Changes in Prolactin and Insulin Resistance in PCOS Patients Undergoing Metformin Treatment: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
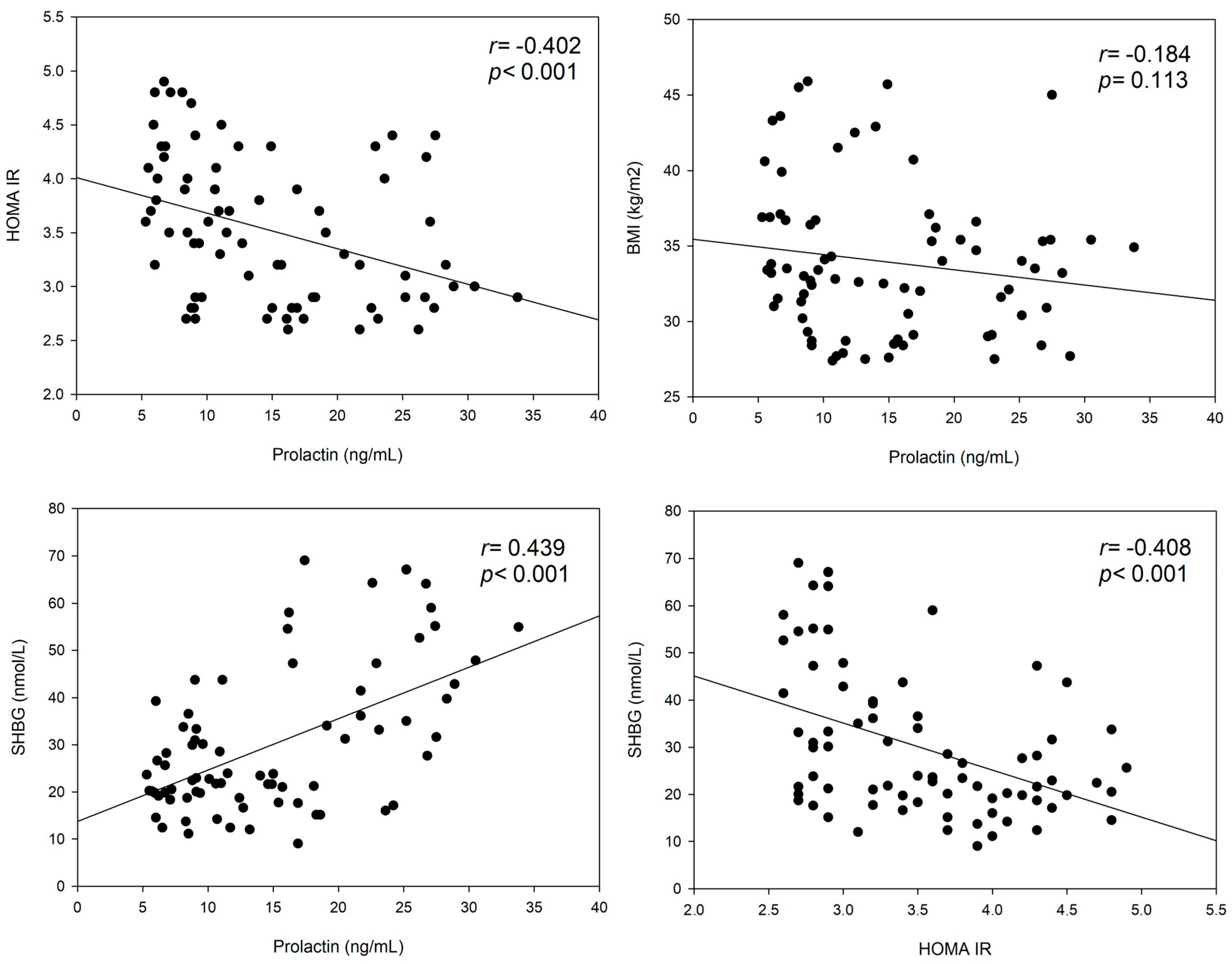
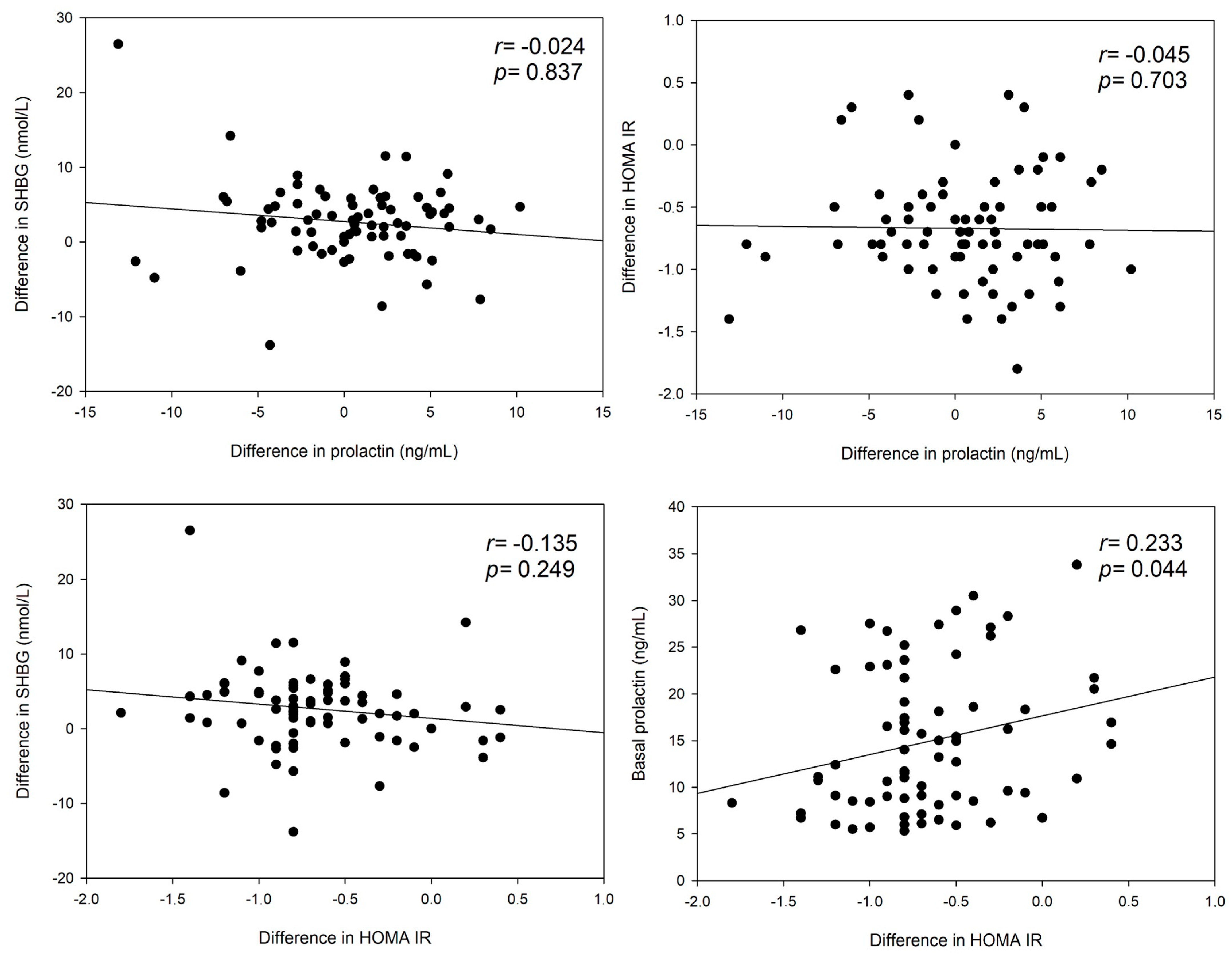
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, W.; Pang, Y. Metabolic Syndrome and PCOS: Pathogenesis and the Role of Metabolites. Metabolites 2021, 11, 869. [Google Scholar] [CrossRef] [PubMed]
- Teede, H.J.; Tay, C.T.; Laven, J.; Dokras, A.; Moran, L.J.; Piltonen, T.T.; Costello, M.F.; Boivin, J.; Redman, L.M.; Boyle, J.A.; et al. Recommendations from the 2023 International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. Hum. Reprod. 2023, 38, 1655–1679. [Google Scholar] [CrossRef]
- Chandrasekaran, S.; Sagili, H. Metabolic syndrome in women with polycystic ovary syndrome. Obstet. Gynaecol. 2018, 20, 245–252. [Google Scholar] [CrossRef]
- Johnson, N.P. Metformin use in women with polycystic ovary syndrome. Ann. Transl. Med. 2014, 2, 56. [Google Scholar] [PubMed]
- Lashen, H. Role of metformin in the management of polycystic ovary syndrome. Ther. Adv. Endocrinol. Metab. 2010, 1, 117–128. [Google Scholar] [CrossRef]
- Al-Nozha, O.; Habib, F.; Mojaddidi, M.; El-Bab, M.F. Body weight reduction and metformin: Roles in polycystic ovary syndrome. Pathophysiology 2013, 20, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Palomba, S.; Falbo, A.; Zullo, F.; Orio, F., Jr. Evidence-Based and Potential Benefits of Metformin in the Polycystic Ovary Syndrome: A Comprehensive Review. Endocr. Rev. 2009, 30, 1–50. [Google Scholar] [CrossRef]
