Comparison of the Analgesic Efficacy between Levobupivacaine 0.25% and Ropivacaine 0.375% for PENG (Pericapsular Nerve Group) Block in the Context of Hip Fracture Surgery of Elderly Patients: A Single-Center, Randomized, and Controlled Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
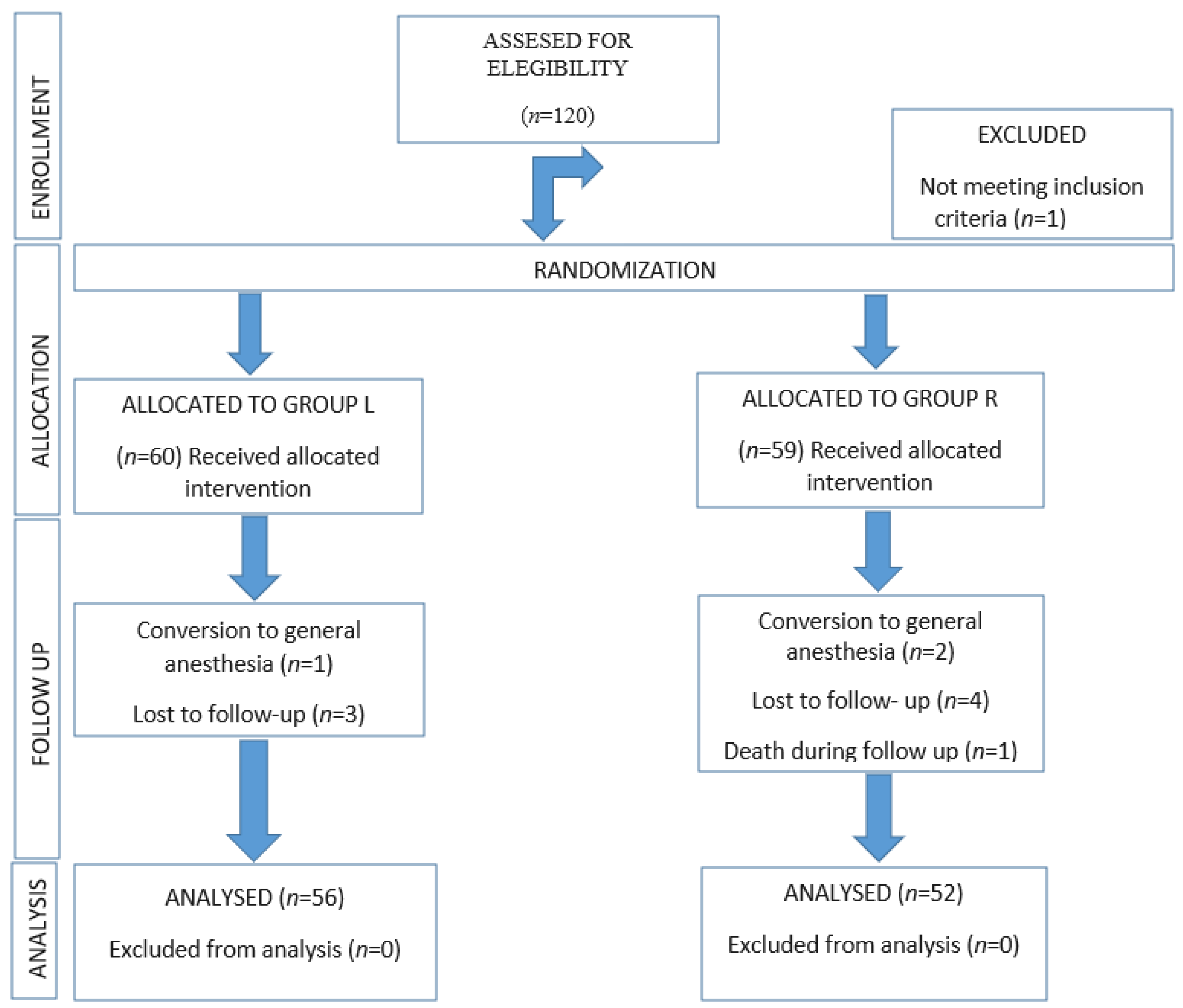
2.2. Patient Screening and Enrolment
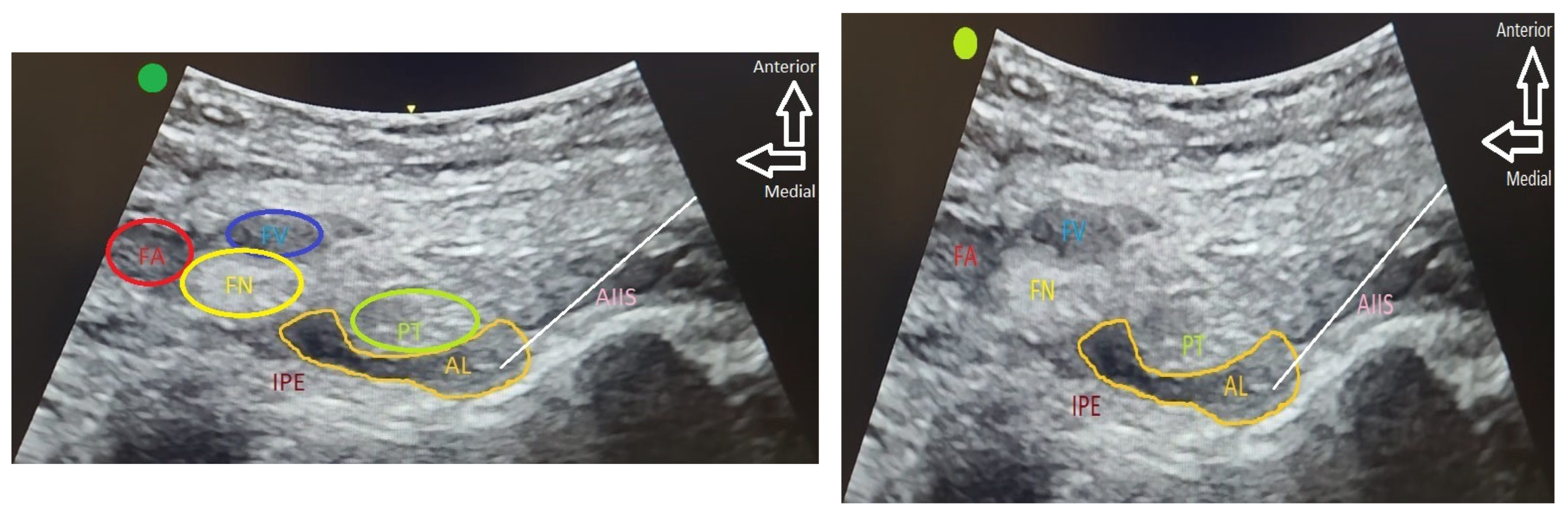
2.3. Intervention
2.4. Data Collection and Outcomes
2.5. Statistical Analysis
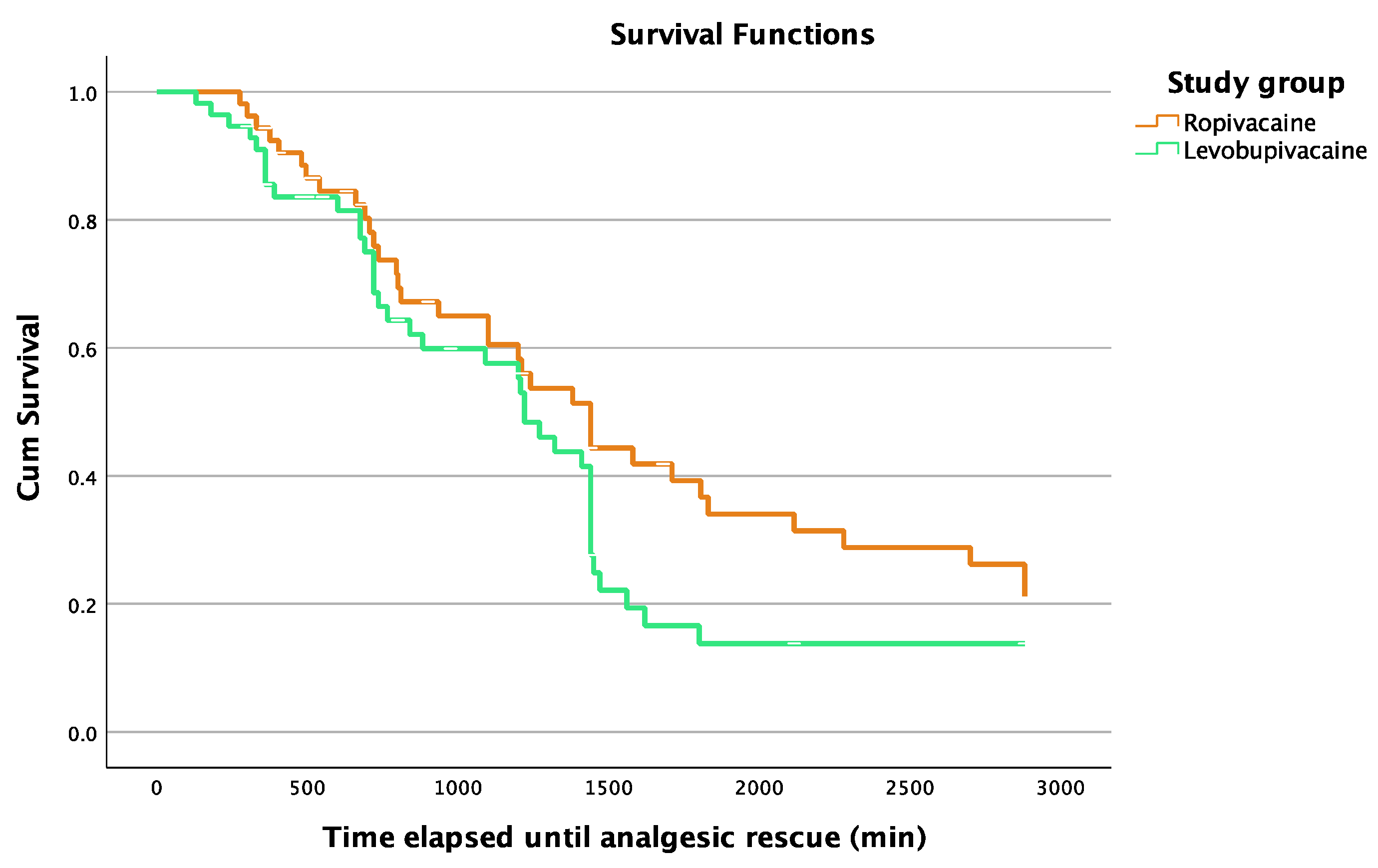
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ojeda-Thies, C.; Sáez-López, P.; Currie, C.T.; Tarazona-Santalbina, F.J.; Alarcón, T.; Muñoz-Pascual, A.; Pareja, T.; Gómez-Campelo, P.; Montero-Fernández, N.; Mora-Fernández, J.; et al. Spanish National Hip Fracture Registry (RNFC): Analysis of its first annual report and international comparison with other established registries. Osteoporos. Int. 2019, 30, 1243–1254. [Google Scholar] [CrossRef] [PubMed]
