Analgesic Efficacy of Oxycodone in Postoperative Dressings after Surgical Treatment of Burn Wounds: A Randomised Controlled Trial
Abstract
1. Introduction
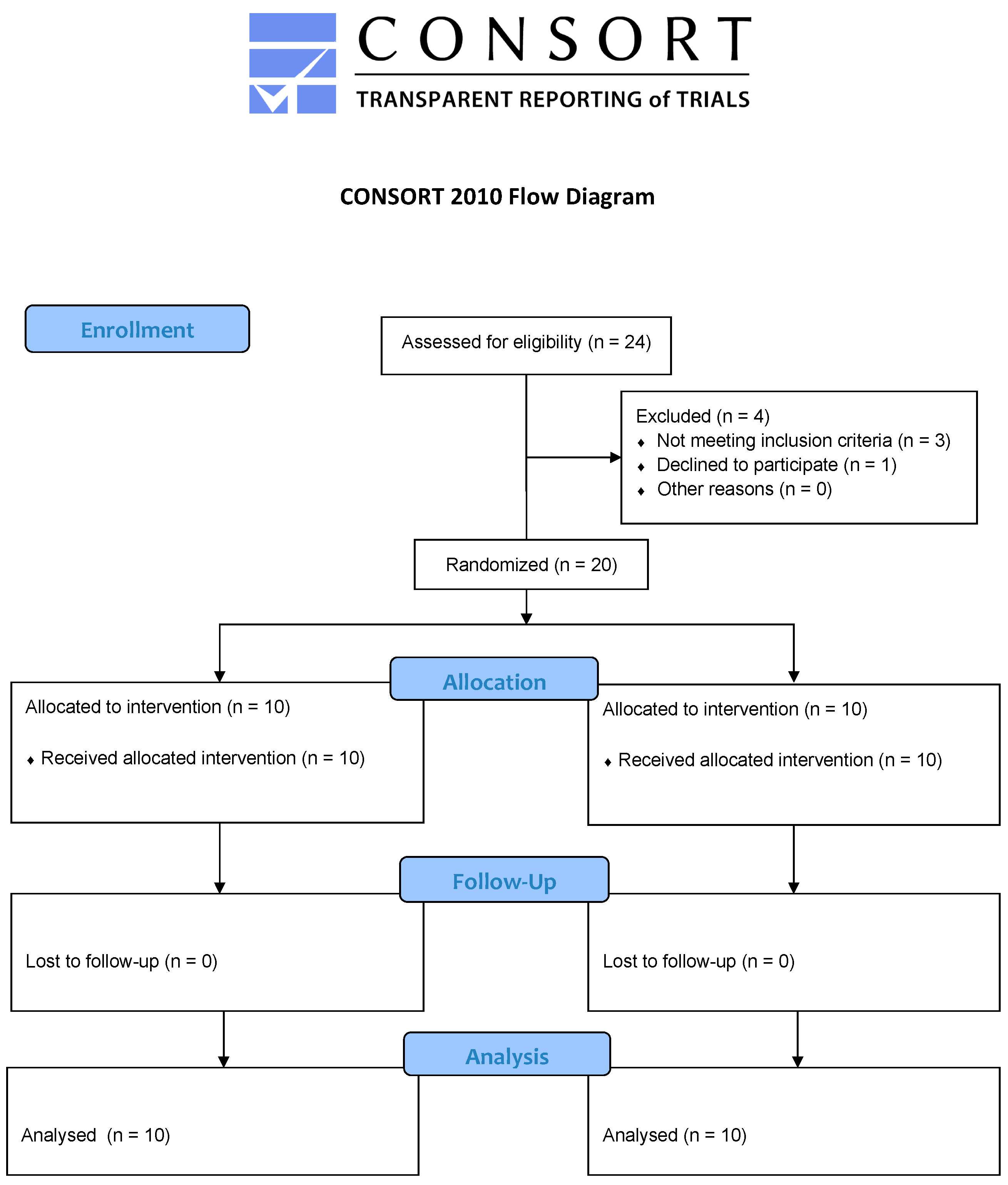
2. Materials and Methods
Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rowan, M.P.; Cancio, L.C.; Elster, E.A.; Burmeister, D.M.; Rose, L.F.; Natesan, S.; Chan, R.K.; Christy, R.J.; Chung, K.K. Burn wound healing and treatment: Review and advancements. Crit. Care 2015, 19, 243. [Google Scholar] [CrossRef] [PubMed]
- Retrouvey, H.; Shahrokhi, S. Pain and the thermally injured patient—A review of current therapies. J. Burn. Care Res. 2015, 36, 315–323. [Google Scholar] [PubMed]
- Askay, S.W.; Patterson, D.R.; Sharar, S.R.; Mason, S.; Faber, B. Pain management in patients with burn injuries. Int. Rev. Psychiatry 2009, 21, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.; Upton, D.; Rippon, M. Treatment for wound pruritus following burns. J. Wound Care 2014, 23, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Wei, L. The application of moist dressing in treating burn wound. Open Med. Wars 2015, 10, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Markiewicz-Gospodarek, A.; Kozioł, M.; Tobiasz, M.; Baj, J.; Radzikowska-Büchner, E.; Przekora, A. Burn wound healing: Clinical complications, medical care, treatment, and dressing types: The current state of knowledge for clinical practice. Int. J. Environ. Res. Public Health 2022, 19, 1338. [Google Scholar] [CrossRef] [PubMed]
- Romanowski, K.S.; Carson, J.; Pape, K.; Bernal, E.; Sharar, S.; Wiechman, S.; Carter, D.; Liu, Y.M.; Nitzschke, S.; Bhalla, P.; et al. American Burn Association guidelines on the management of acute pain in the adult burn patient: A review of the literature, a compilation of expert opinion, and next steps. J. Burn. Care Res. 2020, 41, 1129–1151. [Google Scholar] [CrossRef] [PubMed]
- Roy, T.K.; Uniyal, A.; Akhilesh, T.V. Multifactorial pathways in burn injury-induced chronic pain: Novel targets and their pharmacological modulation. Mol. Biol. Rep. 2022, 49, 12121–12132. [Google Scholar] [CrossRef]
- Guichard, L.; Hirve, A.; Demiri, M.; Martinez, V. Opioid-induced hyperalgesia in patients with chronic pain: A systematic review of published cases. Clin. J. Pain. 2022, 38, 49–57. [Google Scholar] [CrossRef]
- Bechert, K.; Abraham, S.E. Pain Management and Wound Care. J. Am. Col. Certif. Wound Spec. 2009, 1, 65–71. [Google Scholar] [CrossRef]
- Subrahmanyam, M. Topical Application of Honey for Burn Wound Treatment—An Overview. Ann. Burn. Fire Disasters 2007, 20, 137–139. [Google Scholar]
