Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al-Moraissi, E.A.; Ellis, E. Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: A systematic review and meta-analysis. J. Oral Maxillofac. Surg. 2015, 73, 482–493. [Google Scholar] [CrossRef]
- Chrcanovic, B.R. Surgical versus non-surgical treatment of mandibular condylar fractures: A meta-analysis. J. Oral Maxillofac. Surg. 2015, 44, 158–179. [Google Scholar] [CrossRef]
- Kozakiewicz, M.; Walczyk, A. Current Frequency of Mandibular Condylar Process Fractures. J. Clin. Med. 2023, 12, 1394. [Google Scholar] [CrossRef] [PubMed]
- Durmuş Kocaaslan, N.; Karadede Ünal, B.; Çavuş Özkan, M.; Karadede, B.; Çelebiler, Ö. Comparison of different treatment techniques in the mandibular condyle fracture. Turk. J. Trauma Emerg. Surg. 2022, 28, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Zhou, J.; Li, Z. Contrast analysis of open reduction and internal fixation and non-surgical treatment of condylar fracture: A meta-analysis. J. Craniofac. Surg. 2014, 25, 2077–2080. [Google Scholar] [CrossRef] [PubMed]
- Shiju, M.; Rastogi, S.; Gupta, P.; Kukreja, S.; Thomas, R.; Bhugra, A.K.; Parvatha Reddy, M.; Choudhury, R. Fractures of the mandibular condyle—Open versus closed—A treatment dilemma. J. Craniomaxillofac. Surg. 2015, 43, 448–451. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Neff, A.; Kaur, A.; Falci, S.G.M.; de Souza, G.M.; Ellis, E. Treatment for Adult Mandibular Condylar Process Fractures: A Network Meta-Analysis of Randomized Clinical Trials. J. Oral Maxillofac. Surg. 2023, 81, 1252–1269. [Google Scholar] [CrossRef] [PubMed]
- Karan, A.; Kedarnath, N.S.; Reddy, G.S.; Harish Kumar, T.V.S.; Neelima, C.; Bhavani, M.; Nayyar, A.S. Condylar Fractures: Surgical Versus Conservative Management. Ann. Maxillofac. Surg. 2019, 9, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M. Złamania Wyrostka Kłykciowego Żuchwy; PZWL: Warszawa, Poland, 2019; ISBN 978-83-200-5778-2. [Google Scholar]