- Chesser, T.J.S.; Inman, D.; Johansen, A.; Belluati, A.; Pari, C.; Contini, A.; Voeten, S.C.; Hegeman, J.H.; Ponsen, K.J.; Montero-Fernández, N.; et al. Hip fractur systems-European experience. OTA Int. 2020, 3, e050. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Kim, S.H.; Park, K.K.; Kim, S.J.; Bae, J.C.; Choi, Y.S. Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial. J. Clin. Med. 2020, 9, 1605. [Google Scholar] [CrossRef] [PubMed]
- Neuman, M.D.; Feng, R.; Carson, J.L.; Gaskins, L.J.; Dillane, D.; Sessler, D.I.; Sieber, F.; Magaziner, J.; Marcantonio, E.R.; Mehta, S.; et al. Spinal 371 anesthesia or general anesthesia for hip surgery in older adults. N. Engl. J. Med. 2021, 385, 2025–2035. [Google Scholar] [CrossRef]
- Tzimas, P.; Samara, E.; Petrou, A.; Korompilias, A.; Chalkias, A.; Papadopoulos, G. The influence of anesthetic techniques on postoperative cognitive function in elderly patients undergoing hip fracture surgery: General vs spinal anesthesia. Injury 2018, 49, 2221–2226. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.X.; Yang, L.; Ding, L.; Li, S.Y.; Na Qi, Y.; Li, Q. Perioperative outcomes in geriatric patients undergoing hip fracture surgery with different anesthesia techniques: A systematic review and meta-analysis. Medicine 2019, 98, e18220. [Google Scholar] [CrossRef] [PubMed]