- Church, D.; Elsayed, S.; Reid, O.; Wilson, B.; Lindsay, R. Burn Wound Infections. Clin. Microbiol. Rev. 2006, 19, 403–434. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, R. Management of painful wounds in advanced disease. Can. Fam. Physician 2010, 56, 883–885. [Google Scholar] [PubMed]
- Twillman, R.K.; Long, T.D.; Cathers, T.A.; Mueller, D.W. Treatment of painful skin ulcers with topical opioids. J. Pain. Symptom Manag. 1999, 17, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Łapot, K.; Sopata, M.J.; Kotlińska-Lemieszek, A. Topical use of morphine in palliative care patients–a report of two cases. Med. Paliatywna/Palliat. Med. 2016, 8, 144–148. [Google Scholar]
- Stein, C.; Kuchler, S. Non–analgesic effects of opioids: Peripheral opioid effects on inflammation and wound healing. Curr. Pharm. Des. 2012, 18, 6053–6069. [Google Scholar] [CrossRef] [PubMed]
- Ballas, S.K. Treatment of painful sickle cell leg ulcers with topical opioids. Blood 2002, 99, 1096. [Google Scholar] [CrossRef] [PubMed]
- Da Silva Costa, F.L.; Tiussi, L.D.; Nascimento, M.S.; de Souza Correa, A.C.; Yasojima, E.Y.; Avelar Pires, C.A. Diclofenac topical gel in excision wounds maintain quality and reduce phlogistic signals. Acta Cir. Bras. 2014, 29, 328–333. [Google Scholar] [CrossRef]
- Graham, T.; Grocott, P.; Probst, S.; Wanklyn, S.; Dawson, J.; Gethin, G. How are topical opioids used to manage painful cutaneous lesions in palliative care? A critical review. Pain 2013, 154, 1920–1928. [Google Scholar] [CrossRef]
- Watanabe, C.; Komiyama, A.; Yoshizumi, M.; Sakurada, S.; Mizoguchi, H. Morphine antinociception restored by use of methadone in the morphine-resistant inflammatory pain state. Front. Pharmacol. 2020, 11, 593647. [Google Scholar] [CrossRef]
- Marovino, E.; Morgillo, A.; Mazzarella, M.; Randazzo, M.F. Methadone: From Chronic Non-Oncological pain and primary Management of Opioid Hyperalgesia to Disassuefaction of Painkillers Abuse. Qeios 2022. Available online: https://www.qeios.com/read/ABG3ZQ.2 (accessed on 9 January 2024).
- Carlson, A.; Pham, D.; Price, C.; Reisch, J.; Iskander, I.; Ambardekar, A. Intraoperative Methadone Use in Pediatric Burn Patients. J. Burn. Care Res. 2022, 43, 1294–1298. [Google Scholar] [CrossRef] [PubMed]
- Finlayson, K.; Teleni, L.; McCarthy, A.L. Topical Opioids and Antimicrobials for the Management of Pain, Infection, and Infection–Related Odors in Malignant Wounds: A systematic Review. Oncol. Nurs. Forum 2017, 44, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, R.E.; Arndt, D.R.; Hunt, K.L. Analgesic Effects of Topical Methadone. A Rep. Four Cases. Clin. J. Pain. 2005, 21, 190–192. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.Y.; Miller, J.L.; Henry, E.; Heltsley, R.; Woo, S.; Johnson, P.N. Analysis of fentanyl pharmacokinetics, and its sedative effects and tolerance in critically ill children. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2021, 41, 359–369. [Google Scholar] [CrossRef]
