Temporomandibular Joint Minimally Invasive Procedures in the Pediatric Population: A Prospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Minimally Invasive TMJ Surgery
2.2.1. Double-Puncture TMJ Arthrocentesis
2.2.2. TMJ Arthroscopy
2.3. Statistical Analysis
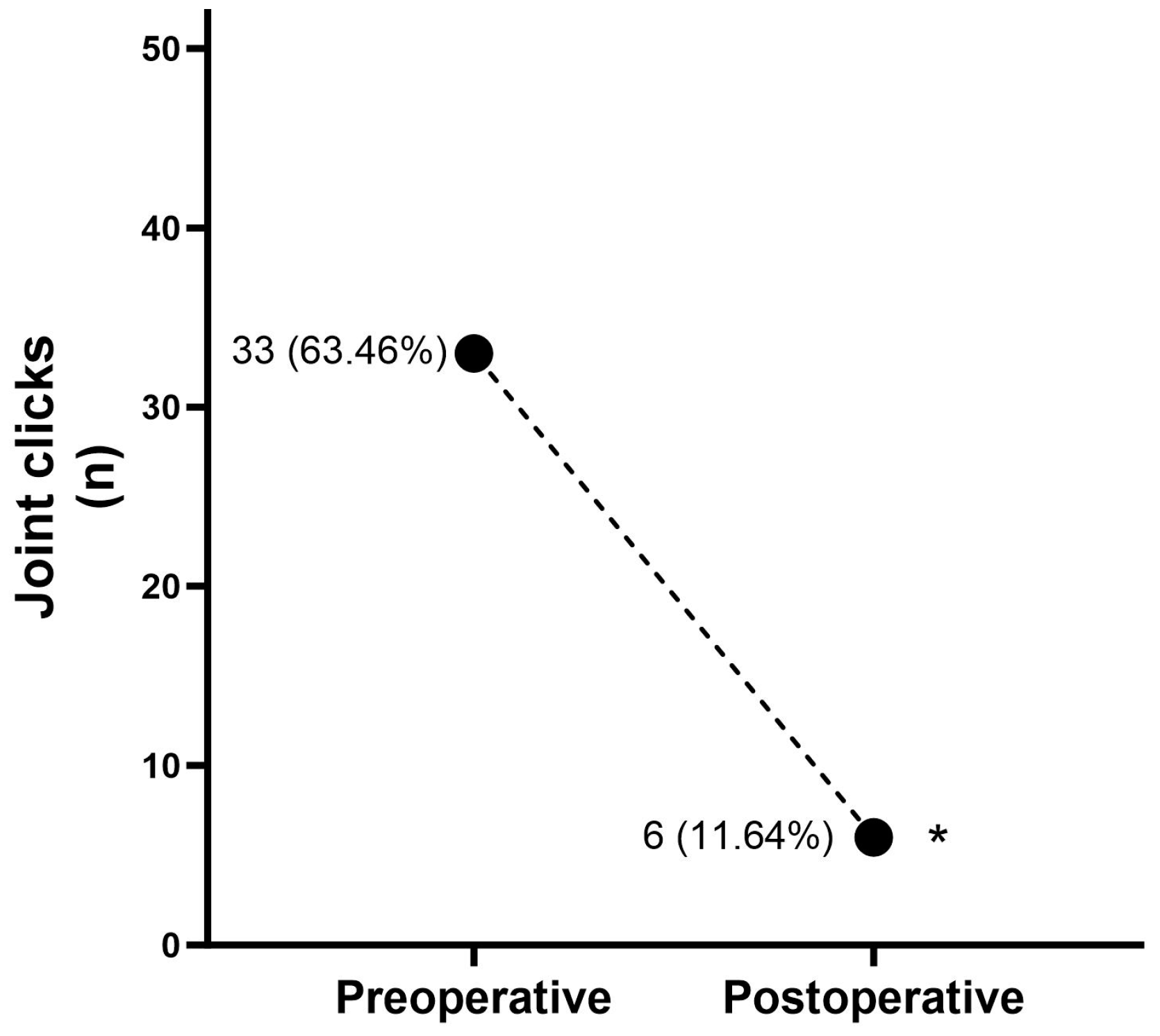
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, D.T.S.; Wong, N.S.M.; Li, S.K.Y.; McGrath, C.P.; Leung, Y.Y. Timing of arthrocentesis in the management of temporomandibular disorders: An integrative review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 1078–1088. [Google Scholar] [CrossRef] [PubMed]
- Ângelo, D.F.; Araújo, R.A.D.; Sanz, D. Surgical complications related to temporomandibular joint arthroscopy: A prospective analysis of 39 single-portal versus 43 double-portal procedures. Int. J. Oral Maxillofac. Surg. 2021, 50, 1089–1094. [Google Scholar] [CrossRef]
- Ângelo, D.F.; Sanz, D.; Cardoso, H.J. Effectiveness of double-puncture temporomandibular joint arthrocentesis with viscosupplementation in different categories of severity-a prospective study. J. Cranio-Maxillo-Facial Surg. 2023, 51, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Tarro, A.W. Minimally Invasive TMJ Surgery: From Arthrocentesis to Advanced Laser Arthroscopy. J. Oral Maxillofac. Surg. 2005, 63, 115–116. [Google Scholar] [CrossRef]
- Vaira, L.A.; Raho, M.T.; Soma, D.; Salzano, G.; Dell’aversana Orabona, G.; Piombino, P.; De Riu, G. Complications and post-operative sequelae of temporomandibular joint arthrocentesis. Cranio J. Craniomandib. Pract. 2018, 36, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Soni, A. Arthrocentesis of Temporomandibular Joint- Bridging the Gap Between Non-Surgical and Surgical Treatment. Ann. Maxillofac. Surg. 2019, 9, 158–167. [Google Scholar] [CrossRef]
- González, L.V.; López, J.P.; Díaz-Báez, D.; Martin-Granizo López, R. Intraoperative complications in temporomandibular joint arthroscopy: A retrospective observational analysis of 899 arthroscopies. J. Cranio-Maxillo-Facial Surg. 2022, 50, 651–656. [Google Scholar] [CrossRef]
