Carboplatin plus Paclitaxel in Combination with the Histone Deacetylate Inhibitor, Vorinostat, in Patients with Recurrent Platinum-Sensitive Ovarian Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Objectives
2.2. Patients
2.3. Treatment Plan
2.4. Assessments and Endpoints
2.5. Statistics
3. Results
3.1. Response
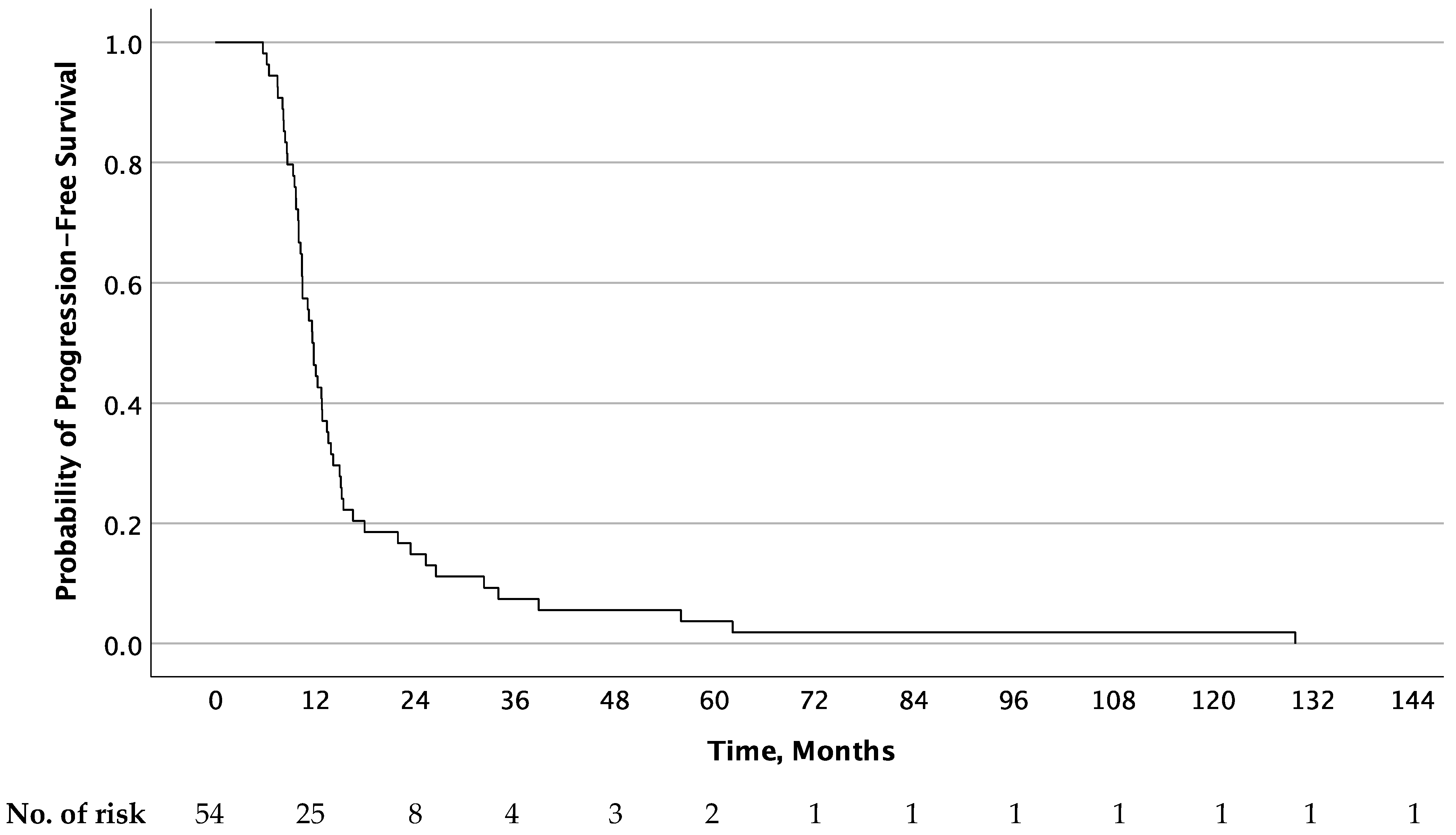
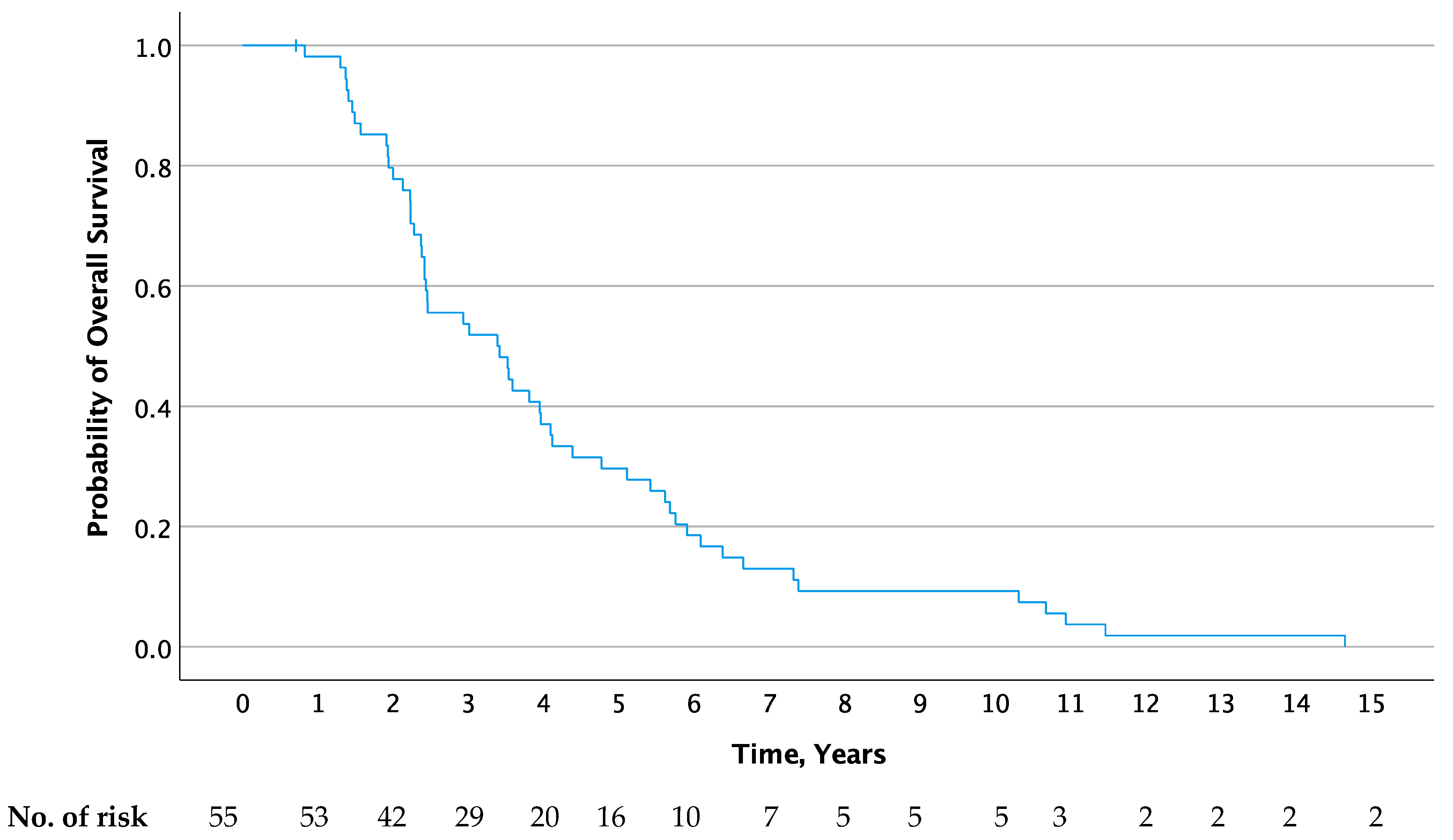
3.2. Progression-Free and Overall Survival
3.3. Toxicity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- Jacobs, I.J.; Menon, U. Progress and challenges in screening for early detection of ovarian cancer. Mol. Cell. Proteom. 2004, 3, 355–366. [Google Scholar] [CrossRef]
- Torre, L.A.; Trabert, B.; DeSantis, C.E.; Miller, K.D.; Samimi, G.; Runowicz, C.D.; Gaudet, M.M.; Jemal, A.; Siegel, R.L. Ovarian cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 284–296. [Google Scholar] [CrossRef]
- The ICON Group. Paclitaxel plus carboplatin versus standard chemotherapy with either single-agent carboplatin or cy-clophosphamide, doxorubicin, and cisplatin in women with ovarian cancer: The ICON3 randomised trial. Lancet 2002, 360, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Markman, M.; Markman, J.; Webster, K.; Zanotti, K.; Kulp, B.; Peterson, G.; Belinson, J. Duration of response to second-line, platinum-based chemotherapy for ovarian cancer: Implications for patient management and clinical trial design. J. Clin. Oncol. 2004, 22, 3120–3125. [Google Scholar] [CrossRef] [PubMed]
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Nikšić, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Estève, J.; et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37,513,025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef] [PubMed]
- Colombo, N.; Sessa, C.; Du Bois, A.; Ledermann, J.; McCluggage, W.G.; McNeish, I.; Morice, P.; Pignata, S.; Ray-Coquard, I.; Vergote, I.; et al. ESMO–ESGO consensus conference recommendations on ovarian cancer: Pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Int. J. Gynecol. Cancer 2019, 29, 728–760. [Google Scholar] [CrossRef]
- du Bois, A.; Weber, B.; Rochon, J.; Meier, W.; Goupil, A.; Olbricht, S.; Barats, J.-C.; Kuhn, W.; Orfeuvre, H.; Wagner, U.; et al. Addition of Epirubicin As a Third Drug to Carboplatin-Paclitaxel in First-Line Treatment of Advanced Ovarian Cancer: A Prospectively Randomized Gynecologic Cancer Intergroup Trial by the Arbeitsgemeinschaft Gynaekologische Onkologie Ovarian Cancer Study Group and the Groupe d’Investigateurs Nationaux pour l’Etude des Cancers Ovariens. J. Clin. Oncol. 2006, 24, 1127–1135. [Google Scholar] [CrossRef]
