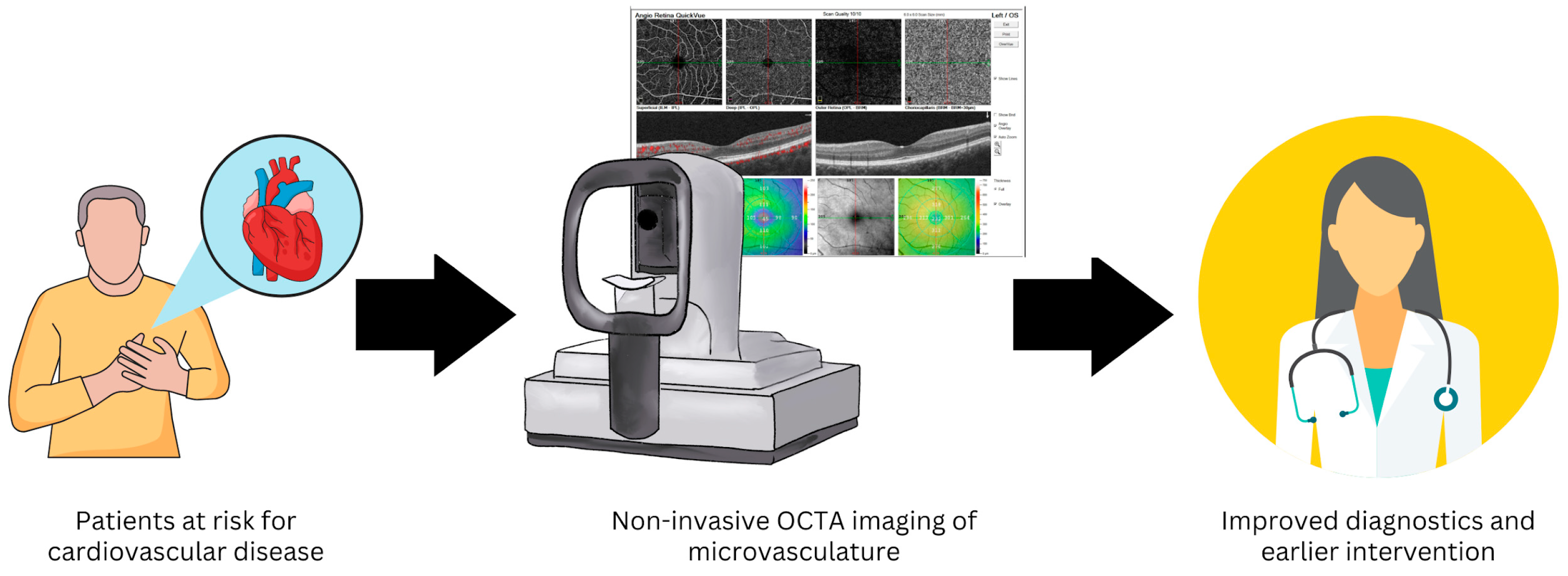
The Eye as the Window to the Heart: Optical Coherence Tomography Angiography Biomarkers as Indicators of Cardiovascular Disease
Abstract
1. Introduction
2. Methods
3. Results and Discussion
3.1. Systemic Arterial Hypertension
3.2. Atherosclerotic Disease
3.3. Congestive Heart Failure
4. Limitations
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AVR | Arteriovenous Ratio |
| CAD | Coronary Artery Disease |
| CHD | Coronary Heart Disease |
| CHF | Congestive Heart Failure |
| CRAE | Central Retinal Artery Equivalent |
| CRVE | Central Retinal Vein Equivalent |
| CTO | Coronary Total Occlusion |
| CVD | Cardiovascular Disease |
| DCP | Deep Capillary/Vascular Plexus |
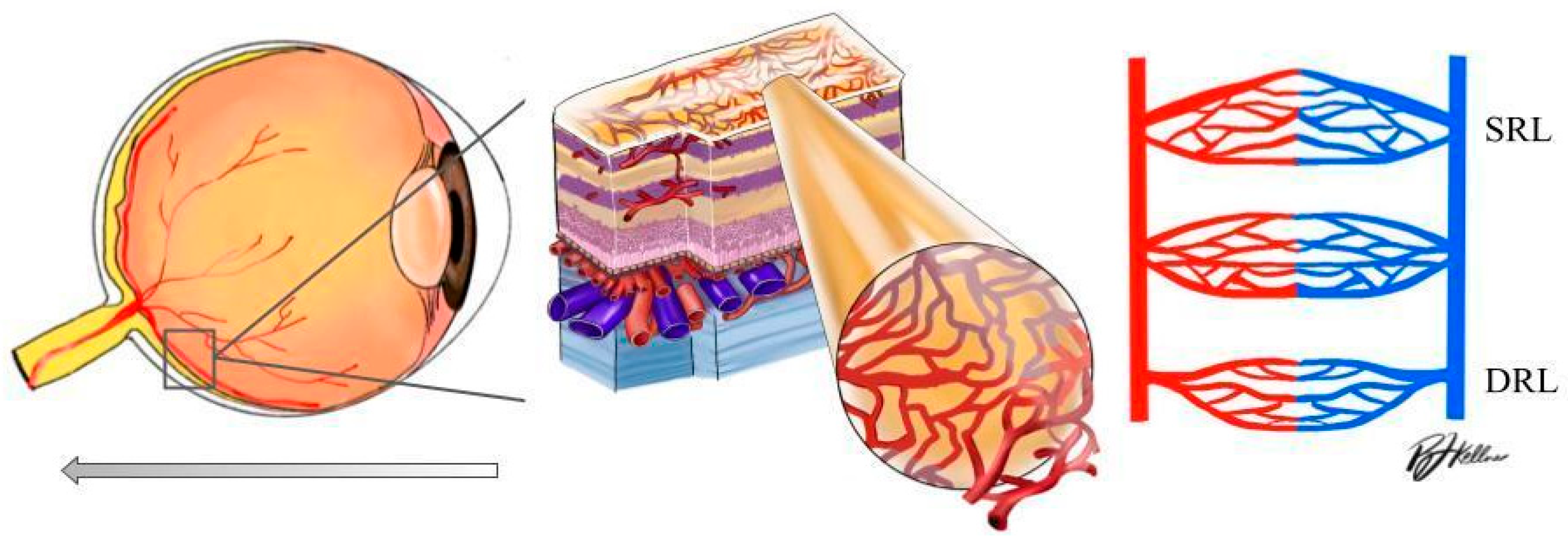
| DRL | Deep Retinal Layer |
| DVP | Deep Vascular Plexus |
| FAZ | Foveal Avascular Zone |
| HF | Heart Failure |
| HTN | Hypertension |
| IS | Ischemic Stroke |
| LAA | Large Artery Atherosclerosis |
| LVEF | Left Ventricular Ejection Fraction |
| MI | Myocardial Infarction |
| NYHA | New York Heart Association |
| OCTA | Optical Coherence Tomography Angiography |
| SAD | Small Artery Disease |
| SCP | Superficial Capillary Plexus |
| SRL | Superficial Retinal Layer |
| SVP | Superficial Vascular Plexus |
| VD | Vascular Density |
References
- World Heath Organization. Cardiovascular Diseases (CVDs). 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 1 July 2023).
- Leung, H.; Wang, J.J.; Rochtchina, E.; Wong, T.Y.; Klein, R.; Mitchell, P. Impact of current and past blood pressure on retinal arteriolar diameter in an older population. J. Hypertens. 2004, 22, 1543–1549. [Google Scholar] [CrossRef] [PubMed]
- Leung, H.; Wang, J.J.; Rochtchina, E.; Tan, A.G.; Wong, T.Y.; Klein, R.; Hubbard, L.D.; Mitchell, P. Relationships between age, blood pressure and retinal vessel diameters in an older population. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2900–2904. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Wang, J.J.; Mackey, D.A.; Wong, T.Y. Retinal vascular caliber: Systemic, environmental, and genetic associations. Surv. Ophthalmol. 2009, 54, 74–95. [Google Scholar] [CrossRef] [PubMed]
- Tanabe, Y.; Kawasaki, R.; Wang, J.J.; Wong, T.Y.; Mitchell, P.; Daimon, M.; Oizumi, T.; Kato, T.; Kawata, S.; Kayama, T. Retinal arteriolar narrowing predicts 5-year risk of hypertension in Japanese people: The Funagata study. Microcirculation 2010, 17, 94–102. [Google Scholar] [CrossRef]
- Jumar, A.; Harazny, J.M.; Ott, C.; Friedrich, S.; Kistner, I.; Striepe, K.; Schmieder, R.E. Retinal capillary rarefaction in patients with type 2 diabetes mellitus. PLoS ONE 2016, 11, e0162608. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.; Wang, J.J.; Wong, T.Y.; Rochtchina, E.; Klein, R.; Leeder, S.R.; Mitchell, P. Retinal arteriolar narrowing is associated with 5-year incident severe hypertension: The Blue Mountains Eye Study. Hypertension 2004, 44, 442–447. [Google Scholar] [CrossRef]
- Peng, X.Y.; Wang, F.H.; Liang, Y.B.; Wang, J.J.; Sun, L.P.; Peng, Y.; Friedman, D.S.; Liew, G.; Wang, N.L.; Wong, T.Y. Retinopathy in persons without diabetes: The Handan Eye Study. Ophthalmology 2010, 117, 531–537. [Google Scholar] [CrossRef]
- Ding, J.; Wai, K.L.; McGeechan, K.; Ikram, M.K.; Kawasaki, R.; Xie, J.; Klein, R.; Klein, B.B.; Cotch, M.F.; Wang, J.J.; et al. Retinal vascular caliber and the development of hypertension: A meta-analysis of individual participant data. J. Hypertens. 2014, 32, 207–215. [Google Scholar] [CrossRef]