- Nogueira, E.F.C.; Lemos, C.A.A.; Vasconcellos, R.J.H.; Moraes, S.L.D.; Vasconcelos, B.C.E.; Pellizzer, E.P. Does arthroscopy cause more complications than arthrocentesis in patients with internal temporomandibular joint disorders? Systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2021, 59, 1166–1173. [Google Scholar] [CrossRef]
- Wolf, J.; Weiss, A.; Dym, H. Technological Advances in Minimally Invasive TMJ Surgery. Dent. Clin. N. Am. 2011, 55, 635–640. [Google Scholar] [CrossRef]
- González-García, R. The Current Role and the Future of Minimally Invasive Temporomandibular Joint Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2015, 27, 69–84. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Wolford, L.M.; Ellis, E., III; Neff, A. The hierarchy of different treatments for arthrogenous temporomandibular disorders: A network meta-analysis of randomized clinical trials. J. Cranio-Maxillo-Facial Surg. 2020, 48, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.H.; Vos, L.M.; Tuin, A.J.; Huddleston Slater, J.J.R.; Gareb, B.; van Bakelen, N.B.; Spijkervet, F.K.L. Arthrocentesis versus non-surgical intervention as initial treatment for temporomandibular joint arthralgia: A randomized controlled trial with long-term follow-up. Int. J. Oral Maxillofac. Surg. 2023, 52, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Moses, J.J.; Poker, I.D. TMJ arthroscopic surgery: An analysis of 237 patients. J. Oral Maxillofac. Surg. 1989, 47, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Rigon, M.; Pereira, L.M.; Bortoluzzi, M.C.; Loguercio, A.D.; Ramos, A.L.; Cardoso, J.R. Arthroscopy for temporomandibular disorders. Cochrane Database Syst. Rev. 2011, 5, Cd006385. [Google Scholar] [CrossRef]
- Fridrich, K.L.; Wise, J.M.; Zeitler, D.L. Prospective comparison of arthroscopy and arthrocentesis for temporomandibular joint disorders. J. Oral Maxillofac. Surg. 1996, 54, 816–820; discussion 821. [Google Scholar] [CrossRef]
- Ângelo, D.F.; Sanz, D.; Cardoso, H.J. Bilateral arthroscopy of the temporomandibular joint: Clinical outcomes and the role of a second intervention-a prospective study. Clin. Oral Investig. 2023, 27, 6167–6176. [Google Scholar] [CrossRef] [PubMed]