- du Bois, A.; Herrstedt, J.; Hardy-Bessard, A.-C.; Müller, H.-H.; Harter, P.; Kristensen, G.; Joly, F.; Huober, J.; Åvall-Lundqvist, E.; Weber, B.; et al. Phase III Trial of carboplatin plus paclitaxel with or without gemcitabine in first-line treatment of epithelial ovarian cancer. J. Clin. Oncol. 2010, 28, 4162–4169. [Google Scholar] [CrossRef]
- Zhong, L.; Li, Y.; Xiong, L.; Wang, W.; Wu, M.; Yuan, T.; Yang, W.; Tian, C.; Miao, Z.; Wang, T.; et al. Small molecules in targeted cancer therapy: Advances, challenges, and future perspectives. Signal Transduct. Target. Ther. 2021, 6, 201. [Google Scholar] [CrossRef]
- Mirza, M.R.; Monk, B.J.; Herrstedt, J.; Oza, A.M.; Mahner, S.; Redondo, A.; Fabbro, M.; Ledermann, J.A.; Lorusso, D.; Vergote, I.; et al. Niraparib Maintenance Therapy in Platinum-Sensitive, Recurrent Ovarian Cancer. N. Engl. J. Med. 2016, 375, 2154–2164. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Nag, S.; Aggarwal, S.; Rauthan, A.; Warrier, N. Maintenance therapy for recurrent epithelial ovarian cancer: Current therapies and future perspectives—A review. J. Ovarian Res. 2019, 12, 103. [Google Scholar] [CrossRef] [PubMed]
- George, A.; Kaye, S.; Banerjee, S. Delivering widespread BRCA testing and PARP inhibition to patients with ovarian cancer. Nat. Rev. Clin. Oncol. 2017, 14, 284–296. [Google Scholar] [CrossRef]
- Jenke, R.; Reßing, N.; Hansen, F.K.; Aigner, A.; Büch, T. Anticancer Therapy with HDAC inhibitors: Mechanism-based combination strategies and future perspectives. Cancers 2021, 13, 634. [Google Scholar] [CrossRef]
- Marks, P.A.; Rifkind, R.A.; Richon, V.M.; Breslow, R.; Miller, T.; Kelly, W.K. Histone deacetylases and cancer: Causes and therapies. Nat. Rev. Cancer 2001, 1, 194–202. [Google Scholar] [CrossRef]
- Arora, S.; Balasubramaniam, S.; Zhang, H.; Berman, T.; Narayan, P.; Suzman, D.; Bloomquist, E.; Tang, S.; Gong, Y.; Sridhara, R.; et al. FDA Approval Summary: Olaparib Monotherapy or in Combination with Bevacizumab for the Maintenance Treatment of Patients with Advanced Ovarian Cancer. Oncologist 2021, 26, e164–e172. [Google Scholar] [CrossRef]
