Risk Factors for Postoperative Acute Kidney Injury Requiring Renal Replacement Therapy in Patients Undergoing Heart Valve Surgery
Abstract
1. Introduction
2. Methods
Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheruku, S.R.; Raphael, J.; Neyra, J.A.; Fox, A.A. Acute Kidney Injury after Cardiac Surgery: Prediction, Prevention, and Management. Anesthesiology 2023, 139, 880–898. [Google Scholar] [CrossRef] [PubMed]
- Tinica, G.; Brinza, C.; Covic, A.; Popa, I.V.; Tarus, A.; Bacusca, A.E.; Burlacu, A. Determinants of acute kidney injury after cardiac surgery: A systematic review. Rev. Cardiovasc. Med. 2020, 21, 601–610. [Google Scholar] [PubMed]
- Hu, J.; Chen, R.; Liu, S.; Yu, X.; Zou, J.; Ding, X. Global incidence and outcomes of adult patients with acute kidney injury after cardiac surgery: A systematic review and meta-analysis. J. Cardiothorac. Vasc. Anesth. 2016, 30, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Vives, M.; Hernandez, A.; Parramon, F.; Estanyol, N.; Pardina, B.; Muñoz, A.; Alvarez, P.; Hernandez, C. Acute kidney injury after cardiac surgery: Prevalence, impact and management challenges. Int. J. Nephrol. Renov. Dis. 2020, 12, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Nadim, M.K.; Forni, L.G.; Bihorac, A.; Hobson, C.; Koyner, J.L.; Shaw, A.; Arnaoutakis, G.J.; Ding, X.; Engelman, D.T.; Gasparovic, H.; et al. Cardiac and Vascular Surgery-Associated Acute Kidney Injury: The 20th International Consensus Conference of the ADQI (Acute Disease Quality Initiative) Group. J. Am. Heart Assoc. 2018, 7, e008834. [Google Scholar] [CrossRef]
- Mariscalco, G.; Lorusso, R.; Dominici, C.; Renzulli, A.; Sala, A. Acute kidney injury: A relevant complication after cardiac surgery. Ann. Thorac. Surg. 2011, 92, 1539–1547. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Bellomo, R. Cardiac surgery-associated acute kidney injury: Risk factors, pathophysiology and treatment. Nat. Rev. Nephrol. 2017, 13, 697–711. [Google Scholar]
- Tecson, K.M.; Brown, D.; Choi, J.W.; Feghali, G.; Gonzalez-Stawinski, G.V.; Hamman, B.L.; Hebeler, R.; Lander, S.R.; Lima, B.; Potluri, S.; et al. Major adverse renal and cardiac events after coronary angiography and cardiac surgery. Ann. Thorac. Surg. 2018, 105, 1724–1730. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 2012, 120, c178-84. [Google Scholar] [CrossRef] [PubMed]
- McIlroy, D.; Bellomo, R.; Billings, F., IV; Karkouti, K.; Prowle, J.; Shaw, A.; Myles, P. Systematic review and consensus definitions for the standardised endpoints in perioperative medicine (StEP) initiative: Renal endpoints. Br. J. Anaesth. 2018, 121, 1013–1024. [Google Scholar] [CrossRef]
- Peng, K.; McIlroy, D.R.; Bollen, B.A.; Billings, F.T.; Zarbock, A.; Popescu, W.M.; Fox, A.A.; Shore-Lesserson, L.; Zhou, S.; Geube, M.A.; et al. Society of Cardiovascular Anesthesiologists clinical practice update for management of acute kidney injury associated with cardiac surgery. Anesth. Analg. 2022, 135, 744–756. [Google Scholar] [CrossRef]
