Limited Intervention in Adult Scoliosis—A Systematic Review
Abstract
1. Introduction
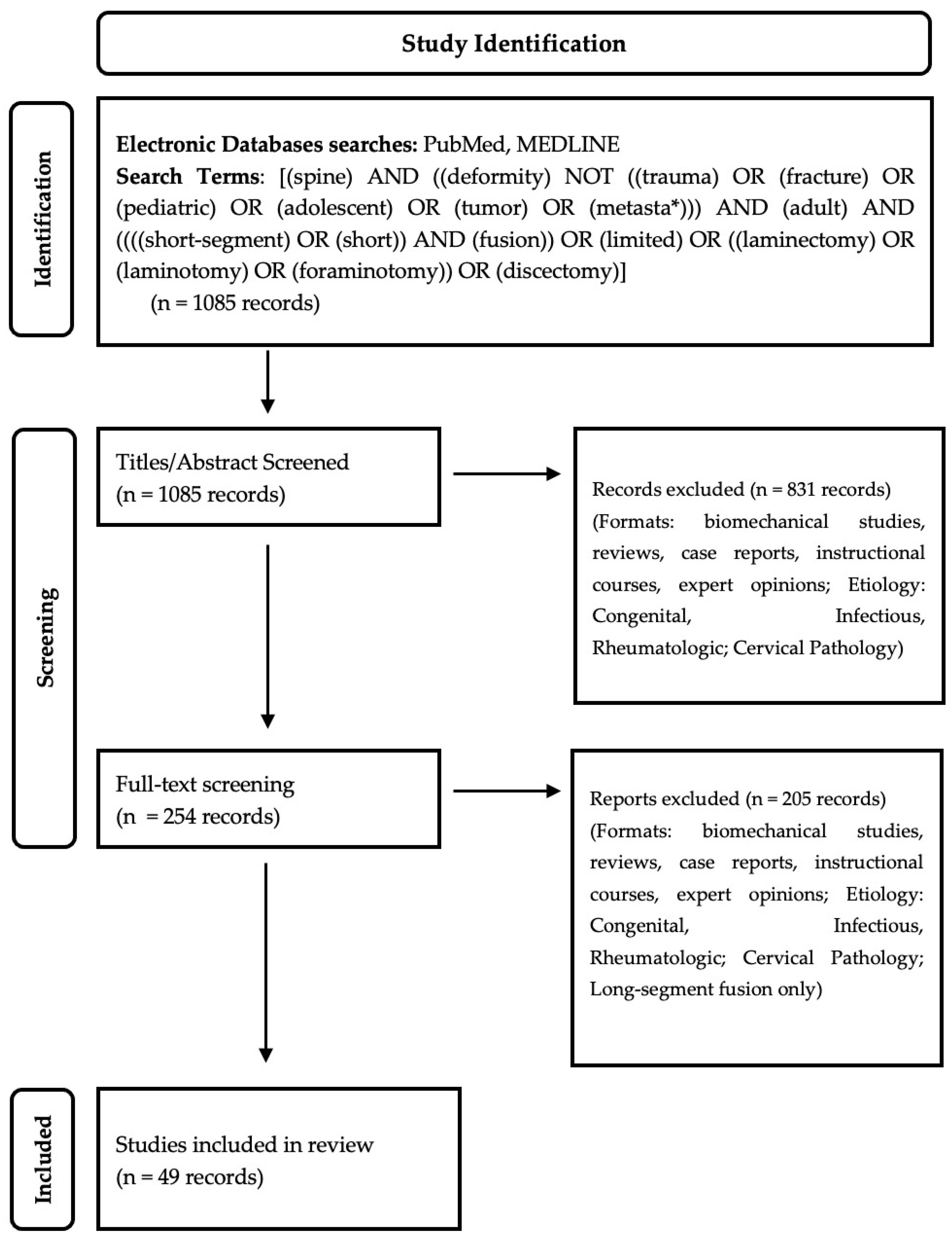
2. Materials and Methods
3. Results
3.1. Long-Segment Fusion: Advantages and Drawbacks
3.2. Patient Selection
3.3. Decompression
3.4. Fusion
3.4.1. Short-Segment Fusion: Does It Provide Relief?
3.4.2. Role in Uncompensated Spinal Deformity?
3.4.3. Fractional Curve Treatment: A Means of Foraminal Decompression
3.4.4. Short-Segment Fusion: Potential Pitfalls?
3.4.5. Interbody vs. Posterior Instrumentation Only
3.4.6. Need for Decompression?
3.5. Dynamic Stabilization—A Potential Future Option?
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nakajima, H.; Matsuo, H.; Naruse, H.; Watanabe, S.; Honjoh, K.; Shoji, K.; Kubota, A.; Matsumine, A. Clinical Impact of Short Limited Lumbar Fusion for Adult Spinal Deformity with Postural and Radiological Abnormalities. Sci. Rep. 2022, 12, 19439. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.-J.; Suk, S.-I.; Park, S.-R.; Kim, J.-H.; Kim, S.-S.; Lee, T.-J.; Lee, J.-J.; Lee, J.-M. Short Fusion versus Long Fusion for Degenerative Lumbar Scoliosis. Eur. Spine J. 2008, 17, 650–656. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Chen, X.; Jia, L.; Song, D. The Clinical Features and Surgical Treatment of Degenerative Lumbar Scoliosis: A Review of 112 Patients. Orthop. Surg. 2009, 1, 176–183. [Google Scholar] [CrossRef]
- Wang, G.; Cui, X.; Jiang, Z.; Li, T.; Liu, X.; Sun, J. Evaluation and Surgical Management of Adult Degenerative Scoliosis Associated With Lumbar Stenosis. Medicine 2016, 95, e3394. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Hawryluk, G.; Mummaneni, P.V.; Wang, M.; Mehra, R.; Wang, M.; Lau, D.; Mayer, R.; Fu, K.-M.; Chou, D. Utility of the MISDEF2 Algorithm and Extent of Fusion in Open Adult Spinal Deformity Surgery with Minimum 2-Year Follow-up. Neurospine 2021, 18, 824–832. [Google Scholar] [CrossRef]
- Song, Z.; Zhang, Z.; Yang, X.; Zhao, Z.; Li, T.; Bi, N.; Wang, Y. Mid- and Long-Term Comparison Analysis of Two Approaches for the Treatment of Level III or Higher Lenke–Silva Adult Degenerative Scoliosis: Radical or Limited Surgery? Orthop. Surg. 2022, 14, 2006–2015. [Google Scholar] [CrossRef]
- Khalifé, M.; Charles, Y.-P.; Riouallon, G.; Lafage, R.; Sabah, Y.; Marie-Hardy, L.; Guigui, P.; Zakine, S.; Ferrero, E. Lumbar Scoliosis and Stenosis: What Outcomes for Which Treatment? Analysis of Three Surgical Techniques in 154 Patients with Minimum Two-Year Follow-up. Orthop. Traumatol. Surg. Res. 2023, 103632. [Google Scholar] [CrossRef]
- Schairer, W.W.; Carrer, A.; Deviren, V.; Hu, S.S.; Takemoto, S.; Mummaneni, P.; Chou, D.; Ames, C.; Burch, S.; Tay, B.; et al. Hospital Readmission After Spine Fusion for AdultSpinal Deformity. Spine 2013, 38, 1681–1689. [Google Scholar] [CrossRef]
- Hart, R.A.; McCarthy, I.; Ames, C.P.; Shaffrey, C.I.; Hamilton, D.K.; Hostin, R. Proximal Junctional Kyphosis and Proximal Junctional Failure. Neurosurg. Clin. N. Am. 2013, 24, 213–218. [Google Scholar] [CrossRef]
- Hart, R.A.; Marshall, L.M.; Hiratzka, S.L.; Kane, M.S.; Volpi, J.; Hiratzka, J.R. Functional Limitations Due to Stiffness as a Collateral Impact of Instrumented Arthrodesis of the Lumbar Spine. Spine 2014, 39, E1468–E1474. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, R.E.; Hyde, J.; Goodrich, J.A.; Rodgers, W.B.; Phillips, F.M. A Prospective, Nonrandomized, Multicenter Evaluation of Extreme Lateral Interbody Fusion for the Treatment of Adult Degenerative Scoliosis: Perioperative Outcomes and Complications. Spine 2010, 35, S322–S330. [Google Scholar] [CrossRef]
- Pateder, D.B.; Gonzales, R.A.; Kebaish, K.M.; Cohen, D.B.; Chang, J.-Y.; Kostuik, J.P. Short-Term Mortality and Its Association With Independent Risk Factors in Adult Spinal Deformity Surgery. Spine 2008, 33, 1224–1228. [Google Scholar] [CrossRef] [PubMed]