- Chen, H.S.; Liu, C.H.; Wu, W.C.; Tseng, H.J.; Lee, Y.S. Optical coherence tomography angiography of the superficial microvasculature in the macular and peripapillary areas in glaucomatous and healthy eyes. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3637–3645. [Google Scholar] [CrossRef]
- Ang, M.; Tan, A.C.S.; Cheung, C.M.G. Optical coherence tomography angiography: A review of current and future clinical applications. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 256, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.C.S.; Tan, G.S.; Denniston, A.K.; Keane, P.A.; Ang, M.; Milea, D.; Chakravarthy, U.; Cheung, C.M.G. An overview of the clinical applications of optical coherence tomography angiography. Eye 2018, 32, 262–286. [Google Scholar] [CrossRef]
- Lee, W.H.; Park, J.H.; Won, Y.; Lee, M.W.; Shin, Y.I.; Jo, Y.J.; Kim, J.Y. Retinal microvascular change in hypertension as measured by optical coherence tomography angiography. Sci. Rep. 2019, 9, 156. [Google Scholar] [CrossRef]
- Yoshikawa, Y.; Shoji, T.; Kanno, J.; Ibuki, H.; Ozaki, K.; Ishii, H.; Ichikawa, Y.; Kimura, I.; Shinoda, K. Evaluation of microvascular changes in the macular area of eyes with rhegmatogenous retinal detachment without macular involvement using swept-source optical coherence tomography angiography. Clin. Ophthalmol. 2018, 12, 2059–2067. [Google Scholar] [CrossRef]
- Wong, T.; Mitchell, P. Hypertensive Retinopathy. N. Engl. J. Med. 2004, 351, 2310–2317. [Google Scholar] [CrossRef]
- Wolf, S.; Arend, O.; Schulte, K.; Ittel, T.H.; Reim, M. Quantification of Retinal Capillary Density and Flow Velocity in Patients with Essential Hypertension. Hypertension 1994, 4, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Hua, D.; Xu, Y.; Zeng, X.; Yang, N.; Jiang, M.; Zhang, X.; Yang, J.; He, T.; Xing, Y. Use of optical coherence tomography angiography for assessment of microvascular changes in the macula and optic nerve head in hypertensive patients without hypertensive retinopathy. Microvasc. Res. 2020, 129, 103969. [Google Scholar] [CrossRef] [PubMed]
- Zeng, R.; Garg, I.; Bannai, D.; Kasetty, M.; Katz, R.; Park, J.Y.; Lizano, P.; Miller, J.B. Retinal Microvasculature and vasoreactivity changes in hypertension using optical coherence tomography-angiography. Graefe’s Arch. Clin. Exp. Ophthalmol. 2022, 260, 3503–3515. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.; Hu, Y.; Huang, M.; Wu, Y.; Zhong, P.; Dong, X.; Wu, Q.; Liu, B.; Li, C.; Xie, J.; et al. Retinal neurovascular impairment in patients with essential hypertension: An optical coherence tomography angiography study. Investig. Ophthalmol. Vis. Sci. 2020, 61, 42. [Google Scholar] [CrossRef] [PubMed]
- Chua, J.; Chin, C.W.L.; Hong, J.; Chee, M.L.; Le, T.T.; Ting, D.S.W.; Wong, T.Y.; Schmetterer, L. Impact of hypertension on retinal capillary microvasculature using optical coherence tomographic angiography. J. Hypertens. 2019, 37, 572–580. [Google Scholar] [CrossRef]
- Donati, S.; Maresca, A.M.; Cattaneo, J.; Grossi, A.; Mazzola, M.; Caprani, S.M.; Premoli, L.; Docchio, F.; Rizzoni, D.; Guasti, L.; et al. Optical coherence tomography angiography and arterial hypertension: A role in identifying subclinical microvascular damage? Eur. J. Ophthalmol. 2021, 31, 158–165. [Google Scholar] [CrossRef]