- Rodkey, D.L.; Pezzi, A.; Hymes, R. Effects of spinal anesthesia in geriatric hip fracture: A propensity-matched study. J. Orthop. Trauma 2022, 36, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Nishi, T.; Maeda, T.; Imatoh, T.; Babazono, A. Comparison of regional with general anesthesia on mortality and perioperative length of stay in older patients after hip fracture surgery. Int. J. Qual. Health Care 2019, 31, 669–675. [Google Scholar] [CrossRef]
- Maxwell, B.G.; Spitz, W.; Porter, J. Association of Increasing Use of Spinal Anesthesia in Hip Fracture Repair with Treating an Aging Patient Population. JAMA Surg. 2020, 155, 167–168. [Google Scholar] [CrossRef]
- Morrison, S.R.; Magaziner, J.; McLaughlin, M.A.; Orosz, G.; Silberzweig, S.B.; Koval, K.J.; Siu, A.L. The impact of post-operative pain on outcomes following hip fracture. Pain 2003, 103, 303–311. [Google Scholar] [CrossRef]
- Aubrun, F.; Marmion, F. The elderly patient and postoperative pain treatment. Best. Pract. Res. Clin. Anaesthesiol. 2007, 21, 109–127. [Google Scholar] [CrossRef]
- Chau, D.L.; Walker, V.; Pai, L.; Cho, L.M. Opiates and elderly: Use and side effects. Clin Interv. Aging 2008, 3, 273–278. [Google Scholar] [CrossRef]
- Poeran, J.; Cozowicz, C.; Zubizarreta, N.; Weinstein, S.M.; Deiner, S.G.; Leipzig, R.M.; Friedman, J.I.; Liu, J.; Mazumdar, M.; Memtsoudis, S.G. Modifiable factors associated with postoperative delirium after hip fracture repair: An age-stratified retrospective cohort study. Eur. J. Anaesthesiol. 2020, 37, 649–658. [Google Scholar] [CrossRef]
- Guay, J.; Parker, M.J.; Griffiths, R.; Kopp, S.L. Peripheral nerve blocks for hip fractures: A cochrane review. Anesth. Analg. 2018, 126, 1695–1704. [Google Scholar] [CrossRef]
- Chen, K.; Klar, G.; Haley, C. Evidence for Regional Anesthesia Blocks for Patients with Hip Fractures. Available online: https://resources.wfsahq.org/atotw/evidence-for-regional-anesthesia-blocks-for-patients-with-hip-fractures-atotw-477/ (accessed on 15 October 2023).