- Frazier, D.D.; Lipson, S.J.; Fossel, A.H.; Katz, J.N. Associations Between Spinal Deformity and Outcomes After Decompression For Spinal Stenosis. Spine 1997, 22, 2025–2029. [Google Scholar] [CrossRef] [PubMed]
- Minamide, A.; Yoshida, M.; Iwahashi, H.; Simpson, A.K.; Yamada, H.; Hashizume, H.; Nakagawa, Y.; Iwasaki, H.; Tsutsui, S.; Kagotani, R.; et al. Minimally Invasive Decompression Surgery for Lumbar Spinal Stenosis with Degenerative Scoliosis: Predictive Factors of Radiographic and Clinical Outcomes. J. Orthop. Sci. 2017, 22, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Aoki, Y.; Nakajima, A.; Takahashi, H.; Sonobe, M.; Terajima, F.; Saito, M.; Takahashi, K.; Ohtori, S.; Watanabe, A.; Nakajima, T.; et al. Influence of Pelvic Incidence-Lumbar Lordosis Mismatch on Surgical Outcomes of Short-Segment Transforaminal Lumbar Interbody Fusion. BMC Musculoskelet. Disord. 2015, 16, 213. [Google Scholar] [CrossRef] [PubMed]
- Bari, T.J.; Heegaard, M.; Bech-Azeddine, R.; Dahl, B.; Gehrchen, M. Lordosis Distribution Index in Short-Segment Lumbar Spine Fusion—Can Ideal Lordosis Reduce Revision Surgery and Iatrogenic Deformity? Neurospine 2021, 18, 543–553. [Google Scholar] [CrossRef] [PubMed]
- Lugue, M.K.T.; Watanabe, K.; Yamazaki, A.; Izumi, T.; Tashi, H.; Wakasugi, M.; Katsumi, K.; Ohashi, M.; Endo, N. Impact of L4/5 Posterior Interbody Fusion With or Without Decompression on Spinopelvic Alignment and Health-Related Quality-of-Life Outcomes. Clin. Spine Surg. Spine Publ. 2020, 33, E504–E511. [Google Scholar] [CrossRef] [PubMed]
- Pugely, A.J.; Martin, C.T.; Gao, Y.; Mendoza-Lattes, S. Causes and Risk Factors for 30-Day Unplanned Readmissions After Lumbar Spine Surgery. Spine 2014, 39, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Kapetanakis, S.; Giovannopoulou, E.; Charitoudis, G.; Kazakos, K. Health-Related Quality of Life (HRQoL) Following Transforaminal Percutaneous Endoscopic Discectomy (TPED) for Lumbar Disc Herniation: A Prospective Cohort Study—Early Results. J. Back Musculoskelet. Rehabil. 2017, 30, 1311–1317. [Google Scholar] [CrossRef]
- Kim, H.S.; Kim, J.Y.; Wu, P.H.; Jang, I.-T. Effect of Dorsal Root Ganglion Retraction in Endoscopic Lumbar Decompressive Surgery for Foraminal Pathology: A Retrospective Cohort Study of Interlaminar Contralateral Endoscopic Lumbar Foraminotomy and Discectomy versus Transforaminal Endoscopic Lumbar Foraminotomy and Discectomy. World Neurosurg. 2021, 148, e101–e114. [Google Scholar] [CrossRef]
- Bai, J.; Zhang, W.; Wang, Y.; An, J.; Zhang, J.; Sun, Y.; Ding, W.; Shen, Y. Application of Transiliac Approach to Intervertebral Endoscopic Discectomy in L5/S1 Intervertebral Disc Herniation. Eur. J. Med. Res. 2017, 22, 14. [Google Scholar] [CrossRef]
- Telfeian, A.E.; Oyelese, A.; Fridley, J.; Gokaslan, Z.L. Transforaminal Endoscopic Decompression in the Setting of Lateral Lumbar Spondylolisthesis. World Neurosurg. 2018, 117, 321–325. [Google Scholar] [CrossRef]
- Madhavan, K.; Chieng, L.O.; McGrath, L.; Hofstetter, C.P.; Wang, M.Y. Early Experience with Endoscopic Foraminotomy in Patients with Moderate Degenerative Deformity. Neurosurg. Focus 2016, 40, E6. [Google Scholar] [CrossRef]
- Brodke, D.S.; Annis, P.; Lawrence, B.D.; Woodbury, A.M.; Daubs, M.D. Reoperation and Revision Rates of 3 Surgical Treatment Methods for Lumbar Stenosis Associated With Degenerative Scoliosis and Spondylolisthesis. Spine 2013, 38, 2287–2294. [Google Scholar] [CrossRef]
- Hasan, S.; McGrath, L.B.; Sen, R.D.; Barber, J.K.; Hofstetter, C.P. Comparison of Full-Endoscopic and Minimally Invasive Decompression for Lumbar Spinal Stenosis in the Setting of Degenerative Scoliosis and Spondylolisthesis. Neurosurg. Focus 2019, 46, E16. [Google Scholar] [CrossRef]
