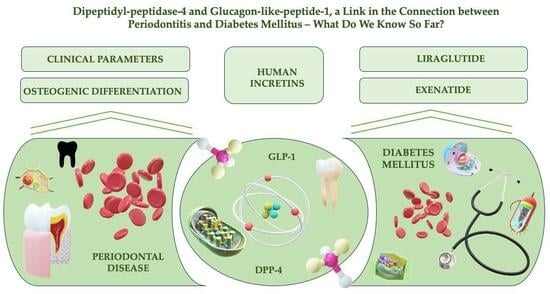
Dipeptidyl-Peptidase-4 and Glucagon-like-Peptide-1, a Link in the Connection between Periodontitis and Diabetes Mellitus—What Do We Know So Far?—A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria for the Selected Studies
2.3. Information Structuring and Review Writing
3. Periodontal Perspective on DPP-4 and GLP-1′s Actions
4. Implications of DPP-4 and GLP-1 in the Association between Diabetes and Periodontitis
5. Future Perspectives
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Beglundh, T.; Sculean, A.; Tonetti, M.S.; EFP Workshop Participants and Methodological Consultants. Treatment of stage I–III periodontitis—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47 (Suppl. S22), 4–60. [Google Scholar] [CrossRef]
- Rosier, B.T.; Marsh, P.D.; Mira, A. Resilience of the Oral Microbiota in Health: Mechanisms That Prevent Dysbiosis. J. Dent. Res. 2018, 97, 371–380. [Google Scholar] [CrossRef]
- Kilian, M.; Chapple, I.L.; Hannig, M.; Marsh, P.D.; Meuric, V.; Pedersen, A.M.; Tonetti, M.S.; Wade, W.G.; Zaura, E. The oral microbiome—An update for oral healthcare professionals. Br. Dent. J. 2016, 221, 657–666. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Lamont, R.J. Beyond the red complex and into more complexity: The polymicrobial synergy and dysbiosis (PSD) model of periodontal disease etiology. Mol. Oral Microbiol. 2012, 27, 409–419. [Google Scholar] [CrossRef]
- Mysak, J.; Podzimek, S.; Sommerova, P.; Lyuya-Mi, Y.; Bartova, J.; Janatova, T.; Prochazkova, J.; Duskova, J. Porphyromonas gingivalis: Major periodontopathic pathogen overview. J. Immunol. Res. 2014, 2014, 476068. [Google Scholar] [CrossRef] [PubMed]
- Nemoto, T.K.; Ohara Nemoto, Y. Dipeptidyl-peptidases: Key enzymes producing entry forms of extracellular proteins in asaccharolytic periodontopathic bacterium Porphyromonas gingivalis. Mol. Oral Microbiol. 2021, 36, 145–156. [Google Scholar] [CrossRef]
- Ohara-Nemoto, Y.; Shimoyama, Y.; Ono, T.; Sarwar, M.T.; Nakasato, M.; Sasaki, M.; Nemoto, T.K. Expanded substrate specificity supported by P1′ and P2′ residues enables bacterial dipeptidyl-peptidase 7 to degrade bioactive peptides. J. Biol. Chem. 2022, 298, 101585. [Google Scholar] [CrossRef] [PubMed]
- Ohara-Nemoto, Y.; Rouf, S.M.; Naito, M.; Yanase, A.; Tetsuo, F.; Ono, T.; Kobayakawa, T.; Shimoyama, Y.; Kimura, S.; Nakayama, K.; et al. Identification and characterization of prokaryotic dipeptidyl-peptidase 5 from Porphyromonas gingivalis. J. Biol. Chem. 2014, 289, 5436–5448. [Google Scholar] [CrossRef]
- Aemaimanan, P.; Sattayasai, N.; Wara-Aswapati, N.; Pitiphat, W.; Suwannarong, W.; Prajaneh, S.; Taweechaisupapong, S. Alanine aminopeptidase and dipeptidyl peptidase IV in saliva of chronic periodontitis patients. J. Periodontol. 2009, 80, 1809–1814. [Google Scholar] [CrossRef]
- Rea, D.; Van Elzen, R.; De Winter, H.; Van Goethem, S.; Landuyt, B.; Luyten, W.; Schoofs, L.; Van Der Veken, P.; Augustyns, K.; De Meester, I.; et al. Crystal structure of Porphyromonas gingivalis dipeptidyl peptidase 4 and structure-activity relationships based on inhibitor profiling. Eur. J. Med. Chem. 2017, 139, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Ohara-Nemoto, Y.; Shimoyama, Y.; Nakasato, M.; Nishimata, H.; Ishikawa, T.; Sasaki, M.; Kimura, S.; Nemoto, T.K. Distribution of dipeptidyl peptidase (DPP) 4, DPP5, DPP7 and DPP11 in human oral microbiota-potent biomarkers indicating presence of periodontopathic bacteria. FEMS Microbiol. Lett. 2018, 365, fny221. [Google Scholar] [CrossRef]