- Dangle, J.; Kukreja, P.; Kalagara, H. Review of current practices of peripheral nerve blocks for hip fracture and surgery. Curr. Anesthesiol. Rep. 2020, 10, 259–266. [Google Scholar] [CrossRef]
- Griffiths, R.; Babu, S.; Dixon, P.; Freeman, N.; Hurford, D.; Kelleher, E.; Moppett, I.; Ray, D.; Sahota, O.; Shields, M.; et al. Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists. Anaesthesia 2021, 76, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Short, A.J.; Barnett, J.J.G.; Gofeld, M.; Baig, E.; Lam, K.; Agur, A.M.R.; Peng, P.W.H. Anatomic study of innervation of the anterior hip capsule: Implication for image-guided intervention. Reg. Anesth. Pain. Med. 2018, 43, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Giron-Arango, L.; Peng, P.W.H.; Chin, K.J.; Brull, R.; Perlas, A. Pericapsular Nerve Group (PENG) Block for Hip Fracture. Reg. Anesth. Pain. Med. 2018, 43, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Domagalska, M.; Ciftci, B.; Reysner, T.; Kolasiński, J.; Wieczorowska-Tobis, K.; Kowalski, G. Pain Management and Functional Recovery after Pericapsular Nerve Group (PENG) block for total hip arthroplasty: A prospective, randomized, double-blinded clinical trial. J. Clin. Med. 2023, 12, 4931. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.Y.; Morrison, C.; Brown, B.; Saies, A.A.; Pawar, R.; Vermeulen, M.; Anderson, S.R.; Lee, T.S.; Doornberg, J.; Kroon, H.M.; et al. Pericapsular Nerve Group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: A single-center double-blinded randomized comparative trial. Reg. Anesth. Pain. Med. 2021, 46, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.; Tang, Y.; Tong, F.; Guo, H.; Zhang, X.L.; Zhou, L.; Ni, H.; Wang, B.; Liu, Y.; Liu, J. The analgesic efficacy of pericapsular nerve group block in patients with intertrochanteric femur fracture: A randomized controlled trial. PLoS ONE 2022, 17, e0275793. [Google Scholar] [CrossRef]
- Li, A.; Wei, Z.; Liu, Y.; Shi, J.; Ding, H.; Tang, H.; Zheng, P.; Gao, Y.; Feng, S. Ropivacaine versus levobupivacaine in peripheral nerve block: A PRISMA-compliant meta-analysis of randomized controlled trials. Medicine 2017, 96, e6551. [Google Scholar] [CrossRef] [PubMed]
- López, M.S.; Hernández, N.S.; Mola, S.J.; García, N.A.; García, J.V. Valoración del dolor en el anciano. Rev. Soc. Esp. Dolor. 2015, 22, 271–274. [Google Scholar] [CrossRef]
- Herrero, M.T.V.; Bueno, S.D.; Moyá, F.B.; De La Torre, M.V.R.I.; García, L.C. Valoración del dolor. Revisión comparativa de escalas y cuestionarios. Rev. Soc. Esp. Dolor. 2018, 25, 228–236. [Google Scholar] [CrossRef]
