Metabolic Disorders in Liver Transplant Recipients: The State of the Art
Abstract
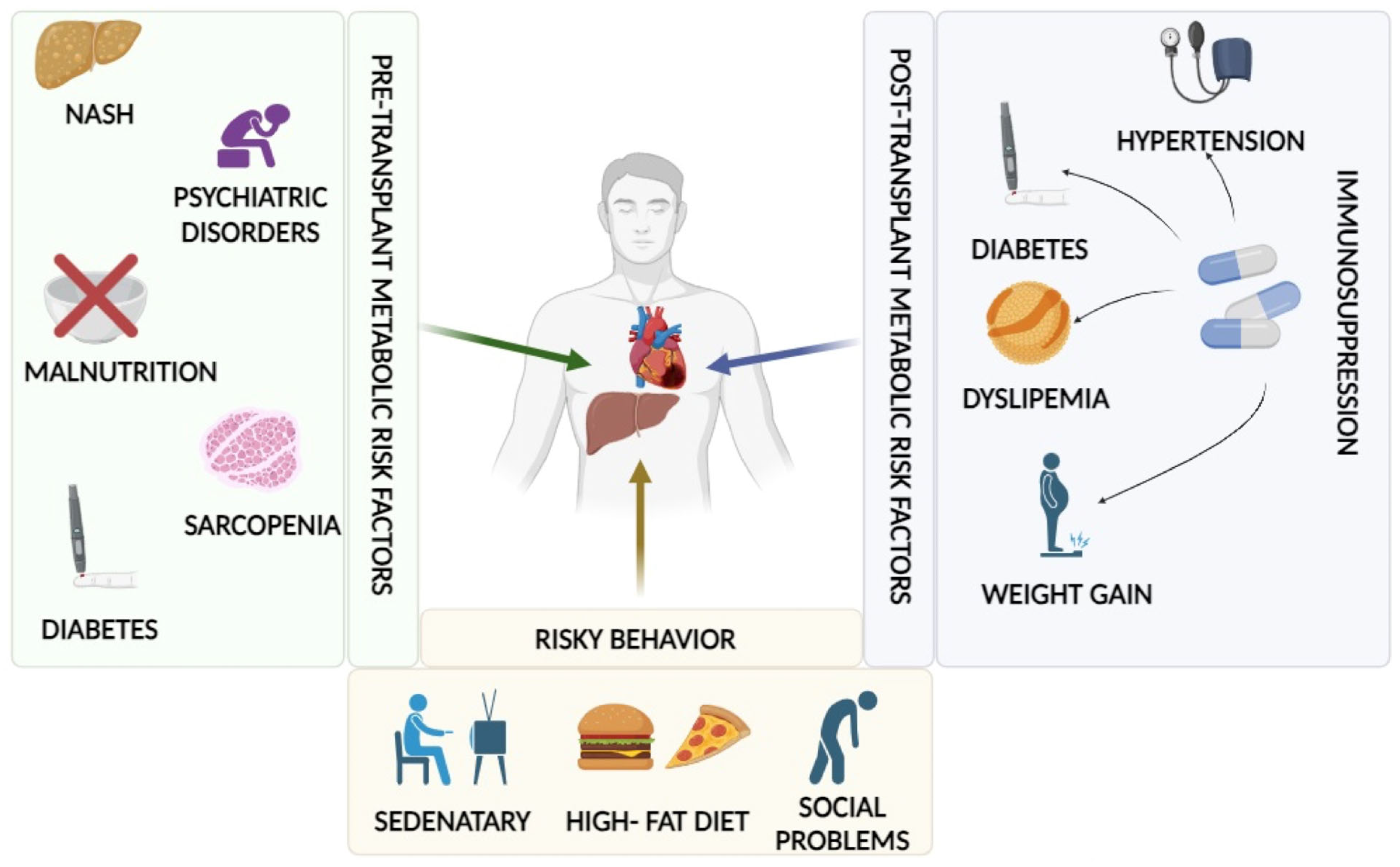
1. Introduction
2. Materials and Methods
3. Metabolic Disorders
3.1. Arterial Hypertension
3.2. Dyslipidemia
3.3. Diabetes Mellitus
3.4. Metabolic Syndrome
3.5. De Novo and Recurrent MASL
4. Post-Transplant Lifestyle
5. Innovative Approaches
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Serrano, M.T.; Sabroso, S.; Esteban, L.M.; Berenguer, M.; Fondevila, C.; Lorente, S.; Cortés, L.; Sanchez-Antolin, G.; Nuño, J.; De la Rosa, G.; et al. Mortality and Causes of Death After Liver Transplantation: Analysis of Sex Differences in a Large Nationwide Cohort. Transpl. Int. 2022, 35, 10263. [Google Scholar] [CrossRef] [PubMed]
- Pfitzmann, R.; Nüssler, N.C.; Hippler-Benscheidt, M.; Neuhaus, R.; Neuhaus, P. Long-Term Results after Liver Transplantation. Transpl. Int. 2008, 21, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Salizzoni, M.; Cerutti, E.; Romagnoli, R.; Lupo, F.; Franchello, A.; Zamboni, F.; Gennari, F.; Strignano, P.; Ricchiuti, A.; Brunati, A.; et al. The First One Thousand Liver Transplants in Turin: A Single-Center Experience in Italy. Transpl. Int. 2005, 18, 1328–1335. [Google Scholar] [CrossRef] [PubMed]
- Watt, K.D.S.; Pedersen, R.A.; Kremers, W.K.; Heimbach, J.K.; Charlton, M.R. Evolution of Causes and Risk Factors for Mortality Post-Liver Transplant: Results of the NIDDK Long-Term Follow-up Study. Am. J. Transplant. 2010, 10, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Bhat, M.; Mara, K.; Dierkhising, R.; Watt, K.D. Gender, Race and Disease Etiology Predict De Novo Malignancy Risk After Liver Transplantation: Insights for Future Individualized Cancer Screening Guidance. Transplantation 2019, 103, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Goodrich, N.P.; Bragg-Gresham, J.L.; Dykstra, D.M.; Punch, J.D.; DebRoy, M.A.; Greenstein, S.M.; Merion, R.M. Characteristics Associated with Liver Graft Failure: The Concept of a Donor Risk Index. Am. J. Transplant. 2006, 6, 783–790. [Google Scholar] [CrossRef]
- Kwong, A.J.; Ebel, N.H.; Kim, W.R.; Lake, J.R.; Smith, J.M.; Schladt, D.P.; Schnellinger, E.M.; Handarova, D.; Weiss, S.; Cafarella, M.; et al. OPTN/SRTR 2021 Annual Data Report: Liver. Available online: https://srtr.transplant.hrsa.gov/annual_reports/2021/Liver.aspx (accessed on 22 January 2024).