- Modesitt, S.C.; Sill, M.; Hoffman, J.S.; Bender, D.P. A phase II study of vorinostat in the treatment of persistent or recurrent epithelial ovarian or primary peritoneal carcinoma: A Gynecologic Oncology Group study. Gynecol. Oncol. 2008, 109, 182–186. [Google Scholar] [CrossRef]
- Mackay, H.J.; Hirte, H.; Colgan, T.; Covens, A.; MacAlpine, K.; Grenci, P.; Wang, L.; Mason, J.; Pham, P.-A.; Tsao, M.S.; et al. Phase II trial of the histone deacetylase inhibitor Belinostat in women with platinum resistant epithelial ovarian cancer and micropapillary (LMP) ovarian tumors. Eur. J. Cancer 2010, 46, 1573–1579. [Google Scholar] [CrossRef]
- Dizon, D.S.; Blessing, J.A.; Penson, R.T.; Drake, R.D.; Walker, J.L.; Johnston, C.M.; DiSilvestro, P.A.; Fader, A.N. A phase II evaluation of belinostat and carboplatin in the treatment of recurrent or persistent platinum-resistant ovarian, fallopian tube, or primary peritoneal carcinoma: A gynecologic oncology group study. Gynecol. Oncol. 2012, 125, 367–371. [Google Scholar] [CrossRef]
- Dizon, D.S.; Damstrup, L.; Finkler, N.J.; Lassen, U.; Celano, P.; Glasspool, R.; Crowley, E.; Lichenstein, H.S.; Knoblach, P.; Penson, R.T. Phase II activity of belinostat (PXD-101), carboplatin, and paclitaxel in women with previously treated ovarian cancer. Int. J. Gynecol. Cancer 2012, 22, 979–986. [Google Scholar] [CrossRef]
- Chobanian, N.H.; Greenberg, V.L.; Gass, J.M.; DeSimone, C.P.; Van Nagell, J.R.; Zimmer, S.G. Histone Deacetylase Inhibitors Enhance Paclitaxel-induced Cell Death in Ovarian Cancer Cell Lines Independent of p53 Status. Anticancer Res. 2004, 24, 539–545. [Google Scholar]
- Ramarao-Milne, P.; Kondrashova, O.; Barry, S.; Hooper, J.D.; Lee, J.S.; Waddell, N. Histone modifying enzymes in gynaecological cancers. Cancers 2021, 13, 816. [Google Scholar] [CrossRef]
- Yoo, J.; Jeon, Y.H.; Lee, D.H.; Kim, G.W.; Lee, S.W.; Kim, S.Y.; Park, J.; Kwon, S.H. HDAC6-selective inhibitors enhance anticancer effects of paclitaxel in ovarian cancer cells. Oncol. Lett. 2021, 21, 201. [Google Scholar] [CrossRef]
- Ramalingam, S.S.; Parise, R.A.; Ramananthan, R.K.; Lagattuta, T.F.; Musguire, L.A.; Stoller, R.G.; Potter, D.M.; Argiris, A.E.; Zwiebel, J.A.; Egorin, M.J.; et al. Phase I and Pharmacokinetic Study of Vorinostat, A Histone Deacetylase Inhibitor, in Combination with Carboplatin and Paclitaxel for Advanced Solid Malignancies. Clin. Cancer Res. 2007, 13, 3605–3610. [Google Scholar] [CrossRef]