- Remolí Sargues, L.; Monferrer Adsuara, C.; Castro Navarro, V.; Navarro Palop, C.; Montero Hernández, J.; Cervera Taulet, E. Swept-source optical coherence tomography angiography automatic analysis of microvascular changes secondary to systemic hypertension. Eur. J. Ophthalmol. 2022, 33, 1452–1458. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Sun, H.; Huang, X.; Qu, Y. Retinal microvascular metrics in untreated essential hypertensives using optical coherence tomography angiography. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Ladores, C.; Hong, J.; Nguyen, D.Q.; Chua, J.; Ting, D.; Schmetterer, L.; Wong, T.Y.; Cheng, C.Y.; Tan, A.C.S. Systemic hypertension associated retinal microvascular changes can be detected with optical coherence tomography angiography. Sci. Rep. 2020, 10, 9580. [Google Scholar] [CrossRef]
- Pascual-Prieto, J.; Burgos-Blasco, B.; Ávila Sánchez-Torija, M.; Fernández-Vigo, J.I.; Arriola-Villalobos, P.; Barbero Pedraz, M.A.; García-Feijoo, J.; Martínez-de-la-Casa, J.M. Utility of optical coherence tomography angiography in detecting vascular retinal damage caused by arterial hypertension. Eur. J. Ophthalmol. 2020, 30, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Terheyden, J.H.; Wintergerst, M.W.M.; Pizarro, C.; Pfau, M.; Turski, G.N.; Holz, F.G.; Finger, R.P. Retinal and Choroidal Capillary Perfusion Are Reduced in Hypertensive Crisis Irrespective of Retinopathy. Transl. Vis Sci Technol. 2020, 9, 42. [Google Scholar] [CrossRef]
- Lim, H.B.; Lee, M.W.; Park, J.H.; Kim, K.; Jo, Y.J.; Kim, J.Y. Changes in ganglion cell-inner plexiform layer thickness and retinal microvasculature in hypertension: An optical coherence tomography angiography study. Am. J. Ophthalmol. 2019, 199, 167–176. [Google Scholar] [CrossRef]
- Shin, Y.I.; Nam, K.Y.; Lee, W.H.; Ryu, C.K.; Lim, H.B.; Jo, Y.J.; Kim, J.Y. Peripapillary microvascular changes in patients with systemic hypertension: An optical coherence tomography angiography study. Sci. Rep. 2020, 10, 6541. [Google Scholar] [CrossRef]
- Takayama, K.; Kaneko, H.; Ito, Y.; Kataoka, K.; Iwase, T.; Yasuma, T.; Matsuura, T.; Tsunekawa, T.; Shimizu, H.; Suzumura, A.; et al. Novel classification of early-stage systemic hypertensive changes in human retina based on OCTA measurement of choriocapillaris. Sci. Rep. 2018, 8, 15163. [Google Scholar] [CrossRef]
- Chua, J.; Le, T.T.; Sim, Y.C.; Chye, H.Y.; Tan, B.; Yao, X.; Wong, D.; Ang, B.W.Y.; Toh, D.F.; Lim, H.; et al. Relationship of quantitative retinal capillary network and myocardial remodeling in systemic hypertension. J. Am. Heart. Assoc. 2022, 11, e024226. [Google Scholar] [CrossRef]
- Tabatabaee, A.; Asharin, M.R.; Dehghan, M.H.; Pourbehi, M.R.; Nasiri-Ahmadabadi, M.; Assadi, M. Retinal vessel abnormalities predict coronary artery diseases. Perfusion 2013, 28, 232–237. [Google Scholar] [CrossRef]
- Wong, T.Y.; Klein, R.; Sharrett, A.R.; Duncan, B.B.; Couper, D.J.; Tielsch, J.M.; Klein, B.E.; Hubbard, L.D. Retinal arteriolar narrowing and risk of coronary heart disease in men and women. The Atherosclerosis Risk in Communities Study. JAMA 2002, 287, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Jiang, J.; Zhang, Y.; Qian, Y.W.; Zhang, J.F.; Wang, Z.L. Retinal and choroidal vascular changes in coronary heart disease: An optical coherence tomography angiography study. Biomed. Opt. Express 2019, 10, 1532–1544. [Google Scholar] [CrossRef] [PubMed]