- Stepanova, M.; Kabbara, K.; Mohess, D.; Verma, M.; Roche-Green, A.; AlQahtani, S.; Ong, J.; Burra, P.; Younossi, Z.M. Nonalcoholic Steatohepatitis Is the Most Common Indication for Liver Transplantation among the Elderly: Data from the United States Scientific Registry of Transplant Recipients. Hepatol. Commun. 2022, 6, 1506–1515. [Google Scholar] [CrossRef] [PubMed]
- Simon, T.G.; Roelstraete, B.; Khalili, H.; Hagström, H.; Ludvigsson, J.F. Mortality in Biopsy-Confirmed Nonalcoholic Fatty Liver Disease: Results from a Nationwide Cohort. Gut 2021, 70, 1375–1382. [Google Scholar] [CrossRef]
- Angulo, P.; Kleiner, D.E.; Dam-Larsen, S.; Adams, L.A.; Bjornsson, E.S.; Charatcharoenwitthaya, P.; Mills, P.R.; Keach, J.C.; Lafferty, H.D.; Stahler, A.; et al. Liver Fibrosis, but No Other Histologic Features, Is Associated with Long-Term Outcomes of Patients with Nonalcoholic Fatty Liver Disease. Gastroenterology 2015, 149, 389–397.e10. [Google Scholar] [CrossRef]
- Vilar-Gomez, E.; Calzadilla-Bertot, L.; Wai-Sun Wong, V.; Castellanos, M.; Aller-de la Fuente, R.; Metwally, M.; Eslam, M.; Gonzalez-Fabian, L.; Alvarez-Quiñones Sanz, M.; Conde-Martin, A.F.; et al. Fibrosis Severity as a Determinant of Cause-Specific Mortality in Patients with Advanced Nonalcoholic Fatty Liver Disease: A Multi-National Cohort Study. Gastroenterology 2018, 155, 443–457.e17. [Google Scholar] [CrossRef]
- Haflidadottir, S.; Jonasson, J.G.; Norland, H.; Einarsdottir, S.O.; Kleiner, D.E.; Lund, S.H.; Björnsson, E.S. Long-Term Follow-up and Liver-Related Death Rate in Patients with Non-Alcoholic and Alcoholic Related Fatty Liver Disease. BMC Gastroenterol. 2014, 14, 166. [Google Scholar] [CrossRef] [PubMed]
- Nasr, P.; Ignatova, S.; Kechagias, S.; Ekstedt, M. Natural History of Nonalcoholic Fatty Liver Disease: A Prospective Follow-up Study with Serial Biopsies. Hepatol. Commun. 2018, 2, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Hagström, H.; Nasr, P.; Ekstedt, M.; Hammar, U.; Stål, P.; Hultcrantz, R.; Kechagias, S. Fibrosis Stage but Not NASH Predicts Mortality and Time to Development of Severe Liver Disease in Biopsy-Proven NAFLD. J. Hepatol. 2017, 67, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Mak, L.-Y.; Chan, A.C.; Wong, T.C.; Dai, W.-C.; She, W.-H.; Ma, K.-W.; Sin, S.-L.; Chu, K.-W.; Seto, W.-K.; Yuen, M.-F.; et al. High Prevalence of de Novo Metabolic Dysfunction-Associated Fatty Liver Disease after Liver Transplantation and the Role of Controlled Attenuation Parameter. BMC Gastroenterol. 2023, 23, 307. [Google Scholar] [CrossRef]
- Gitto, S.; Golfieri, L.; Gabrielli, F.; Falcini, M.; Sofi, F.; Tamè, M.R.; De Maria, N.; Marzi, L.; Mega, A.; Valente, G.; et al. Physical Activity in Liver Transplant Recipients: A Large Multicenter Study. Intern. Emerg. Med. 2023. [Google Scholar] [CrossRef] [PubMed]
- Taneja, S.; Roy, A.; Duseja, A. NASH After Liver Transplantation: Impact of Immunosuppression. J. Clin. Exp. Hepatol. 2023, 13, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, L.S.; Alfie, J.; Barochiner, J.; Cuffaro, P.E.; Rada, M.; Galarza, C.; Waisman, G.D.; Morales, M. Hypertension: The Neglected Complication of Transplantation. Int. Sch. Res. Not. 2013, 2013, 165937. [Google Scholar] [CrossRef]
- Lim, W.H.; Tan, C.; Xiao, J.; Tan, D.J.H.; Ng, C.H.; Yong, J.N.; Fu, C.; Chan, K.E.; Zeng, R.W.; Ren, Y.P.; et al. De Novo Metabolic Syndrome after Liver Transplantation: A Meta-Analysis on Cumulative Incidence, Risk Factors, and Outcomes. Liver Transplant. 2023, 29, 413–421. [Google Scholar] [CrossRef]
- Lemos, B.d.O.; Silva, R.d.C.M.A.; da Silva, R.F. Prevalence and time of development of systemic arterial hypertension in patients after liver transplantation. Arq. Gastroenterol. 2021, 58, 77–81. [Google Scholar] [CrossRef]
- Kuramitsu, K.; Fukumoto, T.; Iwasaki, T.; Tominaga, M.; Matsumoto, I.; Ajiki, T.; Ku, Y. Long-Term Complications after Liver Transplantation. Transplant. Proc. 2014, 46, 797–803. [Google Scholar] [CrossRef]
- Pérez, M.J.; García, D.M.; Taybi, B.J.; Daga, J.A.P.; Rey, J.M.L.; Grande, R.G.; Lombardo, J.D.L.C.; López, J.M.R. Cardiovascular Risk Factors after Liver Transplantation: Analysis of Related Factors. Transplant. Proc. 2011, 43, 739–741. [Google Scholar] [CrossRef]
- Hryniewiecka, E.; Zegarska, J.; Paczek, L. Arterial Hypertension in Liver Transplant Recipients. Transplant. Proc. 2011, 43, 3029–3034. [Google Scholar] [CrossRef]