- Nemoto, T.K.; Ohara-Nemoto, Y. Exopeptidases and gingipains in Porphyromonas gingivalis as prerequisites for its amino acid metabolism. Jpn. Dent. Sci. Rev. 2016, 52, 22–29. [Google Scholar] [CrossRef]
- Cordero, O.J.; Varela-Calviño, R.; López-González, T.; Grujic, M.; Juranic, Z.; Mouriño, C.; Hernández-Rodríguez, Í.; Rodríguez-López, M.; de la Iglesia, B.A.; Pego-Reigosa, J.M. Anti-CD26 autoantibodies are involved in rheumatoid arthritis and show potential clinical interest. Clin. Biochem. 2017, 50, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Ohara-Nemoto, Y.; Nakasato, M.; Shimoyama, Y.; Baba, T.T.; Kobayakawa, T.; Ono, T.; Yaegashi, T.; Kimura, S.; Nemoto, T.K. Degradation of Incretins and Modulation of Blood Glucose Levels by Periodontopathic Bacterial Dipeptidyl Peptidase 4. Infect. Immun. 2017, 85, e00277-17. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G. Interconnection of periodontal disease and comorbidities: Evidence, mechanisms, and implications. Periodontology 2022, 89, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Mainas, G.; Ide, M.; Rizzo, M.; Magan-Fernandez, A.; Mesa, F.; Nibali, L. Managing the Systemic Impact of Periodontitis. Medicina 2022, 58, 621. [Google Scholar] [CrossRef] [PubMed]
- Lalla, E.; Papapanou, P.N. Diabetes mellitus and periodontitis: A tale of two common interrelated diseases. Nat. Rev. Endocrinol. 2011, 7, 738–748. [Google Scholar] [CrossRef] [PubMed]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: A two-way relationship. Diabetologia 2012, 55, 21–31. [Google Scholar] [CrossRef]
- Sanz, M.; Ceriello, A.; Buysschaert, M.; Chapple, I.; Demmer, R.T.; Graziani, F.; Herrera, D.; Jepsen, S.; Lione, L.; Madianos, P.; et al. Scientific evidence on the links between periodontal diseases and diabetes: Consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the International diabetes Federation and the European Federation of Periodontology. Diabetes Res. Clin. Pract. 2018, 137, 231–241. [Google Scholar] [CrossRef]
- Mesa, F.; Magan-Fernandez, A.; Castellino, G.; Chianetta, R.; Nibali, L.; Rizzo, M. Periodontitis and mechanisms of cardiometabolic risk: Novel insights and future perspectives. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 476–484. [Google Scholar] [CrossRef]
- Suzuki, A.; Ji, G.; Numabe, Y.; Ishii, K.; Muramatsu, M.; Kamoi, K. Large-scale investigation of genomic markers for severe periodontitis. Odontology 2004, 92, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Eley, B.M.; Cox, S.W. Correlation between gingival crevicular fluid dipeptidyl peptidase II and IV activity and periodontal attachment loss. A 2-year longitudinal study in chronic periodontitis patients. Oral Dis. 1995, 1, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Beighton, D.; Life, J.S. Trypsin-like, chymotrypsin-like and glycylprolyl dipeptidase activities in gingival crevicular fluid from human periodontal sites with gingivitis. Arch. Oral Biol. 1989, 34, 843–846. [Google Scholar] [CrossRef] [PubMed]