- Aschauer, J.; Aschauer, S.; Pollreisz, A.; Datlinger, F.; Gatterer, C.; Mylonas, G.; Egner, B.; Hofer, D.; Steiner, I.; Hengstenberg, C.; et al. Identification of subclinical microvascular biomarkers in coronary heart disease in retinal imaging. Transl. Vis. Sci. Technol. 2021, 10, 24. [Google Scholar] [CrossRef] [PubMed]
- Matulevičiūtė, I.; Sidaraitė, A.; Tatarūnas, V.; Veikutienė, A.; Dobilienė, O.; Žaliūnienė, D. Retinal and Choroidal Thinning-A Predictor of Coronary Artery Occlusion? Diagnostics 2022, 12, 2016. [Google Scholar] [CrossRef] [PubMed]
- Sideri, A.M.; Kanakis, M.; Katsimpris, A.; Karamaounas, A.; Brouzas, D.; Petrou, P.; Papakonstaninou, E.; Droutsas, K.; Kandarakis, S.; Giannopoulos, G.; et al. Correlation between coronary and retinal microangiopathy in patients with STEMI. Transl. Vis. Sci. Technol. 2023, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Arnould, L.; Guenancia, C.; Azemar, A.; Alan, G.; Pitois, S.; Bichat, F.; Zeller, M.; Gabrielle, P.H.; Bron, A.M.; Creuzot-Garcher, C.; et al. The EYE-MI Pilot Study: A Prospective Acute Coronary Syndrome Cohort Evaluated With Retinal Optical Coherence Tomography Angiography. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4299–4306. [Google Scholar] [CrossRef] [PubMed]
- Zhong, P.; Hu, Y.; Jiang, L.; Peng, Q.; Huang, M.; Li, C.; Kuang, Y.; Tan, N.; Yu, H.; Yang, X. Retinal microvasculature changes in patients with coronary total occlusion on optical coherence tomography angiography. Front. Med. 2021, 8, 708491. [Google Scholar] [CrossRef]
- Ren, Y.; Hu, Y.; Li, C.; Zhong, P.; Liu, H.; Wang, H.; Kuang, Y.; Fu, B.; Wang, Y.; Zhao, H.; et al. Impaired retinal microcirculation in patients with non-obstructive coronary artery disease. Microvasc. Res. 2023, 148, 104533. [Google Scholar] [CrossRef]
- Arnould, L.; Guenancia, C.; Gabrielle, P.H.; Pitois, S.; Baudin, F.; Pommier, T.; Zeller, M.; Bron, A.M.; Creuzot-Garcher, C.; Cottin, Y. Influence of cardiac hemodynamic variables on retinal vessel density measurement on optical coherence tomography angiography in patients with myocardial infarction. J. Fr. Ophtalmol. 2020, 43, 216–221. [Google Scholar] [CrossRef]
- London, A.; Benhar, I.; Schwartz, M. The retina as a window to the brain-from eye research to CNS disorders. Nat. Rev. Neurol. 2013, 9, 44–53. [Google Scholar] [CrossRef]
- Zafar, S.; McCormick, J.; Giancardo, L.; Saidha, S.; Abraham, A.; Channa, R. Retinal imaging for neurological diseases: “A window into the brain”. Int. Ophthalmol. Clin. 2019, 59, 137–154. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Wang, H.; Yang, X.; Jiang, B.; Li, H.; Wang, Y. Multimodal Retinal Imaging for Detection of Ischemic Stroke. Front. Aging Neurosci. 2021, 13, 615813. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Y.; Klein, R.; Couper, D.J.; Cooper, L.S.; Shahar, E.; Hubbard, L.D.; Wofford, M.R.; Sharrett, A.R. Retinal microvascular abnormalities and incident stroke: The atherosclerosis risk in communities study. Lancet 2001, 358, 1134–1140. [Google Scholar] [CrossRef]
- Mitchell, P.; Wang, J.J.; Wong, T.Y.; Smith, W.; Klein, R.; Leeder, S.R. Retinal microvascular signs and risk of stroke and stroke mortality. Neurology 2005, 65, 1005–1009. [Google Scholar] [CrossRef]
- Seidelmann, S.B.; Claggett, B.; Bravo, P.E.; Gupta, A.; Farhad, H.; Klein, B.E.; Klein, R.; Di Carli, M.; Solomon, S.D. Retinal Vessel Calibers in Predicting Long-Term Cardiovascular Outcomes: The Atherosclerosis Risk in Communities Study. Circulation 2016, 134, 1328–1338. [Google Scholar] [CrossRef]