- Parekh, J.; Corley, D.A.; Feng, S. Diabetes, Hypertension and Hyperlipidemia: Prevalence over Time and Impact on Long-Term Survival after Liver Transplantation. Am. J. Transplant. 2012, 12, 2181–2187. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, C.; Vanni, E.; Mirabella, S.; Younes, R.; Boano, V.; Mosso, E.; Nada, E.; Milazzo, V.; Maule, S.; Romagnoli, R.; et al. Risk Factors for Arterial Hypertension after Liver Transplantation. J. Am. Soc. Hypertens. 2018, 12, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Tong, M.-S.; Chai, H.-T.; Liu, W.-H.; Chen, C.-L.; Fu, M.; Lin, Y.-H.; Lin, C.-C.; Chen, S.-M.; Hang, C.-L. Prevalence of Hypertension after Living-Donor Liver Transplantation: A Prospective Study. Transplant. Proc. 2015, 47, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Reis, F.; Parada, B.; Teixeira de Lemos, E.; Garrido, P.; Dias, A.; Piloto, N.; Baptista, S.; Sereno, J.; Eufrásio, P.; Costa, E.; et al. Hypertension Induced by Immunosuppressive Drugs: A Comparative Analysis between Sirolimus and Cyclosporine. Transplant. Proc. 2009, 41, 868–873. [Google Scholar] [CrossRef] [PubMed]
- Lucey, M.R.; Terrault, N.; Ojo, L.; Hay, J.E.; Neuberger, J.; Blumberg, E.; Teperman, L.W. Long-Term Management of the Successful Adult Liver Transplant: 2012 Practice Guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Liver Transplant. 2013, 19, 3–26. [Google Scholar] [CrossRef] [PubMed]
- Neal, D.A.J.; Brown, M.J.; Wilkinson, I.B.; Byrne, C.D.; Alexander, G.J.M. Hemodynamic Effects of Amlodipine, Bisoprolol, and Lisinopril in Hypertensive Patients after Liver Transplantation. Transplantation 2004, 77, 748–750. [Google Scholar] [CrossRef]
- Gitto, S.; Falcini, M.; Marra, F. MEDITRA Research Group Metabolic Disorders After Liver Transplantation. Metab. Syndr. Relat. Disord. 2021, 19, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Gisbert, C.; Prieto, M.; Berenguer, M.; Bretó, M.; Carrasco, D.; de Juan, M.; Mir, J.; Berenguer, J. Hyperlipidemia in Liver Transplant Recipients: Prevalence and Risk Factors. Liver Transplant. Surg. 1997, 3, 416–422. [Google Scholar] [CrossRef]
- Neal, D.A.; Tom, B.D.; Luan, J.A.; Wareham, N.J.; Gimson, A.E.; Delriviere, L.D.; Byrne, C.D.; Alexander, G.J. Is There Disparity between Risk and Incidence of Cardiovascular Disease after Liver Transplant? Transplantation 2004, 77, 93–99. [Google Scholar] [CrossRef]
- Hüsing, A.; Kabar, I.; Schmidt, H.H. Lipids in Liver Transplant Recipients. World J. Gastroenterol. 2016, 22, 3315–3324. [Google Scholar] [CrossRef] [PubMed]
- Mártinez, J.M.A.; Pulido, L.B.; Bellido, C.B.; Usero, D.D.; Aguilar, L.T.; Moreno, J.L.G.; Artacho, G.S.; Díez-Canedo, J.S.; Gómez, L.M.M.; Bravo, M.Á.G. Rescue Immunosuppression with Mammalian Target. of Rapamycin Inhibitor Drugs in Liver Transplantation. Transplant. Proc. 2010, 42, 641–643. [Google Scholar] [CrossRef] [PubMed]
- Saliba, F.; Dharancy, S.; Lorho, R.; Conti, F.; Radenne, S.; Neau-Cransac, M.; Hurtova, M.; Hardwigsen, J.; Calmus, Y.; Dumortier, J. Conversion to Everolimus in Maintenance Liver Transplant Patients: A Multicenter, Retrospective Analysis. Liver Transplant. 2011, 17, 905–913. [Google Scholar] [CrossRef] [PubMed]
- Berg, A.L.; Nilsson-Ehle, P. ACTH Lowers Serum Lipids in Steroid-Treated Hyperlipemic Patients with Kidney Disease. Kidney Int. 1996, 50, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Becker, D.M.; Chamberlain, B.; Swank, R.; Hegewald, M.G.; Girardet, R.; Baughman, K.L.; Kwiterovich, P.O.; Pearson, T.A.; Ettinger, W.H.; Renlund, D. Relationship between Corticosteroid Exposure and Plasma Lipid Levels in Heart Transplant Recipients. Am. J. Med. 1988, 85, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Artz, M.A.; Boots, J.M.M.; Ligtenberg, G.; Roodnat, J.I.; Christiaans, M.H.L.; Vos, P.F.; Blom, H.J.; Sweep, F.C.G.J.; Demacker, P.N.M.; Hilbrands, L.B. Improved Cardiovascular Risk Profile and Renal Function in Renal Transplant Patients after Randomized Conversion from Cyclosporine to Tacrolimus. J. Am. Soc. Nephrol. 2003, 14, 1880–1888. [Google Scholar] [CrossRef] [PubMed]
- Keogh, A.; Macdonald, P.; Harvison, A.; Richens, D.; Mundy, J.; Spratt, P. Initial Steroid-Free versus Steroid-Based Maintenance Therapy and Steroid Withdrawal after Heart Transplantation: Two Views of the Steroid Question. J. Heart Lung Transplant. 1992, 11, 421–427. [Google Scholar] [PubMed]
- Manzarbeitia, C.; Reich, D.J.; Rothstein, K.D.; Braitman, L.E.; Levin, S.; Munoz, S.J. Tacrolimus Conversion Improves Hyperlipidemic States in Stable Liver Transplant Recipients. Liver Transplant. 2001, 7, 93–99. [Google Scholar] [CrossRef]