- Rodriguez-Mansilla, J.; Jimenez-Palomares, M.; Gonzalez-Lopez-Arza, M.V. Scales to evaluate pain in elderly patients suffering from dementia. Help-tools for the physiotherapist, doctor, nurse and occupational therapist. Rev. Esp. Geriatr. Gerontol. 2014, 49, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Mosele, M.; Inelmen, E.; Toffanello, E.; Girardi, A.; Coin, A.; Sergi, G.; Manzato, E. Psychometric properties of the pain assessment in advanced dementia scale compared to self assessment of pain in elderly patients. Dement. Geriatr. Cogn. Disord. 2012, 34, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Cantón-Habas, V.; Rich-Ruiz, M.; Moreno-Casbas, M.T.; Ramírez-Expósito, M.J.; Martínez-Martos, J.M.; Carrera-González, M.D.P. Correlation between biomarkers of pain in saliva and PAINAD scale in elderly people with cognitive impairment and inability to communicate: Descriptive study protocol. BMJ Open 2019, 9, e032927. [Google Scholar] [CrossRef]
- Casati, A.; Putzu, M. Bupivacaine, levobupivacaine and ropivacaine: Are they clinically different? Best Pract. Res. Clin. Anaesthesiol. 2005, 19, 247–268. [Google Scholar] [CrossRef]
- Bräu, M.E.; Branitzki, P.; Olschewski, A.; Vogel, W.; Hempelmann, G. Block of neuronal tetrodotoxin-resistant Na+ currents by stereoisomers of piperidine local anesthetics. Anesth. Analg. 2000, 91, 1499–1505. [Google Scholar] [CrossRef]
- Fournier, R.; Faust, A.; Chassot, O.; Gamulin, Z. Levobupivacaine 0.5% provides longer analgesia after sciatic nerve block using the Labat approach than the same dose of ropivacaine in foot and ankle surgery. Anesth. Analg. 2010, 110, 1486–1489. [Google Scholar] [CrossRef]
- Dyhre, H.; Lang, M.; Wallin, R.; Renck, H. The duration of action of bupivacaine, levobupivacaine, ropivacaine and pethidine in peripheral nerve block in the rat. Acta Anaesthesiol. Scand. 1997, 41, 1346–1352. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Lee, S.; Chin, K.J.; Kim, J.-S.; Kim, H.; Ro, Y.-J.; Koh, W.U. Comparison of the onset time between 0.375% ropivacaine and 0.25% levobupivacaine for ultrasound-guided infraclavicular brachial plexus block: A randomized-controlled trial. Sci. Rep. 2021, 11, 4703. [Google Scholar] [CrossRef] [PubMed]
- Borghi, B.; Facchini, F.; Agnoletti, V.; Adduci, A.; Lambertini, A.; Marini, E.; Gallerani, P.; Sassoli, V.; Luppi, M.; Casati, A. Pain relief and motor function during continuous interscalene analgesia after open shoulder surgery: A prospective, randomized, double-blind comparison between levobupivacaine 0.25%, and ropivacaine 0.25% or 0.4%. Eur. J. Anaesthesiol. 2006, 23, 1005–1009. [Google Scholar] [CrossRef] [PubMed]
| Group L (n = 56) | Group R (n = 52) | |
|---|---|---|
| Age, years | 88.0 (13.0) | 87.0 (7) |
| Gender, n (%) | ||
| Male | 15 (26.8) | 9 (17.3) |
| Female | 41 (73.2) | 43 (82.7) |
| Height, cm | 1.56 (0.13) | 1.57 (0.11) |
| Weight, kg | 65.5 (16.0) | 61.5 (15.75) |