- McGrory, S.; Ballerini, L.; Doubal, F.N.; Staals, J.; Allerhand, M.; Valdes-Hernandez, M.D.C.; Wang, X.; MacGillivray, T.; Doney, A.S.F.; Dhillon, B.; et al. Retinal microvasculature and cerebral small vessel disease in the Lothian Birth Cohort 1936 and Mild Stroke Study. Sci. Rep. 2019, 9, 6320. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Jiang, B.; Li, H.; Yang, X.; Cheng, X.; Hong, H.; Wang, Y. Risk Stratification Tool for Ischemic Stroke: A Risk Assessment Model Based on Traditional Risk Factors Combined With White Matter Lesions and Retinal Vascular Caliber. Front. Neurol. 2021, 12, 696986. [Google Scholar] [CrossRef]
- Zhang, Y.; Shi, C.; Chen, Y.; Wang, W.; Huang, S.; Han, Z.; Lin, X.; Lu, F.; Shen, M. Retinal Structural and Microvascular Alterations in Different Acute Ischemic Stroke Subtypes. J. Ophthalmol. 2020, 2020, 8850309. [Google Scholar] [CrossRef]
- Duan, H.; Xie, J.; Zhou, Y.; Zhang, H.; Liu, Y.; Tang, C.; Zhao, Y.; Qi, H. Characterization of the Retinal Microvasculature and FAZ Changes in Ischemic Stroke and Its Different Types. Transl. Vis. Sci. Technol. 2022, 11, 21. [Google Scholar] [CrossRef]
- Cao, Y.; Yan, J.; Zhan, Z.; Liang, Y.; Han, Z. Macula structure and microvascular changes in recent small subcortical infarct patients. Front. Neurol. 2021, 11, 615252. [Google Scholar] [CrossRef]
- Ye, C.; Kwapong, W.R.; Tao, W.; Lu, K.; Pan, R.; Wang, A.; Liu, J.; Liu, M.; Wu, B. Characterization of macular structural and microvascular changes in thalamic infarction patients: A swept-source optical coherence tomography-angiography study. Brain Sci. 2022, 12, 518. [Google Scholar] [CrossRef]
- Molero-Senosiain, M.; Vidal-Villegas, B.; Pascual-Prieto, J.; Valor-Suarez, C.; Saenz-Frances, F.; Santos-Bueso, E. Correlation between retrograde trans-synaptic degeneration of ganglion cells and optical coherence tomography angiography following ischemic stroke. Cureus 2021, 13, e19788. [Google Scholar] [CrossRef]
- Liang, Y.; Liu, B.; Xiao, Y.; Zeng, X.; Wu, G.; Du, Z.; Fang, Y.; Hu, Y.; Yang, X.; Yu, H. Retinal neurovascular changes in patients with ischemic stroke investigated by optical coherence tomography angiography. Front. Aging Neurosci. 2022, 14, 834560. [Google Scholar] [CrossRef]
- Lu, K.; Kwapong, W.R.; Jiang, S.; Zhang, X.; Xie, J.; Ye, C.; Yan, Y.; Cao, L.; Zhao, Y.; Wu, B. Differences in retinal microvasculature between large artery atherosclerosis and small artery disease: An optical coherence tomography angiography study. Front. Aging Neurosci. 2022, 14, 1053638. [Google Scholar] [CrossRef]
- Jessup, M.; Brozena, S. Medical progress: Heart failure. N. Engl. J. Med. 2003, 348, 2007–2018. [Google Scholar] [CrossRef]
- Gavin, J.B.; Maxwell, L.; Edgar, S.G. Microvascular involvement in cardiac pathology. J. Mol. Cell Cardiol. 1998, 30, 2531–2540. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.P.; Mak, S.; Stewart, D.J. Potential role of the microvasculature in progression of heart failure. Am. J. Cardiol. 1999, 84, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Almeida, O.P.; Flicker, L. The mind of a failing heart: A systematic review of the association between congestive heart failure and cognitive functioning. Intern Med. J. 2001, 31, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Zelis, R.; Sinoway, L.I.; Musch, T.I.; Davis, D.; Just, H. Regional blood flow in congestive heart failure:concept of compensatory mechanisms with short and long time constants. Am. J. Cardiol. 1988, 62, 2–8. [Google Scholar] [CrossRef]