- Lord, J.M.; Flight, I.H.; Norman, R.J. Metformin in polycystic ovary syndrome: Systematic review and meta-analysis. BMJ 2003, 327, 951–953. [Google Scholar] [CrossRef]
- Ponce, A.J.; Galván-Salas, T.; Lerma-Alvarado, R.M.; Ruiz-Herrera, X.; Hernández-Cortés, T.; Valencia-Jiménez, R.; Cárdenas-Rodríguez, L.E.; de la Escalera, G.M.; Clapp, C.; Macotela, Y. Low prolactin levels are associated with visceral adipocyte hypertrophy and insulin resistance in humans. Endocrine 2020, 67, 331–343. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Lu, J.; Xu, Y.; Li, M.; Sun, J.; Zhang, J.; Xu, B.; Xu, M.; Chen, Y.; Bi, Y.; et al. Circulating prolactin associates with diabetes and impaired glucose regulation: A population-based study. Diabetes Care 2013, 36, 1974–1980. [Google Scholar] [CrossRef]
- Yang, H.; Lin, J.; Li, H.; Liu, Z.; Chen, X.; Chen, Q. Prolactin is associated with insulin resistance and beta-cell dysfunction in infertile women with polycystic ovary syndrome. Front. Endocrinol. 2021, 12, 571229. [Google Scholar] [CrossRef] [PubMed]