- Eley, B.M.; Cox, S.W. Cathepsin B/L-, elastase-, tryptase-,trypsin- and dipeptidyl peptidase IV-like activities in gingival crevicular fluid: Correlation with clinical parameters in untreated chronic periodontitis patients. J. Periodontal. Res. 1992, 27, 62–69. [Google Scholar] [CrossRef]
- Jiang, Y.; Brandt, B.W.; Buijs, M.J.; Cheng, L.; Exterkate, R.A.M.; Crielaard, W.; Deng, D.M. Manipulation of Saliva-Derived Microcosm Biofilms to Resemble Dysbiotic Subgingival Microbiota. Appl. Environ. Microbiol. 2021, 87, e02371-20. [Google Scholar] [CrossRef]
- Moraes, R.M.; Lima, G.M.; Oliveira, F.E.; Brito, A.C.; Pereira, R.C.; Oliveira, L.D.; Barros, P.P.; Franco, G.C.; Anbinder, A.L. Exenatide and Sitagliptin Decrease Interleukin 1β, Matrix Metalloproteinase 9, and Nitric Oxide Synthase 2 Gene Expression but Does Not Reduce Alveolar Bone Loss in Rats with Periodontitis. J. Periodontol. 2015, 86, 1287–1295. [Google Scholar] [CrossRef]
- Kumagai, Y.; Konishi, K.; Gomi, T.; Yagishita, H.; Yajima, A.; Yoshikawa, M. Enzymatic properties of dipeptidyl aminopeptidase IV produced by the periodontal pathogen Porphyromonas gingivalis and its participation in virulence. Infect. Immun. 2000, 68, 716–724. [Google Scholar] [CrossRef]
- Shimoyama, Y.; Sasaki, D.; Ohara-Nemoto, Y.; Nemoto, T.K.; Nakasato, M.; Sasaki, M.; Ishikawa, T. Immunoelectron Microscopic Analysis of Dipeptidyl-Peptidases and Dipeptide Transporter Involved in Nutrient Acquisition in Porphyromonas gingivalis. Curr. Microbiol. 2023, 80, 106. [Google Scholar] [CrossRef]
- Mohamed, H.G.; Idris, S.B.; Mustafa, M.; Ahmed, M.F.; Åstrøm, A.N.; Mustafa, K.; Ibrahim, S.O. Impact of Chronic Periodontitis on Levels of Glucoregulatory Biomarkers in Gingival Crevicular Fluid of Adults with and without Type 2 Diabetes. PLoS ONE 2015, 10, e0127660. [Google Scholar] [CrossRef] [PubMed]
- Suvan, J.; Masi, S.; Harrington, Z.; Santini, E.; Raggi, F.; D’Aiuto, F.; Solini, A. Effect of Treatment of Periodontitis on Incretin Axis in Obese and Nonobese Individuals: A Cohort Study. J. Clin. Endocrinol. Metab. 2021, 106, e74–e82. [Google Scholar] [CrossRef] [PubMed]
- Solini, A.; Suvan, J.; Santini, E.; Gennai, S.; Seghieri, M.; Masi, S.; Petrini, M.; D’Aiuto, F.; Graziani, F. Periodontitis affects glucoregulatory hormones in severely obese individuals. Int. J. Obes. 2019, 43, 1125–1129. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, X.; Zhang, L.; Wang, B.; Xu, B.; Zhang, J. GLP-1 inhibits PKCβ2 phosphorylation to improve the osteogenic differentiation potential of hPDLSCs in the AGE microenvironment. J. Diabetes Its Complicat. 2020, 34, 107495. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Chen, R.; Zhang, F.; Ding, M.; Wang, P. Exendin-4 relieves the inhibitory effects of high glucose on the proliferation and osteoblastic differentiation of periodontal ligament stem cells. Arch. Oral Biol. 2018, 91, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Liang, Q.Y.; Du, L.Q.; Zhang, R.; Ding, T.; Ge, S.H. Effects of Exenatide-4 on proliferation, migration and osteogenic differentiation of human periodontal ligament stem cells. Shanghai J. Stomatol. 2020, 29, 225–230. [Google Scholar]