- Saha, M.; Muppala, M.R.; Castaldo, J.E.; Gee, W.; Reed, J.F., 3rd; Morris, D.L. The impact of cardiac index on cerebral hemodynamics. Stroke 1993, 24, 1686–1690. [Google Scholar] [CrossRef]
- Choi, B.R.; Kim, J.S.; Yang, Y.J.; Park, K.M.; Lee, C.W.; Kim, Y.H.; Hong, M.K.; Song, J.K.; Park, S.W.; Park, S.J.; et al. Factors associated with decreased cerebral blood flow in congestive heart failure secondary to idiopathic dilated cardiomyopathy. Am. J. Cardiol. 2006, 97, 1365–1369. [Google Scholar] [CrossRef] [PubMed]
- Meira-Freitas, D.; Melo, L.A., Jr.; Almeida-Freitas, D.B.; Paranhos, A., Jr. Glaucomatous optic nerve head alterations in patients with chronic heart failure. Clin. Ophthalmol. 2012, 6, 623. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Altinkaynak, H.; Kara, N.; Sayın, N.; Güneş, H.; Avşar, S.; Yazıcı, A.T. Subfoveal choroidal thickness in patients with chronic heart failure analyzed by spectral-domain optical coherence tomography. Curr. Eye Res. 2014, 39, 1123–1128. [Google Scholar] [CrossRef]
- Topaloglu, C.; Bekmez, S. Retinal vascular density change in patients with heart failure. Photodiagnosis Photodyn Ther. 2023, 42, 103621. [Google Scholar] [CrossRef]
- Alnawaiseh, M.; Eckardt, F.; Mihailovic, N.; Frommeyer, G.; Diener, R.; Rosenberger, F.; Eckardt, L.; Eter, N.; Lahme, L.; Lange, P.S. Ocular perfusion in patients with reduced left ventricular ejection fraction measured by optical coherence tomography angiography. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 3605–3611. [Google Scholar] [CrossRef]
- Rakusiewicz, K.; Kanigowska, K.; Hautz, W.; Ziółkowska, L. The Impact of Chronic Heart Failure on Retinal Vessel Density Assessed by Optical Coherence Tomography Angiography in Children with Dilated Cardiomyopathy. J. Clin. Med. 2021, 10, 2659. [Google Scholar] [CrossRef] [PubMed]
- Chaikijurajai, T.; Ehlers, J.P.; Tang, W.H. Retinal microvasculature: A potential window into heart failure prevention. JACC Heart Fail. 2022, 10, 785–791. [Google Scholar] [CrossRef] [PubMed]
| OCTA Device | Control Subjects/ Healthy | Patients Subject with Systemic HTN | Anatomic Region of the Retina with Capillary Dropout | OCTA Derived Parameter | Region of Interest/ Scan Type | Estimated Percentage of Dropout | |
|---|---|---|---|---|---|---|---|
| Zeng et al. [18] | Zeiss CIRRUSTM HD-OCT Model 5000; Carl Zeiss Meditec Inc., Dublin, CA, USA | 17 | 24 | SCP | VD (%) | Macula (6 × 6 mm centered on fovea) | −2.86% |
| Terhedyen et al. [26] | Zeiss PLEX Elite 9000; Carl Zeiss Meditec, Dublin, CA, USA | 31 | 28 | DRL | VD (%) | Macula (cube of 3 × 3 mm centered on macula) | −16.50% |
| Sun et al. [24] | AngioVue: Optovue, Inc., Fremont, CA, USA | 46 | 94 | SVP, DVP | Macular Flow | Macula (6 × 6 mm centered on the fovea) | −23.33% (SVP) −9.60% (DVP) |
| Pascual-Prieto et al. [25] | RS-3000 AOCT Nidek Co., Gamagori, Japan | 26 | 23 | SCP, DCP | Macula perfusion density (%) | Macula (4.5 × 4.5 mm centered on fovea) | −11.46% (SCP) −4.88% (DCP) |
| Lee et al. [13] | Cirrus HD-OCT 5000 instrument (Carl Zeiss Meditec, Dublin, CA, USA) with AngioPlex software (ver.10.0; Carl Zeiss Meditec, Jena, Germany) | 50 | 45 | SRL | VD (%) | Macula (3 × 3 mm scan centered on the macula) Inner ring: (between a 1 and 3 mm diameter centered on the macula) | −5.85% |
| Macula (3 × 3 mm scan centered on the macula) 3 mm full: 3 mm diameter centered on the macula | 3.61% | ||||||