- Scrivani, S.J.; Khawaja, S.N.; Bavia, P.F. Nonsurgical Management of Pediatric Temporomandibular Joint Dysfunction. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Mélou, C.; Sixou, J.L.; Sinquin, C.; Chauvel-Lebret, D. Temporomandibular disorders in children and adolescents: A review. Arch. De Pédiatrie 2023, 30, 335–342. [Google Scholar] [CrossRef]
- Derwich, M.; Gottesman, L.; Urbanska, K.; Pawlowska, E. Craniovertebral and Craniomandibular Changes in Patients with Temporomandibular Joint Disorders after Physiotherapy Combined with Occlusal Splint Therapy: A Prospective Case Control Study. Medicina 2022, 58, 684. [Google Scholar] [CrossRef]
- Ouanounou, A.; Goldberg, M.; Haas, D.A. Pharmacotherapy in Temporomandibular Disorders: A Review. J. Can. Dent. Assoc. 2017, 83, h7. [Google Scholar]
- Dimitroulis, G. A new surgical classification for temporomandibular joint disorders. Int. J. Oral Maxillofac. Surg. 2013, 42, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.L.; von Baeyer, C.L.; Spafford, P.A.; van Korlaar, I.; Goodenough, B. The Faces Pain Scale-Revised: Toward a common metric in pediatric pain measurement. Pain 2001, 93, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Goiato, M.C.; Zuim, P.R.J.; Moreno, A.; Dos Santos, D.M.; da Silva, E.V.F.; de Caxias, F.P.; Turcio, K.H.L. Does pain in the masseter and anterior temporal muscles influence maximal bite force? Arch. Oral Biol. 2017, 83, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, L.; Westesson, P.L. Discectomy as an effective treatment for painful temporomandibular joint internal derangement: A 5-year clinical and radiographic follow-up. J. Oral Maxillofac. Surg. 2001, 59, 750–758. [Google Scholar] [CrossRef]
- Ângelo, D.F.; Sanz, D.; Maffia, F.; Cardoso, H.J. Outcomes of IncobotulinumtoxinA Injection on Myalgia and Arthralgia in Patients Undergoing Temporomandibular Joint Arthroscopy: A Randomized Controlled Trial. Toxins 2023, 15, 376. [Google Scholar] [CrossRef]
- Alpaslan, C.; Dolwick, M.F.; Heft, M.W. Five-year retrospective evaluation of temporomandibular joint arthrocentesis. Int. J. Oral Maxillofac. Surg. 2003, 32, 263–267. [Google Scholar] [CrossRef]