- Uribe, J.S.; Beckman, J.; Mummaneni, P.V.; Okonkwo, D.; Nunley, P.; Wang, M.Y.; Mundis, G.M., Jr.; Park, P.; Eastlack, R.; Anand, N.; et al. Does MIS Surgery Allow for Shorter Constructs in the Surgical Treatment of Adult Spinal Deformity? Neurosurgery 2017, 80, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Deukmedjian, A.R.; Ahmadian, A.; Bach, K.; Zouzias, A.; Uribe, J.S. Minimally Invasive Lateral Approach for Adult Degenerative Scoliosis: Lessons Learned. Neurosurg. Focus 2013, 35, E4. [Google Scholar] [CrossRef] [PubMed]
- Park, J.J.; Carreon, L.Y.; Glassman, S.D. Adult Lumbar Degenerative Scoliosis 40° or Less: Outcomes of Surgical Treatment with Minimum 2-Year Follow-up. Spine Deform. 2013, 1, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Tang, X.; Zhao, Y.; Song, K.; Mao, K.; Liu, H.; Wang, Z. Limited Correction of Lumbar Lordosis in the Treatment of Degenerative Scoliosis. Medicine 2020, 99, e19624. [Google Scholar] [CrossRef] [PubMed]
- Amara, D.; Mummaneni, P.V.; Ames, C.P.; Tay, B.; Deviren, V.; Burch, S.; Berven, S.H.; Chou, D. Treatment of Only the Fractional Curve for Radiculopathy in Adult Scoliosis: Comparison to Lower Thoracic and Upper Thoracic Fusions. J. Neurosurg. Spine 2019, 30, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Chou, D.; Mummaneni, P.; Anand, N.; Nunley, P.; La Marca, F.; Fu, K.-M.; Fessler, R.; Park, P.; Wang, M.; Than, K.; et al. Treatment of the Fractional Curve of Adult Scoliosis With Circumferential Minimally Invasive Surgery versus Traditional, Open Surgery: An Analysis of Surgical Outcomes. Glob. Spine J. 2018, 8, 827–833. [Google Scholar] [CrossRef]
- Kasliwal, M.K.; Smith, J.S.; Shaffrey, C.I.; Carreon, L.Y.; Glassman, S.D.; Schwab, F.; Lafage, V.; Fu, K.-M.G.; Bridwell, K.H. Does Prior Short-Segment Surgery for Adult Scoliosis Impact Perioperative Complication Rates and Clinical Outcome among Patients Undergoing Scoliosis Correction? Clinical Article. J. Neurosurg. Spine 2012, 17, 128–133. [Google Scholar] [CrossRef]
- Zurbriggen, C.; Markwalder, T.-M.; Wyss, S. Long-Term Results in Patients Treated with Posterior Instrumentation and Fusion for Degenerative Scoliosis of the Lumbar Spine. Acta Neurochir. 1999, 141, 21–26. [Google Scholar] [CrossRef]
- Feng, Y.; Chen, L.; Gu, Y.; Zhang, Z.-M.; Yang, H.-L.; Tang, T.-S. Restoration of the Spinopelvic Sagittal Balance in Isthmic Spondylolisthesis: Posterior Lumbar Interbody Fusion May Be Better than Posterolateral Fusion. Spine J. 2015, 15, 1527–1535. [Google Scholar] [CrossRef]
- Johnson, R.D.; Valore, A.; Villaminar, A.; Comisso, M.; Balsano, M. Pelvic Parameters of Sagittal Balance in Extreme Lateral Interbody Fusion for Degenerative Lumbar Disc Disease. J. Clin. Neurosci. 2013, 20, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Anand, N.; Baron, E.M.; Thaiyananthan, G.; Khalsa, K.; Goldstein, T.B. Minimally Invasive Multilevel Percutaneous Correction and Fusion for Adult Lumbar Degenerative Scoliosis: A Technique and Feasibility Study. J. Spinal Disord. Tech. 2008, 21, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, K.; Homma, T. One-Stage Three-Dimensional Correction and Fusion: A Multilevel Posterior Lumbar Interbody Fusion Procedure for Degenerative Lumbar Kyphoscoliosis: Technical Note. J. Neurosurg. Spine 2003, 99, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Dakwar, E.; Cardona, R.F.; Smith, D.A.; Uribe, J.S. Early Outcomes and Safety of the Minimally Invasive, Lateral Retroperitoneal Transpsoas Approach for Adult Degenerative Scoliosis. Neurosurg. Focus 2010, 28, E8. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-S.; Park, S.-J.; Chung, S.-S.; Lee, J.-Y.; Yum, T.-H.; Shin, S.-K. Mini-Open Anterior Lumbar Interbody Fusion Combined with Lateral Lumbar Interbody Fusion in Corrective Surgery for Adult Spinal Deformity. Asian Spine J. 2016, 10, 1023. [Google Scholar] [CrossRef] [PubMed]
- Ahlquist, S.; Park, H.Y.; Gatto, J.; Shamie, A.N.; Park, D.Y. Does Approach Matter? A Comparative Radiographic Analysis of Spinopelvic Parameters in Single-Level Lumbar Fusion. Spine J. 2018, 18, 1999–2008. [Google Scholar] [CrossRef]