- Ronco, C.; Bellomo, R.; Kellum, J.A. Acute kidney injury. Lancet 2019, 394, 1949–1964. [Google Scholar] [CrossRef] [PubMed]
- Massoth, C.; Zarbock, A.; Meersch, M. Acute kidney injury in cardiac surgery. Crit. Care Clin. 2021, 37, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L.; Bratteby, L.; Ekroth, R.; Hallhagen, S.; Joachimsson, P.; Van der Linden, J.; Wesslén, O. Renal function during cardiopulmonary bypass: Influence of pump flow and systemic blood pressure. Eur. J. Cardiothorac. Surg. 1994, 8, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Lannemyr, L.; Bragadottir, G.; Krumbholz, V.; Redfors, B.; Sellgren, J.; Ricksten, S.-E. Effects of cardiopulmonary bypass on renal perfusion, filtration, and oxygenation in patients undergoing cardiac surgery. Anesthesiology 2017, 126, 205–213. [Google Scholar] [CrossRef]
- Karim, H.M.R.; Yunus, M.; Saikia, M.K.; Kalita, J.P.; Mandal, M. Incidence and progression of cardiac surgery-associated acute kidney injury and its relationship with bypass and cross clamp time. Ann. Card. Anaesth. 2017, 20, 22–27. [Google Scholar] [PubMed]
- Ranucci, M.; Romitti, F.; Isgrò, G.; Cotza, M.; Brozzi, S.; Boncilli, A.; Ditta, A. Oxygen delivery during cardiopulmonary bypass and acute renal failure after coronary operations. Ann. Thorac. Surg. 2005, 80, 2213–2220. [Google Scholar] [CrossRef] [PubMed]
- Sgouralis, I.; Evans, R.G.; Gardiner, B.S.; Smith, J.A.; Fry, B.C.; Layton, A.T. Renal hemodynamics, function, and oxygenation during cardiac surgery performed on cardiopulmonary bypass: A modeling study. Physiol. Rep. 2015, 3, e12260. [Google Scholar] [CrossRef]
- Clifford, K.M.; Selby, A.R.; Reveles, K.R.; Teng, C.; Hall, R.G., II; McCarrell, J.; Alvarez, C.A. The risk and clinical implications of antibiotic-associated acute kidney injury: A review of the clinical data for agents with signals from the Food and Drug Administration’s Adverse Event Reporting System (FAERS) Database. Antibiotics 2022, 11, 1367. [Google Scholar] [CrossRef]
- Duchnowski, P.; Śmigielski, W. Usefulness of myocardial damage biomarkers in predicting cardiogenic shock in patients undergoing heart valve surgery. Kardiol. Pol. 2024, 82, 423–426. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2021, 42, 3599–3726. [Google Scholar]
- Silverton, N.A.; Lofgren, L.R.; Hall, I.E.; Stoddard, G.J.; Melendez, N.P.; Van Tienderen, M.; Shumway, S.; Stringer, B.J.; Kang, W.-S.; Lybbert, C.; et al. Noninvasive urine oxygen monitoring and the risk of acute kidney injury in cardiac surgery. Anesthesiology 2021, 135, 406–418. [Google Scholar] [CrossRef] [PubMed]