- Shakya, S.; Zhang, X.; Liu, L. Key points in surgical management of mandibular condylar fractures. Chin. J. Traumatol. 2020, 23, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.kronosedm.pl/tytan-r56401/ (accessed on 27 October 2023).
- ASTMF 1839-08; Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments. ASTM International: West Conshohocken, PA, USA, 2016.
- Assari, S.; Darvish, K.; Ilyas, A.M. Biomechanical analysis of second-generation headless compression screws. Injury 2012, 43, 1159–1165. [Google Scholar] [CrossRef]
- Baran, O.; Sagol, E.; Oflaz, H.; Sarikanat, M.; Havitcioglu, H. A biomechanical study on preloaded compression effect on headless screws. Arch. Orthop. Trauma. Surg. 2009, 129, 1601–1605. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, R.; Evans, S.; Kosashvili, Y. Holding power of variable pitch screws in osteoporotic, osteopenic and normal bone: Are all screws created equal? Injury 2010, 41, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.A.; Kuiper, J.H.; Kelly, C.P. Biomechanical Evaluation of a New Composite Bioresorbable Screw. J. Hand Surg. 2006, 31, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Okulski, J.; Krasowski, M.; Konieczny, B.; Zieliński, R. Which of 51 Plate Designs Can Most Stably Fixate the Fragments in a Fracture of the Mandibular Condyle Base? J. Clin. Med. 2023, 12, 4508. [Google Scholar] [CrossRef] [PubMed]
- Mittermiller, P.A.; Bidwell, S.S.; Thieringer, F.M.; Cornelius, C.P.; Trickey, A.W.; Kontio, R.; Girod, S.; AO Trauma Classification Study Group. The Comprehensive AO CMF Classification System for Mandibular Fractures: A Multicenter Validation Study. Craniomaxillofac. Trauma Reconstr. 