- Anand, N.; Rosemann, R.; Khalsa, B.; Baron, E.M. Mid-Term to Long-Term Clinical and Functional Outcomes of Minimally Invasive Correction and Fusion for Adults with Scoliosis. Neurosurg. Focus 2010, 28, E6. [Google Scholar] [CrossRef]
- Lo, W.-L.; Lin, C.-M.; Yeh, Y.-S.; Su, Y.; Tseng, Y.-Y.; Yang, S.-T.; Lin, J.-W. Comparing Miniopen and Minimally Invasive Transforaminal Interbody Fusion in Single-Level Lumbar Degeneration. BioMed Res. Int. 2015, 2015, 168384. [Google Scholar] [CrossRef]
- Seng, C.; Siddiqui, M.A.; Wong, K.P.L.; Zhang, K.; Yeo, W.; Tan, S.B.; Yue, W.-M. Five-Year Outcomes of Minimally Invasive Versus Open Transforaminal Lumbar Interbody Fusion: A Matched-Pair Comparison Study. Spine 2013, 38, 2049–2055. [Google Scholar] [CrossRef]
- Alimi, M.; Hofstetter, C.P.; Tsiouris, A.J.; Elowitz, E.; Härtl, R. Extreme Lateral Interbody Fusion for Unilateral Symptomatic Vertical Foraminal Stenosis. Eur. Spine J. 2015, 24, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Tani, Y.; Saito, T.; Taniguchi, S.; Ishihara, M.; Paku, M.; Adachi, T.; Ando, M. Radiographic and MRI Evidence of Indirect Neural Decompression after the Anterior Column Realignment Procedure for Adult Spinal Deformity. J. Neurosurg. Spine 2022, 37, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Elsamadicy, A.A.; Adogwa, O.; Warwick, H.; Sergesketter, A.; Lydon, E.; Shammas, R.L.; Mehta, A.I.; Vasquez, R.A.; Cheng, J.; Bagley, C.A.; et al. Increased 30-Day Complication Rates Associated with Laminectomy in 874 Adult Patients with Spinal Deformity Undergoing Elective Spinal Fusion: A Single Institutional Study. World Neurosurg. 2017, 102, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Kanayama, M.; Hashimoto, T.; Shigenobu, K.; Togawa, D.; Oha, F. A Minimum 10-Year Follow-up of Posterior Dynamic Stabilization Using Graf Artificial Ligament. Spine 2007, 32, 1992–1996. [Google Scholar] [CrossRef] [PubMed]
- Di Silvestre, M.; Lolli, F.; Bakaloudis, G.; Parisini, P. Dynamic Stabilization for Degenerative Lumbar Scoliosis in Elderly Patients. Spine 2010, 35, 227–234. [Google Scholar] [CrossRef]
- Zhao, Y.; Liang, Y.; Wang, T.; Wang, Z.; Lu, N. A Hybrid Therapeutic Approach for Decreasing Postoperative Complications in Patients with Adult Lumbar Degenerative Scoliosis. Medicine 2020, 99, e21221. [Google Scholar] [CrossRef]
| Author, Year | Study Design | n | Level of Evidence | Cohort | Intervention | Findings |
|---|---|---|---|---|---|---|
| Nakajima et al., 2022 [1] | Retrospective Cohort | 26 | III | Patients with adult spinal deformity | Three-level, Two-stage limited lumbar fusion | Significant improvements in coronal Cobb angle, C7 SVA, and PI-LL mismatch |
| Cho et al., 2008 [2] | Retrospective Cohort | 50 | III | Patients with degenerative lumbar scoliosis | Short fusion VERSUS Long fusion | Significantly better coronal Cobb correction, coronal imbalance, and lateral listhesis correction in long fusion cohort; higher rates of early complications in long fusion, adjacent segment disease in short fusion; no significant difference in post-operative ODI |
| Liu et al., 2009 [3] | Retrospective Cohort | 112 | III | Patients with degenerative lumbar scoliosis | Simple nerve decompression VERSUS short fusion and decompression VERSUS long fusion and decompression | Significantly greater improvement in lumbar scoliosis and lordosis in long fusion cohort over short fusion and simple decompression cohorts; significantly greater improvement in ODI in the long fusion cohort compared to the short fusion and simple decompression cohorts; increased rates of ASD in short fusion cohort—only 53.8% of patients symptomatic |