- A Peng, X.; Zhu, T.; Chen, Q.; Zhang, Y.; Zhou, R.; Li, K.; Hao, X. Simple machine learning model for the prediction of acute kidney injury following noncardiac surgery in geriatric patients: A prospective cohort study. BMC Geriatr. 2024, 24, 549. [Google Scholar] [CrossRef] [PubMed]
- Wald, R.; Beaubien-Souligny, W.; Chanchlani, R.; Clark, E.G.; Neyra, J.A.; Ostermann, M.; Silver, S.A.; Vaara, S.; Zarbock, A.; Bagshaw, S.M. Delivering optimal renal replacement therapy to critically ill patients with acute kidney injury. Intensive Care Med. 2022, 48, 1368–1381. [Google Scholar] [CrossRef]
- Desai, A.S.; Jarcho, A. Levosimendan for the Low Cardiac Output Syndrome after Cardiac Surgery. N. Engl. J. Med. 2017, 376, 2076–2078. [Google Scholar] [CrossRef]
- Denault, A.Y.; Deschamps, A.; Couture, P. Intraoperative hemodynamic instability during and after separation from cardiopulmonary bypass. Semin. Cardiothorac. Vasc. Anesth. 2010, 14, 165–182. [Google Scholar] [CrossRef]
- Carrara, A.; Peluso, L.; Baccanelli, F.; Parrinello, M.; Santarpino, G.; Giroletti, L.; Graniero, A.; Agnino, A.; Albano, G. Relationship between Preoperative Red Cell Distribution Width and Prolonged Postoperative Use of Catecholamines in Minimally Invasive Mitral Valve Surgery Patients: A Retrospective Cohort Study. J. Clin. Med. 2024, 13, 5736. [Google Scholar] [CrossRef]
- Weidemann, F.; Herrmann, S.; Störk, S.; Niemann, M.; Frantz, S.; Lange, V.; Beer, M.; Gattenlohner, S.; Voelker, W.; Ertl, G.; et al. Impact of myocardial fibrosis in patients with symptomatic severe aortic stenosis. Circulation 2009, 120, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Chin, C.W.; Shah, A.S.; McAllister, D.A.; Joanna Cowell, S.; Alam, S.; Langrish, J.P.; Strachan, F.E.; Hunter, A.L.; Choy, A.M.; Lang, C.C.; et al. High-sensitivity troponin I concentrations are a marker of an advanced hypertrophic response and adverse outcomes in patients with aortic stenosis. Eur. Heart J. 2014, 35, 2312–2321. [Google Scholar] [CrossRef] [PubMed]
- Kočková, R.; Línková, H.; Hlubocká, Z.; Mědílek, K.; Tuna, M.; Vojáček, J.; Skalský, I.; Černý, Š.; Malý, J.; Hlubocký, J.; et al. Multiparametric Strategy to Predict Early Disease Decompensation in Asymptomatic Severe Aortic Regurgitation. Circ. Cardiovasc. Imaging 2022, 15, e014901. [Google Scholar] [CrossRef] [PubMed]
- Ferruci, L.; Guralnik, J.M.; Studenski, S.; Fried, L.P.; Cutler, G.B., Jr.; Walston, J.D.; The Interventions on Frailty Working Group. Designing randomized aimed at preventing or delaying functional decline and disability in frail, older persons: A consensus report. J. Am. Geriatr. Soc. 2004, 52, 625–634. [Google Scholar] [CrossRef]
- Velissaris, D.; Pantzaris, N.; Koniari, I.; Koutsogiannis, N.; Karamouzos, V.; Kotroni, I.; Skroumpelou, A.; Ellul, J. C-Reactive protein and frailty in the elderly: A literature review. J. Clin. Med. Res. 2017, 9, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Bruunsgaard, H. The clinical impact of systemic low-level inflammation in elderly populations. With special reference to cardiovascular disease, dementia and mortality. Dan. Med. Bull. 2006, 53, 285–309. [Google Scholar]