- Ahmed, N.; Sidebottom, A.; O’Connor, M.; Kerr, H.-L. Prospective outcome assessment of the therapeutic benefits of arthroscopy and arthrocentesis of the temporomandibular joint. Br. J. Oral Maxillofac. Surg. 2012, 50, 745–748. [Google Scholar] [CrossRef]
- Nitzan, D.W.; Dolwick, M.F.; Martinez, G.A. Temporomandibular joint arthrocentesis: A simplified treatment for severe, limited mouth opening. J. Oral Maxillofac. Surg. 1991, 49, 1163–1167; discussion 1168–1170. [Google Scholar] [CrossRef]
- Sembronio, S.; Albiero, A.M.; Toro, C.; Robiony, M.; Politi, M. Is there a role for arthrocentesis in recapturing the displaced disc in patients with closed lock of the temporomandibular joint? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 105, 274–280; discussion 281. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K. Current role of arthrocentesis, arthroscopy and open surgery for temporomandibular joint internal derangement with inflammatory/degenerative disease; -pitfalls and pearls. J. Oral Maxillofac. Surg. Med. Pathol. 2022, 34, 1–11. [Google Scholar] [CrossRef]
- Indresano, A.T. Surgical arthroscopy as the preferred treatment for internal derangements of the temporomandibular joint. J. Oral Maxillofac. Surg. 2001, 59, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.B.P.; Krishnaswamy, G. A Retrospective Study of Temporomandibular Joint Internal Derangement Treated with Arthrocentesis and Arthroscopy. Proc. Singap. Healthc. 2012, 21, 73–78. [Google Scholar] [CrossRef]
- McCain, J.P.; Sanders, B.; Koslin, M.G.; Quinn, J.D.; Peters, P.B.; Indresano, A.T. Temporomandibular joint arthroscopy: A 6-year multicenter retrospective study of 4,831 joints. J. Oral Maxillofac. Surg. 1992, 50, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Goudot, P.; Jaquinet, A.R.; Hugonnet, S.; Haefliger, W.; Richter, M. Improvement of pain and function after arthroscopy and arthrocentesis of the temporomandibular joint: A comparative study. J. Cranio-Maxillo-Facial Surg. 2000, 28, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Bender, M.E.; Lipin, R.B.; Goudy, S.L. Development of the Pediatric Temporomandibular Joint. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 1–9. [Google Scholar] [CrossRef]