| Wang et al., 2016 [4] | Retrospective Cohort | 108 | III | Patients with degenerative lumbar scoliosis with associated lumbar stenosis | Simple nerve decompression VERSUS short fusion and decompression VERSUS long fusion and decompression | Significant differences between cohorts in post-operative coronal C7 plumb line, sagittal C7 plumb line, and rotational olisthesis; significant difference in post-operative final ODI between cohorts |
| Li et al., 2021 [5] | Retrospective Cohort | 136 | III | Patients with adult spinal deformity | Focal decompression VERSUS short-segment fusion VERSUS full scoliosis correction | Decompression and short fusion with significantly shorter surgical duration, less blood loss, shorter hospital stay; amongst MISDEF2 Class II patients, patients undergoing full correction had significantly higher rates of perioperative complications and revision surgery |
| Song et al., 2022 [6] | Retrospective Cohort | 78 | III | Patients with adult degenerative scoliosis | Short-segment limited fixation VERSUS long-segment radical fixation | No significant differences between cohorts in long-term complications and re-operations; long-segment group had significantly better coronal Cobb, lumbar lordosis, and sagittal balance; long-segment group had significantly higher implant-related complications |
| Khalifé et al., 2023 [7] | Prospective Cohort | 154 | IV | Patients with scoliosis and lumbar stenosis | Lumbar decompression VERSUS short fusion and decompression VERSUS long fusion with deformity correction | Long fusion cohort with significant improvement in ODI, VAS, SF-12, SRS-30 scores at 2 years; significant increases noted in fractional curve Cobb in short fusion and C7 coronal tilt in decompression cohorts; long fusion had highest overall complication rates and revision rates |
| Schairer et al., 2013 [8] | Retrospective Cohort | 836 | III | Patients with adult spinal deformity | Spine fusion | Higher rates of readmission in patients with long fusion; risk factors for readmission were longer fusion length, higher illness severity, and medical comorbidities |
| Hart et al., 2013 [9] | Cross-Sectional | 93 | III | Patients who previously underwent lumbar spine fusion | Lumbar spine fusion | LSDI scores significantly different between 1-level and 5-level arthrodesis group; LSDI and ODI significantly correlated |
| Hart et al., 2014 [10] | Prospective Cohort | 62 | II | Patients with lumbar degenerative disease or spinal deformity | Lumbar spine fusion | All cohorts saw significant decreases in ODI following surgery; patients undergoing 1-level and 5+-level surgery saw significant improvements in physical composite score; patients with 1-level fusion saw significant decrease in LSDI; 3, 4, and 5+-level saw nonsignificant increase in LSDI |
| Isaacs et al., 2010 [11] | Prospective Cohort | 107 | IV | Patients with degenerative scoliosis | Extreme lateral interbody fusion ± posterior fixation | 12.1% major complication rate, which compares favorably to previous literature |
| Pateder et al., 2008 [12] | Retrospective Cohort | 361 | III | Patients with spinal deformity | Deformity correction | Strong association between ASA score and mortality; no association between levels of fusion and mortality |
| Frazier et al., 1997 [13] | Prospective Cohort | 90 | IV | Patients with spinal deformity and spinal stenosis | Laminectomy | Pre-operative scoliosis is associated with decreased improvement in back pain following laminectomy |
| Minamide et al., 2017 [14] | Prospective Cohort | 122 | III | Patients with degenerative lumbar scoliosis with associated lumbar stenosis | Microendoscopic laminectomy or foraminotomy | Significant improvement in VAS-low back pain; clinical outcomes in foraminal stenosis related to pre-op Cobb angle and scoliosis progression |
| Aoki et al., 2015 [15] | Retrospective Cohort | 52 | III | Patients with degenerative lumbar disease | 1 or 2 level TLIF | Significant correlation between post-operative PI-LL mismatch and VAS scores for low back pain, lower extremity pain, and numbness |