- Albu, A.; Florea, S.; Fica, S. Is prolactin the missing link in adipose tissue dysfunction of polycystic ovary syndrome patients? Endocrine 2016, 51, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Macotela, Y.; Ruiz-Herrera, X.; Vázquez-Carrillo, D.I.; Ramírez-Hernandez, G.; Martínez de la Escalera, G.; Clapp, C. The beneficial metabolic actions of prolactin. Front. Endocrinol. 2022, 13, 1001703. [Google Scholar] [CrossRef]
- Krysiak, R.; Kowalcze, K.; Szkróbka, W.; Okopień, B. Impaired Prolactin-Lowering Effects of Metformin in Women with Polycystic Ovary Syndrome. J. Clin. Med. 2023, 12, 5474. [Google Scholar] [CrossRef] [PubMed]
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum. Reprod. 2004, 19, 41–47. [Google Scholar] [CrossRef]
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J.; International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil. Steril. 2018, 110, 364–379. [Google Scholar] [CrossRef]
- Tosi, F.; Bonora, E.; Moghetti, P. Insulin resistance in a large cohort of women with polycystic ovary syndrome: A comparison between euglycaemic-hyperinsulinaemic clamp and surrogate indexes. Hum. Reprod. 2017, 32, 2515–2521. [Google Scholar] [CrossRef]
- Ott, J.; Egarter, C.; Aguilera, A. Dydrogesterone after 60 years: A glance at the safety profile. Gynecol. Endocrinol. 2022, 38, 279–287. [Google Scholar] [CrossRef] [PubMed]
- ISO 15189; Medical laboratories—Requirements for Quality and Competence. International Organization for Standardization: Geneva, Switzerland, 2022.