- Vincenti, F.; Friman, S.; Scheuermann, E.; Rostaing, L.; Jenssen, T.; Campistol, J.M.; Uchida, K.; Pescovitz, M.D.; Marchetti, P.; Tuncer, M.; et al. Results of an International, Randomized Trial Comparing Glucose Metabolism Disorders and Outcome with Cyclosporine versus Tacrolimus. Am. J. Transplant. 2007, 7, 1506–1514. [Google Scholar] [CrossRef]
- Morrisett, J.D.; Abdel-Fattah, G.; Kahan, B.D. Sirolimus Changes Lipid Concentrations and Lipoprotein Metabolism in Kidney Transplant Recipients. Transplant. Proc. 2003, 35, 143S–150S. [Google Scholar] [CrossRef]
- Ricoult, S.J.H.; Manning, B.D. The Multifaceted Role of mTORC1 in the Control of Lipid Metabolism. EMBO Rep. 2013, 14, 242–251. [Google Scholar] [CrossRef]
- Claes, K.; Meier-Kriesche, H.-U.; Schold, J.D.; Vanrenterghem, Y.; Halloran, P.F.; Ekberg, H. Effect of Different Immunosuppressive Regimens on the Evolution of Distinct Metabolic Parameters: Evidence from the Symphony Study. Nephrol. Dial. Transplant. 2012, 27, 850–857. [Google Scholar] [CrossRef] [PubMed]
- Murakami, N.; Riella, L.V.; Funakoshi, T. Risk of Metabolic Complications in Kidney Transplantation after Conversion to mTOR Inhibitor: A Systematic Review and Meta-Analysis. Am. J. Transplant. 2014, 14, 2317–2327. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.W. Cardiovascular Toxicities of Immunosuppressive Agents. Am. J. Transplant. 2002, 2, 807–818. [Google Scholar] [CrossRef] [PubMed]
- European Association for The Study of the Liver. EASL Clinical Practice Guidelines: Liver Transplantation. J. Hepatol. 2016, 64, 433–485. [Google Scholar] [CrossRef] [PubMed]
- Authors/Task Force Members; ESC Committee for Practice Guidelines (CPG). ESC National Cardiac Societies 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias: Lipid Modification to Reduce Cardiovascular Risk. Atherosclerosis 2019, 290, 140–205. [Google Scholar] [CrossRef] [PubMed]
- Page, R.L.; Miller, G.G.; Lindenfeld, J. Drug Therapy in the Heart Transplant Recipient: Part IV: Drug-Drug Interactions. Circulation 2005, 111, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Gazi, I.F.; Liberopoulos, E.N.; Athyros, V.G.; Elisaf, M.; Mikhailidis, D.P. Statins and Solid Organ Transplantation. Curr. Pharm. Des. 2006, 12, 4771–4783. [Google Scholar] [CrossRef]
- Shaw, S.M.; Chaggar, P.; Ritchie, J.; Shah, M.K.H.; Baynes, A.C.; O’Neill, N.; Fildes, J.E.; Yonan, N.; Williams, S.G. The Efficacy and Tolerability of Ezetimibe in Cardiac Transplant Recipients Taking Cyclosporin. Transplantation 2009, 87, 771–775. [Google Scholar] [CrossRef]
- Almutairi, F.; Peterson, T.C.; Molinari, M.; Walsh, M.J.; Alwayn, I.; Peltekian, K.M. Safety and Effectiveness of Ezetimibe in Liver Transplant Recipients with Hypercholesterolemia. Liver Transplant. 2009, 15, 504–508. [Google Scholar] [CrossRef]
- Rosenson, R.S.; Hegele, R.A.; Fazio, S.; Cannon, C.P. The Evolving Future of PCSK9 Inhibitors. J. Am. Coll. Cardiol. 2018, 72, 314–329. [Google Scholar] [CrossRef] [PubMed]
- Warden, B.A.; Kaufman, T.; Minnier, J.; Duell, P.B.; Fazio, S.; Shapiro, M.D. Use of PCSK9 Inhibitors in Solid Organ Transplantation Recipients. JACC Case Rep. 2020, 2, 396–399. [Google Scholar] [CrossRef] [PubMed]
- Reiner, Z. Managing the Residual Cardiovascular Disease Risk Associated with HDL-Cholesterol and Triglycerides in Statin-Treated Patients: A Clinical Update. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Zein, N.N.; Abdulkarim, A.S.; Wiesner, R.H.; Egan, K.S.; Persing, D.H. Prevalence of Diabetes Mellitus in Patients with End-Stage Liver Cirrhosis Due to Hepatitis C, Alcohol, or Cholestatic Disease. J. Hepatol. 2000, 32, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Asrani, S.K.; Saracino, G.; O’Leary, J.G.; Gonzalez, S.; Kim, P.T.; McKenna, G.J.; Klintmalm, G.; Trotter, J. Recipient Characteristics and Morbidity and Mortality after Liver Transplantation. J. Hepatol. 2018, 69, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, J.; Riaz, D.R.; Shi, G.; Liu, C.; Dai, Y. Outcomes of Liver Transplantation for Nonalcoholic Steatohepatitis: A Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2014, 12, 394–402.e1. [Google Scholar] [CrossRef] [PubMed]
- Jenssen, T.; Hartmann, A. Post-Transplant Diabetes Mellitus in Patients with Solid Organ Transplants. Nat. Rev. Endocrinol. 2019, 15, 172–188. [Google Scholar] [CrossRef]
- Dungan, K.M.; Braithwaite, S.S.; Preiser, J.-C. Stress Hyperglycaemia. Lancet 2009, 373, 1798–1807. [Google Scholar] [CrossRef]
- American Diabetes Association. 15. Diabetes Care in the Hospital: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44, S211–S220. [Google Scholar] [CrossRef]