| Preoperative Characteristics of Patients | Values All Patients (n = 603) | Values Patients with RRT (n = 43) | Values Patients Without RRT (n = 560) | p-Value |
|---|---|---|---|---|
| Age, years | 65 (57–71) | 70 (59–76) | 65 (56–70) | <0.001 |
| Male: men, n (%) | 353 (58) | 23 (53) | 330 (58) | 0.59 |
| LV ejection fraction, (%) | 60 (50–65) | 58 (45–65) | 60 (50–65) | 0.38 |
| EuroSCORE II, % | 2.4 (1.4–3.9) | 3.5 (2.4–5.5) | 2.35 (1.35–3.8) | <0.001 |
| Atrial fibrillation, n (%) | 235 (38) | 27 (63) | 208 (37) | <0.001 |
| Previous myocardial infarction, n (%) | 44 (7) | 4 (9) | 40 (7) | 0.59 |
| Diabetes mellitus, n (%) | 93 (15) | 9 (21) | 84 (15) | 0.29 |
| Hemoglobin, g/dL | 13.7 (12.7–14.7) | 12.8 (10.8–13.2) | 13.8 (12.8–14.7) | <0.001 |
| GFR, mL/min/1.73 m2, n (%) | 67 (55–81) | 54 (36–64) | 68 (57–84) | <0.001 |
| Creatinine, [mmol/L] | 68 (46–93) | 118 (90–142) | 65 (45–92) | <0.001 |
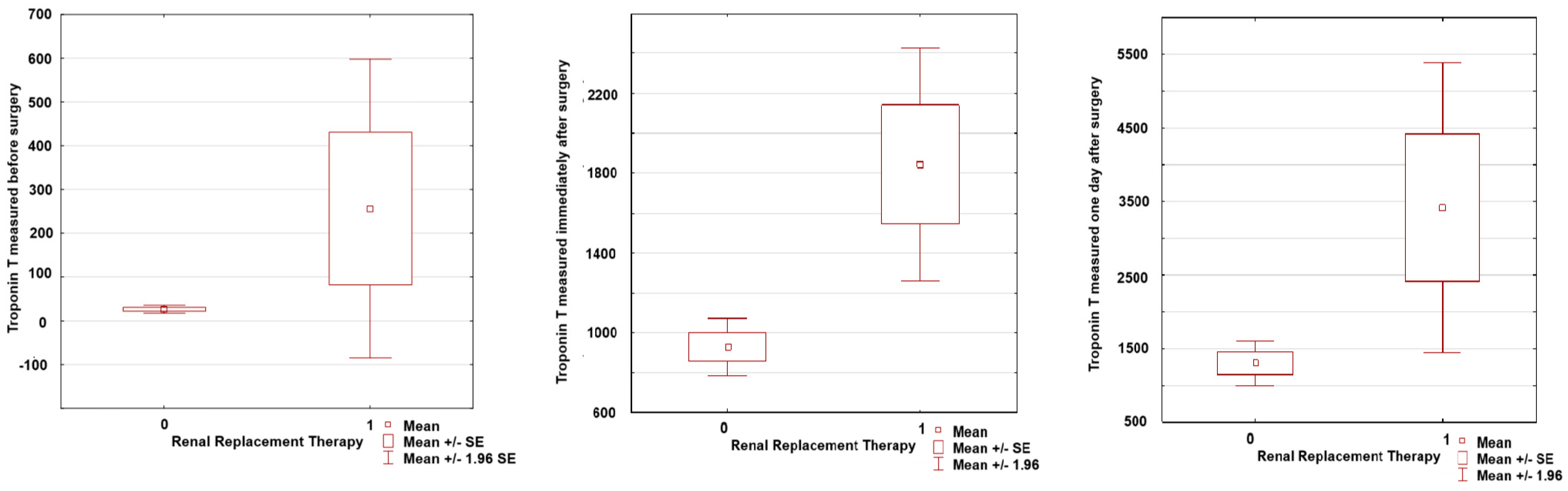
| TnT, ng/L | 14.4 (8–33) | 24 (11.7–36) | 12(7–21) | <0.001 |
| Nt-proBNP, pg/mL | 924 (321–2239) | 2951 (934–4480) | 855 (294–1939) | <0.001 |
| CRP, mg/dL | 0.3 (0.1–0.5) | 0.4 (0.2–0.6) | 0.2 (0.1–0.4) | <0.001 |
| Aortic cross-clamp time, min | 87 (60–131) | 140 (78–155) | 87 (60–129) | ns |
| Cardiopulmonary bypass time, min | 114 (83–169) | 190 (115–215) | 113 (79–160) | 0.055 |
| Postoperative characteristics of patients | ||||
| Prolonged Postoperative Use of Catecholamines (more than 48 h), n (%) | 202 (33) | 39 (90) | 163 (29) | <0.001 |
| Mechanical circulatory support, n (%) | 22 (4) | 11 (25) | 11 (2) | <0.001 |
| Multiple organ dysfunction syndrome, n (%) | 40 (6) | 34 (79) | 6 (1) | <0.001 |
| Postoperative stroke, n (%) | 19 (3) | 11 (25) | 8 (1) | <0.001 |
| Hospital stay after surgery, day | 11 (8–17) | 28 (12–36) | 10 (8–16) | <0.001 |
| ICU, day | 9 (8–14) | 17 (6–30) | 3 (2–5) | <0.001 |
| Re-sternotomy, n (%) | 80 (13) | 9 (21) | 71 (12) | 0.12 |
| 30-day mortality, n (%) | 29 (4.8) | 18 (41) | 11 (1,9) | <0.001 |
| TnT II, ng/L | 732 (387–1501) | 2011 (952–2670) | 648 (366–1261) | <0.001 |
| TnT I, ng/L | 645 (361–1121) | 1262 (712–2223) | 599 (345–976) | <0.001 |
| Main procedures | ||||
| AVR, n (%) | 321 (53) | 15 (34) | 306 (54) | 0.01 |
| AVP, n (%) | 10 (2) | 3 (2) | 9 (2) | 0.72 |
| AVR + MVR, n (%) | 55 (9) | 12 (28) | 43 (8) | <0.001 |
| AVR + MVP, n (%) | 11 (2) | 0 (0) | 11 (2) | 0.35 |
| AVP + MVP, n (%) | 3 (0.5) | 0 (0) | 3 (0.5) | 0.5 |
| MVP, n (%) | 97 (16) | 11 (25) | 88 (15) | 0.36 |
| MVR, n (%) | 107 (17) | 6 (14) | 101 (18) | 0.49 |
| Concomitant procedure | ||||
| CABG, n (%) | 88 (15) | 11 (25) | 74 (13) | 0.02 |
| TVR, n (%) | 3 (0,5) | 0 (0) | 3 (0.5) | 0.63 |