- Boegl, M.; Dewailly, D.; Marculescu, R.; Steininger, J.; Ott, J.; Hager, M. The LH:FSH Ratio in Functional Hypothalamic Amenorrhea: An Observational Study. J. Clin. Med. 2024, 13, 1201. [Google Scholar] [CrossRef]
- Hager, M.; Nouri, K.; Imhof, M.; Egarter, C.; Ott, J. The impact of a standardized micronutrient supplementation on PCOS-typical parameters: A randomized controlled trial. Arch. Gynecol. Obstet. 2019, 300, 455–460. [Google Scholar] [CrossRef]
- Selzer, C.; Ott, J.; Dewailly, D.; Marculescu, R.; Steininger, J.; Hager, M. Prolactin levels in functional hypothalamic amenorrhea: A retrospective case-control study. Arch. Gynecol. Obstet. 2024, 309, 651–658. [Google Scholar] [CrossRef]
- Wagner, R.; Heni, M.; Linder, K.; Ketterer, C.; Peter, A.; Böhm, A.; Hatziagelaki, E.; Stefan, N.; Staiger, H.; Häring, H.-U.; et al. Age dependent association of serum prolactin with glycaemia and insulin sensitivity in humans. Acta Diabetol. 2014, 51, 71–78. [Google Scholar] [CrossRef]
- Chen, F.; Liao, Y.; Chen, M.; Yin, H.; Chen, G.; Huang, Q.; Chen, L.; Yang, X.; Zhang, W.; Wang, P.; et al. Evaluation of the Efficacy of Sex Hormone-Binding Globulin in Insulin Resistance Assessment Based on HOMA-IR in Patients with PCOS. Reprod. Sci. 2021, 28, 2504–2513. [Google Scholar] [CrossRef]
- Tűű, L.; Nas, K.; Török, M.; Várbíró, S. SHBG Levels Do Not Correlate with Insulin Levels in PCOS with Appropriate Fasting Insulin Sensitivity. J. Clin. Med. 2024, 13, 838. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.; Minjie, C.; Weichun, Z.; Huihuang, Y.; Guishan, C.; Qingxia, H.; Xiaoping, Y.; Lan, C.; Ping, W.; Chujia, L.; et al. Efficacy of sex hormone-binding globulin on predicting metabolic syndrome in newly diagnosed and untreated patients with polycystic ovary syndrome. Hormones 2020, 19, 439–445. [Google Scholar] [CrossRef]
- Lim, S.S.; Norman, R.J.; Davies, M.J.; Moran, L.J. The effect of obesity on polycystic ovary syndrome: A systematic review and meta-analysis. Obes. Rev. 2013, 14, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Plymate, S.R.; Matej, L.A.; Jones, R.E.; Friedl, K.E. Inhibition of sex hormone-binding globulin production in the human hepatoma (Hep G2) cell line by insulin and prolactin. J. Clin. Endocrinol. Metab. 1988, 67, 460–464. [Google Scholar] [CrossRef]
- Zhu, J.L.; Chen, Z.; Feng, W.J.; Long, S.L.; Mo, Z.C. Sex hormone-binding globulin and polycystic ovary syndrome. Clin. Chim. Acta 2019, 499, 142–148. [Google Scholar] [CrossRef]
- Billa, E.; Kapolla, N.; Nicopoulou, S.C.; Koukkou, E.; Venaki, E.; Milingos, S.; Antsaklis, A.; Adamopoulos, D.A. Metformin administration was associated with a modification of LH, prolactin and insulin secretion dynamics in women with polycystic ovarian syndrome. Gynecol. Endocrinol. 2009, 25, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Hamad, I.N.; Kadhim, S.A.A.; Fawzi, H.A.; Al-Temimi, S.M.; Mohammad, B.; Swadi, A. Effects of combined metformin and cabergoline versus metformin alone on ovarian and hormonal activities in Iraqi patients with PCOS and hyperprolactinemia: A randomized clinical trial. J. Med. Life 2023, 16, 1615–1621. [Google Scholar] [PubMed]