| Hua et al. [17] | OCTA using prototype AngioVue, software within the AngioVue device (RTVue XR Avanti with AngioVue, Optovue Inc., Fremont, CA, USA) | 40 | 22 | SVP | VD (%) | Macula (3.0 × 3.0-mm) Parafovea: (3 mm diameter circle centered on the macula) | −7.33% |
| Chua et al. [20] | AngioVue (Optovue, Inc., Fremont, CA, USA). | 59 (well controlled BP) | 18 | DVP | Retinal Capillary Density (%) | Macula (6.0 × 6.0 mm2 field of view centered on the fovea) | −21.61% |
| Donati et al. [21] | AngioVue System on the RTVue XR Avanti device (Optovue, Inc., Fremont, CA, USA) | 30 | 30 | DVP | VD (%) | Macula (3 × 3 mm2 area) Parafoveal area (whole image minus foveal area). | −2.15% |
| Whole macula (3 × 3 mm2 square area) | −2.33% | ||||||
| Lim et al. [27] | Zeiss Cirrus 5000 system (Carl Zeiss Meditec, Dublin, CA, USA) | 117 | 52 | SRL | VD (mm−1) | Macula (3 × 3 mm scan): 3 mm total area | −3.98% |
| Peng et al. [19] | RTVue-XR Avanti OCT System; Optovue, Inc., Fremont, CA, USA | 30 | 113 | SVP DVP | VD (%) | Macula (mean 6 × 6-mm2 ) | −1.76 (SRL) −4.43% (DRL) |
| Parafoveal area (a concentric circle 1 mm to the fovea) | −2.41% (SRL) −4.36% (DRL) | ||||||
| Sargues et al. [22] | Swept Source OCTA: SS-OCT Triton (Topcon, Tokyo, Japan) with automated OCTARA (OCT Angiography Ratio Analysis) algorithm provided by the device | 71 | 93 | DCP | VD (%) | Macula (4.5 × 4.5 mm) Parafovea (between external ring of 2.5 mm of diameter and a central area of 1 mm of diameter). | −1.54% |
| Xu et al. [23] | AngioVue system on the Avanti Spectral Domain OCT device (Optovue RTVue XR Avanti; Optovue Inc., Fremont, CA, USA). | 79 | 137 | DRL | VD (%) | Macula (6 × 6 mm) centered at the fovea | −9.69% |
| OCTA Device | Control Subject/Healthy | Patients Subject with CAD | Anatomic Region of the Retina with Capillary Dropout | OCTA Derived Parameter | Region of Interest/ Scan Type | Estimated Percentage of Dropout | |
|---|---|---|---|---|---|---|---|
| Matuleviciute et al. [35] | OCT DRI OCT Triton (Topcon, Tokyo, Japan) | 82 | 26 (3 vessel disease, 76 MI) | SCP, DCP | VD (%) | Macula (3 × 3 and 6 × 6 mm images of central macular area) | Data presented as OR |
| Aschauer et al. [34] | PLEX Elite 9000 (Carl Zeiss Meditec) | 18 | 27 | SCP, DCP | VD (%) | Macula (6 × 6 fovea centered) | Raw data not presented |
| Arnould et al. [37] | CIRRUS HD-OCT, Model 5000; Carl Zeiss Meditec AG with Angiography software (Angioplex, version 10; Carl Zeiss Meditec AG) | 44 | 237 CAD | SCP | VD (%) | Macula (3 × 3 mm) | Raw data not presented |
| Zhong et al. [38] | RTVue-XR Avanti; Optovue, Fremont, CA, USA | 116 | 102 CTO with CAD | SRL | VD (%) | Macula mean (6 × 6 mm2) | −4.17% |
| Parafoveal (area between 1–3 mm concentric ring centered on the fovea) | −5.67% | ||||||
| Ren et al. [39] | AngioVue (RTVue-XR Avanti; Optovue, Fremont, CA, USA | 58 | 62 (OCAD) | SVP, DVP | VD (%) | Parafoveal (region between the 1–3 mm concentric ring center of the fovea) | −13.14% (SVP) −9.55% (DVP) |
| Macula whole (6 × 6 mm2) | −11.93% (SVP) −13.85% (DVP) | ||||||
| Sideri et al. [36] | DRI OCT Triton Swept Source Optical Coherence Tomograh (Topcon, Tokyo, Japan). | 77 | 88 | SCP, DCP | VD (%) | Macula (3 × 3 mm centered on the fovea) perifoveal (are between the 1–3 mm) | Complete raw data not provided for control group |
| OCTA Device | Control Subject/Healthy | Patients Subject with Ischemic Stroke | Anatomic Region of the Retina with Capillary Dropout | OCTA Derived Parameter | Region of Interest/ Scan Type | Estimated Percentage of Dropout | |