- Stapelberg, F. Challenges in anaesthesia and pain management for burn injuries. Anaesth. Intensive Care 2020, 48, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.F.; Huang, Y.H.; Lai, H.C.; Wu, Z.F. Analgesia/Nociception Index May Not Be an Ideal Surrogate Postoperative Pain Measurement Tool for Burn Injury Patients Undergoing Propofol-Based General Anesthesia. J. Med. Sci. 2020, 40, 299–300. [Google Scholar]
- Gencer, M.; Sezen, O. A study comparing the effect of premedication with intravenous midazolam or dexmedetomidine on ketamine-fentanyl sedoanalgesia in burn patients: A randomized clinical trial. Burns 2021, 47, 101–109. [Google Scholar] [CrossRef]
- Nosek, K.; Leppert, W.; Puchała, Ł.; Łoń, K. Efficacy and safety of topical morphine: A narrative review. Pharmaceutics 2022, 14, 1499. [Google Scholar] [CrossRef]
- Maida, V.; Corban, J. Topical Medical Cannabis: A New Treatment for Wound Pain—Three Cases of Pyoderma Gangrenosum. J. Pain. Symptom Manag. 2017, 54, 732–736. [Google Scholar] [CrossRef]
- Farley, P. Should topical opioid analgesics be regarded as effective and safe when applied to chronic cutaneous lesions? J. Pharm. Pharmacol. 2011, 63, 747–756. [Google Scholar] [CrossRef]
- Skiveren, J.; Haedersdal, M.; Philipsen, P.A.; Wiegell, S.R.; Wulf, H.C. Morphine Gel 0.3% Does not relieve Pain During Topical Photodynamic Therapy: A randomized, Double–blind, Placebo–controlled Study. Acta Derm. Venereol. 2006, 86, 409–411. [Google Scholar] [CrossRef] [PubMed]
- Watterson, G.; Howard, R.; Goldman, A. Peripheral opioids in inflammatory pain. Arch. Dis. Child. 2004, 89, 679–681. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Vives, R.; Choi, M.S.; Young, M.T.; Over, P.; Ziembicki, J.; Corcos, A.; Gerlach, J.C. Second-degree burns with six etiologies treated with autologous noncultured cell-spray grafting. Burns 2016, 42, e99–e106. [Google Scholar] [CrossRef] [PubMed]
- Tetteh, L.; Aziato, L.; Mensah, G.P.; Vehviläinen-Julkunen, K.; Kwegyir-Afful, E. Burns pain management: The role of nurse–patient communication. Burns 2021, 47, 1416–1423. [Google Scholar] [CrossRef] [PubMed]
- Wibbenmeyer, L.; Eid, A.; Kluesner, K.; Heard, J.; Zimmerman, B.; Kealey, G.P.; Brennan, T. An evaluation of factors related to postoperative pain control in burn patients. J. Burn Care Res. 2015, 36, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Nosanov, L.B.; Brandt, J.L.; Schneider, D.M.; Johnson, L.S. Pain management in burn patients. Curr. Trauma. Rep. 2020, 6, 161–173. [Google Scholar] [CrossRef]