- Ghaneei, A.; Jowkar, A.; Hasani Ghavam, M.R.; Ghaneei, M.E. Cabergoline plus metformin therapy effects on menstrual irregularity and androgen system in polycystic ovary syndrome women with hyperprolactinemia. Iran. J. Reprod. Med. 2015, 13, 93–100. [Google Scholar] [PubMed]
- Elsersy, M.A. Efficacy of combined cabergoline and metformin compared to metformin alone on cycle regularity in patients with polycystic ovarian disease with hyperprolactinemia: A randomized clinical trial. J. Obstet. Gynecol. India 2017, 67, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Di Guardo, F.; Ciotta, L.; Monteleone, M.; Palumbo, M. Male equivalent polycystic ovarian syndrome: Hormonal, metabolic, and clinical aspects. Int. J. Fertil. Steril. 2020, 14, 79–83. [Google Scholar] [PubMed]
- Krysiak, R.; Kowalcze, K.; Okopień, B. Pituitary effects of metformin in men with early-onset androgenic alopecia. J. Clin. Pharmacol. 2022, 62, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Krysiak, R.; Szkróbka, W.; Okopień, B. Endogenous testosterone determines metformin action on prolactin levels in hyperprolactinaemic men: A pilot study. Basic Clin. Pharmacol. Toxicol. 2020, 126, 110–115. [Google Scholar] [CrossRef]
- Delcour, C.; Robin, G.; Young, J.; Dewailly, D. PCOS and Hyperprolactinemia: What do we know in 2019? Clin. Med. Insights Reprod. Health 2019, 13, 1179558119871921. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murdoch, A.P.; Dunlop, W.; Kendall-Taylor, P. Studies of prolactin secretion in polycystic ovary syndrome. Clin. Endocrinol. 1986, 24, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Laatikainen, T.; Tulenheimo, A. Prolactin pulsatility in polycystic ovarian disease. J. Endocrinol. Investig. 1985, 8, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Venturoli, S.; Porcu, E.; Fabbri, R.; Magrini, O.; Gammi, L.; Paradisi, R.; Forcacci, M.; Bolzani, R.; Flamigni, C. Episodic pulsatile secretion of FSH, LH, prolactin, oestradiol, oestrone, and LH circadian variations in polycystic ovary syndrome. Clin. Endocrinol. 1988, 28, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, C.; Rampini, P.; Malinverni, A.; Scarduelli, C.; Benco, R.; Caldara, R.; Barbieri, C.; Testori, G.; Crosignani, P.G. Inhibition of luteinizing hormone release by dopamine infusion in healthy women and in various pathophysiologi- cal conditions. Acta Endocrinol. 1981, 97, 436–440. [Google Scholar]
- Leblanc, H.; Lachelin, G.C.; Abu-Fadil, S.; Yen, S.S. Effects of dopamine infusion on pituitary hormone secretion in humans. J. Clin. Endocrinol. Metab. 1976, 43, 668–674. [Google Scholar] [CrossRef]
- Pehrson, J.J.; Jaffee, W.L.; Vaitukaitis, J.L. Effect of dopamine on gonadotropin- releasing hormone-induced gonadotropin secretion in postmenopausal women. J. Clin. Endocrinol. Metab. 1983, 56, 889–892. [Google Scholar] [CrossRef] [PubMed]