- Zhuo, Z.; Cai, X.-Y.; Xie, Q. Is Anterior Disc Displacement without Reduction Associated with Temporomandibular Joint Condylar Height in Juvenile Patients under 20y. J. Oral Maxillofac. Surg. 2014, 73, 843–849. [Google Scholar] [CrossRef]
- Xie, Q.; Yang, C.; He, D.; Cai, X.; Ma, Z.; Shen, Y.; Abdelrehem, A. Will unilateral temporomandibular joint anterior disc displacement in teenagers lead to asymmetry of condyle and mandible? A longitudinal study. J. Cranio-Maxillo-Facial Surg. 2016, 44, 590–596. [Google Scholar] [CrossRef]
- Choi, D.D.; Vandenberg, K.; Smith, D.; Davis, C.; McCain, J.P. Is Temporomandibular Joint Arthroscopy Effective in Managing Pediatric Temporomandibular Joint Disorders in the Short- and Long-Term? J. Oral Maxillofac. Surg. 2020, 78, 44–51. [Google Scholar] [CrossRef]
- AbdulRazzak, N.J.; Sadiq, J.A.; Jiboon, A.T. Arthrocentesis versus glucocorticosteroid injection for internal derangement of temporomandibular joint. Oral Maxillofac. Surg. 2021, 25, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Karian, V.; Morton, H.; Schefter, Z.J.; Smith, A.; Rogan, H.; Morse, B.; LeBel, A. OnabotulinumtoxinA for Pediatric Migraine. Pain Manag. Nurs. 2023, 24, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Mulpuri, K.; Schaeffer, E.K.; Sanders, J.; Zaltz, I.; Kocher, M.S. Evidence-based Recommendations for Pediatric Orthopaedic Practice. J. Pediatr. Orthop. 2018, 38, e551–e555. [Google Scholar] [CrossRef] [PubMed]
- Raphael, K.G.; Tadinada, A.; Bradshaw, J.M.; Janal, M.N.; Sirois, D.A.; Chan, K.C.; Lurie, A.G. apenic consequences of botulinum toxin injections in the masticatory muscles: A pilot study. J. Oral Rehabil. 2014, 41, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Bevilaqua Grossi, D.; Lipton, R.B.; Bigal, M.E. Temporomandibular disorders and migraine chronification. Curr. Pain Headache Rep. 2009, 13, 314–318. [Google Scholar] [CrossRef]
- AAPD. Acquired Temporomandibular Disorders in Infants, Children, and Adolescents. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2019; Volume 2023, pp. 484–492. [Google Scholar]
- Horton, L.M.; John, R.M.; Karibe, H.; Rudd, P. Jaw disorders in the pediatric population. J. Am. Assoc. Nurse Pract. 2016, 28, 294–303. [Google Scholar] [CrossRef]