| Body Mass Index, kg/m2 | 25.14 (4.86) | 24.36 (5.65) |
| Duration of surgery, min | 49.0 (25.0) | 50.0 (19.0) |
| Type of fracture, n (%) | ||
| Sub-capital | 24 (42.9) | 14 (26.9) |
| Pertrochanteric | 31 (55.4) | 36 (69.2) |
| Sub-pertrochanteric | 1 (1.8) | 0 (0) |
| Others | 2 (3.8) | |
| Type of surgery, n (%) | ||
| Partial Hip Arthroplasty | 24 (42.9) | 14 (26.9) |
| Endomedullary Nailing | 32 (57.1) | 37 (71.2) |
| Others | 0 (0) | 1 (1.9) |
| Group L | Group R | p | |
|---|---|---|---|
| Arrival to OT | |||
| VAS R | 0.0 (3) (n = 38) | 0.00 (4) (n = 40) | 0.674 |
| VAS A | 8.0 (5) (n = 37) | 8.00 (4) (n = 39) | 0.487 |
| PAINAD R | 0.0 (0) (n = 56) | 0.00 (0) (n = 52) | 0.273 |
| PAINAD A | 6.0 (4) (n = 56) | 5.00 (5) (n = 52) | 0.239 |
| AlgoPlus R | 0.0 (0) (n = 56) | 0.00 (0) (n = 52) | 0.431 |
| AlgoPlus A | 4.0 (2) (n = 56) | 3.00 (2) (n = 52) | 0.872 |
| 10 min after block | |||
| VAS R | 0.00 (0) (n = 38) | 0.00 (0) (n = 40) | 0.479 |
| VAS A | 3.00 (4) (n = 38) | 2.00 (4) (n = 39) | 0.346 |
| PAINAD R | 0.00 (0) (n = 56) | 0.00 (0) (n = 52) | 0.919 |
| PAINAD A | 2.00 (2) (n = 56) | 1.00 (3) (n = 52) | 0.381 |
| AlgoPlus R | 0.00 (0) (n = 56) | 0.00 (0) (n = 52) | 0.757 |
| AlgoPlus A | 1.00 (1) (n = 56) | 1.00 (2) (n = 52) | 0.426 |
| Sitting for the SAB | |||
| VAS | 0.00 (3) (n = 39) | 0.00 (1) (n = 40) | 0.581 |
| PAINAD | 0.00 (2) (n = 56) | 0.00 (1) (n = 52) | 0.443 |
| AlgoPlus | 0.00 (1) (n = 54) | 0.00 (1) (n = 51) | 0.294 |
| At discharge of PCU | |||
| VAS R | 0.00 (0) (n = 39) | 0.00 (0) (n = 41) | 0.492 |
| VAS A | 0.00 (3) (n = 37) | 0.00 (2) (n = 41) | 0.481 |
| PAINAD R | 0.00 (0) (n = 55) | 0.00 (0) (n = 52) | 0.529 |
| PAINAD A | 0.00 (2) (n = 55) | 0.00 (1) (n = 52) | 0.236 |
| AlgoPlus R | 0.00 (0) (n = 53) | 0.00 (0) (n = 52) | 0.956 |
| AlgoPlus A | 0.00 (1) (n = 55) | 0.00 (1) (n = 52) | 0.248 |
| 6 h after block | |||
| VAS R | 0.00 (0) (n = 40) | 0.00 (0) (n = 40) | 0.913 |
| VAS A | 1.00 (4) (n = 38) | 0.00 (3) (n = 40) | 0.479 |
| PAINAD R | 0.00 (0) (n = 54) | 0.00 (0) (n = 51) | 0.364 |
| PAINAD A | 1.00 (3) (n = 54) | 0.00 (1) (n = 51) | 0.264 |
| AlgoPlus R | 0.00 (0) (n = 52) | 0.00 (0) (n = 51) | 0.093 |
| AlgoPlus A | 1.00 (2) (n = 54) | 0.00 (1) (n = 51) | 0.458 |
| 12 h after block | |||
| VAS R | 0.00 (0) (n = 29) | 0.00 (0) (n = 34) | 0.508 |
| VAS A | 2.50 (4) (n = 26) | 2.00 (6) (n = 33) | 1.000 |
| PAINAD R | 0.00 (0) (n = 43) | 0.00 (0) (n = 45) | 0.314 |
| PAINAD A | 2.00 (3) (n = 43) | 1.00 (3) (n = 45) | 0.539 |
| AlgoPlus R | 0.00 (0) (n = 41) | 0.00 (0) (n = 44) | 0.188 |
| AlgoPlus A | 1.00 (2) (n = 43) | 1.00 (3) (n = 45) | 0.836 |
| 24 h after block | |||
| VAS R | 0.00 (1) (n = 18) | 0.00 (1) (n = 21) | 0.878 |