- Sharif, A.; Hecking, M.; de Vries, A.P.J.; Porrini, E.; Hornum, M.; Rasoul-Rockenschaub, S.; Berlakovich, G.; Krebs, M.; Kautzky-Willer, A.; Schernthaner, G.; et al. Proceedings from an International Consensus Meeting on Posttransplantation Diabetes Mellitus: Recommendations and Future Directions. Am. J. Transplant. 2014, 14, 1992–2000. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.-C.; Lin, J.-R.; Chen, H.-P.; Tsai, Y.-F.; Yu, H.-P. Prevalence, Predictive Factors, and Survival Outcome of New-Onset Diabetes after Liver Transplantation: A Population-Based Cohort Study. Medicine 2016, 95, e3829. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Stepanova, M.; Saab, S.; Kalwaney, S.; Clement, S.; Henry, L.; Frost, S.; Hunt, S. The Impact of Type 2 Diabetes and Obesity on the Long-Term Outcomes of More than 85 000 Liver Transplant Recipients in the US. Aliment. Pharmacol. Ther. 2014, 40, 686–694. [Google Scholar] [CrossRef]
- Brodosi, L.; Petta, S.; Petroni, M.L.; Marchesini, G.; Morelli, M.C. Management of Diabetes in Candidates for Liver Transplantation and in Transplant Recipients. Transplantation 2022, 106, 462–478. [Google Scholar] [CrossRef] [PubMed]
- Roccaro, G.A.; Goldberg, D.S.; Hwang, W.-T.; Judy, R.; Thomasson, A.; Kimmel, S.E.; Forde, K.A.; Lewis, J.D.; Yang, Y.-X. Sustained Posttransplantation Diabetes Is Associated with Long-Term Major Cardiovascular Events Following Liver Transplantation. Am. J. Transplant. 2018, 18, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, P. New-Onset Diabetes after Liver Transplantation: From Pathogenesis to Management. Liver Transplant. 2005, 11, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Saliba, F.; Lakehal, M.; Pageaux, G.-P.; Roche, B.; Vanlemmens, C.; Duvoux, C.; Dumortier, J.; Salamé, E.; Calmus, Y.; Maugendre, D.; et al. Risk Factors for New-Onset Diabetes Mellitus Following Liver Transplantation and Impact of Hepatitis C Infection: An Observational Multicenter Study. Liver Transplant. 2007, 13, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Heit, J.J.; Apelqvist, A.A.; Gu, X.; Winslow, M.M.; Neilson, J.R.; Crabtree, G.R.; Kim, S.K. Calcineurin/NFAT Signalling Regulates Pancreatic Beta-Cell Growth and Function. Nature 2006, 443, 345–349. [Google Scholar] [CrossRef]
- Rodriguez-Rodriguez, A.E.; Triñanes, J.; Velazquez-Garcia, S.; Porrini, E.; Vega Prieto, M.J.; Diez Fuentes, M.L.; Arevalo, M.; Salido Ruiz, E.; Torres, A. The Higher Diabetogenic Risk of Tacrolimus Depends on Pre-Existing Insulin Resistance: A Study in Obese and Lean Zucker Rats. Am. J. Transplant. 2013, 13, 1665–1675. [Google Scholar] [CrossRef]
- Odenwald, M.A.; Roth, H.F.; Reticker, A.; Segovia, M.; Pillai, A. Evolving Challenges with Long-Term Care of Liver Transplant Recipients. Clin. Transplant. 2023, 37, e15085. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45, S83–S96. [Google Scholar] [CrossRef]
- Zhang, Z.-J.; Zheng, Z.-J.; Shi, R.; Su, Q.; Jiang, Q.; Kip, K.E. Metformin for Liver Cancer Prevention in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2012, 97, 2347–2353. [Google Scholar] [CrossRef] [PubMed]
- Vanhove, T.; Remijsen, Q.; Kuypers, D.; Gillard, P. Drug-Drug Interactions between Immunosuppressants and Antidiabetic Drugs in the Treatment of Post-Transplant Diabetes Mellitus. Transplant. Rev. 2017, 31, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Sweiss, H.; Selznick, L.; Contreras, J.; Long, C.; Hall, R.; Bhayana, S.; Patel, R.; Klein, K. Safety and Efficacy of Sodium-Glucose Cotransporter-2 Inhibitors in Solid Organ Transplant Recipients. Prog. Transplant. 2023, 33, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Mok, M.; Harrison, J.; Battistella, M.; Farrell, A.; Leung, M.; Cheung, C. Use of Sodium-Glucose Co-Transporter 2 Inhibitors in Solid Organ Transplant Recipients with Pre-Existing Type 2 or Post-Transplantation Diabetes Mellitus: A Systematic Review. Transplant. Rev. 2023, 37, 100729. [Google Scholar] [CrossRef] [PubMed]
- Neumiller, J.J.; Wood, L.; Campbell, R.K. Dipeptidyl Peptidase-4 Inhibitors for the Treatment of Type 2 Diabetes Mellitus. Pharmacotherapy 2010, 30, 463–484. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.; Lee, M.J.; Choe, E.Y.; Jung, C.H.; Wang, H.J.; Kim, M.S.; Kim, Y.S.; Park, J.Y.; Kang, E.S. Effects of Dipeptidyl Peptidase-4 Inhibitors on Hyperglycemia and Blood Cyclosporine Levels in Renal Transplant Patients with Diabetes: A Pilot Study. Endocrinol. Metab. 2016, 31, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Soliman, A.R.; Fathy, A.; Khashab, S.; Shaheen, N.; Soliman, M.A. Sitagliptin Might Be a Favorable Antiobesity Drug for New Onset Diabetes after a Renal Transplant. Exp. Clin. Transplant. 2013, 11, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Spiritos, Z.; Abdelmalek, M.F. Metabolic Syndrome Following Liver Transplantation in Nonalcoholic Steatohepatitis. Transl. Gastroenterol. Hepatol. 2021, 6, 13. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, e285–e290. [Google Scholar] [CrossRef]