- Vasey, P.A.; Herrstedt, J.; Jelic, S. ESMO minimum clinical recommendations for diagnosis, treatment and follow-up of epithelial ovarian carcinoma. Ann. Oncol. 2005, 16, i13–i15. [Google Scholar] [CrossRef]
- Rustin, G.J.S.; Vergote, I.; Eisenhauer, E.; Pujade-Lauraine, E.; Quinn, M.; Thigpen, T.; du Bois, A.; Kristensen, G.; Jakobsen, A.; Sagae, S.; et al. Definitions for Response and Progression in Ovarian Cancer Clinical Trials Incorporating RECIST 1.1 and CA 125 Agreed by the Gynecological Cancer Intergroup (GCIG). Int. J. Gynecol. Cancer 2011, 21, 419–423. [Google Scholar] [CrossRef]
- Therasse, P.; Arbuck, S.G.; Eisenhauer, E.A.; Wanders, J.; Kaplan, R.S.; Rubinstein, L.; Verweij, J.; Van Glabbeke, M.; van Oosterom, A.T.; Christian, M.C.; et al. New Guidelines to Evaluate the Response to Treatment in Solid Tumors. J. Natl. Cancer Inst. 2000, 92, 205–216. [Google Scholar] [CrossRef]
- The ICON and AGO Collaborators. Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: The ICON4/AGO-OVAR-2.2 trial. Lancet 2003, 361, 2099–2106. [Google Scholar] [CrossRef]
- Delgado, A.; Guddati, A.K. Clinical endpoints in oncology—A primer. Am. J. Cancer Res. 2021, 11, 1121–1131. [Google Scholar]
- Wagner, U.; Marth, C.; Largillier, R.; Kaern, J.; Brown, C.; Heywood, M.; Bonaventura, T.; Vergote, I.; Piccirillo, M.C.; Fossati, R.; et al. Final overall survival results of phase III GCIG CALYPSO trial of pegylated liposomal doxorubicin and carboplatin vs. paclitaxel and carboplatin in platinum-sensitive ovarian cancer patients. Br. J. Cancer 2012, 107, 588–591. [Google Scholar] [CrossRef]
- Pfisterer, J.; Plante, M.; Vergote, I.; du Bois, A.; Hirte, H.; Lacave, A.J.; Wagner, U.; Stähle, A.; Stuart, G.; Kimmig, R.; et al. Gemcitabine plus carboplatin compared with carboplatin in patients with platinum-sensitive recurrent ovarian cancer: An intergroup trial of the AGO-OVAR, the NCIC CTG, and the EORTC GCG. J. Clin. Oncol. 2006, 24, 4699–4707. [Google Scholar] [CrossRef]
- Mendivil, A.A.; Micha, J.P.; Brown, J.V.; Rettenmaier, M.A.; Abaid, L.N.; Lopez, K.L.; Goldstein, B.H. Increased incidence of severe gastrointestinal events with first-line paclitaxel, carboplatin, and vorinostat chemotherapy for advanced-stage epithelial ovarian, primary peritoneal, and fallopian tube cancer. Int. J. Gynecol. Cancer 2013, 23, 533–539. [Google Scholar] [CrossRef]
