR | NR | NR | Full digital flexion/extension at 12 m | NR |
| Erçin et al. (2022) | Postoperative IV fluids, analgesics, antibiotics & anticoagulants, Volar splint applied, and flaps checked every 4 h | 6 m | 6 m | 0/11 (0%) | Union at 6 m for all patients | P1 (M): 3 P2 (M): 3 P3 (M): 4 P4 (F): 3 P5 (M): 4 P6 (M): 3 P7 (M): 4 P8 (F): 7 P9 (M): 3 P10 (M): 5 P11 (M): 4 | NR | NR | NR |
| Ferguson and Bogoch (1999) | Hand splint for 3 m postoperatively and then casted | 27 m | 27 m | 0/1 (0%) | Graft incorporation observed at 27 m | NR | Pain free | 0° to 70° active MPJ ROM | NR |
| Ireland and Taleisnkik (1986) | Short arm cast immobilization for 6 w postoperatively | First FU: 2 m Second FU: 3 m | 3 m | 0/1 (0%) | Non-union healed 3 m postoperatively | NR | NR | NR | NR |
| Jupiter et al. (1985) | NR | NR | P1: 12 w P2: 12 w P3: 8 w P4: 12 w P5: 12 w P6: 8 w (2.7 m) | 0/6 (0%) | NR | NR | NR | Pre: Post P1: MPJ: 0/90°: 0/90° TAM: 250°:250° P2: MPJ: 0/10°:0/70° TAM: 250°:250° P3: MPJ: 0/90°:0/90° TAM: 190°:200° P4: MPJ: 0/45°:0/65° TAM: 170°:210° P5: 2nd metacarpal MPJ: 0–90°:0–90° TAM: 250°:250° P6: MPJ: 0/50°:0/80° TAM: 195°:245° | NR |
| Milhoan et al. (2022) | Ulnar gutter splint immobilization for 2 w | 1st FU: 2 w 2nd FU: 6 w 3rd Fu: 6 m | NR | NR | NR | NR | Pain resolution at 2 w FU | Recovered full active and passive digital motion at 6 m | NR |
| Sakai et al. (1988) | NR | 7 m | 2 m | 0/1 (0%) | NR | NR | NR | NR | NR |
| Tsai et al. (1981) | NR | 43 m | NR | NR | NR | NR | NR | 2nd toe (index finger): ML: 50/65° PIPJ: 40/45° DIPJ: 15/30° 3rd toe (little finger): ML: 40/65° PIPJ: 30/60° DIPJ: 20/45° | 26 lb |
| Vegas et al. (2012) | NR | 9 m | 9 m | 0/1 (0%) | Unequivocal bone union signs at 9 m | NR | NR | NR | NR |
| Wei et al. (1999) | NR | 57 m | NR | NR | NR | NR | NR | NR | NR |
| Zargarbashi et al. (2018) | Active motion & physical therapy as soon as possible and K-wires removal at 6 w postoperatively | 1.5 m | 6 m | 0/1 (0%) | Healed 6 m post-treatment | NR | NR | NR | NR |
| Study | Pinch Strength | Surgical Complications | Return to ADLs | Patient Satisfaction | Sensation |
|---|---|---|---|---|---|
| Aguilera et al. (2022) | NR | Zero | M1: NR M2: Returned to everyday unrestricted activities M3: NR F: NR | NR | NR |
| Akmaz et al. (2004) | NR | Pintract infection in 1 patient, treated successfully with wound dressings and oral antibiotics | All able to use their hands for daily activities postoperatively | NR | Adequate circulation and sensation in all fingers |
| Anderson et al. (2022) | NR | Zero | Capable of performing ADLs and associated hobbies at 5 y postoperatively | Overall pleased | 6/10 at digit tip |
| Christen et al. (2022) | NR | Zero | NR | P1: NR P2: NR P3: Satisfied P4: NR | NR |
| Cogsil et al. (2022) | M: Pre/Post (lb): 22/11 F: 10 lb vs. 22 lb contralaterally | Zero | NR | NR | NR |
| Deng et Al. (2020) | NR | NR | NR | NR | NR |
| Doi and Sakai (1994) | NR | NR | NR | NR | NR |
| Ebraheim et al. (1997) | NR | NR | Return to previous occupation at 12 m | NR | NR |