- Yang, C.; Jia, X.; Wang, Y.; Fan, J.; Zhao, C.; Yang, Y.; Shi, X. Trends and Influence Factors in the Prevalence, Intervention, and Control of Metabolic Syndrome among US Adults, 1999–2018. BMC Geriatr. 2022, 22, 979. [Google Scholar] [CrossRef] [PubMed]
- Laish, I.; Braun, M.; Mor, E.; Sulkes, J.; Harif, Y.; Ben Ari, Z. Metabolic Syndrome in Liver Transplant Recipients: Prevalence, Risk Factors, and Association with Cardiovascular Events. Liver Transplant. 2011, 17, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Graziadei, I.W.; Cárdenas, A. Cardiovascular Diseases after Liver Transplantation—A Still Emerging and Unsolved Problem! Liver Transplant. 2015, 21, 870–872. [Google Scholar] [CrossRef] [PubMed]
- Dadlani, A.; Lee, T.-H. Management of Metabolic Syndrome after Liver Transplant. Clin. Liver Dis. 2023, 21, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.W.-S.; Dufour, J.-F.; Schattenberg, J.M.; et al. A New Definition for Metabolic Dysfunction-Associated Fatty Liver Disease: An International Expert Consensus Statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.; Anstee, Q.M.; Marietti, M.; Hardy, T.; Henry, L.; Eslam, M.; George, J.; Bugianesi, E. Global Burden of NAFLD and NASH: Trends, Predictions, Risk Factors and Prevention. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Han, M.A.T.; Olivo, R.; Choi, C.J.; Pyrsopoulos, N. De Novo and Recurrence of Metabolic Dysfunction-Associated Fatty Liver Disease after Liver Transplantation. World J. Hepatol. 2021, 13, 1991–2004. [Google Scholar] [CrossRef] [PubMed]
- Villeret, F.; Dharancy, S.; Erard, D.; Abergel, A.; Barbier, L.; Besch, C.; Boillot, O.; Boudjema, K.; Coilly, A.; Conti, F.; et al. Inevitability of Disease Recurrence after Liver Transplantation for NAFLD Cirrhosis. JHEP Rep. 2023, 5, 100668. [Google Scholar] [CrossRef]
- Silva, A.C.; Nogueira, P.; Machado, M.V. Hepatic Steatosis after Liver Transplantation: A Systematic Review and Meta-Analysis. Liver Transplant. 2023, 29, 431–448. [Google Scholar] [CrossRef]
- Narayanan, P.; Mara, K.; Izzy, M.; Dierkhising, R.; Heimbach, J.; Allen, A.M.; Watt, K.D. Recurrent or De Novo Allograft Steatosis and Long-Term Outcomes After Liver Transplantation. Transplantation 2019, 103, e14–e21. [Google Scholar] [CrossRef]
- Gitto, S.; Mannelli, N.; Tassi, A.; Gabrielli, F.; Nascimbeni, F.; Andreone, P. Liver Transplantation and Nonalcoholic Steatohepatitis: The State of the Art. Metab. Target. Organ. Damage 2022, 2, 7. [Google Scholar] [CrossRef]
- Beekman, L.; Berzigotti, A.; Banz, V. Physical Activity in Liver Transplantation: A Patient’s and Physicians’ Experience. Adv. Ther. 2018, 35, 1729–1734. [Google Scholar] [CrossRef] [PubMed]
- Krasnoff, J.B.; Vintro, A.Q.; Ascher, N.L.; Bass, N.M.; Paul, S.M.; Dodd, M.J.; Painter, P.L. A Randomized Trial of Exercise and Dietary Counseling after Liver Transplantation. Am. J. Transplant. 2006, 6, 1896–1905. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.E.; Lombardero, M.; Lake, J.R.; Wiesner, R.H.; Zetterman, R.K.; Hoofnagle, J.H. Weight Change and Obesity after Liver Transplantation: Incidence and Risk Factors. Liver Transplant. Surg. 1998, 4, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Nurwanti, E.; Uddin, M.; Chang, J.-S.; Hadi, H.; Syed-Abdul, S.; Su, E.C.-Y.; Nursetyo, A.A.; Masud, J.H.B.; Bai, C.-H. Roles of Sedentary Behaviors and Unhealthy Foods in Increasing the Obesity Risk in Adult Men and Women: A Cross-Sectional National Study. Nutrients 2018, 10, 704. [Google Scholar] [CrossRef] [PubMed]
- Kallwitz, E.R.; Loy, V.; Mettu, P.; Von Roenn, N.; Berkes, J.; Cotler, S.J. Physical Activity and Metabolic Syndrome in Liver Transplant Recipients. Liver Transplant. 2013, 19, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Mosconi, G.; Cuna, V.; Tonioli, M.; Totti, V.; Roi, G.S.; Sarto, P.; Stefoni, S.; Trerotola, M.; Costa, A.N. Physical Activity in Solid Organ Transplant Recipients: Preliminary Results of the Italian Project. Kidney Blood Press. Res. 2014, 39, 220–227. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: At A Glance. Available online: https://www.who.int/europe/publications/i/item/9789240014886 (accessed on 23 January 2024).