- Janyst, K.; Janyst, M.; Siernicka, M.; Lasek, W. Synergistic antitumor effects of histone deacetylase inhibitor scriptaid and bortezomib against ovarian cancer cells. Oncol. Rep. 2018, 39, 1999–2005. [Google Scholar] [CrossRef]
- Matulonis, U.; Berlin, S.; Lee, H.; Whalen, C.; Obermayer, E.; Penson, R.; Liu, J.; Campos, S.; Krasner, C.; Horowitz, N. Phase I study of combination of vorinostat, carboplatin, and gemcitabine in women with recurrent, platinum-sensitive epithelial ovarian, fallopian tube, or peritoneal cancer. Cancer Chemother. Pharmacol. 2015, 76, 417–423. [Google Scholar] [CrossRef]
- Booth, C.M.; Eisenhauer, E.A.; Gyawali, B.; Tannock, I.F. Progression-free survival should not be used as a primary end point for registration of anticancer drugs. J. Clin. Oncol. 2023, 41, 4968–4972. [Google Scholar] [CrossRef]
- Aghajanian, C.; Blank, S.V.; Goff, B.A.; Judson, P.L.; Teneriello, M.G.; Husain, A.; Sovak, M.A.; Yi, J.; Nycum, L.R. OCEANS: A randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J. Clin. Oncol. 2012, 30, 2039–2045. [Google Scholar] [CrossRef]
- Coleman, R.L.; Oza, A.M.; Lorusso, D.; Aghajanian, C.; Oaknin, A.; Dean, A.; Colombo, N.; Weberpals, J.I.; Clamp, A.; Scambia, G.; et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 390, 1949–1961. [Google Scholar] [CrossRef]
- del Campo, J.M.; Matulonis, U.A.; Malander, S.; Provencher, D.; Mahner, S.; Follana, P.; Waters, J.; Berek, J.S.; Woie, K.; Oza, A.M.; et al. Niraparib Maintenance Therapy in Patients with Recurrent Ovarian Cancer after a Partial Response to the Last Platinum-Based Chemotherapy in the ENGOT-OV16/NOVA Trial. J. Clin. Oncol. 2019, 37, 2968–2973. [Google Scholar] [CrossRef]
- Poveda, A.; Floquet, A.; Ledermann, J.A.; Asher, R.; Penson, R.T.; Oza, A.M.; Korach, J.; Huzarski, T.; Pignata, S.; Friedlander, M.; et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): A final analysis of a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2021, 22, 620–631. [Google Scholar] [CrossRef]
- Disilvestro, P.; Banerjee, S.; Colombo, N.; Scambia, G.; Kim, B.G.; Oaknin, A.; Friedlander, M.; Lisyanskaya, A.; Floquet, A.; Leary, A.; et al. Overall Survival with Maintenance Olaparib at a 7-Year Follow-Up in Patients with Newly Diagnosed Advanced Ovarian Cancer and a BRCA Mutation: The SOLO1/GOG 3004 Trial. J. Clin. Oncol. 2023, 41, 609–617. [Google Scholar] [CrossRef]