| TVP, n (%) | 159 (26) | 17 (39) | 142 (25) | 0.04 |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | Odds Ratio | 95% Cl | p-Value | Odds Ratio | 95% Cl | p-Value |
| Age, years | 1.073 | 1.035–1.112 | <0.001 | 1.084 | 1.031–1.1140 | <0.001 |
| GFR < 60 mL/min/1.73 m2, n (%) | 0.955 | 0.937–0.973 | <0.001 | |||
| Hemoglobin, g/dL | 0.642 | 0.532–0.776 | <0.001 | |||
| NT-proBNP, pg/mL | 2.241 | 1.695–2.961 | <0.001 | |||
| CRP, mg/dL | 2.069 | 1.517–2.822 | <0.001 | 1.727 | 1.157–2.576 | 0.007 |
| EuroSCORE II, % | 1.168 | 1.093–1.249 | <0.001 | |||
| Atrial fibrillation, n (%) | 2.855 | 1.501–5.431 | 0.001 | |||
| Prolonged Postoperative Use of Catecholamines (more than 48 h), n (%) | 14.378 | 5.972–34-612 | <0.001 | 5.399 | 1.973–14.770 | 0.001 |
| TnT, ng/L | 2.063 | 1.541–2.761 | <0.001 | |||
| TnT I, ng/L | 2.500 | 1.745–3.583 | <0.001 | |||
| TnT II, ng/L | 2.401 | 1.768–3.261 | <0.001 | 2.058 | 1.361–3.113 | <0.001 |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | Odds Ratio | 95% Cl | p-Value | Odds Ratio | 95% Cl | p-Value |
| Age, years | 1.097 | 1.050–1.147 | <0.001 | 1.118 | 1.049–1.328 | <0.001 |
| GFR < 60 mL/min/1.73 m2, n (%) | 0.954 | 0.934–0.975 | <0.001 | |||
| Hemoglobin, g/dL | 0.625 | 0.505–0.774 | <0.001 | |||
| NT-proBNP, pg/mL | 2.271 | 1.655–3.118 | <0.001 | |||
| CRP, mg/dL | 2.236 | 1.585–3.156 | <0.001 | 2.017 | 1.278–3.181 | 0.002 |
| EuroSCORE II, % | 1.153 | 1.079–1.232 | <0.001 | |||
| Atrial fibrillation, n (%) | 3.715 | 1.723–8.008 | <0.001 | |||
| Prolonged Postoperative Use of Catecholamines (more than 48 h), n (%) | 21.468 | 6.480–71.121 | <0.001 | 7.618 | 2.181–26.610 | 0.001 |
| TnT, ng/L | 2.193 | 1.602–3.001 | <0.001 | |||
| TnT I, ng/L | 2.609 | 1.754–3.881 | <0.001 | |||
| TnT II, ng/L | 2.390 | 1.721–3.331 | <0.001 | 1.830 | 1.161–2.883 | 0.009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duchnowski, P.; Śmigielski, W. Risk Factors for Postoperative Acute Kidney Injury Requiring Renal Replacement Therapy in Patients Undergoing Heart Valve Surgery. J. Clin. Med. 2024, 13, 7811. https://doi.org/10.3390/jcm13247811
Duchnowski P, Śmigielski W. Risk Factors for Postoperative Acute Kidney Injury Requiring Renal Replacement Therapy in Patients Undergoing Heart Valve Surgery. Journal of Clinical Medicine. 2024; 13(24):7811. https://doi.org/10.3390/jcm13247811
Chicago/Turabian StyleDuchnowski, Piotr, and Witold Śmigielski. 2024. "Risk Factors for Postoperative Acute Kidney Injury Requiring Renal Replacement Therapy in Patients Undergoing Heart Valve Surgery" Journal of Clinical Medicine 13, no. 24: 7811. https://doi.org/10.3390/jcm13247811
APA StyleDuchnowski, P., & Śmigielski, W. (2024). Risk Factors for Postoperative Acute Kidney Injury Requiring Renal Replacement Therapy in Patients Undergoing Heart Valve Surgery. Journal of Clinical Medicine, 13(24), 7811. https://doi.org/10.3390/jcm13247811