- Mehdipour, A.; Aghaali, M.; Janatifar, Z.; Saleh, A. Prevalence of Oral Parafunctional Habits in Children and Related Factors: An Observational Cross-sectional Study. Int. J. Clin. Pediatr. Dent. 2023, 16, 308–311. [Google Scholar] [CrossRef]
- Braido, G.; Campi, L.B.; Jordani, P.C.; Fernandes, G.; GonÇalves, D.A.G. Temporomandibular disorder, body pain and systemic diseases: Assessing their associations in adolescents. J. Appl. Oral Sci. Rev. FOB 2020, 28, e20190608. [Google Scholar] [CrossRef]
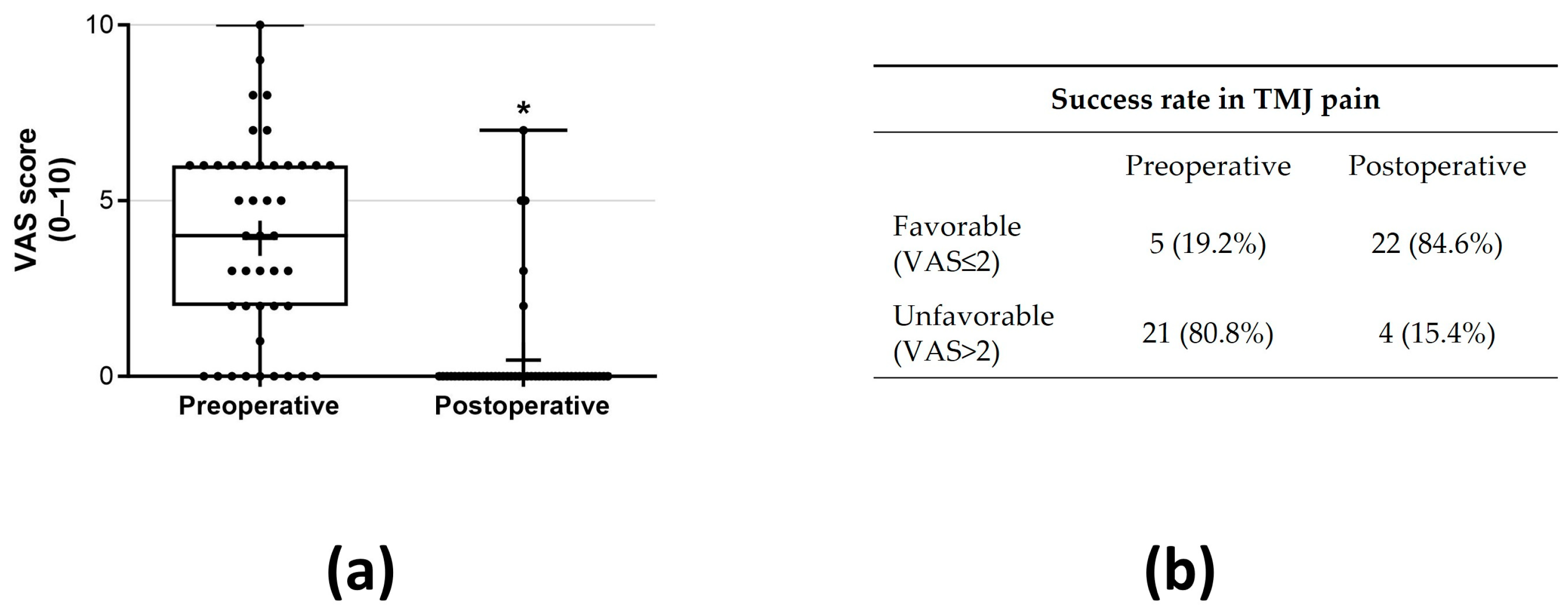
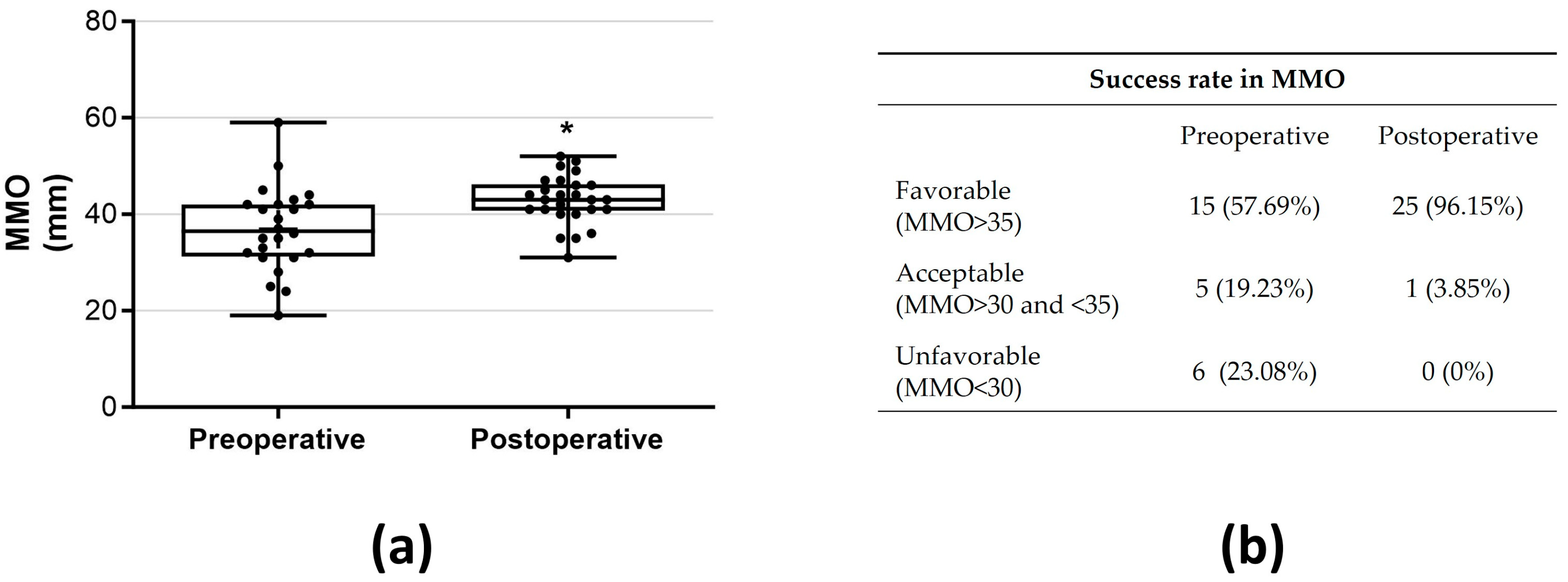

| Good | No pain or only mild pain level (VAS ≤ 2 on a 0–10 scale) and MMO ≥ 35 mm |
| Acceptable | No pain or only mild pain level (VAS ≤ 2 on a 0–10 scale) and MMO ≥ 30 mm and <35 mm |
| Failure | Constant or moderate pain (VAS > 2 on a 0–10 scale) and/or MMO < 30 mm |
| Number of Patients | 26 | |
|---|---|---|
| Sex | Number of patients (%) | |
| Female | 18 (69.2%) | |
| Male | 8 (30.8%) | |
| Mean age (mean ± SD) | 14.81 ± 2.30 (10–17) | |
| Parafunctional habits | Number of patients (%) | |
| Awake bruxism | 13 (50.0%) | |
| Sleep bruxism | 7 (26.9%) | |
| Past orofacial treatments/events | Number of patients (%) | |
| Orthodontic treatment | 8 (30.77%) | |
| Wisdom teeth removal | 2 (7.69%) | |
| Facial trauma | 2 (7.69%) | |
| Other comorbidities | Number of patients (%) | |
| Asthma | 4 (15.39%) | |
| Allergic rhinitis | 1 (3.85%) | |
| Depression | 1 (3.85%) | |
| Joints affected by arthrogenous disorder | Number of joints (%) | |
| Total | 48 (92.31%) | |
| Right side only | 0 (0%) | |
| Left side only | 4 (15.38%) | |
| Bilateral | 22 (84.62%) | |
| Arthrogenous diagnosis | Number of joints (%) | |
| DDwoR + arthralgia | 10 (20.83%) | |
| DDwR | 9 (18.75%) | |
| Arthralgia | 8 (16.67%) | |
| DDwR + arthralgia | 7 (14.58%) | |
| DDwoR | 4 (8.33%) | |
| DDwoR + OA | 3 (6.25%) | |
| DDwoR + OA + arthralgia | 2 (4.17%) | |
| DDwR + OA + arthralgia | 2 (4.17%) | |
| DDwoR+ condylar resorption | 1 (2.08%) | |
| DDwR + condylar resorption + arthralgia | 1 (2.08%) | |
| DDwoR + disc perforation | 1 (2.08%) | |
| Myogenous diagnosis | Number of patients (%) | |
| Myalgia | 18 (69.23%) | |
| I | 3 (11.54%) | |