- Wilson, A.J.; Gupta, V.G.; Liu, Q.; Yull, F.; Crispens, M.A.; Khabele, D. Panobinostat enhances olaparib efficacy by modifying expression of homologous recombination repair and immune transcripts in ovarian cancer. Neoplasia 2022, 24, 63–75. [Google Scholar] [CrossRef]
- Shetty, M.G.; Pai, P.; Deaver, R.E.; Satyamoorthy, K.; Babitha, K.S. Histone deacetylase 2 selective inhibitors: A versatile therapeutic strategy as next generation drug target in cancer therapy. Pharmacol. Res. 2021, 170, 105695. [Google Scholar] [CrossRef]
- Huang, R.; Langdon, S.P.; Tse, M.; Mullen, P.; Um, I.H.; Faratian, D.; Harrison, D.J. The role of HDAC2 in chromatin remodelling and response to chemotherapy in ovarian cancer. Oncotarget 2015, 7, 4695–4711. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Histological-verified epithelial ovarian, peritoneal, or fallopian tube carcinoma. | Patients treated with an experimental drug within the last 4 weeks before inclusion, and patients who received other concomitant anticancer treatments. |
| Women ≥ 18 years. | Patients having an active infection or who have received intravenous antibacterial or antifungal medicine within the last 2 weeks before inclusion. |
| ECOG performance status ≤ 2. | Previous treatment with more than first-line chemotherapy. |
| Expected duration of life > 3 months. | Patients previously treated with an HDAC inhibitor. Patients who have been treated with Valproate for convulsions can be included; however, only if the treatment has taken place > 30 days before inclusion. |
| Previous treatment regimen containing platinum and paclitaxel. | Patients treated with steroid who are not stabilized on a firm dose equivalent to a maximum of 10 mg prednisolone per day for the last 4 weeks before inclusion. |
| Platinum and paclitaxel sensitive tumor, defined as a minimum of 6 months from cessation of treatment until disease progression. | Progression during treatment with first-line chemotherapy containing platinum/paclitaxel or disease progression less than 6 months after treatment cessation. |
| Measurable or assessable lesion. Patients having increased CA-125 as the only sign of recurrence are also eligible. | Concomitant serious and/or non-controllable medical condition such as non-controllable infection (including HIV-infected patients), hypertension, ischemic heart disease, myocardial infarction within the last 6 months, or congestive heart failure. |