- Pérez-Amate, È.; Roqué-Figuls, M.; Fernández-González, M.; Giné-Garriga, M. Exercise Interventions for Adults after Liver Transplantation. Cochrane Database Syst. Rev. 2023, 5, CD013204. [Google Scholar] [CrossRef]
- Anastácio, L.R.; Davisson Correia, M.I.T. Nutrition Therapy: Integral Part of Liver Transplant Care. World J. Gastroenterol. 2016, 22, 1513–1522. [Google Scholar] [CrossRef]
- Sugihara, K.; Yamanaka-Okumura, H.; Teramoto, A.; Urano, E.; Katayama, T.; Morine, Y.; Imura, S.; Utsunomiya, T.; Shimada, M.; Takeda, E. Recovery of Nutritional Metabolism after Liver Transplantation. Nutrition 2015, 31, 105–110. [Google Scholar] [CrossRef]
- Plauth, M.; Cabré, E.; Campillo, B.; Kondrup, J.; Marchesini, G.; Schütz, T.; Shenkin, A.; Wendon, J. ESPEN ESPEN Guidelines on Parenteral Nutrition: Hepatology. Clin. Nutr. 2009, 28, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, A.J.; Aranda-Michel, J. Nutrition for the Liver Transplant Patient. Liver Transplant. 2006, 12, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Rezende Anastácio, L.; García Ferreira, L.; Costa Liboredo, J.; de Sena Ribeiro, H.; Soares Lima, A.; García Vilela, E.; Correia, M.I.T.D. Overweight, Obesity and Weight Gain up to Three Years after Liver Transplantation. Nutr. Hosp. 2012, 27, 1351–1356. [Google Scholar] [CrossRef] [PubMed]
- Kouz, J.; Vincent, C.; Leong, A.; Dorais, M.; Räkel, A. Weight Gain after Orthotopic Liver Transplantation: Is Nonalcoholic Fatty Liver Disease Cirrhosis a Risk Factor for Greater Weight Gain? Liver Transplant. 2014, 20, 1266–1274. [Google Scholar] [CrossRef] [PubMed]
- Hammad, A.; Kaido, T.; Aliyev, V.; Mandato, C.; Uemoto, S. Nutritional Therapy in Liver Transplantation. Nutrients 2017, 9, 1126. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Lista, J.; Alcala-Diaz, J.F.; Torres-Peña, J.D.; Quintana-Navarro, G.M.; Fuentes, F.; Garcia-Rios, A.; Ortiz-Morales, A.M.; Gonzalez-Requero, A.I.; Perez-Caballero, A.I.; Yubero-Serrano, E.M.; et al. Long-Term Secondary Prevention of Cardiovascular Disease with a Mediterranean Diet and a Low-Fat Diet (CORDIOPREV): A Randomised Controlled Trial. Lancet 2022, 399, 1876–1885. [Google Scholar] [CrossRef] [PubMed]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean Diet and Multiple Health Outcomes: An Umbrella Review of Meta-Analyses of Observational Studies and Randomised Trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Gitto, S.; Golfieri, L.; Sofi, F.; Tamè, M.R.; Vitale, G.; DE Maria, N.; Marzi, L.; Mega, A.; Valente, G.; Borghi, A.; et al. Adherence to Mediterranean Diet in Liver Transplant Recipients: A Cross-Sectional Multicenter Study. Minerva Gastroenterol. 2023. [Google Scholar] [CrossRef]
- Sainz-Barriga, M.; Baccarani, U.; Scudeller, L.; Risaliti, A.; Toniutto, P.L.; Costa, M.G.; Ballestrieri, M.; Adani, G.L.; Lorenzin, D.; Bresadola, V.; et al. Quality-of-Life Assessment Before and After Liver Transplantation. Transplant. Proc. 2005, 37, 2601–2604. [Google Scholar] [CrossRef]
- Varshney, M.; Dhingra, K.; Choudhury, A. Psychosocial Assessment and Management-Related Issues Among Liver Transplant Recipients. J. Clin. Exp. Hepatol. 2024, 14, 101261. [Google Scholar] [CrossRef]
- Bonkovsky, H.L.; Snow, K.K.; Malet, P.F.; Back-Madruga, C.; Fontana, R.J.; Sterling, R.K.; Kulig, C.C.; Di Bisceglie, A.M.; Morgan, T.R.; Dienstag, J.L.; et al. Health-Related Quality of Life in Patients with Chronic Hepatitis C and Advanced Fibrosis. J. Hepatol. 2007, 46, 420–431. [Google Scholar] [CrossRef][Green Version]
- Magistri, P.; Marzi, L.; Guerzoni, S.; Vandelli, M.; Mereu, F.; Ascari, F.; Guidetti, C.; Tarantino, G.; Serra, V.; Guerrini, G.P.; et al. Impact of a Multidisciplinary Team on Alcohol Recidivism and Survival After Liver Transplant for Alcoholic Disease. Transplant. Proc. 2019, 51, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Rogal, S.S.; Dew, M.A.; Fontes, P.; DiMartini, A.F. Early Treatment of Depressive Symptoms and Long-Term Survival After Liver Transplantation. Am. J. Transplant. 2013, 13, 928–935. [Google Scholar] [CrossRef] [PubMed]
- Golfieri, L.; Gitto, S.; Vukotic, R.; Andreone, P.; Marra, F.; Morelli, M.C.; Cescon, M.; Grandi, S. Impact of Psychosocial Status on Liver Transplant Process. Ann. Hepatol. 2019, 18, 804–809. [Google Scholar] [CrossRef] [PubMed]