- Quigley, M.E.; Rakoff, J.S.; Yen, S.S. Increased luteinizing hormone sensitivity to dopamine inhibition in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 1981, 52, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Barnes, R.B.; Lobo, R.A. Central opioid activity in polycystic ovary syndrome with and without dopaminergic modulation. J. Clin. Endocrinol. Metab. 1985, 61, 779–782. [Google Scholar] [CrossRef] [PubMed]
- Barnes, R.B.; Mileikowsky, G.N.; Cha, K.Y.; Spencer, C.A.; Lobo, R.A. Effects of dopa- mine and metoclopramide in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 1986, 63, 506–509. [Google Scholar] [CrossRef]
- Buvat, J.; Buvat-Herbaut, M.; Marcolin, G.; Racadot, A.; Fourlinnie, J.C.; Beuscart, R.; Fossati, P. A double blind controlled study of the hormonal and clinical effects of bromocriptine in the polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 1986, 63, 119–124. [Google Scholar] [CrossRef]
- Steingold, K.A.; Lobo, R.A.; Judd, H.L.; Lu, J.K.; Chang, R.J. The effect of bromocrip- tine on gonadotropin and steroid secretion in polycystic ovarian disease. J. Clin. Endocrinol. Metab. 1986, 62, 1048–1051. [Google Scholar] [CrossRef] [PubMed]
- Azziz, R.; Carmina, E.; Chen, Z.; Dunaif, A.; Laven, J.S.; Legro, R.S.; Lizneva, D.; Natterson-Horowtiz, B.; Teede, H.J.; Yildiz, B.O. Polycystic ovary syndrome. Nat. Rev. Dis. Primers 2016, 2, 16057. [Google Scholar] [CrossRef] [PubMed]
- Robin, G.; Catteau-Jonard, S.; Young, J.; Dewailly, D. Physiopathological link between polycystic ovary syndrome and hyperprolactinemia: Myth or reality? GynecolObstetFertil 2011, 39, 141–145. [Google Scholar] [CrossRef]
- Christin-Maître, S.; Delemer, B.; Touraine, P.; Young, J. Prolactinoma and estro- gens: Pregnancy, contraception and hormonal replacement therapy. Ann. Endocrinol. 2007, 68, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Touraine, P.; Goffin, V. Physiologie de la prolactine. EMC-Gynécologie 2015, 11, 1–13. [Google Scholar]
- Corenblum, B.; Donovan, L. The safety of physiological estrogen plus progestin replacement therapy and with oral contraceptive therapy in women with patho- logical hyperprolactinemia. FertilSteril 1993, 59, 671–673. [Google Scholar]
- Testa, G.; Vegetti, W.; Motta, T.; Alagna, F.; Bianchedi, D.; Carlucci, C.; Bianchi, M.; Parazzini, F.; Crosignani, P.G. Two-year treatment with oral contraceptives in hyperprolactinemic patients. Contraception 1998, 58, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Acién, P.; Mauri, M.; Gutierrez, M. Clinical and hormonal effects of the combina- tion gonadotrophin-releasing hormone agonist plus oral contraceptive pills con- taining ethinyl-oestradiol (EE) and cyproterone acetate (CPA) versus the EE-CPA pill alone on polycystic ovarian disease-related hyperandrogenisms. Hum. Reprod. 1997, 12, 423–429. [Google Scholar] [PubMed]
| Age (years) 1 | 26 (23; 29) | |
| BMI (kg/m2) 1 | 33.2 (30.2; 36.6) | |
| PCOS phenotype 2 | A | 20 (26.7) |
| B | 19 (25.3) | |
| C | 19 (25.3) | |
| D | 17 (22.7) | |
| LH (mIU/mL) 1 | 10.2 (7.7; 15.8) | |