| Signed informed consent before inclusion. | Previous treatment for or another concomitant malignant disease within the last 5 years, except for curative-treated carcinoma in situ cervical cancer, or basal cell carcinoma. |
| Prepared to appear for the planned follow-up visits and capable of handling toxicity. | Previous severe allergic reactions in connection with carboplatin, paclitaxel, or agents within the histone deacetylase inhibitor group. |
| Normal organ functions * | Women of child-bearing age. Women must have undergone surgical removal of the ovaries or be post-menopausal with no menstruation during the previous year. |
| Peripheral neuropathy ≥ grade 2, unless this is due to a medical condition. | |
| Patients with history of severe hypersensitive reactions with regards to products containing cyclosporine or K-vitamin) and/or patients with known hypersensitivity towards agents chemically connected to paclitaxel, carboplatin, or vorinostat. | |
| Patients with known cerebral metastases or clinical signs of cerebral metastases. |
| N = 55 | |
|---|---|
| Age, median (range) | 62 (44–78) |
| ECOG performance status, n (%) | |
| 0 | 49 (89.1) |
| 1 | 5 (9.0) |
| 2 | 1 (1.8) |
| Malignancy, n (%) | |
| Ovarian | 43 (72.7) |
| Primary peritoneal carcinoma | 10 (18.1) |
| Fallopian tube carcinoma | 2 (3.6) |
| Histologic subtype and tumor grade, n (%) | |
| Serous | |
| High grade | 28 (50.9) |
| Intermediate | 10 (18.2) |
| Low grade | 5 (9.1) |
| Unknown | 7 (12.7) |
| Endometrioid | |
| High grade | 1 (1.8) |
| Unknown | 1 (1.8) |
| Clear cell | 1 (1.8) |
| Mixed endometrioid/serous | |
| High grade | 1 (1.8) |
| Transitional cell | |
| High grade | 1 (1.8) |
| Platinum-free interval, months | |
| 6–12 | 10 (18.2) |
| >12–18 | 22 (40.0) |
| >18–24 | 8 (14.5) |
| >24 | 15 (27.3) |
| Response | First-Line Treatment n (%) | Second-Line Treatment n (%) | Duration of Responses (Months) | First-Line n = 45 | Second-Line n = 33 | Secondary Response Rates Based on Duration of First-Line Response n = 29 (%) |
|---|---|---|---|---|---|---|
| CR | 32 (58.1) | 14 (25.5) | <6 | 1 | ||
| PR | 13 (23.6) | 19 (34.5) | 6–12 | 6 | 14 | 3 (50) |
| SD | 7 (12.7) | 20 (36.4) | >12–18 | 21 | 12 | 13 (62) |
| Unknown | 3 (5.5) | 2 (3.6) | >18–24 | 6 | 2 | 4 (67) |
| >24 | 12 | 4 | 9 (75) |
| Adverse Events | Any Grade n (%) | Grade 1–2 n (%) | Grade 3–4 n (%) |
|---|---|---|---|
| Non-haematological (patients, n = 55) | |||
| Diarrhea | 28 (50.9) | 25 (45.5) | 3 (5.5) |