|---|---|---|---|---|---|---|---|
| Duan et al. [50] | AngioVue, RTVue XR Avanti spectral domain OCT, Optovue, Fremont, CA, USA | 43 | 52 | DRL | Vascular Area Density | Macula (3 × 3 centered at the fovea) | Data presented as OR |
| Cao et al. [51] | Avanti RTVue-XR tool (Optovue, Fremont, CA, USA;) | 46 | 40 | SRCP, DRCP | VD (%) | Macula (information not provided; whole) | −4.83% (SRCP) −6.26% (DRCP) |
| Zhang et al. [49] | RTVue XR with AngioVue (software version 2017.1.0.155; Optovue, Inc., Fremont, CA, USA). | 65 | 69 | DCP | VD (%) | Macula (3 × 3 mm2 around the fovea) | −3.98% (LAA) −2.73% (SAA) |
| Ye et al. [52] | VG 200; SVision Imaging Limited Luoyang, China) | 31 | 35 | SVP | VD (%) | Macula (3 × 3 mm annulus around the fovea) | Raw data not provided |
| Molero-Senosiain et al. [53] | RS-3000, Nidek Co. | 50 | 15 | RPCP + SCP + IPR, DCP | VD (%) | Macula (4.5 × 4.5 mm) | −24.93% (RPCP + SCP + IPR) −33.82% (DVP) |
| Liang et al. [54] | RTVue-XR Avanti; Optovue | 109 | 159 | SCP, DCP | VD (%) | Whole macula (6 × 6 mm2) | −3.82% (SCP) −6.03 (DCP) |
| Parafovea (1- to 3 mm annulus foveal region) | −5.13 (SCP) −5.04 (DCP) |
| OCTA Device | Control Subjects/ Healthy | Patients Subject with CHF | Anatomic Region of the Retina with Capillary Dropout | OCTA Derived Parameter | Region of Interest/ Scan Type | Estimated Percentage of Dropout | |
|---|---|---|---|---|---|---|---|
| Rakusiewicz et al. [67] | RTVue-XR (Angiovue; Optovue Inc., Fremont, CA, USA). | 30 | 30 | SCP | VD (%) | Whole macula (3 × 3 mm area centered at fovea) | −7.28% |
| Parafoveal (ring with an internal diameter of 1 mm and external of 3 mm) | −6.23% | ||||||
| Topaloglu et al. [65] | DRI OCT (Triton, Topcon, Tokyo, Japan) | 36 | 18 (NYHA III) | DCP | Capillary Plexus Perfusion | Macula (3 × 3 mm2) | −15.27% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kellner, R.L.; Harris, A.; Ciulla, L.; Guidoboni, G.; Verticchio Vercellin, A.; Oddone, F.; Carnevale, C.; Zaid, M.; Antman, G.; Kuvin, J.T.; et al. The Eye as the Window to the Heart: Optical Coherence Tomography Angiography Biomarkers as Indicators of Cardiovascular Disease. J. Clin. Med. 2024, 13, 829. https://doi.org/10.3390/jcm13030829
Kellner RL, Harris A, Ciulla L, Guidoboni G, Verticchio Vercellin A, Oddone F, Carnevale C, Zaid M, Antman G, Kuvin JT, et al. The Eye as the Window to the Heart: Optical Coherence Tomography Angiography Biomarkers as Indicators of Cardiovascular Disease. Journal of Clinical Medicine. 2024; 13(3):829. https://doi.org/10.3390/jcm13030829
Chicago/Turabian StyleKellner, Rebecca L., Alon Harris, Lauren Ciulla, Giovanna Guidoboni, Alice Verticchio Vercellin, Francesco Oddone, Carmela Carnevale, Mohamed Zaid, Gal Antman, Jeffrey T. Kuvin, and et al. 2024. "The Eye as the Window to the Heart: Optical Coherence Tomography Angiography Biomarkers as Indicators of Cardiovascular Disease" Journal of Clinical Medicine 13, no. 3: 829. https://doi.org/10.3390/jcm13030829
APA StyleKellner, R. L., Harris, A., Ciulla, L., Guidoboni, G., Verticchio Vercellin, A., Oddone, F., Carnevale, C., Zaid, M., Antman, G., Kuvin, J. T., & Siesky, B. (2024). The Eye as the Window to the Heart: Optical Coherence Tomography Angiography Biomarkers as Indicators of Cardiovascular Disease. Journal of Clinical Medicine, 13(3), 829. https://doi.org/10.3390/jcm13030829