| Bari et al., 2021 [16] | Retrospective Cohort | 149 | III | Patients with degenerative lumbar disease | Fusion surgery ≤ 4 levels | Hypolordotic group had increased odds of 1-year revision surgery; linear correlation between pre-operative pelvic incidence and post-operative lordosis distribution |
| Lugue et al., 2020 [17] | Retrospective Case-Control | 119 | III | Patients with degenerative lumbar disease | L4/L5 PLIF | Significant increase in local lordosis, correlated with increase in lumbar lordosis; high PI-LL and SVA cohorts had decreased clinical outcomes |
| Pugely et al., 2014 [18] | Prospective Cohort | 15,668 | III | Patients undergoing lumbar spine surgery | Lumbar spine surgery | Lowest risk of readmission with discectomy and highest risk with deformity surgery |
| Kapetanakis et al., 2017 [19] | Prospective Cohort | 76 | III | Patients with lumbar disc herniation | Percutaneous transforaminal endoscopic discectomy | Significant improvements seen in all domains of SF-36 scores |
| Kim et al., 2021 [20] | Retrospective Cohort | 100 | IV | Patients with lumbar disc herniation | transforaminal endoscopic lumbar foraminotomy and discectomy VERSUS interlaminar contralateral endoscopic lumbar foraminotomy and discectomy | Interlaminar approach associated with reduced rates of post-operative dysesthesia; both cohorts had favorable clinical outcomes |
| Bai et al., 2017 [21] | Prospective Cohort | 39 | III | Patients with lumbar disc herniation | Inter-vertebral approach VERSUS trans-iliac approach | No significant differences in operative time and post-operative VAS scores between the cohorts |
| Telfeian et al., 2018 [22] | Case Series | 4 | IV | Patients with lumbar disc herniation in setting of lateral lumbar listhesis | Percutaneous transforaminal endoscopic discectomy | Most patients saw improvements in ODI and VAS sustained for 1 year follow-up |
| Madhavan et al., 2016 [23] | Retrospective Cohort | 16 | III | Patients with scoliotic deformity and unilateral radicular pain secondary to foraminal stenosis | Endoscopic foraminal decompression surgery | Significant improvement in VAS for radicular leg pain post-operatively |
| Brodke et al., 2013 [24] | Retrospective Cohort | 90 | III | Patients with lumbar stenosis in setting of spinal deformity | Interspinous spacer VERSUS laminectomy only VERSUS laminectomy and short-segment fusion | Significantly higher recurrence rate in interspinous spacer cohort; laminectomy alone cohort had highest 5-year survival on Kaplan-Meier analysis |
| Hasan et al., 2019 [25] | Prospective Cohort | 45 | III | Patients with degenerative spinal deformity with associated lumbar stenosis | Full-endoscopic VERSUS minimally invasive unilateral laminotomy for bilateral decompression | Endoscopic cohort had significantly shorter hospital stay, lower adverse events, and improved early ODI scores |
| Uribe et al., 2017 [26] | Retrospective Cohort | 84 | III | Patients undergoing adult spinal deformity correction | Minimally invasive VERSUS open approaches | MIS cohort had shorter construct lengths, lower blood loss, and shorter hospital length of stay |
| Deukmedjian et al., 2013 [27] | Retrospective Cohort | 27 | III | Patients who underwent surgical correction of adult degenerative scoliosis | Lumbar interbody fusion with augmentation dependent on deformity severity | Most cohorts showed improvements in radiographic and clinical outcomes; patients who were undertreated did not show significant improvements |
| Park et al., 2013 [28] | Retrospective Cohort | 105 | IV | Patients with adult lumbar degenerative scoliosis with a coronal Cobb angle of <40° | Decompression and instrumented fusion | Significant improvements noted in ODI, SF-36, and VAS scores post-operatively |