2019, 12, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Zieliński, R.; Krasowski, M.; Okulski, J. Forces Causing One-Millimeter Displacement of Bone Fragments of Condylar Base Fractures of the Mandible after Fixation by All Available Plate Designs. Materials 2019, 12, 3122. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, R.; Kozakiewicz, M.; Konieczny, B.; Krasowski, M.; Okulski, J. Mechanical Evaluation of Titanium Plates for Osteoesynthesis High Neck Condylar Fracture of Mandible. Materials 2020, 13, 592. [Google Scholar] [CrossRef]
- Goldstein, S. The mechanical properties of trabecular bone: Dependence on anatomic location and function. J. Biomech. 1987, 20, 1055–1061. [Google Scholar] [CrossRef]
- Chapman, J.R.; Harrington, R.M.; Lee, K.M.; Anderson, P.A.; Tencer, A.F.; Kowalski, D. Factors Affecting the Pullout Strength of Cancellous Bone Screws. J. Biomech. Eng. 1996, 118, 391–398. [Google Scholar] [CrossRef]
- Schindeler, A.; Mills, R.J.; Bobyn, J.D.; Little, D.G. Preclinical models for orthopedic research and bone tissue engineering. J. Orthop. Res. 2018, 36, 832–840. [Google Scholar] [CrossRef]
- Cutcliffe, H.C.; DeFrate, L.E. Four-Point Bending Testing for Mechanical Assessment of Mouse Bone Structural Properties. Methods Mol. Biol. 2021, 2230, 199–215. [Google Scholar] [CrossRef]
- Alkan, A.; Metin, M.; Muğlali, M.; Ozden, B.; Celebi, N. Biomechanical comparison of plating techniques for fractures of the mandibular condyle. Br. J. Oral Maxillofac. Surg. 2007, 45, 145–149. [Google Scholar] [CrossRef]
- Pilling, E.; Eckelt, U.; Loukota, R.; Schneider, K.; Stadlinger, B. Comparative evaluation of ten different condylar base fracture osteosynthesis techniques. Br. J. Oral Maxillofac. Surg. 2010, 48, 527–531. [Google Scholar] [CrossRef]