- Ordin, Y.S.; Karayurt, Ö. Effects of a Support Group Intervention on Physical, Psychological, and Social Adaptation of Liver Transplant Recipients. Exp. Clin. Transplant. 2016, 14, 329–337. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Febrero, B.; Ramírez, P.; Martínez-Alarcón, L.; Abete, C.; Galera, M.; Ríos, A.; Robles-Martínez, R.; Ramírez-Pino, P.M.; Almela, J.; Ramis, G.; et al. Group Psychotherapy Could Improve Depression in Cirrhotic Patients on the Liver Transplant Waiting List. Transplant. Proc. 2019, 51, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Costa, E.G.; Colussi, G.; Meneguzzi, C.; Grazioli, S.; Tonizzo, M. Group Therapy for Alcohol Addiction Treatment before Liver Transplantation Reduces Post-Transplant Alcohol Relapse: Preliminary Results of a Monocentric Retrospective Study. Dig. Liver Dis. 2023, 55, S54. [Google Scholar] [CrossRef]
- Rodrigue, J.R.; Nelson, D.R.; Hanto, D.W.; Reed, A.I.; Curry, M.P. Patient-Reported Immunosuppression Nonadherence 6 to 24 Months after Liver Transplant: Association with Pretransplant Psychosocial Factors and Perceptions of Health Status Change. Prog. Transplant. 2013, 23, 319–328. [Google Scholar] [CrossRef]
- Goetzmann, L.; Moser, K.S.; Vetsch, E.; Klaghofer, R.; Naef, R.; Russi, E.W.; Buddeberg, C.; Boehler, A. How Does Psychological Processing Relate to Compliance Behaviour after Lung Transplantation? A Content Analytical Study. Psychol. Health Med. 2007, 12, 94–106. [Google Scholar] [CrossRef]
- Goetzinger, A.M.; Blumenthal, J.A.; O’Hayer, C.V.; Babyak, M.A.; Hoffman, B.M.; Ong, L.; Davis, R.D.; Smith, S.R.; Rogers, J.G.; Milano, C.A.; et al. Stress and Coping in Caregivers of Patients Awaiting Solid Organ Transplantation. Clin. Transplant. 2012, 26, 97–104. [Google Scholar] [CrossRef]
- Boscarino, J.A.; Lu, M.; Moorman, A.C.; Gordon, S.C.; Rupp, L.B.; Spradling, P.R.; Teshale, E.H.; Schmidt, M.A.; Vijayadeva, V.; Holmberg, S.D.; et al. Predictors of Poor Mental and Physical Health Status among Patients with Chronic Hepatitis C Infection: The Chronic Hepatitis Cohort Study (CHeCS). Hepatology 2015, 61, 802–811. [Google Scholar] [CrossRef]
- Cipolletta, S.; Entilli, L.; Nucci, M.; Feltrin, A.; Germani, G.; Cillo, U.; Volpe, B. Psychosocial Support in Liver Transplantation: A Dyadic Study with Patients and Their Family Caregivers. Front. Psychol. 2019, 10, 2304. [Google Scholar] [CrossRef]
| METABOLIC DISORDER | PHARMACOLOGICAL APPROACHES | LIFESTYLE CHANGES | REF. |
|---|---|---|---|
| ARTERIAL HYPERTENSION | Calcium channel blockers | [28,29,30] | |
| Selective beta-receptor blockers | Weight loss if necessary | ||
| Angiotensin-converting enzyme inhibitors | Increased physical activity | ||
| Angiotensin II receptor blockers | Reduction in sodium intake | ||
| Loop diuretics | |||
| DYSLIPIDEMIA | Statin | [48,49,50,51,52,54,55] | |
| Ezetimibe | Weight loss if necessary | ||
| Fibrates | Increased physical activity | ||
| iPCSK9 | Balanced diet | ||
| Icosapent ethyl | |||
| T2 DIABETES MELLITUS | Biguanides | [72,73,75,76,78,79] | |
| GLP1-RAs | Weight loss if necessary | ||
| SGLT-2i | Increased physical activity | ||
| DPP-4i | Hypoglycemic diet | ||
| Insulin | |||
| MASL | Addressing the altered metabolic factor | Weight loss if necessary | [99] |
| No approved medications | Increased physical activity |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gabrielli, F.; Golfieri, L.; Nascimbeni, F.; Andreone, P.; Gitto, S. Metabolic Disorders in Liver Transplant Recipients: The State of the Art. J. Clin. Med. 2024, 13, 1014. https://doi.org/10.3390/jcm13041014
Gabrielli F, Golfieri L, Nascimbeni F, Andreone P, Gitto S. Metabolic Disorders in Liver Transplant Recipients: The State of the Art. Journal of Clinical Medicine. 2024; 13(4):1014. https://doi.org/10.3390/jcm13041014
Chicago/Turabian StyleGabrielli, Filippo, Lucia Golfieri, Fabio Nascimbeni, Pietro Andreone, and Stefano Gitto. 2024. "Metabolic Disorders in Liver Transplant Recipients: The State of the Art" Journal of Clinical Medicine 13, no. 4: 1014. https://doi.org/10.3390/jcm13041014
APA StyleGabrielli, F., Golfieri, L., Nascimbeni, F., Andreone, P., & Gitto, S. (2024). Metabolic Disorders in Liver Transplant Recipients: The State of the Art. Journal of Clinical Medicine, 13(4), 1014. https://doi.org/10.3390/jcm13041014