| II | 7 (26.92%) | |
| III | 8 (30.77%) | |
| Treatment performed | Number of joints (%) | |
| TMJ arthrocentesis | 32 (66.67%) | |
| TMJ arthroscopy | 16 (33.33%) | |
| Follow-up period (days) | 419.2 ± 363.5 (31–1277 days) | |
| Success Rate | ||
|---|---|---|
| A Single Minimally Invasive TMJ Surgery | Minimally Invasive TMJ Surgery + Additional Arthrocentesis | |
| Good–acceptable | 20 (75.92%) | 22 (84.62%) |
| Failure | 6 (23.08%) | 4 (15.38%) |
| VAS Pain | MMO | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Minimally Invasive TMJ Surgery | N Joints (%) | Preoperative VAS Pain, M ± SD | p | Postoperative VAS Pain, M ± SD | p | Preoperative MMO, M ± SD | p | Posoperative MMO, M ± SD | p |
| TMJ arthrocentesis | 32 (66.67%) | 4.04 ± 2.70 | 0.84 | 0.52 ± 1.65 | 0.89 | 35.65 ± 7.75 | 0.86 | 43.76 ± 5.11 | 0.45 |
| TMJ arthroscopy | 16 (33.33%) | 3.76 ± 3.03 | 0.47 ± 1.38 | 37.56 ± 10.68 | 41.44 ± 4.93 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ângelo, D.F.; Lopes, C.S.; Sanz, D.; Faria-Teixeira, M.C.; Marques, R.; Maffia, F.; Cardoso, H.J. Temporomandibular Joint Minimally Invasive Procedures in the Pediatric Population: A Prospective Study. J. Clin. Med. 2024, 13, 672. https://doi.org/10.3390/jcm13030672
Ângelo DF, Lopes CS, Sanz D, Faria-Teixeira MC, Marques R, Maffia F, Cardoso HJ. Temporomandibular Joint Minimally Invasive Procedures in the Pediatric Population: A Prospective Study. Journal of Clinical Medicine. 2024; 13(3):672. https://doi.org/10.3390/jcm13030672
Chicago/Turabian StyleÂngelo, David Faustino, Cláudia Sacramento Lopes, David Sanz, Maria Cristina Faria-Teixeira, Rute Marques, Francesco Maffia, and Henrique José Cardoso. 2024. "Temporomandibular Joint Minimally Invasive Procedures in the Pediatric Population: A Prospective Study" Journal of Clinical Medicine 13, no. 3: 672. https://doi.org/10.3390/jcm13030672
APA StyleÂngelo, D. F., Lopes, C. S., Sanz, D., Faria-Teixeira, M. C., Marques, R., Maffia, F., & Cardoso, H. J. (2024). Temporomandibular Joint Minimally Invasive Procedures in the Pediatric Population: A Prospective Study. Journal of Clinical Medicine, 13(3), 672. https://doi.org/10.3390/jcm13030672