- Kot, C.C.S.; Verstraete, F.J.M.; Garcia, T.C.; Stover, S.M.; Arzi, B. Biomechanical evaluation of locking versus nonlocking 2.0-mm malleable L-miniplate fixation of simulated caudal mandibular fractures in cats. Am. J. Vet Res. 2022, 83, ajvr.22.03.0043. [Google Scholar] [CrossRef]
- Olivera, L.B.; Sant’ Ana, E.; Manzato, A.J.; Guerra, F.L.; Arnett, G.W. Biomechanical in vitro evaluation of three stable internal fixation techniques used in sagittal osteotomy of the mandibular ramus: A study in sheep mandibles. J. Appl. Oral Sci. 2012, 20, 419–426. [Google Scholar] [CrossRef]
- Cheng, C.K.; Wang, X.H.; Luan, Y.C.; Zhang, N.Z.; Liu, B.L.; Ma, X.Y.; Nie, M.D. Challenges of pre-clinical testing in orthopedic implant development. Med. Eng. Phys. 2019, 72, 49–54. [Google Scholar] [CrossRef]
- Marturello, D.M.; Wei, F.; Déjardin, L.M. Characterization of the torsional structural properties of feline femurs and surrogate bone models for mechanical testing of orthopedic implants. Vet Surg. 2019, 48, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Sikora, M.; Chęciński, M.; Nowak, Z.; Chęcińska, K.; Olszowski, T.; Chlubek, D. The Use of Titanium 3D Mini-Plates in the Surgical Treatment of Fractures of the Mandibular Condyle: A Systematic Review and Meta-Analysis of Clinical Trials. J. Clin. Med. 2021, 10, 3604. [Google Scholar] [CrossRef] [PubMed]
- Agnihotry, A.; Fedorowicz, Z.; Nasser, M.; Gill, K.S. Resorbable versus titanium plates for orthognathic surgery. Cochrane Database Syst. Rev. 2017, 10, CD006204. [Google Scholar] [CrossRef] [PubMed]
- Dorri, M.; Oliver, R. WITHDRAWN: Resorbable versus titanium plates for facial fractures. Cochrane Database Syst. Rev. 2018, 5, CD007158. [Google Scholar] [CrossRef] [PubMed]