| VAS A | 4.50 (4) (n = 15) | 3.50 (5) (n = 20) | 0.382 |
| PAINAD R | 0.00 (0) (n = 25) | 0.00 (0) (n = 33) | 0.397 |
| PAINAD A | 4.00 (2) (n = 25) | 2.00 (5) (n = 33) | 0.374 |
| AlgoPlus R | 0.00 (0) (n = 25) | 0.00 (0) (n = 33) | 0.401 |
| AlgoPlus A | 2.50 (2) (n = 25) | 1.50 (3) (n = 33) | 0.174 |
| 48 h after block or at time of analgesic rescue | |||
| VAS R | 0.00 (2) (n = 38) | 0.00 (2) (n = 40) | 0.526 |
| VAS A | 5.00 (4) (n = 36) | 5.00 (4) (n = 39) | 0.864 |
| PAINAD R | 0.00 (0) (n = 56) | 0.00 (0) (n = 52) | 0.950 |
| PAINAD A | 3.00 (2) (n = 56) | 3.00 (4) (n = 52) | 0.551 |
| AlgoPlus R | 0.00 (0) (n = 56) | 0.00 (0) (n = 52) | 0.865 |
| Algoplus A | 2.00 (2) (n = 56) | 2.00 (2) (n = 52) | 0.724 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salgado-García, D.; Díaz-Álvarez, A.; González-Rodríguez, J.L.; López-Iglesias, M.R.; Sánchez-López, E.; Sánchez-Ledesma, M.J.; Martínez-Trufero, M.I. Comparison of the Analgesic Efficacy between Levobupivacaine 0.25% and Ropivacaine 0.375% for PENG (Pericapsular Nerve Group) Block in the Context of Hip Fracture Surgery of Elderly Patients: A Single-Center, Randomized, and Controlled Clinical Trial. J. Clin. Med. 2024, 13, 770. https://doi.org/10.3390/jcm13030770
Salgado-García D, Díaz-Álvarez A, González-Rodríguez JL, López-Iglesias MR, Sánchez-López E, Sánchez-Ledesma MJ, Martínez-Trufero MI. Comparison of the Analgesic Efficacy between Levobupivacaine 0.25% and Ropivacaine 0.375% for PENG (Pericapsular Nerve Group) Block in the Context of Hip Fracture Surgery of Elderly Patients: A Single-Center, Randomized, and Controlled Clinical Trial. Journal of Clinical Medicine. 2024; 13(3):770. https://doi.org/10.3390/jcm13030770
Chicago/Turabian StyleSalgado-García, Daniel, Agustín Díaz-Álvarez, José Luis González-Rodríguez, María Rocío López-Iglesias, Eduardo Sánchez-López, Manuel Jesús Sánchez-Ledesma, and María Isabel Martínez-Trufero. 2024. "Comparison of the Analgesic Efficacy between Levobupivacaine 0.25% and Ropivacaine 0.375% for PENG (Pericapsular Nerve Group) Block in the Context of Hip Fracture Surgery of Elderly Patients: A Single-Center, Randomized, and Controlled Clinical Trial" Journal of Clinical Medicine 13, no. 3: 770. https://doi.org/10.3390/jcm13030770
APA StyleSalgado-García, D., Díaz-Álvarez, A., González-Rodríguez, J. L., López-Iglesias, M. R., Sánchez-López, E., Sánchez-Ledesma, M. J., & Martínez-Trufero, M. I. (2024). Comparison of the Analgesic Efficacy between Levobupivacaine 0.25% and Ropivacaine 0.375% for PENG (Pericapsular Nerve Group) Block in the Context of Hip Fracture Surgery of Elderly Patients: A Single-Center, Randomized, and Controlled Clinical Trial. Journal of Clinical Medicine, 13(3), 770. https://doi.org/10.3390/jcm13030770


.png)