| FSH (mIU/mL) 1 | 5.6 (4.6; 6.3) | |
| LH:FSH ratio 1 | 2.1 (1.4; 2.7) | |
| Total testosterone (ng/mL) 1 | 0.54 (0.41; 0.69) | |
| SHBG (nmol/L) 1 | 23.8 (19.1; 39.2) | |
| HOMA IR 1 | 3.5 (2.9; 4.1) | |
| Prolactin (ng/mL) 1 | 12.7 (8.5; 21.7) | |
| Parameter | Before Treatment | 6–8 Months Follow-Up | p | Difference |
|---|---|---|---|---|
| LH (mIU/mL) | 10.2 (7.7; 15.8) | 9.7 (7.9; 12.8) | <0.001 | −0.35 (−2.2; 0.7) |
| FSH (mIU/mL) | 5.6 (4.6; 6.3) | 5.8 (4.9; 6.8) | 0.460 | 0.3 (−0.5; 1.3) |
| LH:FSH ratio | 2.1 (1.4; 2.7) | 1.8 (1.5; 2.1) | <0.001 | −0.2 (−0.7; 0.1) |
| Total testosterone (ng/mL) | 0.54 (0.41; 0.69) | 0.48 (0.38; 0.62) | 0.105 | −0.04 (−0.08; 0.0) |
| SHBG (nmol/L) | 23.8 (19.1; 39.2) | 29.0 (21.6; 40.9) | 0.264 | 2.8 (0.0; 5.1) |
| HOMA IR | 3.5 (2.9; 4.1) | 2.8 (2.3; 3.3) | <0.001 | −0.8 (−0.9; −0.5) |
| Prolactin (ng/mL) | 12.7 (8.5; 21.7) | 13.7 (9.3; 19.5) | 0.737 | 0.6 (−2.7; 3.6) |
| Prolactin ≤ 14.9 ng/mL (n = 42) | Prolactin > 14.9 ng/mL (n = 33) | ||
|---|---|---|---|
| Prolactin (ng/mL) | Before treatment | 8.9 (6.7; 10.9) | 22.6 (17.1; 26.8) |
| Follow-up | 10.3 (7.5; 14.4) | 21.6 (13.9; 27.3) | |
| p | 0.018 | 0.422 | |
| HOMA IR | Before treatment | 3.8 (3.4; 4.3) | 3.0 (2.8; 3.6) |
| Follow-up | 3.0 (2.5; 3.5) | 2.6 (13.9; 27.3) | |
| p | <0.001 | <0.001 | |
| SHBG (nmol/L) | Before treatment | 21.7 (18.7; 28.3) | 36.1 (21.1; 54.7) |
| Follow-up | 25.1 (19.8; 33.1) | 39.8 (26.7; 55.5) | |
| p | 0.058 | 0.717 | |
| LH:FSH ratio | Before treatment | 2.1 (1.4; 2.7) | 2.1 (1.5; 2.8) |
| Follow-up | 1.8 (1.5; 2.2) | 1.7 (1.4; 2.2) | |
| p | <0.001 | <0.001 | |
| Testosterone (ng/mL) | Before treatment | 0.58 (0.45; 0.70) | 0.51 (0.37; 0.64) |
| Follow-up | 0.51 (0.39; 0.63) | 0.45 (0.37; 0.58) | |
| p | 0.206 | 0.327 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goldstein, T.; Ott, J.; Katzensteiner, P.; Krysiak, R.; Marculescu, R.; Boegl, M.; Hager, M. Changes in Prolactin and Insulin Resistance in PCOS Patients Undergoing Metformin Treatment: A Retrospective Study. J. Clin. Med. 2024, 13, 7781. https://doi.org/10.3390/jcm13247781
Goldstein T, Ott J, Katzensteiner P, Krysiak R, Marculescu R, Boegl M, Hager M. Changes in Prolactin and Insulin Resistance in PCOS Patients Undergoing Metformin Treatment: A Retrospective Study. Journal of Clinical Medicine. 2024; 13(24):7781. https://doi.org/10.3390/jcm13247781
Chicago/Turabian StyleGoldstein, Tal, Johannes Ott, Paula Katzensteiner, Robert Krysiak, Rodrig Marculescu, Magdalena Boegl, and Marlene Hager. 2024. "Changes in Prolactin and Insulin Resistance in PCOS Patients Undergoing Metformin Treatment: A Retrospective Study" Journal of Clinical Medicine 13, no. 24: 7781. https://doi.org/10.3390/jcm13247781
APA StyleGoldstein, T., Ott, J., Katzensteiner, P., Krysiak, R., Marculescu, R., Boegl, M., & Hager, M. (2024). Changes in Prolactin and Insulin Resistance in PCOS Patients Undergoing Metformin Treatment: A Retrospective Study. Journal of Clinical Medicine, 13(24), 7781. https://doi.org/10.3390/jcm13247781