- Fuessinger, M.A.; Gass, M.; Woelm, C.; Cornelius, C.P.; Zimmerer, R.M.; Poxleitner, P.; Schlager, S.; Metzger, M.C. Analyzing the Fitting of Novel Preformed Osteosynthesis Plates for the Reduction and Fixation of Mandibular Fractures. J. Clin. Med. 2021, 10, 5975. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Kawamata, S.; Suzuki, S.; Ishikawa, Y.; Ikeda, Y.; Yasuge, E.; Kogi, S.; Ogawa, A.; Izumisawa, M.; Yamada, H. Condyle Fracture Fixed with Custom-Made Titanium Mesh and a Miniplate: A Case Report. Am. J. Case Rep. 2023, 24, e940681. [Google Scholar] [CrossRef] [PubMed]


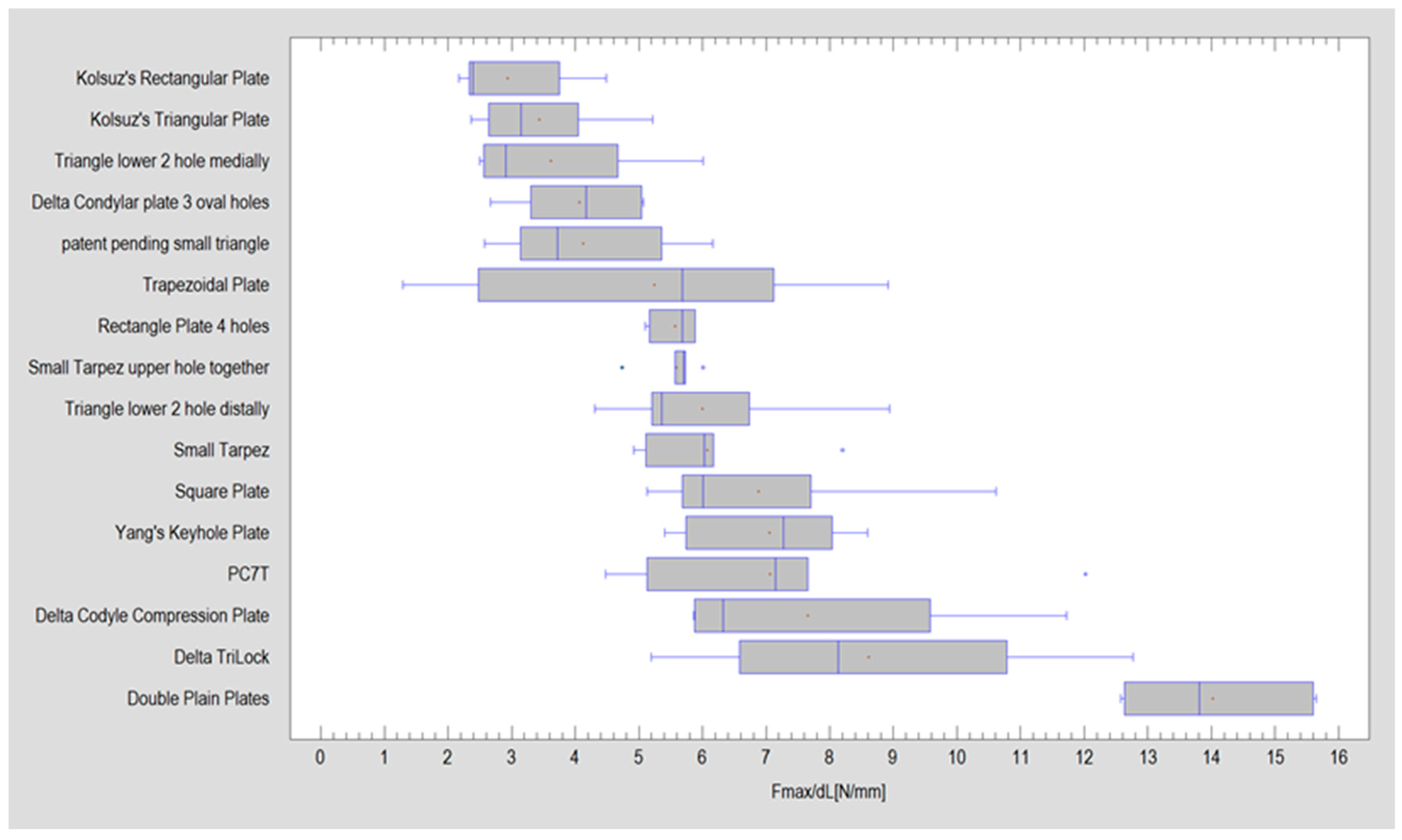
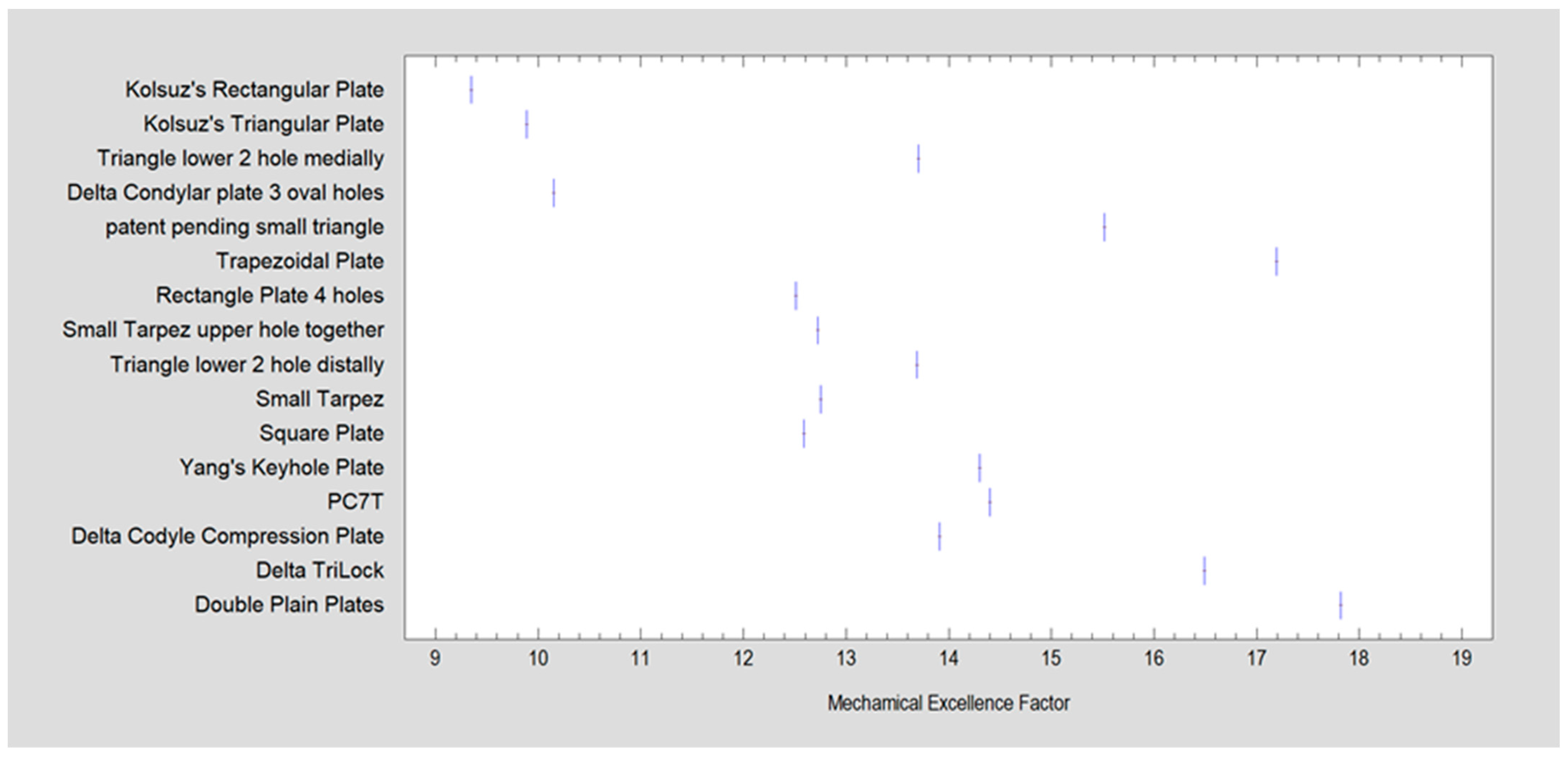
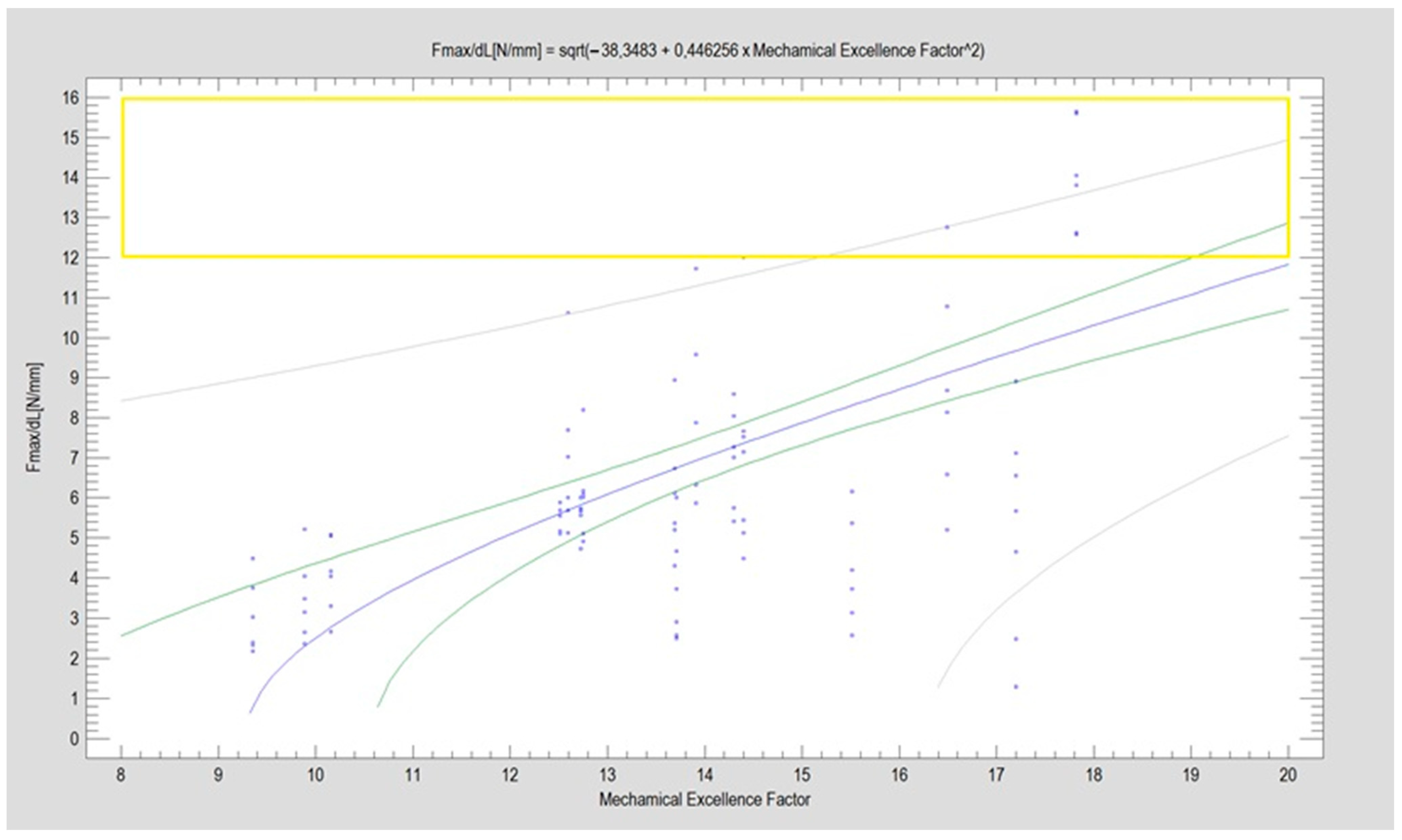
| Name | Design Code | Design | H [mm] | W [mm] | S [mm2] | MEF | Fmax/dL [N/mm] | |
|---|---|---|---|---|---|---|---|---|
| Kolsuz’s rectangular plate | Plate 48 |  | 11.4 | 10.1 | 49 | 67 | 9.4 | 2.94 ± 0.88 |
| Kolsuz’s triangular plate | Plate 47 |  | 14 | 10.4 | 58 | 79 | 9.9 | 3.43 ± 0.96 |
| Triangle lower 2 holes medially | Plate 45 |  | 18.1 | 9.8 | 67 | 90 | 13.7 | 3.61 ± 1.31 |
| Delta condylar plate 3 oval holes | Plate 37 |  | 17 | 11.4 | 64 | 87 | 10.2 | 4.07 ± 0.87 |
| Patent pending small triangle * | Plate 11 |  | 13.5 | 8 | 138 | 151 | 15.5 | 4.12 ± 1.25 |
| Trapezoidal plate | Plate 51 |  | 20 | 18 | 189 | 213 | 17.2 | 5.24 ± 2.66 |
| Rectangular plate 4 holes | Plate 32 |  | 11 | 8.5 | 37 | 55 | 12.5 | 5.57 ± 0.32 |
| Small trapeze upper hole together | Plate 34 |  | 11.1 | 12.1 | 40 | 61 | 12.7 | 5.60 ± 0.40 |
| Triangle lower 2 holes distally | Plate 42 |  | 17.8 | 10 | 67 | 90 | 13.7 | 6.00 ± 1.50 |
| Small trapeze | Plate 33 |  | 11.6 | 11.6 | 41 | 61 | 12.8 | 6.08 ± 1.06 |
| Square plate | Plate 31 |  | 10 | 10 | 39 | 57 | 12.6 | 6.88 ± 1.85 |
| Yang’s keyhole plate | Plate 46 |  | 19.7 | 9.9 | 80 | 106 | 14.3 | 7.05 ± 1.15 |
| PC7T | Plate 49 |  | 15 | 12.8 | 86 | 110 | 14.4 | 7.06 ± 2.52 |
| Delta condyle compression plate * | Plate 14 |  | 15.3 | 8.8 | 179 | 191 | 13.9 | 7.65 ± 2.24 |