- Emery, M.A.; Eitan, S. Drug-specific differences in the ability of opioids to manage burn pain. Burns 2020, 46, 503–513. [Google Scholar] [CrossRef]
- Duchin, E.R.; Moore, M.; Carrougher, G.J.; Min, E.K.; Gordon, D.B.; Stewart, B.T.; Sabel, J.; Jo-Nes, A.; Pham, T.N. Burn patients’ pain experiences and perceptions. Burns 2021, 47, 1627–1634. [Google Scholar] [CrossRef]
- Olczak, B.; Kowalski, G.; Leppert, W.; Zaporowska–Stachowiak, I.; Wieczorowska–Tobis, K. Analgesic efficacy, adverse effects and safety of oxycodone administered as continuous intravenous infusion in patients after total hip arthroplasty. J. Pain. Res. 2017, 10, 1027–1032. [Google Scholar] [CrossRef]
- Sheridan, R.L.; Stoddard, F.J.; Kazis, L.E.; Lee, A.; Li, N.C.; Kagan, R.J.; Palmieri, T.L.; Meyer, W.J.; Nicolai, M.; Stubbs, T.; et al. Long-term posttraumatic stress symptoms vary inversely with early opiate dosing in children recovering from serious burns: Effects durable at 4 years. J. Trauma Acute Care Surg. 2014, 76, 828–832. [Google Scholar] [CrossRef]
- Shu, F.; Liu, H.; Lou, X.; Zhou, Z.; Zhao, Z.; Liu, Y.; Bai, X.; Luo, P.; Zheng, Y.; Xiao, S.; et al. Analysis of the predictors of hypertrophic scarring pain and neuropathic pain after burn. Burns 2022, 48, 1425–1434. [Google Scholar] [CrossRef] [PubMed]
- Stein, C.; Kuchler, S. Targeting inflammation and wound healing by opioids. Trends Pharmacol. Sci. 2013, 34, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Da Costa Ferreira, S.A.; Serna González, C.V.; Thum, M.; da Costa Faresin, A.A.; Woo, K.; de Gouveia Santos, V.L.C. Topical therapy for pain management in malignant fungating wounds: A scoping review. J. Clin. Nurs. 2023, 32, 3015–3029. [Google Scholar] [CrossRef] [PubMed]
- Fransen, J.; Bastami, S.; Sjoberg, F.; Uppugunduri, S.; Huss, F.R.M. Evaluating topical opioid gel on donor site pain: A small randomized double blind controlled trial. Int. J. Surg. Open 2016, 4, 5–9. [Google Scholar] [CrossRef]
- Rook, J.M.; Hasan, W.; McCarson, K.E. Temporal effects of topical morphine application on cutaneous wound healing. Anesthesiology 2008, 109, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Poonawala, T.; Farooqui, M.; Ericson, M.E.; Gupta, K. Topical fentanyl stimulates healing of ischemic wounds in diabetic rats. J. Diabetes 2015, 7, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Ondrovics, M.; Hoelbl–Kovacic, A.; Fux, D.A. Opioids: Modulators of angiogenesis in wound healing and cancer. Oncotarget 2017, 8, 25783–25796. [Google Scholar] [CrossRef]