| Liang et al., 2020 [29] | Retrospective Cohort | 58 | III | Patients with adult degenerative scoliosis | Deformity correction surgery | Patients with limited correction in setting of sagittal imbalance had significantly worse radiographic outcomes but demonstrated no significant differences in coronal Cobb angles, ODI, or VAS |
| Amara et al., 2019 [30] | Retrospective Cohort | 99 | III | Patients with adult scoliosis | Fractional curve limited fusion VERSUS instrumentation to lower thoracic spine VERSUS instrumentation to upper thoracic spine | Fractional curve treatment with significantly lower rates of medical complications, lower blood loss, shorter hospital stays, and reduced discharge to acute rehab; Significantly increased risk of extension surgery |
| Chou et al., 2018 [31] | Retrospective Cohort | 118 | III | Patients with adult scoliosis | Minimally invasive VERSUS open fractional curve correction | MIS approach with significantly less instrumented and decompressed levels; similar clinical outcomes in both cohorts |
| Kasliwal et al., 2012 [32] | Retrospective Cohort | 60 | III | Patients with previous short-segment fusion for adult scoliosis VERSUS patients undergoing initial operation | Scoliosis deformity correction | No significant differences in complications, perioperative morbidity/mortality, and clinical outcomes |
| Zurbriggen et al., 1999 [33] | Case series | 40 | IV | Patients with degenerative lumbar scoliosis | Posterior instrumentation and fusion | Improvements seen in radiographic and clinical outcomes following surgical intervention |
| Feng et al., 2015 [34] | Prospective Cohort | 159 | III | Patients with isthmic spondylolisthesis | Posterolateral fusion VERSUS Posterior lumbar interbody fusion | PLIF better at augmenting lumbar lordosis and aiding with the restoration of spinopelvic parameters |
| Johnson et al., 2013 [35] | Retrospective Cohort | 22 | III | Patients with degenerative lumbar disc disease | Extreme lateral interbody fusion | Significant improvements in segmental lordosis, scoliotic Cobb angle, and clinical outcomes |
| Anand et al., 2008 [36] | Retrospective Cohort | 12 | IV | Patients with degenerative lumbar scoliosis | Circumferential MIS fusion of deformity | Post-operative improvements seen in coronal Cobb angle, VAS score, and TIS score. |
| Hasegawa and Homma 2003 [37] | Case Series | 23 | IV | Patients with degenerative lumbar kyphoscoliosis | Multi-level posterior lumbar interbody fusion | Significant improvements in JOA score, Cobb angle, and torsional deformity noted post-operatively |
| Dakwar et al., 2010 [38] | Retrospective Cohort | 25 | IV | Patients with adult degenerative deformity | Lateral interbody fusion via transpsoas approach | VAS and ODI improvements seen post-operatively |
| Lee et al., 2016 [39] | Prospective Cohort | 32 | III | Patients with adult degenerative deformity | Lateral and Anterior lumbar interbody fusion with posterior fixation | ALIF levels with greater post-op segmental lordosis compared to LLIF levels; also noted greater increase in segmental lordosis; sagittal parameters all improved post-operatively; see worse parameters at follow-up, but still improved compared to pre-op |
| Ahlquist et al., 2018 [40] | Retrospective Cohort | 164 | III | Patients undergoing lumbar fusion | Anterior VERSUS Lateral VERSUS transforaminal VERSUS posterior lumbar interbody fusion | ALIF and LLIF with significant improvements in segmental lordosis, anterior and posterior disc heights, and foraminal height; ALIF and LLIF outperformed PLIF in improvements seen post-op; ALIF only technique to significantly increase proportion of PI-LL < 10° |
| Anand et al., 2010 [41] | Retrospective Cohort | 28 | IV | Patients with adult scoliosis | Minimally invasive correction of deformity, 3+ levels | Improvements in VAS, TIS, ODI, and SF-36 scores; lower perioperative morbidity |