- Ma, X.; Meng, J.; Jia, M.; Bi, L.; Zhou, Y.; Wang, Y.; Hu, J.; He, G.; Luo, X. Exendin-4, a glucagon-like peptide-1 receptor agonist, prevents osteopenia by promoting bone formation and suppressing bone resorption in aged ovariectomized rats. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2013, 28, 1641–1652. [Google Scholar] [CrossRef]
- Wang, M.; Liu, M.; Zheng, J.; Xiong, L.; Wang, P. Exendin-4 regulates the MAPK and WNT signaling pathways to alleviate the osteogenic inhibition of periodontal ligament stem cells in a high glucose environment. Open Med. 2023, 18, 20230692. [Google Scholar] [CrossRef]
- Sawada, N.; Adachi, K.; Nakamura, N.; Miyabe, M.; Ito, M.; Kobayashi, S.; Miyajima, S.I.; Suzuki, Y.; Kikuchi, T.; Mizutani, M.; et al. Glucagon-Like Peptide-1 Receptor Agonist Liraglutide Ameliorates the Development of Periodontitis. J. Diabetes Res. 2020, 2020, 8843310. [Google Scholar] [CrossRef]
- Pang, Y.; Yuan, X.; Guo, J.; Wang, X.; Yang, M.; Zhu, J.; Wang, J. The effect of liraglutide on the proliferation, migration, and osteogenic differentiation of human periodontal ligament cells. J. Periodontal Res. 2019, 54, 106–114. [Google Scholar] [CrossRef]
- Zhang, Y.; Yuan, X.; Wu, Y.; Pei, M.; Yang, M.; Wu, X.; Pang, Y.; Wang, J. Liraglutide regulates bone destruction and exhibits anti-inflammatory effects in periodontitis in vitro and in vivo. J. Dent. 2020, 94, 103310. [Google Scholar] [CrossRef]
- Zhai, S.; Liu, C.; Vimalraj, S.; Subramanian, R.; Abullais, S.S.; Arora, S.; Saravanan, S. Glucagon-like peptide-1 receptor promotes osteoblast differentiation of dental pulp stem cells and bone formation in a zebrafish scale regeneration model. Peptides 2023, 163, 170974. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Pang, Y.; Pei, M.; Li, Y.; Yuan, X.; Tang, R.; Wang, J. Therapeutic Potential of Liraglutide for Diabetes-Periodontitis Comorbidity: Killing Two Birds with One Stone. J. Diabetes Res. 2022, 2022, 8260111. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gheonea, T.C.; Șurlin, P.; Nicolae, F.M.; Gheorghe, D.N.; Popescu, D.M.; Rogoveanu, I. Dipeptidyl-Peptidase-4 and Glucagon-like-Peptide-1, a Link in the Connection between Periodontitis and Diabetes Mellitus—What Do We Know So Far?—A Scoping Review. J. Clin. Med. 2024, 13, 903. https://doi.org/10.3390/jcm13030903
Gheonea TC, Șurlin P, Nicolae FM, Gheorghe DN, Popescu DM, Rogoveanu I. Dipeptidyl-Peptidase-4 and Glucagon-like-Peptide-1, a Link in the Connection between Periodontitis and Diabetes Mellitus—What Do We Know So Far?—A Scoping Review. Journal of Clinical Medicine. 2024; 13(3):903. https://doi.org/10.3390/jcm13030903
Chicago/Turabian StyleGheonea, Theodora Claudia, Petra Șurlin, Flavia Mirela Nicolae, Dorin Nicolae Gheorghe, Dora Maria Popescu, and Ion Rogoveanu. 2024. "Dipeptidyl-Peptidase-4 and Glucagon-like-Peptide-1, a Link in the Connection between Periodontitis and Diabetes Mellitus—What Do We Know So Far?—A Scoping Review" Journal of Clinical Medicine 13, no. 3: 903. https://doi.org/10.3390/jcm13030903
APA StyleGheonea, T. C., Șurlin, P., Nicolae, F. M., Gheorghe, D. N., Popescu, D. M., & Rogoveanu, I. (2024). Dipeptidyl-Peptidase-4 and Glucagon-like-Peptide-1, a Link in the Connection between Periodontitis and Diabetes Mellitus—What Do We Know So Far?—A Scoping Review. Journal of Clinical Medicine, 13(3), 903. https://doi.org/10.3390/jcm13030903