- Gupta, K.; Poonwala, T.; Leva–Young, B.K.; Ericson, M.E.; Ammbashankar, N.S.; Hebbel, R.P. Abnormal Angiogenesis, Neurogenesis and Lymphangiogenesis in the Skin Underlies Delayed Wound Healing in the Sickle Mouse: Acceleration of Healing by Topical Opioids. Blood 2005, 106, 3177. [Google Scholar] [CrossRef]
- Vang, D.; Ericson, M.; Ansonoff, M.A.; Pintar, J.E.; Hebbel, R.P.; Gupta, K. Morphine Stimulates Wound Healing Via Mu Opioid Receptor and Promotes Wound Closure in Sickle Mice. Blood 2011, 118, 2118. [Google Scholar] [CrossRef]
| Group 1 (20 mg Oxycodone) n = 10 | Group 2 (10 mg Oxycodone) n = 10 | p-Value | |
|---|---|---|---|
| ASA | 2.1 (SD = 0.7) | 2.2 (SD = 0.6) | 0.7486 |
| Comorbidities: | |||
| Hypertension | 3 | 5 | 0.6499 |
| Alcohol abuse | 2 | 3 | >0.9999 |
| Age (years) | 45.6 (SD = 15.7) | 541.2 (SD = 17.1) | 0.9556 |
| Sex (F/M) | 4/6 | 3/7 | 0.9999 |
| Height (cm) | 171.8 (SD = 7.5) | 173.0 (SD = 9.7) | 0.5392 |
| Weight (kg) | 89.3 (SD = 8.4) | 80.9 (SD = 15.2) | 0.2542 |
| Wound surface (%) | 13.7 (SD = 4.0) | 12.7 (SD = 4.5) | 0.5136 |
| Wound localisation: | |||
| Chest | 3 | 4 | |
| Abdomen | 3 | 2 | |
| Chest and abdomen | 4 | 4 | 0.8425 |
| The volume of octanidol (mL) | 346.0 (SD = 79.9) | 395.0 (SD = 103.9) | 0.1787 |
| FN received during surgery (mcg) | 244 (SD = 39.5) | 301.0 (SD = 146.5) | 0.3606 |
| Surgery duration (min) | 97.00 (SD = 38.2) | 94.5 (SD = 42.5) | 0.9272 |
| Patients | Postoperative | Dressing Oxycodone Concentration mg/mL | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 h | 2 h | 3 h | 6 h | |||||||||||
| SOC | SNC | NRS | SOC | SNC | NRS | SOC | SNC | NRS | SOC | SNC | NRS | After Surgery | ||
| Group 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.06 |
| 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.06 | |
| 3 | 1.78 | 0 | 0 | 2.15 | 0 | 0 | 1.56 | 0 | 0 | 1.24 | 0 | 0 | 0.06 | |
| 4 | 1.72 | 0 | 0 | 3.15 | 0 | 0 | 1.12 | 0 | 0 | 0 | 0 | 0 | 0.04 | |
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.06 | |
| 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.06 | |
| 7 | 1.82 | 0 | 0 | 2.43 | 0 | 0 | 1.77 | 0 | 0 | 1.64 | 0 | 2 | 0.05 | |
| 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0.04 | |
| 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.06 | |
| 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.04 | |
| Group 2 | 1 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0.03 |
| 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0.03 | |
| 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.03 | |
| 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.05 | |
| 5 | 0 | 0 | 0 | 1.28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.025 | |
| 6 | 1.25 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.02 | |