| Lo et al., 2015 [42] | Retrospective Cohort | 973 | III | Patients with adult degenerative deformity | Single-level fusion | Mini-Open and MIS with lower EBL, VAS, LOS, and infections; longer surgery time for both |
| Seng et al., 2013 [43] | Retrospective Cohort | 80 | III | Patients with adult degenerative deformity | Open VERSUS minimally invasive transforaminal lumbar interbody fusion | Perioperative variables—MIS had higher fluoroscopic time, less blood loss and morphine usage, and less time to ambulation and less LOS; all groups with significant improvements in patient-reported outcomes—no significant differences between groups; all groups with significant fusion by 5 years—open TLIF had nonsignificantly higher rates within 6 months and 2 years |
| Alimi et al., 2015 [44] | Retrospective Cohort | 23 | III | Patients with single-level unilateral vertical foraminal stenosis with radicular pain | Single-level extreme lateral interbody fusion | Significant increases in foraminal height and disc height; significant decrease in coronal Cobb, VAS-Leg, VAS-Buttock, and VAS-Back |
| Tani et al., 2022 [45] | Retrospective Cohort | 36 | III | Patients with adult spinal deformity | Anterior column reconstruction, lateral lumbar interbody fusion, and percutaneous pedicle screw fixation | Patients had significantly increased lumbar lordosis, thoracic kyphosis, and segmental disc angles after intervention; significantly decreased PI-LL and spino-vertebral angle; significant increases in disc heights, foraminal height, and cross-sectional area; decreases in ligamentum flavum thickness and disc bulge thickness; significant decrease in ODI |
| Elsamadicy et al., 2017 [46] | Retrospective cohort | 874 | III | Patients with adult spinal deformity | Spinal fusion alone VERSUS spinal fusion with laminectomy | Laminectomy cohort with increased blood loss, blood transfusions, and durotomies intra-op; higher rate of ICU post-op |
| Kanayama et al., 2007 [47] | Retrospective cohort | 56 | III | Patients with adult spinal deformity | Graf ligamentoplasty | No significant differences in segmental lordosis—see a reduction in range of motion at the operative level; significant improvement in JOA scores from pre-op to follow-up. Unfavorable outcomes in degenerative scoliosis and lateral listhesis |
| Di Silvestre et al., 2010 [48] | Retrospective cohort | 29 | III | Patients with adult spinal deformity | Dynamic Stabilization without fusion | Significant improvements in ODI, RDQ, and VAS Back and Leg; significant improvements in scoliosis, Cobb angle, lateral listhesis, and anterior vertebral translation |
| Zhao et al., 2020 [49] | Retrospective cohort | 16 | III | Patients with adult lumbar degenerative scoliosis | Short-segment decompression and fusion WITH proximal segment stabilization | Significant changes seen in radiographic measures as well as in VAS Back + Leg and ODI |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammed, Z.J.; Worley, J.; Hiatt, L.; Rajaram Manoharan, S.R.; Theiss, S. Limited Intervention in Adult Scoliosis—A Systematic Review. J. Clin. Med. 2024, 13, 1030. https://doi.org/10.3390/jcm13041030
Mohammed ZJ, Worley J, Hiatt L, Rajaram Manoharan SR, Theiss S. Limited Intervention in Adult Scoliosis—A Systematic Review. Journal of Clinical Medicine. 2024; 13(4):1030. https://doi.org/10.3390/jcm13041030
Chicago/Turabian StyleMohammed, Zuhair Jameel, John Worley, Luke Hiatt, Sakthivel Rajan Rajaram Manoharan, and Steven Theiss. 2024. "Limited Intervention in Adult Scoliosis—A Systematic Review" Journal of Clinical Medicine 13, no. 4: 1030. https://doi.org/10.3390/jcm13041030
APA StyleMohammed, Z. J., Worley, J., Hiatt, L., Rajaram Manoharan, S. R., & Theiss, S. (2024). Limited Intervention in Adult Scoliosis—A Systematic Review. Journal of Clinical Medicine, 13(4), 1030. https://doi.org/10.3390/jcm13041030