| Delta TriLock * | Plate 02 |  | 15.4 | 8.8 | 174 | 187 | 16.5 | 8.61 ± 2.52 |
| Double plain plates * | Plate 20 |  | 16.5 | 3.4 | 227 | 236 | 17.8 | 14.02 ± 1.24 |
| Homogenous Groups 1 | Mean Fmax/dL | Name |
|---|---|---|
| X | 2.94 | Kolsuz’s rectangular plate |
| X | 3.43 | Kolsuz’s triangular plate |
| XX | 3.61 | Triangle lower 2 holes medially |
| XXX | 4.07 | Delta condylar plate 3 oval holes |
| XXX | 4.12 | Patent pending small triangle |
| XXX | 5.24 | Trapezoidal plate |
| XXX | 5.57 | Rectangle plate 4 holes |
| XXX | 5.6 | Small trapeze upper hole together |
| XXX | 6 | Triangle lower 2 holes distally |
| XXX | 6.08 | Small trapeze |
| XXX | 6.88 | Square plate |
| XXX | 7.05 | Yang’s keyhole plate |
| XXX | 7.06 | PC7T |
| XX | 7.65 | Delta condyle compression plate |
| X | 8.61 | Delta TriLock |
| X | 14.02 | Double plain plates |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okulski, J.; Kozakiewicz, M.; Krasowski, M.; Zieliński, R.; Szymor, P. Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options. J. Clin. Med. 2024, 13, 905. https://doi.org/10.3390/jcm13030905
Okulski J, Kozakiewicz M, Krasowski M, Zieliński R, Szymor P. Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options. Journal of Clinical Medicine. 2024; 13(3):905. https://doi.org/10.3390/jcm13030905
Chicago/Turabian StyleOkulski, Jakub, Marcin Kozakiewicz, Michał Krasowski, Rafał Zieliński, and Piotr Szymor. 2024. "Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options" Journal of Clinical Medicine 13, no. 3: 905. https://doi.org/10.3390/jcm13030905
APA StyleOkulski, J., Kozakiewicz, M., Krasowski, M., Zieliński, R., & Szymor, P. (2024). Optimal Plate Choice for High-Neck Mandibular Condyle Fracture: A Mechanistic Analysis of 16 Options. Journal of Clinical Medicine, 13(3), 905. https://doi.org/10.3390/jcm13030905