| Nausea | 45 (81.8) | 44 (80.0) | 1 (1.8) |
| Vomiting | 27 (49.1) | 25 (45.5) | 2 (3.6) |
| Dyspepsia | 7 (12.7) | 7 (12.7) | 0 (0) |
| Constipation | 22 (40.0) | 20 (36.4) | 2 (3.6) |
| Cystitis | 9 (16.4) | 9 (16.4) | 0 (0) |
| Sensory neuropathy | 41 (74.5) | 39 (70.9) | 2 (3.6) |
| Motor | 22 (40.0) | 20 (36.4) | 2 (3.6) |
| Pain | 42 (76.3) | 39 (70.9) | 3 (5.5) |
| Stomatitis | 30 (54.5) | 30 (54.5) | 0 (0) |
| Skin | 17 (30.9) | 17 (30.9) | 0 (0) |
| Nail disorder | 7 (12.7) | 6 (10.9) | 1 (1.8) |
| Allergic reaction | 7 (12.7) | 5 (9.1) | 2 (3.6) |
| Dyspnea | 15 (27.3) | 14 (25.5) | 1 (1.8) |
| Fever in absence of infection | 8 (14.5) | 8 (14.5) | 0 (0) |
| Fatigue | 50 (90.9) | 36 (65.5) | 14 (25.5) |
| Anorexia | 44 (80.0) | 41 (74.5) | 3 (5.5) |
| Myalgia | 34 (61.8) | 33 (60) | 1 (1.8) |
| Arthralgia | 27 (49.1) | 27 (49.1) | 0 (0) |
| Haematological (patients, n = 50) | |||
| Neutropenia 1 | 42 (84) | 15 (30) | 27 (54) |
| Thrombocytopenia 2 | 43 (86) | 33 (66) | 10 (20) |
| Anemia 3 | 45 (90) | 45 (90) | 0 (0) |
| Increased creatinine | 5 (10) | 5 (10) | 0 (0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meteran, H.; Knudsen, A.Ø.; Jørgensen, T.L.; Nielsen, D.; Herrstedt, J. Carboplatin plus Paclitaxel in Combination with the Histone Deacetylate Inhibitor, Vorinostat, in Patients with Recurrent Platinum-Sensitive Ovarian Cancer. J. Clin. Med. 2024, 13, 897. https://doi.org/10.3390/jcm13030897
Meteran H, Knudsen AØ, Jørgensen TL, Nielsen D, Herrstedt J. Carboplatin plus Paclitaxel in Combination with the Histone Deacetylate Inhibitor, Vorinostat, in Patients with Recurrent Platinum-Sensitive Ovarian Cancer. Journal of Clinical Medicine. 2024; 13(3):897. https://doi.org/10.3390/jcm13030897
Chicago/Turabian StyleMeteran, Hanieh, Anja Ør Knudsen, Trine Lembrecht Jørgensen, Dorte Nielsen, and Jørn Herrstedt. 2024. "Carboplatin plus Paclitaxel in Combination with the Histone Deacetylate Inhibitor, Vorinostat, in Patients with Recurrent Platinum-Sensitive Ovarian Cancer" Journal of Clinical Medicine 13, no. 3: 897. https://doi.org/10.3390/jcm13030897
APA StyleMeteran, H., Knudsen, A. Ø., Jørgensen, T. L., Nielsen, D., & Herrstedt, J. (2024). Carboplatin plus Paclitaxel in Combination with the Histone Deacetylate Inhibitor, Vorinostat, in Patients with Recurrent Platinum-Sensitive Ovarian Cancer. Journal of Clinical Medicine, 13(3), 897. https://doi.org/10.3390/jcm13030897