| Erçin et al. (2022) | NR | Donor site hematoma: 1 Recipient site hematoma: 1 Recipient site prolonged seroma: 1 | NR | P1 (M): 3, P2 (M): 4 P3 (M): 3, P4 (F): 3 P5 (M): 4, P6 (M): 4 P7 (M): 3, P8 (F): 4 P9 (M): 3, P10 (M): 4 P11 (M): 4 (1 = very bad, 5 = excellent) | NR |
| Ferguson and Bogoch (1999) | NR | NR | Carry out work/leisure activities | NR | NR |
| Ireland and Taleisnkik (1986) | NR | NR | NR | NR | NR |
| Jupiter et al. (1985) | NR | NR | NR | NR | NR |
| Milhoan et al. (2022) | NR | Zero | Cleared to resume normal activities at 6 w postoperatively | NR | NR |
| Sakai et al. (1988) | NR | Zero | NR | NR | NR |
| Tsai et al. (1981) | Between thumb & 2nd toe/index finger: 9 lb Between thumb & 3rd toe (little finger): 6.5 lb | NR | Returned to former job in grain elevator | NR | Two-point discrimination: 2nd toe/index finger: 15 mm 3rd toe/little finger: 12 mm |
| Vegas et al. (2012) | NR | NR | NR | NR | NR |
| Wei et al. (1999) | Pulp-to-pulp pinch on L hand: 2.5kg Tripod pinch power on R hand: 3.6 kg | Zero | Returned to previous activities and job as a guard, uses a gas pistol and drives a motorcycle to work. | NR | Moving two-point discrimination at 57 m FU: Thumbs: 4-mm 3 new fingers: range of 4 to 1 mm |
| Zargarbashi et al. (2018) | NR | Zero | NR | NR | NR |
| Mean Age (years) | % of Patients with Dominant Hand Affected | Mean Prior # of Bone Operations | Mean Time from Injury to Graft (months) | Mean Time from Last Intervention (months) | % Atrophic Nonunions | % Nonunions due to Infection | Mean Time to Follow-Up (months) | |
|---|---|---|---|---|---|---|---|---|
| Value | 30.2 | 41.7 | 1.3 | 9.7 | 4.5 | 50 | 8.9 | 12.4 |
| N Studies | 18 | 7 | 16 | 15 | 10 | 7 | 16 | 16 |
| Mean Postoperative Immobilization Time (Weeks) | Mean Time to Union (Months) | % of Graft Failures | % of Pain Improvement | % of Complications | % of Patients Return to ADLs | % Patient Satisfaction Rate | % of Improved Functionality | |
|---|---|---|---|---|---|---|---|---|
| Value | 1.7 | 6.9 | 0 | 76 | 11.8 | 4.5 m | 61.5 | 100 |
| N Studies | 8 | 14 | 14 | 8 | 10 | 10 | 3 | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El Sewify, O.; Abi-Rafeh, J.; Legler, J.; Karimi, S.; Baradaran, A.; Efanov, J.I. Clinical, Radiologic, and Functional Outcomes following Bone Grafting for Metacarpal Non-Unions: A Systematic Review. J. Clin. Med. 2024, 13, 1148. https://doi.org/10.3390/jcm13041148
El Sewify O, Abi-Rafeh J, Legler J, Karimi S, Baradaran A, Efanov JI. Clinical, Radiologic, and Functional Outcomes following Bone Grafting for Metacarpal Non-Unions: A Systematic Review. Journal of Clinical Medicine. 2024; 13(4):1148. https://doi.org/10.3390/jcm13041148
Chicago/Turabian StyleEl Sewify, Omar, Jad Abi-Rafeh, Jack Legler, Shayan Karimi, Aslan Baradaran, and Johnny I. Efanov. 2024. "Clinical, Radiologic, and Functional Outcomes following Bone Grafting for Metacarpal Non-Unions: A Systematic Review" Journal of Clinical Medicine 13, no. 4: 1148. https://doi.org/10.3390/jcm13041148
APA StyleEl Sewify, O., Abi-Rafeh, J., Legler, J., Karimi, S., Baradaran, A., & Efanov, J. I. (2024). Clinical, Radiologic, and Functional Outcomes following Bone Grafting for Metacarpal Non-Unions: A Systematic Review. Journal of Clinical Medicine, 13(4), 1148. https://doi.org/10.3390/jcm13041148