| 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1.16 | 0 | 0 | 0.025 | |
| 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.025 | |
| 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.03 | |
| 10 | 1.18 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 8 | 1.09 | 0 | 0 | 0.025 | |
| Group 1 (20 mg Oxycodone) n = 10 | Group 2 (10 mg Oxycodone) n = 10 | p-Value | |
|---|---|---|---|
| NRS postoperative | |||
| 1 h | 0 (0–0) | 0 (0–0) | 1.0 |
| 2 h | 0 (0–0) | 0.9 (0–6) | 0.9999 |
| 3 h | 0 (0–0) | 0.8 (0–8) | 0.9999 |
| 6 h | 0 (0–0) | 0.5 (0–5) | 0.9999 |
| Serum oxycodone concentration levels (ng/mL) | |||
| 1 h | 0.5320 (SD = 0.8569) | 0.2430 (SD = 0.5126) | 0.3731 |
| 2 h | 0.7730 (SD = 1.268) | 0.1280 (SD = 0.4048) | 0.2105 |
| 3 h | 0.4450 (SD = 0.7334) | 0.0000 (SD = 0.0000) | 0.2105 |
| 6 h | 0.2880 (SD = 0.6144) | 0.2250 (SD = 0.4746) | 0.7214 |
| Serum noroxycodone concentration levels (ng/mL) | |||
| 1 h | 0 (0–0) | 0 (0–0) | 1.0 |
| 2 h | 0 (0–0) | 0 (0–0) | 1.0 |
| 3 h | 0 (0–0) | 0 (0–0) | 1.0 |
| 6 h | 0 (0–0) | 0 (0–0) | 1.0 |
| Dressing oxycodone concentration (mg/mL) | |||
| After surgery | 0.0530 (SD = 0.0095) | 0.0290 (SD = 0.0081) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowalski, G.; Leppert, W.; Domagalska, M.; Grochowicka, M.; Teżyk, A.; Słowiński, K.; Bienert, A.; Szkutnik-Fiedler, D.; Wieczorowska-Tobis, K. Analgesic Efficacy of Oxycodone in Postoperative Dressings after Surgical Treatment of Burn Wounds: A Randomised Controlled Trial. J. Clin. Med. 2024, 13, 784. https://doi.org/10.3390/jcm13030784
Kowalski G, Leppert W, Domagalska M, Grochowicka M, Teżyk A, Słowiński K, Bienert A, Szkutnik-Fiedler D, Wieczorowska-Tobis K. Analgesic Efficacy of Oxycodone in Postoperative Dressings after Surgical Treatment of Burn Wounds: A Randomised Controlled Trial. Journal of Clinical Medicine. 2024; 13(3):784. https://doi.org/10.3390/jcm13030784
Chicago/Turabian StyleKowalski, Grzegorz, Wojciech Leppert, Małgorzata Domagalska, Monika Grochowicka, Artur Teżyk, Krzysztof Słowiński, Agnieszka Bienert, Danuta Szkutnik-Fiedler, and Katarzyna Wieczorowska-Tobis. 2024. "Analgesic Efficacy of Oxycodone in Postoperative Dressings after Surgical Treatment of Burn Wounds: A Randomised Controlled Trial" Journal of Clinical Medicine 13, no. 3: 784. https://doi.org/10.3390/jcm13030784
APA StyleKowalski, G., Leppert, W., Domagalska, M., Grochowicka, M., Teżyk, A., Słowiński, K., Bienert, A., Szkutnik-Fiedler, D., & Wieczorowska-Tobis, K. (2024). Analgesic Efficacy of Oxycodone in Postoperative Dressings after Surgical Treatment of Burn Wounds: A Randomised Controlled Trial. Journal of Clinical Medicine, 13(3), 784. https://doi.org/10.3390/jcm13030784







